Abstract
The molecular pathogenesis of sporadic parathyroid adenomas is incompletely understood. The possible role of cyclin-dependent kinase inhibitor (CDKI) genes was raised by recognition of cyclin D1 as a parathyroid oncogene, identification of rare germline mutations in CDKI genes in patients with multiple endocrine neoplasia type 1; that in rodents, mutation in Cdkn1b caused parathyroid tumors; and subsequently through identification of rare predisposing germline sequence variants and somatic mutation of CDKN1B, encoding p27kip1, in sporadic human parathyroid adenoma. We therefore sought to determine whether mutations/variants in the other six CDKI genes CDKN1A, CDKN1C, CDKN2A, CDKN2B, CDKN2C, and CDKN2D, encoding p21, p57, p14ARF/p16, p15, p18, and p19, respectively, contribute to the development of typical parathyroid adenomas. In a series of 85 sporadic parathyroid adenomas, direct DNA sequencing identified alterations in five adenomas (6 %): Two contained distinct heterozygous changes in CDKN1A, one germline and one of undetermined germline status; one had a CDKN2B germline alteration, accompanied by loss of the normal allele in the tumor (LOH); two had variants of CDKN2C, one somatic and one germline with LOH. Abnormalities of three of the mutant proteins were readily demonstrable in vitro. Thus, germline mutations/rare variants in CDKN1A, CDKN2B, and CDKN2C likely contribute to the development of a significant subgroup of common sporadic parathyroid adenomas, and somatic mutation in CDKN2C further suggests a direct role for CDKI alteration in conferring a selective growth advantage to parathyroid cells, providing novel support for the concept that multiple CDKIs can play primary roles in human neoplasia.
Electronic supplementary material
The online version of this article (doi:10.1007/s12672-013-0147-9) contains supplementary material, which is available to authorized users.
Keywords: Primary Hyperparathyroidism, Multiple Endocrine Neoplasia Type, Parathyroid Adenoma, Missense Variant, Parathyroid Tumor
Primary hyperparathyroidism is a relatively common endocrine disorder, with a prevalence of 1–3/1,000 population (even higher in adults and especially postmenopausal women), and is most often caused by sporadic parathyroid adenomas. Three genes, MEN1, CCND1/cyclin D1, and CDKN1B, are established genetic drivers (by recurrent, intragenic mutation plus experimental induction of hyperparathyroidism) of sub-sets of sporadic parathyroid adenomas [1]. The most frequently involved among these, MEN1, is somatically inactivated by mutation in 12–20 % of sporadic adenomas [1] (and possibly up to 35 %, based on recent whole exome sequencing studies of a small cohort [2, 3]), so additional molecular insight into the genetic basis of these tumors is needed.
Peri-centromeric rearrangement of chromosome 11, which places the cyclin D1 coding exons under direct regulation of the parathyroid hormone (PTH) gene regulatory region, occurs in ∼8 % of parathyroid adenomas [4, 5], and cyclin D1 activation by this and other mechanisms has been observed in 20–40 % of adenomas. Cyclin D1, together with partner cyclin-dependent kinases (CDKs), regulates the G1 to S phase transition of the cell cycle, which raised the candidacy of CDK inhibitors (CDKIs) as potential parathyroid tumor genes. Evidence for CDKI involvement came initially from a rodent model in which mutation in the p27kip1 CDKI gene caused tumors in multiple endocrine tissues including parathyroid [6], and from the discovery of p27kip1 mutations [6, 7] and germline mutations in other CDKI genes [8] in patients with multiple endocrine neoplasia type 1 or related states. Subsequently, CDKN1B, encoding p27kip1, has been implicated in the pathogenesis of sporadic parathyroid adenomas through the identification of rare predisposing germline sequence variants and clonal, tumor-specific mutation [9], identified in ∼5 % of patients. Sporadic adenomas have not been extensively investigated for mutations in the other CDKI gene family members; CDKN2A, CDKN2B, and CDKN2C have been examined in a small series of cases with no mutations having been identified [10, 11]. More generally, evidence that CDKIs are authentic drivers in human tumorigenesis has been sparse, despite the appeal of their candidacy and efforts to mimic their actions therapeutically. We therefore sequenced the coding regions of all seven CDKI genes (excluding the previously analyzed CDKN1B) in a panel of 85 sporadic parathyroid adenomas.
Materials and Methods
Patients and Samples
Tumor samples were obtained from 85 patients who had undergone parathyroidectomy for the management of primary hyperparathyroidism with typical presentations, surgically and histopathologically proven to be caused by a single, sporadic parathyroid adenoma with no atypical and/or malignant features. No patient had a family history of primary hyperparathyroidism, a personal or family history suggestive of multiple endocrine neoplasias, or a personal history of head/ neck irradiation. All of the tumors included in this study had previously been analyzed for CDKN1B sequence variants [9]. Blood from the same patients was also obtained to serve as a source of matched germline DNA. All samples were obtained with informed consent in accordance with institutional review board-approved protocols. Genomic DNA was extracted by proteinase K digestion followed by phenol–chloroform extraction and ethanol precipitation.
PCR and DNA Sequence Analysis
All coding regions and intron–exon boundaries of CDKN1A, CDKN2A, CDKN2B, CDKN2C, and CDKN2D plus the non-variable portions of CDKN1C were polymerase chain reaction (PCR)-amplified in our series of 85 sporadic parathyroid adenomas; the 3′ portion of the first coding exon of CDKN1C contains highly variable PAPA (proline and alanine) repeats and was therefore not included in our analysis. PCR was performed in 20-ul reactions containing 25 ng of sample DNA, 20 pmol of each primer, 200 uM of dNTP, 2 mM magnesium chloride, and 1.25 U of Taq Gold DNA polymerase (Applied Biosystems). Thermal cycles began with a single denaturation step of 95 °C for 10 min; 35 cycles of 95 °C for 30 s, 55–58 °C for 1 min, and 72 °C for 30 s; and ended with a single extension step at 72 °C for 10 min. Exons with high G-C content (CDKN2D exon 1 and CDKN1C exon 3) were PCR-amplified using the Advantage-GC 2 PCR kit (Invitrogen) under conditions recommended by the manufacturer, using 1 M G-C Melt. Primers used for PCR and sequencing are listed in Supplementary Table 1. The PCR products were sequenced in both forward and reverse directions with the same primers used for PCR using standard Sanger sequencing methodology by GENEWIZ, Inc. Sequence data were analyzed using the Staden Package [12] and Sequencher (GeneCodes) software to align multiple tumor sample sequences along with reference sequences (UCSC hg19) and to visually scrutinize for possible variants in the tumor and control samples. Complete, high-quality sequence data for CDKN1A (encoding p21), CDKN2B (encoding p15), and CDKN2C (encoding p18) were obtained from all 85 samples; for CDKN2D (encoding p19) from 78 samples; for CDKN1C (encoding p57) from 81 samples; and for CDKN2A (encoding p14ARF and p16) from 67 samples. Even in the instances with less than complete sequence data (due to technical or sample quality issues), there was generally greater than 90 % base coverage. Variations from the reference sequence were confirmed by sequencing of an independently generated PCR product; non-tumor, control DNA from the same individual was also sequenced to determine if variants were germline or somatic. dbSNP build 137 was queried for the presence of identified variants in the general population. Loss of heterozygosity analyses were performed at using microsatellite markers D9S157, D9S171, D9S1853, D1S507, and D1S2664 in selected cases, as previously described [9, 13].
Cell Culture
HEK293 cells (ATCC) were grown in complete Dulbecco’s modified Eagle’s medium (DMEM supplemented with 2 μM glutamine, 10 % fetal calf serum, and 1× antibiotic–antimycotic) at 37 °C and 5 % CO2. Transient transfection was carried out with Lipofectamine 2000 (Invitrogen).
CDKI Expression Analysis
Missense sequence variations identified in patient samples were introduced in the respective pcDNA3.1 CDKI expression construct for p15, p18, or p21 [8] by site-directed mutagenesis (SDM) (Stratagene). Primers used for SDM are listed in Supplementary Table 2. HEK293 cells were transfected with pcDNA3.1 vector alone or with constructs of wild-type CDKI or missense variant of CDKI. Protein whole-cell lysates were prepared in 1× TBS with 0.1 % Igepal. Nuclear and cytoplasmic extract was prepared with the NEPER kit (Pierce).
Equal amounts of protein (50 μg) were analyzed by Western blot. Antibodies used were as follows: p15 (Cell Signaling, 4822), p18 (Santa Cruz, sc-1208), p21 (Santa Cruz, sc-6246), p84 (GeneTex, GTX70220), tubulin (Calbiochem, CP06), and NPT-II (Upstate, 06–747). Anti-tubulin and anti-p84 detected protein loading and cellular fractionation (tubulin is cytoplasmic, and p84 is nuclear). NPT-II protein is expressed from the mammalian expression vector pcDNA3.1, and therefore, anti-NPT-II antibody detected transfection efficiency.
GST Pull-Down Assays
GST or GST-fusion proteins (GST-CDK2 or GST-CDK6) were expressed and purified on glutathione sepharose beads (Amersham-Pharmacia) as described [8]. 35S-Methionine labeled in vitro translated (IVT) wild-type or missense mutant proteins were incubated in 1× PBS overnight at 4 °C with GST alone, or with GST-CDK2 or GST-CDK6 coupled to glutathione sepharose beads. Beads were washed thoroughly with 1× PBS, and the bound labeled IVT proteins were visualized by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) followed by autoradiography.
Statistical Analysis
Data were presented as mean ± SD from at least three independent experiments. Differences between groups were compared by unpaired Student’s t tests, and the differences were considered to be significant if p values were less than 0.05.
Results
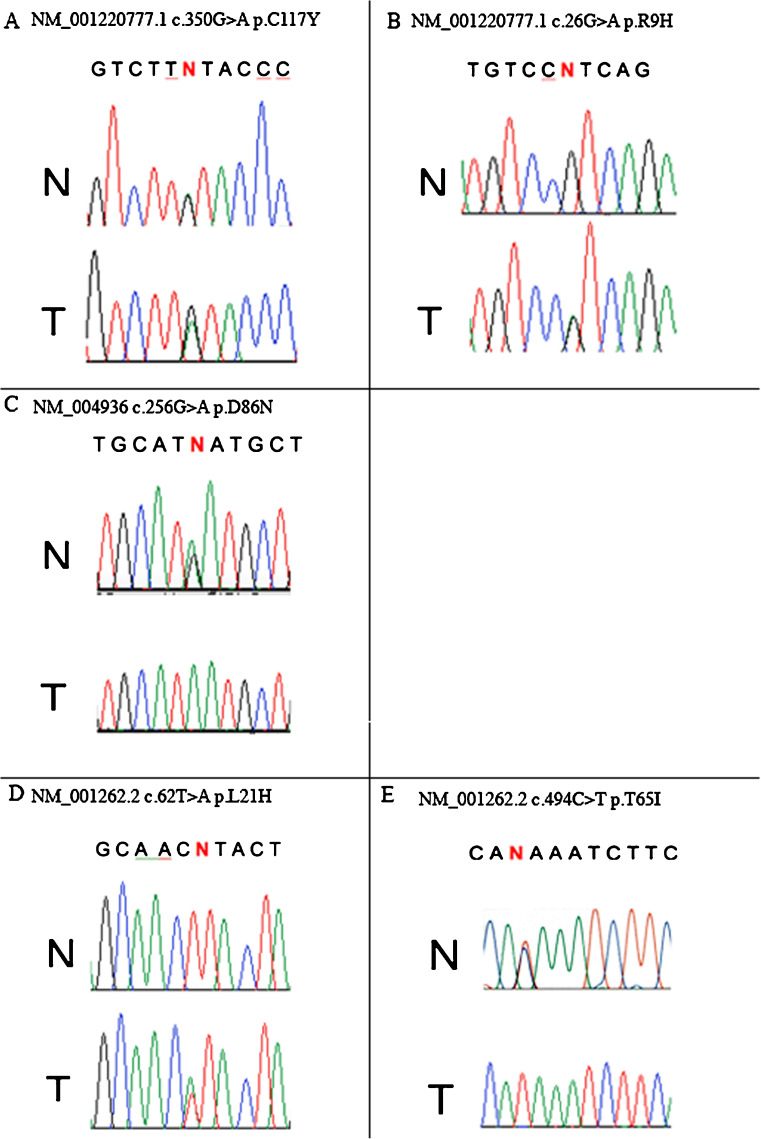
The coding regions of CDKN1A, CDKN1C, CDKN2A, CDKN2B, CDKN2C, and CDKN2D were examined by direct sequencing of genomic DNA from 85 parathyroid adenomas. Notably, while no mutations of potential pathogenic significance were identified in CDKN1C, CDKN2A, or CDKN2D, non-synonymous, intragenic point mutations in CDKN1A, CDKN2B, or CDKN2C were identified and confirmed in five tumors (5.9 %) (Table 1, Fig. 1).
Table 1.
Mutation summary
| Patient | Age | Gene | Protein | Nucleotide affected | Amino acid change | Somatic/germline | LOH | Evidence for pathogenicity |
|---|---|---|---|---|---|---|---|---|
| 1 | 82 | CDKN1A | p21 | c.350G > A | Cys117Tyr | Germline | No | genetic |
| 2 | 64 | CDKN1A | p21 | c.26G > A | Arg9His | ND | No | Cytoplasmic accumulation/abnormal migration and genetic |
| 3 | 69 | CDKN2B | p15 | c.256G > A | Asp86Asn | Germline | Yesa | Impaired CDK6 binding and genetic |
| 4 | 60 | CDKN2C | p18 | c.62 T > A | Leu21His | Somatic | No | Impaired CDK6 binding, abnormal migration and genetic |
| 5 | 53 | CDKN2C | p18 | c.494C > T | Thr165Ile | Germline | Yesb | genetic |
aLOH within and surrounding the CDKN2B gene was established using microsatellite markers D9S157, D9S171, and D9S1853 and direct DNA sequencing
bLOH within and surrounding the CDKN2C gene was established using microsatellite markers D1S507 and D1S2664, and direct DNA sequencing
Fig. 1.
CDKI sequence variants. a Mutation in CDKN1A, encoding p21. Germline and tumor sequences show heterozygosity [cytosine/thymine] at position 350 of the coding sequence. b Mutation in CDKN1A, encoding p21. Germline sequence shows guanine at position 26. The tumor shows acquired heterozygosity [guanine/adenine] at this position. c Mutation and LOH in CDKN2B encoding p15. Germline sequence (N) shows heterozygosity at position 256 of the coding sequence. In the tumor (T), the normal guanine is lost and the abnormal adenine remains. d Mutation in CDKN2C, encoding p18. Germline sequence shows a thymine at position 62 of the coding sequence. The tumor shows acquired heterozygosity [thymine/adenine] at this position. e Mutation and LOH in CDKN2C, encoding p18. Germline sequence shows heterozygosity at position 454 of the coding sequence. In the tumor, the normal cytosine is lost, and the abnormal thymine remains
Two tumors contained CDKN1A variants. The first was a heterozygous germline missense substitution c.350G > A, changing the encoded cysteine at position 117 of p21 to tyrosine (Cys117Tyr (NM_001220777.1 c.350G > A p.C117Y). This sequence variant has previously been described as a heterozygous change in a single oral squamous cell carcinoma [14] but not in any of the over 5,500 additional tumor samples in the COSMIC database [15] and has been detected only once in more than 4,000 alleles in the dbSNP database [16]. This patient, like all of the patients included in this study, had no family history of primary hyperparathyroidism, nor was DNA from family members available for examination. The second mutation was a heterozygous single-nucleotide change, c.26G > A, resulting in a substitution of histidine for arginine at position 9 (Arg9His) in the p21 protein (NM_001220777.1 c.26G > A p.R9H). Matched germline DNA from this individual was degraded, and therefore the presence of this variant in the germline could not be assessed. This base change has not been reported in the dbSNP database [16] or in any of the more than 5,500 tumors sequenced in the published literature [15, 17–19]. Interestingly, a slightly different, apparently heterozygous change at the same position in p21, changing Arg9 to cysteine, was reported in a single breast cancer sample [18].
CDKN2B alteration was found in one case. This was a germline, missense variant accompanied by loss of the normal allele in the tumor. The altered base resides in exon 2 and converts the encoded p15 residue from aspartic acid, which is highly conserved across species, into asparagine (NM_004936 c.256G > A p.D86N). This patient, like all of the patients included in this study, had no family history of primary hyperparathyroidism, nor was DNA from family members available for examination. This germline sequence variant has been reported only once in the published literature, in a patient with a metastatic pancreatic endocrine tumor [20], and not in any of the more than 5,600 tumor samples in the COSMIC database [15]. This change has been observed in 9 out of more than 4,000 alleles (0.2 %) in dbSNP build 137 [16].
CDKN2C variants were detected in two tumors. The first was a somatic, heterozygous missense mutation in exon 2 (first coding exon) that converts the encoded amino acid in p18 from the original leucine, which is highly conserved across species, to histidine (NM_001262.2 c.62 T > A p.L21H) and has not been observed in more than 6,600 sequenced tumors in the COSMIC database [15] or in dbSNP build 137. The second CDKN2C variant was a germline, missense alteration in exon 3, resulting in a substitution of isoleucine for the original threonine (NM_001262.2 c.494C > T p.T165I), accompanied by loss of the normal allele in the tumor. This patient, like all of the patients included in this study, had no family history of primary hyperparathyroidism, nor was DNA from family members available for examination. This base change has been reported in only one of over 4,000 alleles in dbSNP build 137 [16] and has not been observed in more than 6,600 sequenced tumors in the COSMIC database [15].
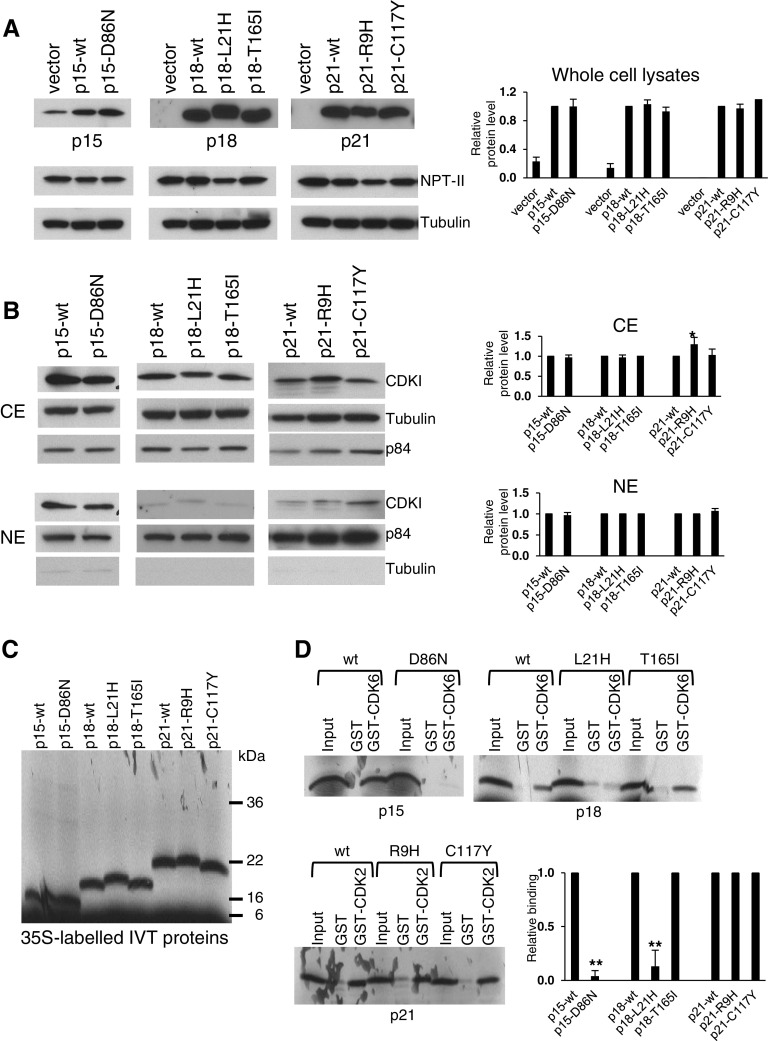
To investigate functional consequences of the detected CDKI variants, plasmid expression vectors were constructed. Expression of CDKI missense variants was analyzed in transiently transfected HEK293 cells. No abnormality in protein expression was detected for any of the missense variants (Fig. 2a). Protein bands corresponding to p18-L21H and p21-R9H migrated slower (Fig. 2a) compared with their respective wild-type protein, which suggests a change in protein charge or structure from the amino acid substitution affecting the migration rate of the mutant proteins. Protein level of p21-R9H was higher in the cytoplasm compared with wild-type p21 (Fig. 2b). Cytoplasmic accumulation of p21 has been shown to adversely affect its normal cell cycle inhibitory function in the nucleus [21, 22], and a previous study has established that p21 localization in normal parathyroid glands is exclusively nuclear [23]. GST pull-down assays were performed to determine the binding of wild-type or missense variants to prototypical cyclin-dependent kinases CDK2 or CDK6; due to insolubility of the GST-CDK4 fusion protein, CDK4 binding was not analyzed [8]. Notably, two variants (p15-D86N and p18-L21H) were impaired for binding to CDK6 (Fig. 2c). Thus, fully three of five variants were functionally impaired or showed other abnormal properties in at least one assay. It should be noted that additional functional impairments that might be parathyroid cell–context-specific would have been missed because of the unavailability of parathyroid cell lines to perform these assays.
Fig. 2.
Functional characterization of CDKI variants. a Protein expression in whole cell lysates of HEK293 cells transfected with wild type or mutagenized cDNA expression constructs. Top panel was probed with the indicated specific anti-CDKI antibody, middle panel with anti-NPTII antibody (to assess transfection efficiency), and lower panel with anti-tubulin antibody (to assess protein loading). Relative level of wild-type (wt) and mutant protein expression is shown (n = 3), with wt protein level = 1. b Protein level in nuclear and cytoplasmic extracts of HEK293 cells transfected with wild-type or mutagenized cDNA expression constructs. Top panels of cytoplasmic extract (CE), and bottom panels of nuclear extract (NE) were probed with the indicated specific anti-CDKI antibody, anti-tubulin (to assess protein loading in CE, and to assess the efficiency of sub-cellular fractionation in NE), or with anti-p84 (to assess protein loading in the NE, and to assess the efficiency of sub-cellular fractionation in the CE). Relative level of wt and mutant protein expression in CE and NE is shown (n = 3), with wt protein level = 1, *p = 0.04. c In vitro translated (IVT) proteins used for GST pull-down assay in 'D'. 35S-Methionine labeled wild-type or mutagenized proteins were generated by in vitro translation from cDNA expression constructs. IVT proteins were detected by SDS-PAGE and autoradiography. d Protein-binding to CDK2 or CDK6. GST pull-down assay for binding to GST, GST-CDK2, or GST-CDK6 of 35S-methionine labeled IVT wt or mutagenized proteins. The bound IVT protein was detected by SDS-PAGE and autoradiography. Input lane contained 10 % of the IVT product incubated with GST, GST-CDK2, or GST-CDK6. Relative binding of wt and mutant protein to GST-fusion proteins is shown with wt protein binding = 1 (n = 3 for p15 and p18; n = 2 for p21), **p < 0.001
Discussion
Rare abnormalities in several cyclin-dependent kinase inhibitor genes have been found in patients with multiple endocrine neoplasia type 1 and related hyperparathyroid states [8], and mutation in the p27kip1 CDKI is the pathogenetic basis for a rodent model of endocrine lesions including parathyroid neoplasia [6]. A subsequent investigation, focused on typically presenting sporadic parathyroid adenomas, identified rare predisposing germline variants and acquired clonal mutations in CDKN1B, encoding p27kip1 [9], but whether additional CDKI genes may be involved in sporadic hyperparathyroidism has not been extensively examined. The present study strikingly identified five abnormalities in three additional CDKI genes, CDKN1A, CDKN2B, and CDKN2C, in a series of 85 sporadic parathyroid adenomas. Among these five variants, three were germline missense mutations, one was a somatic missense mutation, and for one the somatic/germline status was indeterminate because of sample availability. Impaired functions of the expressed protein were readily demonstrated in vitro for three of the five mutations. These identified DNA abnormalities are highly likely to be of pathogenic importance because (a) they occur in genes previously implicated in familial hyperparathyroidism; (b) their prevalence in the literature and population databases is exceedingly rare or nil; (c) genetically engineered mice lacking p18 and p21 expression demonstrate an increased incidence of parathyroid tumor formation [24]; (d) the presence of a somatic mutation in at least one case demonstrates a significant selective advantage in the tumor; and (e) abnormal function/property of the expressed mutation-bearing protein was readily demonstrable for three of the mutations. Furthermore, these data give important support to the concept that CDKIs can play a central role in human neoplasia; though they do not appear to commonly function as classical tumor suppressor genes, indicated by their exceedingly low frequency of biallelic inactivation. Interestingly, with the exception of p16 in melanoma, mutational analyses of other tumor types have generally failed to provide validation of CDKIs’ role in human tumorigenesis, with mutation rates of 0.04 to 0.36 % [15]. It appears that endocrine cell types may provide a particularly vulnerable context in which mutations can effectively drive tumorigenesis, reflected by a 6.5- to 30-fold increase in the mutation rate.
The discovery of these new CDKI germline sequence abnormalities in patients with typically-presenting (in the sixth through ninth decades of life) solitary parathyroid adenomas, and without family histories of parathyroid or other endocrine disease, adds substantial weight to the concept that rare variants contribute to sporadic hyperparathyroidism as reduced-penetrance predisposition alleles. Remarkably, combined with previous observations on the role of CDKN1B in sporadic adenomas [9], approximately 10 % of this sporadic tumor panel harbors mutations or variants of likely pathogenic significance in this subset of four CDKI genes. Thus, such variants may make a larger contribution to hyperparathyroidism on the population level than do higher penetrance alleles (e.g., in MEN1, CASR, CDC73/HRPT2) found in the rare kindreds that are readily ascertained in clinical practice to have familial hyperparathyroidism. Interestingly, while the frequency of germline mutations of other familial hyperparathyroidism genes (MEN1, CASR, CDC73/HRPT2) was reported to be elevated in patients with sporadic hyperparathyroidism presenting at ages ≤45 years [25], none of the patients with germline CDKI gene variants in the present study were young, consistent with the reduced-penetrance concept. This support for the “rare variant, common disease” model of the genetic contribution to human disorders, as opposed to the “common variant, common disease” model, appears to parallel low-penetrance AIP mutations in pituitary adenoma predisposition [26]. Indeed, rare variants in the population may be more prevalent than previously assumed, as indicated by data released from recent large exome sequencing projects [27, 28]. As such, it is unsurprising that three of the five variants identified in this study are present in population sequence databases. Considering that their frequency in such databases is considerably lower than the frequency of primary hyperparathyroidism in the general population and that no information is available on the parathyroid disease status of individuals in these databases, the presence of these variants in population databases could indeed be representative of individuals with, or at risk of developing, primary hyperparathyroidism. To examine the potential role of CDKI genotyping in “personalized medicine,” i.e., individualized risk assessment or management, future study of penetrance and frequency of de novo mutations in extended families of probands ascertained with sporadic adenomas should be pursued.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOC 52 kb)
Acknowledgments
We wish to thank Ms. Kristin Corrado for expert technical assistance. This work was supported in part by grants DHHS/NIDCR 5 T32-DE07302 and 1 F32-DE021307 (to J.C.G.) from the National Institutes of Health; the Intramural Research Program of the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (SKA; Project number: 1ZIADK075035-03); and by the Murray-Heilig Fund in Molecular Medicine.
Disclosures
The authors disclose no potential conflicts of interest.
References
- 1.Costa-Guda J & Arnold A (2013) Hyperparathyroidism. In: Thakker RV, Whyte MP, Eisman JA, & Igarashi T (ed) Genetics of Bone Biology and Skeletal Disease. San Diego, CA, Academic Press, pp 397–408
- 2.Cromer MK, et al. Identification of somatic mutations in parathyroid tumors using whole-exome sequencing. J Clin Endocrinol Metab. 2012;97(9):E1774–E1781. doi: 10.1210/jc.2012-1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Newey PJ, et al. Whole-exome sequencing studies of nonhereditary (sporadic) parathyroid adenomas. J Clin Endocrinol Metab. 2012;97(10):E1995–E2005. doi: 10.1210/jc.2012-2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yi Y, Nowak NJ, Pacchia AL, Morrison C. Chromosome 11 genomic changes in parathyroid adenoma and hyperplasia: array CGH, FISH, and tissue microarrays. Genes Chromosomes Cancer. 2008;47(8):639–648. doi: 10.1002/gcc.20565. [DOI] [PubMed] [Google Scholar]
- 5.Westin G, Bjorklund P, Akerstrom G. Molecular genetics of parathyroid disease. World J Surg. 2009;33(11):2224–2233. doi: 10.1007/s00268-009-0022-6. [DOI] [PubMed] [Google Scholar]
- 6.Pellegata NS, et al. Germ-line mutations in p27Kip1 cause a multiple endocrine neoplasia syndrome in rats and humans. Proc Natl Acad Sci U S A. 2006;103(42):15558–15563. doi: 10.1073/pnas.0603877103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Georgitsi M, et al. Germline CDKN1B/p27Kip1 mutation in multiple endocrine neoplasia. J Clin Endocrinol Metab. 2007;92(8):3321–3325. doi: 10.1210/jc.2006-2843. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal SK, Mateo CM, Marx SJ. Rare germline mutations in cyclin-dependent kinase inhibitor genes in multiple endocrine neoplasia type 1 and related states. J Clin Endocrinol Metab. 2009;94(5):1826–1834. doi: 10.1210/jc.2008-2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Costa-Guda J, Marinoni I, Molatore S, Pellegata NS, Arnold A. Somatic mutation and germline sequence abnormalities in CDKN1B, encoding p27Kip1, in sporadic parathyroid adenomas. J Clin Endocrinol Metab. 2011;96(4):E701–E706. doi: 10.1210/jc.2010-1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tahara H, Smith AP, Gaz RD, Arnold A. Loss of chromosome arm 9p DNA and analysis of the p16 and p15 cyclin-dependent kinase inhibitor genes in human parathyroid adenomas. J Clin Endocrinol Metab. 1996;81(10):3663–3667. doi: 10.1210/jc.81.10.3663. [DOI] [PubMed] [Google Scholar]
- 11.Tahara H, et al. Parathyroid tumor suppressor on 1p: analysis of the p18 cyclin-dependent kinase inhibitor gene as a candidate. J Bone Miner Res. 1997;12(9):1330–1334. doi: 10.1359/jbmr.1997.12.9.1330. [DOI] [PubMed] [Google Scholar]
- 12.Staden R. The Staden sequence analysis package. Mol Biotechnol. 1996;5(3):233–241. doi: 10.1007/BF02900361. [DOI] [PubMed] [Google Scholar]
- 13.Shattuck TM, et al. Mutational analysis of Smad3, a candidate tumor suppressor implicated in TGF-beta and menin pathways, in parathyroid adenomas and enteropancreatic endocrine tumors. J Clin Endocrinol Metab. 2002;87(8):3911–3914. doi: 10.1210/jc.87.8.3911. [DOI] [PubMed] [Google Scholar]
- 14.Ibrahim SO, Lillehaug JR, Vasstrand EN. Mutations of the cell cycle regulatory genes p16INK4A and p21WAF1 and the metastasis-inducing gene S100A4 are infrequent and unrelated to p53 tumour suppressor gene status and data on survival in oropharyngeal squamous cell carcinomas. Anticancer Res. 2003;23(6C):4593–4600. [PubMed] [Google Scholar]
- 15.Forbes SA, et al. COSMIC: mining complete cancer genomes in the Catalogue of Somatic Mutations in Cancer. Nucleic Acids Res. 2011;39(Database issue):D945–950. doi: 10.1093/nar/gkq929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sherry ST, et al. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. 2001;29(1):308–311. doi: 10.1093/nar/29.1.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shiohara M, et al. Absence of WAF1 mutations in a variety of human malignancies. Blood. 1994;84(11):3781–3784. [PubMed] [Google Scholar]
- 18.McKenzie KE, et al. Altered WAF1 genes do not play a role in abnormal cell cycle regulation in breast cancers lacking p53 mutations. Clin Cancer Res. 1997;3(9):1669–1673. [PubMed] [Google Scholar]
- 19.Staalesen V, Leirvaag B, Lillehaug JR, Lonning PE. Genetic and epigenetic changes in p21 and p21B do not correlate with resistance to doxorubicin or mitomycin and 5-fluorouracil in locally advanced breast cancer. Clin Cancer Res. 2004;10(10):3438–3443. doi: 10.1158/1078-0432.CCR-03-0796. [DOI] [PubMed] [Google Scholar]
- 20.Lindberg D, Akerstrom G, Westin G. Evaluation of CDKN2C/p18, CDKN1B/p27 and CDKN2B/p15 mRNA expression, and CpG methylation status in sporadic and MEN1-associated pancreatic endocrine tumours. Clin Endocrinol (Oxf) 2008;68(2):271–277. doi: 10.1111/j.1365-2265.2007.03034.x. [DOI] [PubMed] [Google Scholar]
- 21.Blagosklonny MV. Are p27 and p21 cytoplasmic oncoproteins? Cell Cycle. 2002;1(6):391–393. doi: 10.4161/cc.1.6.262. [DOI] [PubMed] [Google Scholar]
- 22.Sherr CJ, Roberts JM. CDK inhibitors: positive and negative regulators of G1-phase progression. Genes Dev. 1999;13(12):1501–1512. doi: 10.1101/gad.13.12.1501. [DOI] [PubMed] [Google Scholar]
- 23.Tokumoto M, et al. Parathyroid cell growth in patients with advanced secondary hyperparathyroidism: vitamin D receptor and cyclin-dependent kinase inhibitors, p21 and p27. Nephrol Dial Transplant. 2003;18(3):iii9–iii12. doi: 10.1093/ndt/gfg1003. [DOI] [PubMed] [Google Scholar]
- 24.Franklin DS, Godfrey VL, O'Brien DA, Deng C, Xiong Y. Functional collaboration between different cyclin-dependent kinase inhibitors suppresses tumor growth with distinct tissue specificity. Mol Cell Biol. 2000;20(16):6147–6158. doi: 10.1128/MCB.20.16.6147-6158.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Starker LF, et al. Frequent germ-line mutations of the MEN1, CASR, and HRPT2/CDC73 genes in young patients with clinically non-familial primary hyperparathyroidism. Hormones & Cancer. 2012;3(1–2):44–51. doi: 10.1007/s12672-011-0100-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vierimaa O, et al. Pituitary adenoma predisposition caused by germline mutations in the AIP gene. Science. 2006;312(5777):1228–1230. doi: 10.1126/science.1126100. [DOI] [PubMed] [Google Scholar]
- 27.Kiezun A, et al. Exome sequencing and the genetic basis of complex traits. Nat Genet. 2012;44(6):623–630. doi: 10.1038/ng.2303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keinan A, Clark AG. Recent explosive human population growth has resulted in an excess of rare genetic variants. Science. 2012;336(6082):740–743. doi: 10.1126/science.1217283. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC 52 kb)