Abstract
Objective: The aim of this study was to determine the prevalence of curable and pseudoarthrosis stages of adolescent lumbar spondylolysis under high school students complaining of and seeking medical consultation for low back pain.
Patients and Methods: We analyzed age, sex, morbidity, presence of spina bifida occulta (SBO), and competitive sport discipline of patients with lumbar spondylolysis. We then stratified their pathological stage using a modified classification system via magnetic resonance imaging and computed tomography.
Results: Of 507 patients, 451 lesions in 268 patients were diagnosed with lumbar spondylolysis (average age, 14.7 years; sex ratio, 215:53 male/female). Morbidity levels were as follows: L1, 1 lesion in 1 patient; L2, 9 lesions in 5 patients; L3, 38 lesions in 25 patients; L4, 106 lesions in 74 patients; L5, 297 lesions in 189 patients, and SBO verified in 111 patients. A total of 264 patients played a specific sport: baseball, 93; soccer, 49; volleyball, 21; track and field, 21; basketball, 20; others, 164. The prevalence of curable- and pseudoarthrosis-stage lumbar spondylolysis was 206 lesions in 142 patients, and 141 lesions in 87 patients, respectively.
Conclusion: With 59.3% of patients having curable-stage lumbar spondylolysis, adolescent athletes with low back pain are urged to seek consultation. Furthermore, clinicians should perform magnetic resonance imaging to avoid misdiagnosis.
Keywords: adolescent, lumbar spondylolysis, stage, pseudoarthrosis
Introduction
Lumbar spondylolysis is the primary cause of fatigue fracture, and presents as low back pain in adolescent athletes. As the symptoms of lumbar spondylolysis are slight compared with those of limb fatigue fractures, patients may not seek medical consultation. Although many athletes experience low back pain due to spondylolysis, the overall condition is difficult to understand.
Many adolescent athletes with complaints of low back pain visit our hospital. They undergo magnetic resonance imaging (MRI) to observe the presence of bone marrow edema around the pedicle, which signifies curable lumbar spondylolysis. With positive findings of bone marrow edema, patients undergo computed tomography (CT), where the shapes of the axial and sagittal defects are assessed to determine the stage of lumbar spondylolysis. For curable fresh fractures with bone marrow edema, the goal is to obtain bony fusion through conservative therapy. Hence, the athlete would be prohibited from participating in sports and would undergo physiotherapy. A semi-hard lumbosacral back brace would also be prescribed and worn. In the case of a pseudoarthrotic lesion without the prospect of bone fusion, the aim of therapy is the relief of low back pain. Thus, overall, the goal of therapy is to return to competition without low back pain.
This study aimed to analyze the characteristics of adolescent athletes presenting with low back pain upon their first hospital visit, and to further assess their stages of lumbar spondylolysis. Furthermore, this study aimed to determine the prevalence of curable and pseudoarthrosis stages of adolescent lumbar spondylolysis.
Patients and Methods
All procedures involving human participants were in accordance with the ethical standards of the institutional research committee (NO 17-01) and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. From April 2014 to March 2017, 507 adolescents presented to our hospital with the chief complaint of low back pain. Patients were diagnosed as having lumbar spondylolysis based on the presence of a fracture line in the pars interarticularis. Imaging was conducted via plain X ray, CT, or by observing a high signal change around the pedicle using short T1 inversion recovery via MRI.
We evaluated the occupation of lumbar spondylolysis in patients who visited our hospital with complaint of low back pain. Furthermore, we analyzed the age, sex, morbidity, presence of spina bifida occulta (SBO), and competitive sport discipline in patients with lumbar spondylolysis. We calculated the proportion of spondylolysis accompanying low back pain, and compared between sexes using a chi-square test. According to our previous research, we stratified all patient’s pathological stage using either a modified classification via MRI and axial slice classification via CT (as per Sairyo et al.1); Figure 1a–h), or via sagittal slice classification using CT (as per Oba2); Figure 2a–l).
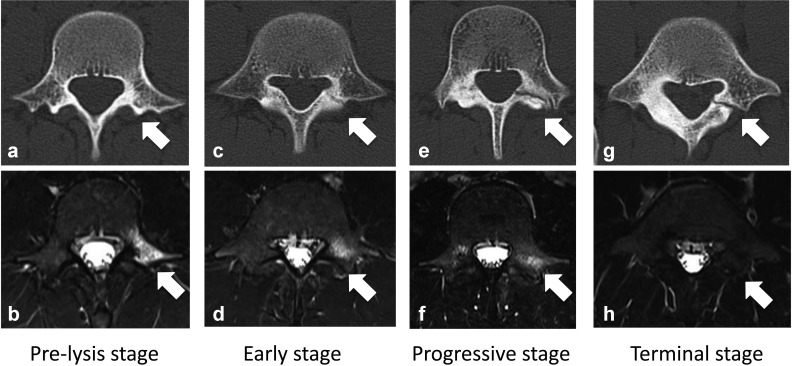
Figure 1.
Axial slice classification. (a, b) Pre-lysis stage: no fracture line visible on CT, but bone marrow edema present on MRI. (c, d) Early stage: partial gap on CT, and bone marrow edema on MRI. (e, f) Progressive stage: clear gap on CT, and bone marrow edema on MRI. (g, h) Terminal stage: defect on CT, but no bone marrow edema on MRI. CT, computed tomography; MRI, magnetic resonance imaging. Figures a, c, e and g were taken with CT, and Figures b, d, f and h were taken with MRI.
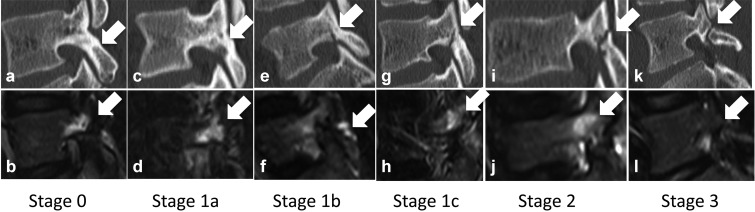
Figure 2.
Sagittal slice classification. (a, b) Stage 0: no fracture line visible on CT, but bone marrow edema visible on MRI. (c, d) Stage 1a: partial bone absorption on CT, and bone marrow edema on MRI. (e, f) Stage 1b: partial fracture line less than half of lamina thickness on CT, and bone marrow edema on MRI. (g, h) Stage 1c: partial fracture line more than half of lamina thickness on CT, and bone marrow edema on MRI. (i, j) Stage 2: penetrated fracture line on CT, and bone marrow edema on MRI. (k, l) Stage 3: penetrated fracture line on CT, but no bone marrow edema on MRI. CT, computed tomography; MRI, magnetic resonance imaging.
If bilateral lesions were found on one vertebra in the same patient, they were counted as two lesions. Lesions on multiple vertebral levels were also counted separately. Recurrent cases with multiple hospital visits were counted as separate cases. A t-test was used as a statistical analysis.
Results
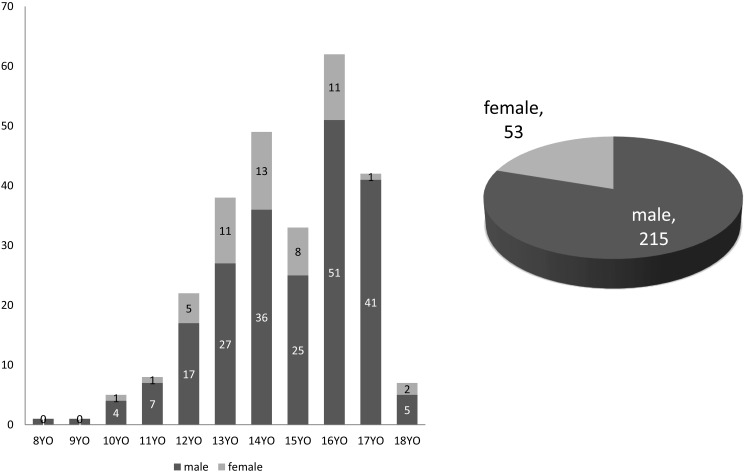
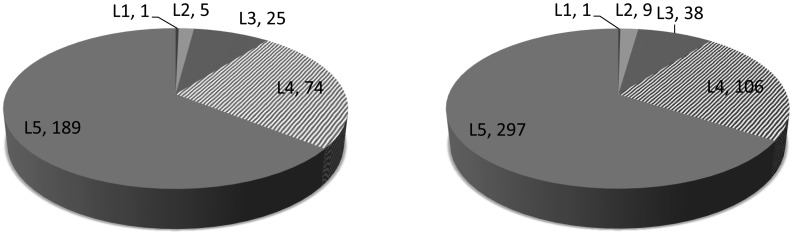
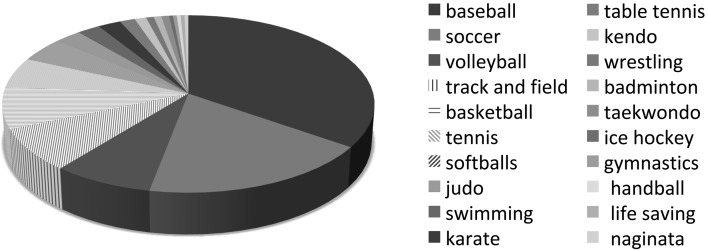
We examined 507 patients (360 boys; 147 girls) with low back pain. Of these patients, 268 (52.9%) were diagnosed with lumbar spondylolysis. Subjects were 8 to 18 years of age, with an average age of 14.7 years (Figure 3a). The sex ratio of subjects diagnosed with lumbar spondylolysis was 215 (80.2%) boys to 53 (19.8%) girls (Figure 3b). The proportion of spondylolysis among low back pain complainants was significantly higher in boys than in girls (p < 0.01). In 268 cases of lumbar spondylolysis, 451 lesions were confirmed. Among them, 157 laminae had bilateral lesions on both sides of one vertebra in the same patient, and 137 laminae had lesions on only one side. The number of lesions per vertebra was as follows: L1, 1 lesion in 1 case; L2, 9 lesions in 5 cases (4 patients had bilateral lesions); L3, 38 lesions in 25 cases (13 patients had bilateral lesions); L4, 106 lesions in 74 cases (32 patients had bilateral lesions); L5, 297 lesions in 189 cases (108 patients had bilateral lesions) (Figures 4a, b). Two hundred forty-four cases involved a single morbidity vertebral level, and 24 cases involved multiple vertebral levels in the same patient. Among these 24 patients, 22 had lesions on 2 vertebral levels, and 2 patients had lesions on 3 vertebral levels. SBO was confirmed in 111 cases. Two hundred sixty-four patients played a specific sport everyday: baseball, 93; soccer, 49; volleyball, 21; track and field, 21; basketball, 20; tennis, 15; softball, 12; judo, 7; swimming, 6; karate, 6; table tennis, 4; kendo, 3; wrestling, 2; badminton, 2; taekwondo, 2; ice hockey, 1; rhythmic gymnastics, 1; handball, 1; life-saving, 1; naginata exercise, 1 (Figure 5). Four patients did not participate in any daily sport.
Figure 3.
(a) Age distribution showing two peaks at 13 and 16 years of age. (b) Sex ratio showing male cases being four times more likely than female cases.
Figure 4.
Distribution by vertebral level: (a) number of cases and (b) number of lesions.
Figure 5.
Distribution by sport.
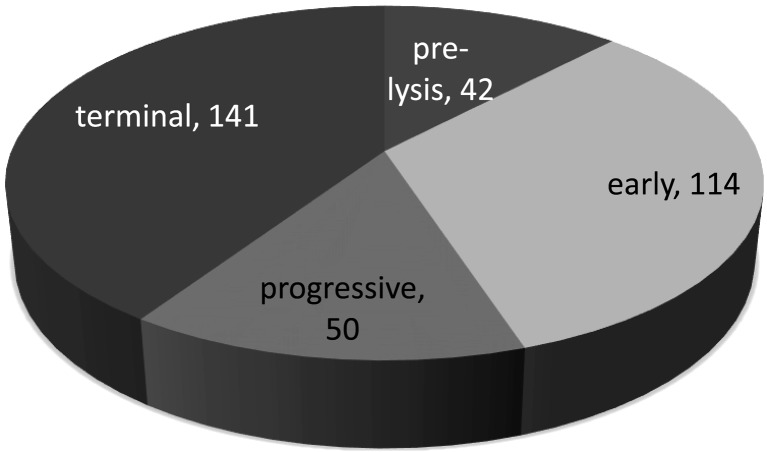
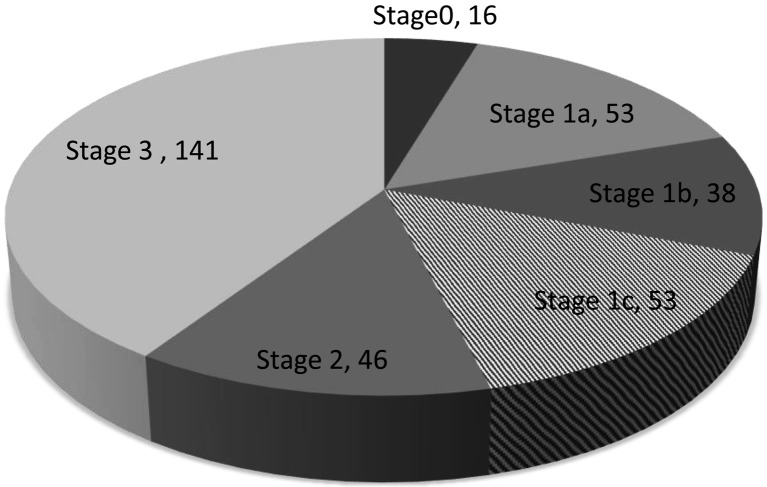
In 202 cases, 347 lesions were detected using CT staging. Based on axial slice classification, 42 lesions were of the pre-lysis stage, 114 lesions were in the early stage, 50 lesions were in the progressive stage, and 141 lesions were in the terminal stage (Figure 6). Based on sagittal slice classification, 16 lesions were in stage 0, 53 lesions were in stage 1a, 38 lesions were in stage 1b, 53 lesions were in stage 1c, 46 lesions were in stage 2, and 141 lesions were in stage 3 (Figure 7).
Figure 6.
Distribution based on axial slice classification.
Figure 7.
Distribution based on sagittal slice classification.
The prevalence of lesions within the curable stage, which includes pre-lysis, early, and progressive axial stages, and sagittal stages of 0, 1a, 1b, 1c, and 2, was 206 lesions in 142 cases. One hundred and forty-one lesions in 87 cases were found in the pseudoarthrosis-stage. Thirty-seven patients had both curable and pseudoarthrosis stages of spondylolysis.
Discussion
With MRI, detection of fresh lumbar spondylolysis based on bone marrow edema is possible, even in the absence of a fracture line. Therefore, with MRI, lumbar spondylolysis can be diagnosed at an earlier stage. The widespread use of MRI, allowing the lumbar spine to be more easily visualized, would increase the detection of spondylolysis with fresh fracture upon an initial hospital visit. Compared with previous studies, the proportion of pseudoarthrosis patients diagnosed at a first visit is considered to be decreasing. We believe that it is possible to reduce the number of pseudoarthrosis cases with early detection through both medical examination, and early MRI imaging. Spondylolysis in the pre-lysis stage has a high rate for curability with conservative therapy3).
In the 507 patients who presented with the primary complaint of low back pain, 268 (52.6%) patients had lumbar spondylolysis. Notably, 59.7% of male patients complaining of low back pain were diagnosed as having spondylolysis, while only 36.1% of females received the same diagnosis. If an adolescent male athlete visits the hospital with complaints of back pain, we should strongly suspect lumbar spondylolysis, whereas in female athletes, further medical examination is needed for differential diagnosis.
Sport discipline may affect the occurrence of spondylolysis. In the current investigation, the incidence of lumbar spondylolysis in professional baseball and soccer players was 44.1% and 38.1%, respectively. The frequency of diagnosis in the review by Sakai et al. was consistent with the results found in this study4).
In patients with pseudoarthrosis on the contralateral side, the fusion rate of freshly injured unilateral lumbar spondylolysis is very low5). Since bilateral lesions are biomechanically unstable, they have difficulty reaching union.
In this study, staging was done with axial and sagittal slices; however, the disease stage in these slices do not necessarily coincide. In six cases, the axial slice disease classification was judged to be more serious than the sagittal slice classification. According to another report6), sagittal CT image classification related to dynamic stability is useful for evaluation of bone union and treatment policy decision making. Hence, we believe that the combination of sagittal and axial slice observation would be beneficial to detect the fracture line in its early stages.
Conservative treatment of spondylolysis may lead to an unfavorable outcome in a case of spondylolysis with SBO7). The unequal distribution of stresses at the pars interarticularis is thought to interfere with fracture healing, and, as a result, altered spinal biomechanics cause the spine to be more unstable. In this study, 111 (41.4%) of 268 spondylolysis patients had SBO. In a previous report8), the incidence of spondylolysis with SBO was 16.2%, which is higher than that in subjects without SBO (5.0%). The reason for spondylolysis may therefore be connected with the presence of SBO.
Important factors that influence bone fusion are not well understood. Once a spondylotic fracture progresses to the terminal stage, it is impossible for athletes to obtain bony fusion with conservative therapy, and pseudoarthrosis will be permanent. The fusion rate of one-sided spondylolysis is higher than that of bilateral cases. Thus, it is important that we detect spondylolysis during its pre-lysis or early stages, before bilateral sides are affected. This study has a limitation: some patients were examined using only CT or MRI.
Conclusion
With 59.3% of patients having curable-stage lumbar spondylolysis, adolescent athletes experiencing low back pain are urged to seek consultation, and clinicians should perform MRI to avoid misdiagnosis.
Conflict of Interest
None.
Acknowledgment
The authors thank Atsuko Taya and Yoshiko Sakuma, medical clerks at the Mito Clinical Education and Training Center, University of Tsukuba Hospital, and Mito Kyodo General Hospital, for their contributions to data analysis.
References
- 1.Sairyo K, Sakai T, Yasui N. Conservative treatment of lumbar spondylolysis in childhood and adolescence: the radiological signs which predict healing. J Bone Joint Surg Br 2009; 91: 206–209. doi: 10.1302/0301-620X.91B2.21256 [DOI] [PubMed] [Google Scholar]
- 2.Oba S. Prevention of lumbar spondylolysis – for early consultation and diagnosis. Nihon Rinsho Sport Igakukaishi 2008; 16: 339–348(J Jpn Soc Clin Sports Med). [Google Scholar]
- 3.Gamada H, Tatsumura M, Shibao Y. Analysis of adolescent lumbar spondylolysis cases in pre-lysis stage. J Spine Res 2018; 9: 1436–1442(in Japanese, Abstract in English). [Google Scholar]
- 4.Sakai T, Sairyo K, Suzue N. Incidence and etiology of lumbar spondylolysis: review of the literature. J Orthop Sci 2010; 15: 281–288. doi: 10.1007/s00776-010-1454-4 [DOI] [PubMed] [Google Scholar]
- 5.Tatsumura M, Gamada H, Imoo Y. Fusion rate of fresh injured unilateral lumbar spondylolysis with pseudoarthrosis on contralateral side. Nihon Rinsho Sport Igakukaishi 2017; 25: 367–373(J Jpn Soc Clin Sports Med). [Google Scholar]
- 6.Kamiya M, Hanamura S, Wakao N. Usefulness of CT sagittal image in conservative treatment of lumbar spondylolysis in childhood and adolescence. J Spine Res 2015; 6: 176–179(in Japanese, Abstract in English). [Google Scholar]
- 7.Ishimoto R, Tatsumura M, Gamada H. The effect of posterior and/or lateral vertebral arch defects on conservative treatment of lumbar spondylolysis. Nihon Rinsho Sport Igakukaishi 2018; 26: 442–450(J Jpn Soc Clin Sports Med). [Google Scholar]
- 8.Sakai T, Sairyo K, Takao S. Incidence of lumbar spondylolysis in the general population in Japan based on multidetector computed tomography scans from two thousand subjects. Spine 2009; 34: 2346–2350. doi: 10.1097/BRS.0b013e3181b4abbe [DOI] [PubMed] [Google Scholar]