Abstract
Background
Although studies and interest in sarcopenia have increased, it is still a matter of debate which muscle mass index better represents the aging process. We compared 3 indices for muscle mass (appendicular skeletal muscle mass [ASM]/weight, ASM/height2, and the body mass index [BMI]-adjusted muscle mass index [ASM/BMI]) to determine which better reflected the aging process in terms of the decline in bone mineral density (BMD), visual acuity (VA), hearing power, renal function, pulmonary function, and handgrip strength.
Methods
We performed a retrospective cross-sectional study using the Korea National Health and Nutrition Examination Survey in the Korean population. Between 2008 and 2011, a total of 14,415 men and 17,971 women aged 10 years or older participated in the study. We plotted the changes in the 3 indices of muscle mass and compared these with changes in BMD, VA, hearing power, renal function, pulmonary function, and handgrip strength according to each age group.
Results
The ASM/BMI showed similar changes in terms of surrogate markers of the aging process, while the ASM/weight and ASM/height2 showed no correlation.
Conclusions
Among muscle indices for sarcopenia, only the ASM/BMI represented the aging process.
Keywords: Aging, Sarcopenia
INTRODUCTION
Sarcopenia is an age-related decline in the skeletal muscle mass and muscle strength.[1,2] Since the first introduction by Rosenberg and Roubenoff [1] the etiology, pathophysiology, risk factors, and consequences of sarcopenia have been widely investigated worldwide.[3,4,5,6,7,8,9,10] Because sarcopenia is associated with the impairment of physical function, the risk of falls, as well as excess mortality,[3,11,12,13] it has been known as a new disease entity in geriatric population.[14,15]
Although several research groups have suggested different operational diagnostic criteria and algorithms for sarcopenia, low muscle mass, low muscle strength, and decreased physical performance are commonly used to define sarcopenia.[14,16,17,18,19]
Although the accurate measurement of muscle mass is an essential to diagnose sarcopenia,[20] several study groups from different regions has used one of the differently calculated indices for muscle mass to define sarcopenia.[14,16,17,18,19]
Some used weight-adjusted muscle mass to diagnose sarcopenia, and to present association between sarcopenia and medical problems.[17] The European Working Group on Sarcopenia in Older People (EWGSOP) and International Working Group on Sarcopenia (IWGS) suggested muscle mass adjusted for height squared, although they used different algorithms and cut off values to diagnose sarcopenia.[14,16] The Foundation for the National Institutes of Health (FNIH) Sarcopenia Project suggested muscle mass adjusted for body mass index (BMI), after applying a classification and regression tree (CART) analytical approach.[19]
However, diagnostic index of muscle mass remains still debate, because each consensus group has used different diagnostic index for muscle mass for sarcopenia.[14,16,17,18,19]
These different indices for muscle mass gave rise to very diverse prevalence estimates in the elderly population.[21,22,23]
Although the diagnostic index for muscle mass should be estimated to represent aging process sufficiently, considering sarcopenia as one of aging process, there has been no study investigating which index of muscle mass represents aging process.
The purpose of this study was to investigate which index of muscle mass represent aging process, using data of the Korea National Health and Nutrition Examination Survey (KNHANES).
METHODS
This study is a cross-sectional study on dataset from the Fourth and Fifth KNHANES conducted during 2008 to 2011, a nationally representative cross sectional and population-based survey, conducted by the Korea Centers for Disease Control and Prevention (KCDC).
We included 32,386 participants who were aged 10 years or older in our analysis.
1. Assessment of muscle mass
The dual energy X-ray absorptiometry (DXA; Hologic Inc., Bedford, MA, USA) was used to measure the appendicular skeletal muscle mass (ASM, kg), defined as the sum of the lean soft tissue mass of the arms and legs.
Three indices for muscle mass were calculated and plotted according to each age group.
One was the ASM divided by height squared (ASM/height2, expressed as kg/m2) proposed by Baumgartner et al.[2] another was ASM as a percentage of body (ASM/weight) expressed as a percentage, which was modified from the study of Janssen et al.[17]. The other was ASM divided by BMI (ASM/BMI, expressed as m2).[19]
2. Assessment of aging process
After consensus meetings, T-scores of bone mineral density (BMD; presence of osteoporosis), visual acuity (VA) hearing power, renal function and pulmonary function were selected as surrogate markers of aging process. In addition, handgrip strength, which was obtained from another cohort of KNHANSE between 2014 and 2015, was also plotted according to each age group.
3. BMD
T-score of BMD of the total femur were obtained by DXA (Hologic Inc.). The densitometers were calibrated daily with a phantom supplied by the manufacturer to maintain the stability of the DXA measurements. The BMD of total femur were measured with DXA using standard procedures. T-score of BMD was plotted according to the age groups.
4. VA
Distant VA was measured at a distance of 4 m by using an international standard vision chart (Jin' s vision chart, Seoul, Korea).[24] Presenting VA (PVA) was measured and plotted. The PVA was considered the uncorrected VA for subjects who did not wear glasses and the spectacle-corrected VA for those who wore glasses.[25]
5. Hearing power
Pure-tone audiometry, the gold standard for hearing loss evaluation, was conducted by a SA 203 audiometer (Entomed, Malmö, Sweden) in the study population. The test was conducted in a soundproof booth and the instruction was given by certain otolaryngologists trained to operate the audiometry. Subjects used supra-auricular headphones in a soundproof booth, and only air conduction was measured. Study subjects pushed a button when they heard a tone. Test frequencies were 0.5, 1, 2, 3, 4, and 6 kHz. The maximum dB was defined as the higher value between the mean threshold of hearing level in right and left ear as a marker representing hearing power.[26]
6. Renal function
Renal function was estimated as creatinine clearance (CrCl), that was calculated based on the Cockcroft and Gault equation; CrCl=([140-age]×ideal body weight)/(serum creatinine×72) (×0.85 for females).[27] Creatinine clearance was plotted according to each age group.
7. Pulmonary function
A model 1,022 Spirometer (SensorMedics, Yorba Linda, CA, USA) was used for pulmonary function test (PFT). Spirometry was conducted with standardized equipment following guidelines from the American Thoracic Society/European Respiratory Society.[28] Spirometry was repeated at least 3 times to ensure reproducibility and validity. The PFT results were calculated based on the reference values from published predictive equations for Korean patient populations, using computer programs and reviewed by trained physicians.[29] Forced vital capacity was plotted according to the age group.
8. Handgrip strength
Handgrip strength refers to coordination between the 4 fingers and the thumb and is a measure of hand power used to grip an object. In the KNHANES, handgrip strength was measured in kilograms using a digital grip strength dynamometer (TKK 5401; Takei, Niigata, Japan). The test is repeated 3 times with each hand, starting with the dominant hand.[30] The maximal strength was used to plot in each age group.
9. Statistical analysis
Data analysis was performed using SPSS Statistics for Windows, version 16 (IBM Corp., Armonk, NY, USA). In order to determine which index of muscle mass represents aging process, we plotted the value of each index according to age groups and compared each plot with plots of variables (VA, hearing power, renal function, and pulmonary function) representing aging process. And, we also plotted the handgrip strength, one of the important surrogate markers to define sarcopenia, according to each age group.
RESULTS
A total of 32,386 Korean adults aged 10 years or older were included in this study: 4,516, 3,624, 5,776, 5,307, 4,978, 4,467, 3,024, and 694 participants belonged to the 10 to 19, 20 to 29, 30 to 39, 40 to 49, 50 to 59, 60 to 69, 70 to 79, and 80 years or older age groups, respectively.
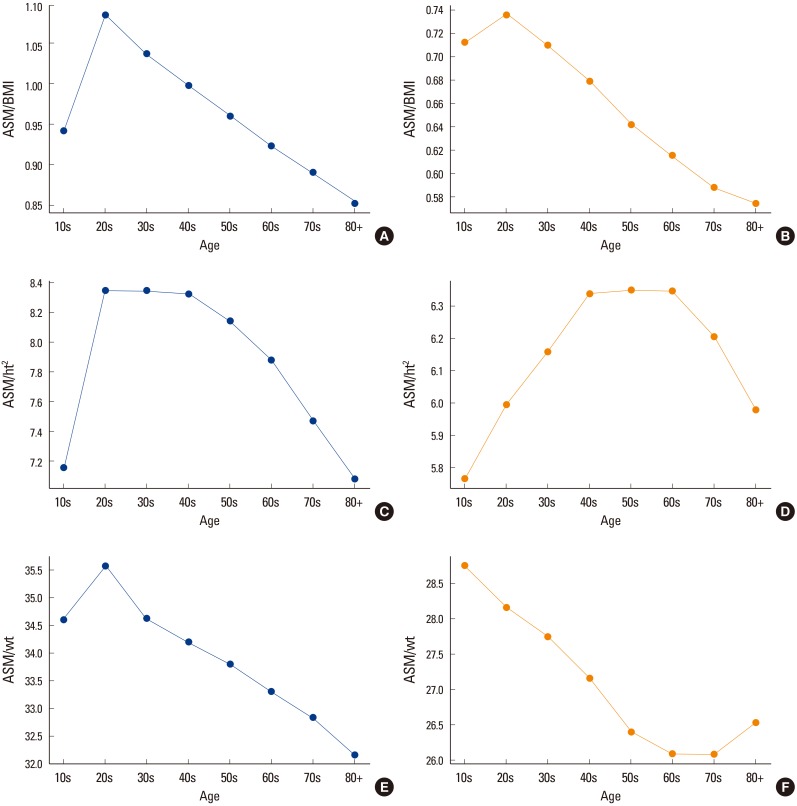
Each index (ASM/height2, ASM/weight, and ASM/BMI) for muscle mass showed different pattern with each other (Fig. 1).
Fig. 1. (A) Body mass index (BMI)-adjusted appendicular skeletal muscle mass (ASM) of men in each age group. (B) BMI-adjusted ASM of women in each age group. (C) Height square-adjusted ASM of men in each age group. (D) Height square-adjusted ASM of women in each age group. (E) Weight-adjusted ASM of men in each age group. (F) Weight-adjusted ASM of women in each age group. ht, height; wt, weight.
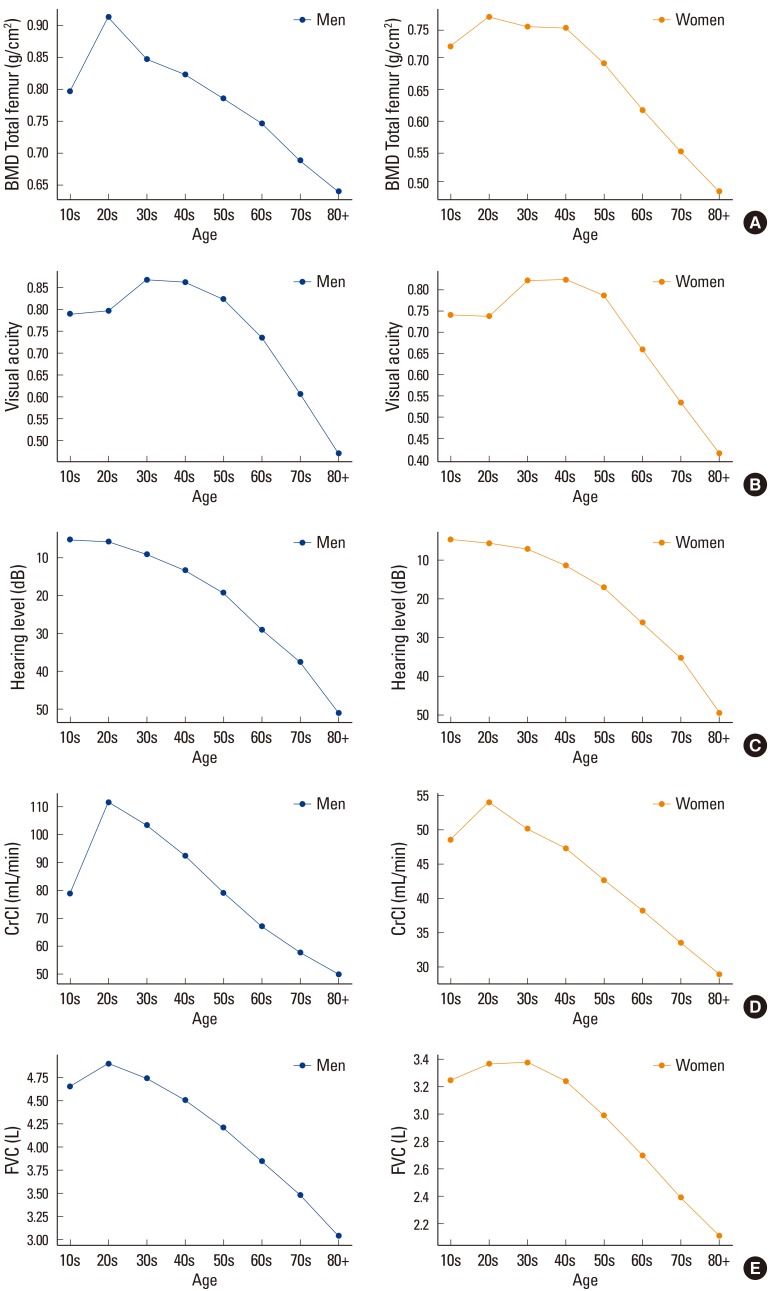
With the peak of 20 to 29/30 to 39 years of age, BMD, VA, hearing power, renal function, and pulmonary function decreased with age (Fig. 2). Only hearing power was falling steadily from 10 to 19 age group.
Fig. 2. (A) Bone mineral density of total femur in each age group. (B) Visual acuity of total femur in each age group. (C) Hearing power of total femur in each age group. (D) Renal function of total femur in each age group. (E) Pulmonary function of total femur in each age group. BMD, bone mineral density; CrCl, creatinine clearance; FVC, forced vital capacity.
When we compared graph patterns of ASM/height2, ASM/weight, and ASM/BMI, only ASM/BMI showed similar patterns with the surrogate markers (BMD, VA, hearing power, renal function, and pulmonary function) of aging process (Fig. 1).
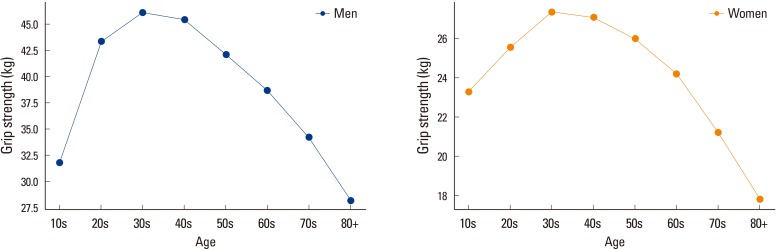
The handgrip strength decreased with age after the peak of 30 to 39 years of age (Fig. 3).
Fig. 3. Handgrip strength in each age group.
DISCUSSION
Sarcopenia has been defined as low muscle mass, low muscle strength, and decreased physical performance,[14,16,17,18,19] although several research groups have used different operational diagnostic criteria and algorithms for sarcopenia.
To evaluate muscle strength, hand grip strength has been measured as index of muscle strength.[9,20,31] For physical performance, gait speed has been used as index of muscle performance.[20] Although muscle mass is not specifically a predictor of muscle strength or physical performance, it is significantly correlated with these parameters. Therefore, the accurate measurement of muscle mass is an essential to diagnose sarcopenia.[20]
For measurement of muscle mass, fat-free mass derived from a whole body DXA scan are the most widely used and best characterized measurement tool,[20] although several measurement methods for skeletal muscle mass are available in research and clinical field.[20,32]
Several study groups from different regions has used one of the differently calculated indices for muscle mass to define sarcopenia.[14,16,17,18,19]
Historically, ASM, that is a sum of the muscle mass of both arms and legs, is usually used for the skeletal muscle mass index. However, muscle mass is generally correlated with whole body size, indicating that subjects with a larger body size may have higher muscle mass.[33] Therefore, when evaluating the adequacy of muscle mass, the level of ASM has been used after adjusting differently for body size by using height squared (ASM/height2), weight (ASM/weight), or BMI (ASM/ BMI).[2,17,19]
Historically, Since Baumgartner et al.[2] suggested ASM/height2 in the New Mexico Elder Health Survey, many researchers have used this index to define sarcopenia, and some have reported associations between this index and many clinical outcomes including physical disability and frailty.[12,34,35] However, because this index is positively correlated with BMI, it has the limitation that subjects with a greater BMI due to a larger amount of fat are less likely to be classified as having sarcopenia.[36,37]
In 2002, Janssen et al.[17] proposed a weight-adjusted muscle mass index. Sarcopenia as defined by this weight-adjusted skeletal muscle index was significantly related to functional impairment and disability.[17] This weight-adjusted model was subsequently modified as ASM/weight. This index has been widely used as an alternative method together with the height squared-adjusted index described by Baumgartner et al.[2] and Janssen et al.[17].
More recently, the FNIH Sarcopenia Project introduced the ASM/BMI index in 2014.[19] This index is growing recently.[19,38] The recent study reported that this new sarcopenia definition by FNIH can predict 6-year mortality among Korean men.[39]
Since 2010, several definitional algorithms have been developed by using differently calculated index for muscle mass. The EWGSOP and IWGS used muscle mass adjusted for height squared, although they used different algorithms and cut off values to diagnose sarcopenia.[14,16] The FNIH Sarcopenia Project [19] suggested muscle mass adjusted for BMI, after applying a CART analytical approach.[19] It is now clear that different definitional approaches yield very different prevalence estimates in the elderly population.[21]
Historically, height square or weight adjusted muscle mass has been used to diagnose sarcopenia.[2,17] Recently, to adopt concept of sarcopenia, outcome-based definition of sarcopenia has been conducted in term of muscle mass.[19,32]
In this study, we compared changes of these indices according to age group and found ASM/BMI is best similar with change of surrogate markers of aging process. Moreover, the only ASM/BMI showed the similar pattern of handgrip strength, which has been used as one of the most important diagnostic criteria of sarcopenia.
And these changes were more prominent in men group rather than women group.
Generally, men have larger body size and lower fat percent compared with women. These can explain the study results.
There is a limitation in this study. We cannot compare the change of muscle indices with the longitudinal aging process in individual level, because we conducted cross-sectional study.
CONCLUSION
In conclusion, our results showed that ASM/BMI is best index of muscle mass to reflect aging process, among several tools to measure sarcopenia.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Rosenberg IH, Roubenoff R. Stalking sarcopenia. Ann Intern Med. 1995;123:727–728. doi: 10.7326/0003-4819-123-9-199511010-00014. [DOI] [PubMed] [Google Scholar]
- 2.Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol. 1998;147:755–763. doi: 10.1093/oxfordjournals.aje.a009520. [DOI] [PubMed] [Google Scholar]
- 3.Landi F, Liperoti R, Fusco D, et al. Sarcopenia and mortality among older nursing home residents. J Am Med Dir Assoc. 2012;13:121–126. doi: 10.1016/j.jamda.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 4.Amigues I, Schott AM, Amine M, et al. Low skeletal muscle mass and risk of functional decline in elderly community-dwelling women: the prospective EPIDOS study. J Am Med Dir Assoc. 2013;14:352–357. doi: 10.1016/j.jamda.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Gao L, Jiang J, Yang M, et al. Prevalence of sarcopenia and associated Factors in Chinese community-dwelling elderly: comparison between rural and urban areas. J Am Med Dir Assoc. 2015;16:1003.e1–1003.e6. doi: 10.1016/j.jamda.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 6.Bae EJ, Kim YH. Factors affecting sarcopenia in Korean adults by age groups. Osong Public Health Res Perspect. 2017;8:169–178. doi: 10.24171/j.phrp.2017.8.3.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moon SS. Low skeletal muscle mass is associated with insulin resistance, diabetes, and metabolic syndrome in the Korean population: the Korea National Health and Nutrition Examination Survey (KNHANES) 2009-2010. Endocr J. 2014;61:61–70. doi: 10.1507/endocrj.ej13-0244. [DOI] [PubMed] [Google Scholar]
- 8.Landi F, Onder G, Bernabei R. Sarcopenia and diabetes: two sides of the same coin. J Am Med Dir Assoc. 2013;14:540–541. doi: 10.1016/j.jamda.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Leenders M, Verdijk LB, van der Hoeven L, et al. Patients with type 2 diabetes show a greater decline in muscle mass, muscle strength, and functional capacity with aging. J Am Med Dir Assoc. 2013;14:585–592. doi: 10.1016/j.jamda.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Morley JE, Malmstrom TK, Rodriguez-Mañas L, et al. Frailty, sarcopenia and diabetes. J Am Med Dir Assoc. 2014;15:853–859. doi: 10.1016/j.jamda.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 11.Hirani V, Blyth F, Naganathan V, et al. Sarcopenia is associated with incident disability, institutionalization, and mortality in community-dwelling older men: the concord health and ageing in men project. J Am Med Dir Assoc. 2015;16:607–613. doi: 10.1016/j.jamda.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Morley JE, Abbatecola AM, Argiles JM, et al. Sarcopenia with limited mobility: an international consensus. J Am Med Dir Assoc. 2011;12:403–409. doi: 10.1016/j.jamda.2011.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pfortmueller CA, Lindner G, Exadaktylos AK. Reducing fall risk in the elderly: risk factors and fall prevention, a systematic review. Minerva Med. 2014;105:275–281. [PubMed] [Google Scholar]
- 14.Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc. 2011;12:249–256. doi: 10.1016/j.jamda.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cesari M, Vellas B. Sarcopenia: a novel clinical condition or still a matter for research? J Am Med Dir Assoc. 2012;13:766–767. doi: 10.1016/j.jamda.2012.07.020. [DOI] [PubMed] [Google Scholar]
- 16.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–423. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002;50:889–896. doi: 10.1046/j.1532-5415.2002.50216.x. [DOI] [PubMed] [Google Scholar]
- 18.Chen LK, Liu LK, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101. doi: 10.1016/j.jamda.2013.11.025. [DOI] [PubMed] [Google Scholar]
- 19.Studenski SA, Peters KW, Alley DE, et al. The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerontol A Biol Sci Med Sci. 2014;69:547–558. doi: 10.1093/gerona/glu010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mijnarends DM, Meijers JM, Halfens RJ, et al. Validity and reliability of tools to measure muscle mass, strength, and physical performance in community-dwelling older people: a systematic review. J Am Med Dir Assoc. 2013;14:170–178. doi: 10.1016/j.jamda.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 21.Kim KM, Jang HC, Lim S. Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean J Intern Med. 2016;31:643–650. doi: 10.3904/kjim.2016.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coin A, Sarti S, Ruggiero E, et al. Prevalence of sarcopenia based on different diagnostic criteria using DEXA and appendicular skeletal muscle mass reference values in an Italian population aged 20 to 80. J Am Med Dir Assoc. 2013;14:507–512. doi: 10.1016/j.jamda.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 23.Lee WJ, Liu LK, Peng LN, et al. Comparisons of sarcopenia defined by IWGS and EWGSOP criteria among older people: results from the I-Lan longitudinal aging study. J Am Med Dir Assoc. 2013;14:528.e1–528.e7. doi: 10.1016/j.jamda.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 24.Jin YH. A new LogMAR vision chart: Jin's vision chart. J Korean Ophthalmol Soc. 1997;38:2036–2044. [Google Scholar]
- 25.Suh YW, Lee JS, Heo H, et al. Vision improvement with refractive correction does not completely exclude major eye diseases: analyses of visually impaired South Korean population in the Korea National Health and Nutrition Examination Survey 2009-2011. J Ophthalmol. 2017;2017:3412904. doi: 10.1155/2017/3412904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lee J, Han K, Song JJ, et al. Sarcopenia and hearing loss in older Koreans: findings from the Korea national health and nutrition examination survey (KNHANES) 2010. PLoS One. 2016;11:e0150281. doi: 10.1371/journal.pone.0150281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 28.American Thoracic Society. Standardization of Spirometry, 1994 Update. Am J Respir Crit Care Med. 1995;152:1107–1136. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 29.Choi JK, Paek D, Lee JO. Normal predictive values of spirometry in Korean population. Tuberc Respir Dis. 2005;58:230–242. [Google Scholar]
- 30.Kwak Y, Kim Y. Quality of life and subjective health status according to handgrip strength in the elderly: a cross-sectional study. Aging Ment Health. 2017 doi: 10.1080/13607863.2017.1387766. [DOI] [PubMed] [Google Scholar]
- 31.Roh YH, Noh JH, Gong HS, et al. Effect of low appendicular lean mass, grip strength, and gait speed on the functional outcome after surgery for distal radius fractures. Arch Osteoporos. 2017;12:41. doi: 10.1007/s11657-017-0335-2. [DOI] [PubMed] [Google Scholar]
- 32.Heymsfield SB, Gonzalez MC, Lu J, et al. Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc. 2015;74:355–366. doi: 10.1017/S0029665115000129. [DOI] [PubMed] [Google Scholar]
- 33.Gallagher D, DeLegge M. Body composition (sarcopenia) in obese patients: implications for care in the intensive care unit. JPEN J Parenter Enteral Nutr. 2011;35:21s–28s. doi: 10.1177/0148607111413773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abe T, Thiebaud RS, Loenneke JP, et al. Influence of severe sarcopenia on cardiovascular risk factors in nonobese men. Metab Syndr Relat Disord. 2012;10:407–412. doi: 10.1089/met.2012.0057. [DOI] [PubMed] [Google Scholar]
- 35.Jeon YK, Shin MJ, Kim MH, et al. Low pulmonary function is related with a high risk of sarcopenia in community-dwelling older adults: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008-2011. Osteoporos Int. 2015;26:2423–2429. doi: 10.1007/s00198-015-3152-8. [DOI] [PubMed] [Google Scholar]
- 36.Newman AB, Kupelian V, Visser M, et al. Sarcopenia: alternative definitions and associations with lower extremity function. J Am Geriatr Soc. 2003;51:1602–1609. doi: 10.1046/j.1532-5415.2003.51534.x. [DOI] [PubMed] [Google Scholar]
- 37.Estrada M, Kleppinger A, Judge JO, et al. Functional impact of relative versus absolute sarcopenia in healthy older women. J Am Geriatr Soc. 2007;55:1712–1719. doi: 10.1111/j.1532-5415.2007.01436.x. [DOI] [PubMed] [Google Scholar]
- 38.McLean RR, Shardell MD, Alley DE, et al. Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: the foundation for the National Institutes of Health (FNIH) sarcopenia project. J Gerontol A Biol Sci Med Sci. 2014;69:576–583. doi: 10.1093/gerona/glu012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moon JH, Kim KM, Kim JH, et al. Predictive values of the new sarcopenia index by the foundation for the national institutes of health sarcopenia project for mortality among older Korean adults. PLoS One. 2016;11:e0166344. doi: 10.1371/journal.pone.0166344. [DOI] [PMC free article] [PubMed] [Google Scholar]