Abstract
Background
Basic fibroblast growth factor (bFGF) regulates maintenance of stemness and modulation of osteo/odontogenic differentiation and mineralization in stem cells from human exfoliated deciduous teeth (SHEDs). Mineralization in the bones and teeth is in part controlled by pericellular levels of inorganic phosphate (Pi), a component of hydroxyapatite, and inorganic pyrophosphate (PPi), an inhibitor of mineralization. The progressive ankylosis protein (gene ANKH; protein ANKH) and ectonucleotide pyrophosphatase phosphodiesterase 1 (ENPP1/ENPP1) increase PPi and inhibit mineralization, while tissue-nonspecific alkaline phosphatase (ALPL; TNAP) is a critical pro-mineralization enzyme that hydrolyzes PPi. We hypothesized that regulation by bFGF of mineralization in SHEDs occurs by modulation of Pi/PPi-associated genes.
Methods
Cells were isolated from human exfoliated deciduous teeth and characterized for mesenchymal stem cell characteristics. Cells were treated with bFGF, and the osteogenic differentiation ability was determined. The mRNA expression was evaluated using real-time polymerase chain reaction. The mineralization was examined using alizarin red S staining.
Results
Cells isolated from primary teeth expressed mesenchymal stem cell markers, CD44, CD90, and CD105, and were able to differentiate into osteo/odontogenic and adipogenic lineages. Addition of 10 ng/ml bFGF to SHEDs during in vitro osteo/odontogenic differentiation decreased ALPL mRNA expression and ALP enzyme activity, increased ANKH mRNA, and decreased both Pi/PPi ratio and mineral deposition. Effects of bFGF on ALPL and ANKH expression were detected within 24 h. Addition of 20 mM fibroblast growth factor receptor (FGFR) inhibitor SU5402 revealed the necessity of FGFR-mediated signaling, and inclusion of 1 μg/ml cyclohexamide (CHX) implicated the necessity of protein synthesis for effects on ALPL and ANKH. Addition of exogenous 10 μm PPi inhibited mineralization and increased ANKH, collagen type 1a1 (COL1A1), and osteopontin (SPP1) mRNA, while addition of exogenous Pi increased mineralization and osterix (OSX), ANKH, SPP1, and dentin matrix protein 1 (DMP1) mRNA. The effects of PPi and Pi on mineralization could be replicated by short-term 3- and 7-day treatments, suggesting signaling effects in addition to physicochemical regulation of mineral deposition.
Conclusion
This study reveals for the first time the effects of bFGF on Pi/PPi regulators in SHEDs and implicates these factors in how bFGF directs osteo/odontogenic differentiation and mineralization by these cells.
Electronic supplementary material
The online version of this article (10.1186/s13287-018-1093-9) contains supplementary material, which is available to authorized users.
Keywords: Basic fibroblast growth factor, Stem cells isolated from human exfoliated deciduous teeth, Phosphate, Pyrophosphate
Background
Basic fibroblast growth factor (bFGF; also known as FGF2) is a member of the fibroblast growth factor family of related signaling molecules crucial for development, maintenance, and repair of tissues. While it regulates various cell processes including proliferation, migration, and differentiation, bFGF also controls maintenance of stemness in human stem cells [1, 2]. In this regard, bFGF preserves the undifferentiated state of human pluripotent stem cells [3]. Downregulation of OCT3/4 is observed in human embryonic stem cells treated with fibroblast growth factor receptor (FGFR) inhibitor, suggesting a role for bFGF in regulation of genes governing pluripotency [4]. Hence, bFGF is employed as one of the key components in growth medium for human embryonic stem cells and human induced pluripotent stem cells.
Stem cells isolated from human exfoliated deciduous teeth (SHEDs) were reported in 2003 [5]. The appeal of these postnatal mesenchymal stem cells (MSCs) is that they can be obtained non-invasively (isolated after natural exfoliation of primary teeth) and show the multipotent ability to differentiate into osteogenic, adipogenic, and neurogenic lineages [6]. Although they are considered to be MSCs based on known developmental processes, SHEDs exhibit novel characteristics compared with bone marrow-derived MSCs, possibly due in part to their origin from cranial neural crest-derived ectomesenchyme and/or different patterns of signaling that occur in the craniofacial-dental region compared to the postcranial skeleton [5].
Functions of bFGF have been established in regulating some aspects of SHED biology. As it does for embryonic stem cells, addition of bFGF to culture medium maintains stemness in SHEDs in long-term culture [7]. In this context, bFGF enhances colony-forming unit (CFU) ability and the expression of pluripotent markers (e.g., OCT4, REX1, and NANOG) [7], but does not influence cell proliferation [7, 8]. bFGF plays a potent role in regulating the differentiation of SHEDs into an odontoblast-like phenotype. Previous reports demonstrate that bFGF attenuates tissue-nonspecific alkaline phosphatase (gene: ALPL; protein: TNAP) expression and mineral deposition by SHEDs and dental pulp stem cells (DPSCs), in vitro [1, 9]. bFGF inhibits RUNX2 and BGLAP mRNA expression as well as mineral deposition by SHEDs in vitro via the regulation of ERK and Wnt signaling [8]. In addition, bFGF treatment of SHEDs leads to the reduction of ectopic bone formation in vivo [8]. Further, inhibition of endogeneous bFGF function using a chemical inhibitor of fibroblast growth factor receptor (FGFR) leads to increased mineralization upon osteogenic induction [6]. Correspondingly, SHEDs transfected with shRNA against bFGF exhibit higher mineral deposition than controls [6]. All of this accumulated evidence strongly supports a negative influence of bFGF on differentiation of SHEDs into mature, mineralizing odontoblast-like cells.
Inorganic phosphate (Pi) and pyrophosphate (PPi) play crucial roles in physiological and pathological extracellular matrix (ECM) mineralization. Pi is a primary component of hydroxyapatite crystals that are deposited in the biomineralization of the bone and teeth, while PPi is a potent inhibitor of crystal precipitation and growth [10]. In addition to their physicochemical roles in mineralization, both Pi and PPi have been reported to have signaling effects on cells, though mechanisms remain incompletely understood. The addition of Pi promoted mineralization in rat osteoblasts [11]. Conversely, PPi supplementation resulted in reduction of mineral deposition in vitro with reduced cell proliferation and collagen synthesis in murine cementoblasts [12]. Local pericellular Pi and PPi concentrations are regulated by TNAP, ectonucleotide pyrophosphatase/phosphodiesterase-1 (ENPP1;ENPP1), and the progressive ankylosis protein (ANKH; ANKH in humans and Ank/ANK in mice) [10]. TNAP cleaves extracellular PPi into Pi, facilitating ECM mineralization. ENPP1 increases extracellular PPi by cleaving nucleotide triphosphates, while ANKH regulates transport of intracellular PPi to the extracellular space. Functions of ANKH and ENPP1 result in increased extracellular PPi and subsequently inhibit mineralization. Studies on human loss-of-function mutations and genetically engineered mouse models have demonstrated that TNAP, ENPP1, and ANKH/ANK have profound effects on skeletal and dental mineralization [12–18].
To date, little is known about how bFGF affects expression of Pi/PPi regulators. Studies using MC3T3.E1 murine pre-osteoblasts showed that bFGF upregulates Enpp1 and Ank mRNA expression, while Alpl mRNA levels are downregulated [19]. Another report demonstrated that bFGF inhibits ALPL expression in SHEDs [9]. However, an influence of bFGF on the other key Pi/PPi regulatory genes in SHEDs has not yet been investigated, making it unclear how these genes contribute to bFGF regulation of osteo/odontoblast differentiation and mineralization. In the present study, we aimed to investigate in SHEDs the effect of bFGF on Pi and PPi regulatory genes and roles of Pi and PPi on mineralization of SHEDs.
Methods
Cell isolation and culture
The study was approved by Human Research Ethics Committee, Faculty of Dentistry, Chulalongkorn University (Approval number 2015-007). The procedure was performed according to the Declaration of Helsinki. Informed consent was obtained from parents. Primary teeth with no pathological lesions scheduled for extraction according to the clinical treatment plan were collected and stored in culture medium. Dental pulp tissues were obtained, and an explantation protocol was applied for cell isolation, using 35-mm tissue culture plate [2, 6]. The migrated cells were subcultured when cell confluence was achieved. Cells were cultured in Dulbecco’s modified Eagle medium (DMEM, Gibco, USA) supplemented with 10% fetal bovine serum (Gibco, USA), 2 mM l-glutamine (Gibco, USA), 100 U/mL penicillin (Gibco, USA), 100 μg/mL streptomycin (Gibco, USA), and 5 μg/mL amphotericin B (Gibco, USA). Cells were maintained in 100% humidity at 37 °C and 5% carbon dioxide.
In experiments described below, cells were treated with the following reagents: 10 ng/ml recombinant human bFGF (Invitrogen, USA), 20 mM FGFR inhibitor (SU5402; Calbiochem, USA), 5 mM sodium phosphate (Na2HPO4; Sigma-Aldrich, USA), 10 uM sodium pyrophosphate tetrabasic (Na4O7P2; Sigma-Aldrich, USA), and 1 μg/ml cyclohexamide (CHX; Sigma-Aldrich, USA). ALP was generously provided by Assistant Professor Jeerus Sucharitakul (Faculty of Dentistry, Chulalongkorn University, Thailand).
Flow cytometry
Single cell suspensions were obtained by detaching cells with trypsin/EDTA solution. Cells were centrifuged, and the supernatant culture medium was discarded. Cells were rinsed with 1% FBS in PBS and further immunostained with primary antibodies conjugated to fluorescent dye, including anti-human CD44 (BD Bioscience Pharmingen, USA), PerCP-CyTM5.5-conjugated anti-human CD90 (BD Bioscience Pharmingen, USA), PE-conjugated anti-human CD105 (BD Bioscience Pharmingen, USA), and PerCP-conjugated anti-CD45 (BD Bioscience Pharmingen, USA). Cells were analyzed using a FACSCalibur flow cytometer using CellQuest software for operation and gating (BD Bioscience, USA).
Osteo/odontogenic induction
Cells were seeded in 24-well plates at a density of 50,000 cells per well. After 24 h, culture medium was replaced with osteogenic induction medium consisting of growth medium supplemented with 252.39 μM L(+)-ascorbic acid sodium salt, 10 mM β-glycerophosphate, and 100 nM dexamethasone. The medium was changed every 48 h. Mineral deposition was analyzed using alizarin red S staining, as described below. Osteogenic marker gene expression was determined using quantitative real-time polymerase chain reaction, as described below. To test involvement of FGF signaling, in some experiments, SHEDs were pretreated with an FGFR inhibitor (SU5402) 30 min prior to bFGF exposure and cells were maintained in osteogenic induction medium supplemented with bFGF and SU5402 for the length of the experiment.
Adipogenic induction
Cells were seeded in 24-well plates at a density of 12,500 cells per well. Adipogenic induction medium consisted of growth medium supplemented with 0.1 mg/mL insulin, 1 mM dexamethasone, 1 mM isobutylmethylxanthine (IBMX), and 0.2 mM indomethacin. The medium was changed every 72 h. Oil Red O staining was performed to evaluate intracellular lipid accumulation according to a previously published protocol [2].
Alkaline phosphatase activity (ALP) assay
Cells were lysed in an alkaline lysis buffer. The samples were then incubated with p-nitrophenol phosphate solution (2 mg/mL, Invitrogen, USA). After 15 min, the reaction was stopped by the addition of 50 mM NaOH. The absorbance was measured at 410 nm. Total protein was evaluated using a bicinchoninic acid (BCA) assay (Thermo Scientific, USA). ALP activity was calculated and normalized to the amount of total protein.
Alizarin red S staining
Alizarin red S staining was employed to determine calcium deposition in culture [20]. Cells were fixed with cold methanol for 10 min and washed with deionized water. Subsequently, cells were incubated with 1% alizarin red S solution for 3 min at room temperature under gentle agitation. Cells were then washed with deionized water to remove excess staining. Precipitated dye was solubilized in 10% w/v cetylpyridinium chloride solution, and the absorbance was measured at 570 nm.
Quantitative polymerase chain reaction (QPCR)
RNA isolation was performed using RiboEx total RNA isolation solution (GeneAll, Seoul, South Korea). Complimentary DNA (cDNA) was synthesized from RNA using reverse transcriptase ImPromII kit (Promega, Madison, WI, USA). QPCR was performed using FastStart Essential DNA Green Master kit (Roche Diagnostic, USA) on the MiniOpticon real-time PCR system (Bio-Rad, USA). Target gene expression values were normalized to 18S expression values and further normalized to controls. Oligonucleotide sequences are listed in Additional file 1: Table S1.
Phosphate and pyrophosphate assay
After osteo/odontogenic differentiation, the culture medium was collected and analyzed using the EnzChek® Phosphate assay kit (Molecular PROBES, Oregon, USA) for quantitative analysis of Pi and the EnzChek® Pyrophosphate assay kit (Molecular PROBES, Oregon, USA) for detecting free PPi following the manufacturer’s protocol. Absorbance was measured at 360 nm.
Statistical analyses
Each experiment was performed using cells from at least four different donors. The Mann-Whitney U test was employed for comparisons of two groups. For comparison of three or more groups, the Kruskal-Wallis test was performed, followed by pairwise comparison with type I error correction. All statistical analyses were performed using Prism 7 (GraphPad Software, CA, USA). Statistical significance was indicated by p < 0.05.
Results
SHED cell isolation and characterization
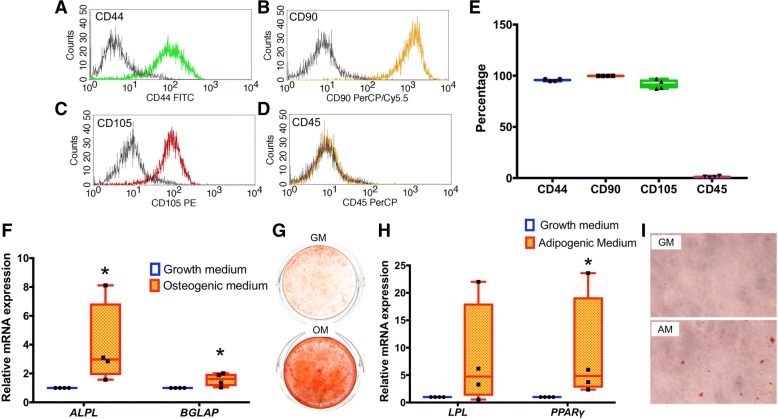
Cells were harvested from pulp chambers of the extracted primary teeth. Expression of mesenchymal and hematopoietic stem cell surface markers was evaluated using flow cytometry. Consistent with expectations for SHEDs, the isolated cells expressed MSC markers, CD44, CD90, and CD105 (Fig. 1a–c), but lacked expression of hematopoietic stem cell marker, CD45 (Fig. 1d). The percentage of cells expressing CD44, CD90, and CD105 was over 95%, 99%, and 92%, respectively (Fig. 1e). In contrast, only 1% were CD45-expressing cells. Significant upregulation of ALPL and bone γ-carboxyglutamate protein (BGLAP) mRNA expression was observed after osteo/odontogenic induction for 7 days (Fig. 1f), and after 14 days, a marked increase of mineral deposition was evident (Fig. 1g). Upregulation of adipogenic markers, lipoprotein lipase (LPL) and peroxisome proliferator-activated receptor γ (PPARγ), was observed after adipogenic induction for 8 days (Fig. 1h), and intracellular lipid accumulation was subsequently observed after 16 days (Fig. 1i). This combined evidence of MSC markers and multipotent differentiation ability confirms the MSC-like characteristics of the isolated SHED cells.
Fig. 1.
SHED cell isolation and characterization. Cells harvested from primary teeth were analyzed by flow cytometry and found to express MSC markers, a CD44, b CD90, and c CD105, but lack expression of hematopoietic stem cell marker, d CD45. e MSC markers are expressed in more than 90% of cells, with CD45 expressed in only about 1% of cells. f Significant upregulation of ALPL and BGLAP mRNA expression is observed after osteogenic induction of SHED cells for 7 days. g Increased mineral deposition by SHED cells under osteogenic induction is evident after 14 days. h Upregulation of LPL and PPARγ is observed after adipogenic induction of SHED cells for 8 days. i Intracellular lipid accumulation is observed after adipogenic induction for 16 days. GM growth medium, OM osteogenic induction medium, AM adipogenic induction medium. Asterisks indicated the statistically significant difference compared to the control (p < 0.05)
bFGF inhibits in vitro mineralization and alters osteo/odontogenic gene expression in SHEDs
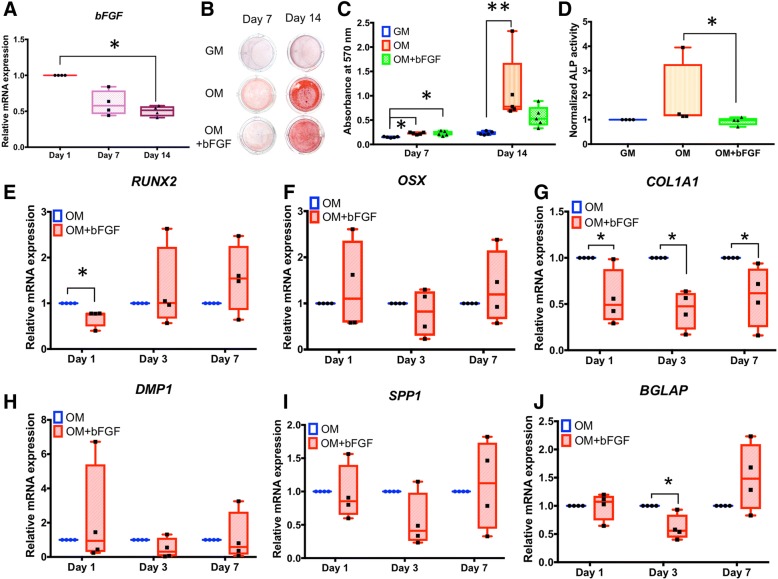
During osteo/odontogenic induction over 14 days, bFGF mRNA levels were reduced in a time-dependent manner until they were decreased by about 50% (p < 0.05) (Fig. 2a). Addition of 10 ng/mL bFGF to odontogenic induction medium led to the significant attenuation of mineral deposition at 14 days (p < 0.01) (Fig. 2b, c). This observation correlated with reduced ALP enzymatic activity in the bFGF-treated group after osteo/odontogenic induction for 7 days (Fig. 2d). Based on effects of bFGF on in vitro mineralization and ALP, we further investigated effects on genes associated with osteo/odontogenic differentiation and mineralization (Fig. 2e–j). bFGF treatment reduced mRNA expression of transcription factor, Runt-related transcription factor 2 (RUNX2), on day 1 (40%; p < 0.05), but did not affect OSX expression (Fig. 2e, f). bFGF decreased COL1A1 mRNA (by 40–50%; p < 0.05) on all days (Fig. 2g) and BGLAP (by 40%; p < 0.05) on day 3 (Fig. 2h), but did not affect expression of SPP1 or DMP1 (Fig. 2i, j).
Fig. 2.
bFGF inhibits in vitro mineralization and alters osteogenic/odontogenic gene expression in SHEDs. a Expression of bFGF is reduced 50% (p < 0.05) in SHED cells during osteogenic induction over 14 days. Inclusion of 10 ng/mL bFGF in osteogenic induction medium significantly attenuates mineral deposition at 14 days (b, c) and reduces ALP enzymatic activity at 7 days (d). e–j Addition of bFGF reduces mRNA expression of RUNX2 (day 1), COL1A1 (days 1, 3, and 7), and BGLAP (day 3) (p < 0.05 for all), but does not significantly affect expression of OSX, SPP1, or DMP1. The Mann-Whitney U test was employed for comparisons of two groups. The Kruskal-Wallis test followed by pairwise comparison was used for comparison of three groups. Bars indicated the statistically significant difference (*p < 0.05, **p < 0.01). GM growth medium, OM osteogenic induction medium
bFGF alters expression of phosphate/pyrophosphate regulatory genes in SHEDs
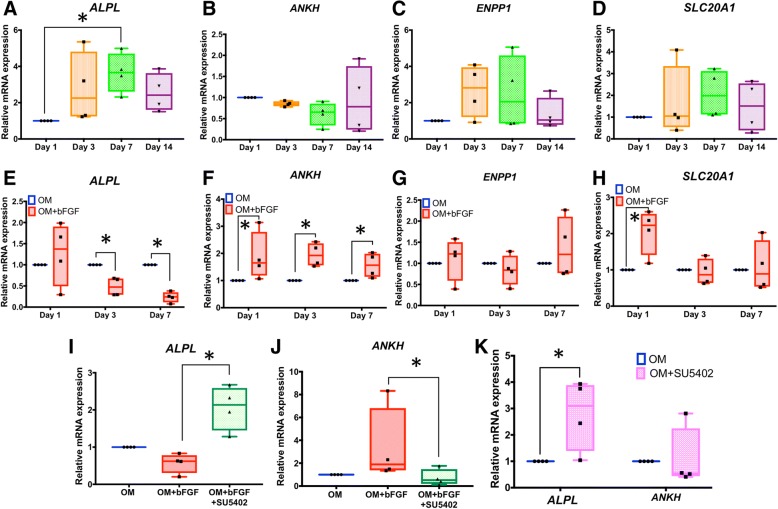
Experiments above confirmed bFGF regulates mineralization, ALP, and osteo/odontogenic genes in SHEDs. We next sought to determine if bFGF regulates expression of Pi/PPi regulatory genes, including ALPL, ANKH, ENPP1, and the sodium-Pi transporter, solute carrier family 20 member 1 (SLC20A1), during osteo/odontogenic differentiation in SHEDs. Examination of mRNA levels over 14 days of osteo/odontogenic differentiation demonstrated that ALPL was upregulated at day 7 (3-fold; p < 0.05) (Fig. 3a), while expression of ANKH tended towards decrease and ENPP1 and SLC20A1 tended towards increase, though these changes were not significant within the parameters of these experiments (Fig. 3b–d).
Fig. 3.
bFGF alters expression of phosphate/pyrophosphate regulatory genes in SHEDs. a SHED cells cultured in osteogenic medium over 14 days increase ALPL mRNA (day 7; p < 0.05), with no significant alterations in b ANKH, c ENPP1, or d SLC20A1 expression. Inclusion of 10 ng/mL bFGF in osteogenic induction medium e reduces ALPL mRNA (days 3 and 7), f increases ANKH mRNA (days 1, 3, and 7), g does not significantly affect ENPP1 mRNA, and h increases SLC20A1 mRNA (day 1). Addition of 20 mM FGFR inhibitor (SU5402) inhibits bFGF-induced changes in i ALPL and j ANKH on day 7. k Addition of 20 mM SU5402 in the absence of exogenous bFGF increases ALPL (p < 0.05) but does not affect ANKH expression. The Mann-Whitney U test was employed for comparison of two groups. The Kruskal-Wallis test followed by pairwise comparison was used for comparison of three or more groups. Bars indicated the statistically significant difference. OM osteogenic induction medium (*p < 0.05)
The influence of bFGF on Pi/PPi regulatory gene expression was determined in osteogenic induction medium. bFGF treatment significantly inhibited ALPL mRNA expression on days 3 and 7 after (by 50% or more; p < 0.05) (Fig. 3e). Significant upregulation of ANKH mRNA was observed on all days (between 50 and 100% increased; p < 0.05) (Fig. 3f). bFGF did not alter ENPP1 expression during osteo/odontogenic induction (Fig. 3g) and induced SLC20A1 mRNA (more than 100%; p < 0.05) on day 1 but not on later days (Fig. 3h).
SHEDs were pretreated with an FGFR inhibitor (SU5402) to confirm the involvement of bFGF signaling in modulation of ALPL and ANKH mRNA. SU5402 supplementation attenuated the influence of bFGF on both ALPL and ANKH mRNA expression, blocking the inhibitory effect of bFGF on ALPL (Fig. 3i) and preventing induction of ANKH upregulation (Fig. 3j). Inhibition of endogenous bFGF function by addition of SU5402 to osteogenic medium (in the absence of exogenous bFGF addition) resulted in a significant increase of ALPL expression at 7 days (3-fold; p < 0.050), but no significant regulation of ANKH mRNA levels (Fig. 3k).
In time course experiments, cells were supplemented with bFGF and maintained in growth medium with expression assayed at 6, 12, and 24 h. bFGF inhibition of ALPL mRNA began between 12 and 24 h (about 70% decrease; p < 0.05) (Fig. 4a). In contrast, the induction of ANKH mRNA by bFGF was observed at 6, 12, and 24 h (approximately 50–75% increase; p < 0.05) (Fig. 4b). Inclusion of FGFR inhibitor, SU5402, in growth medium for 24 h effectively abolished effects of bFGF on ALPL and ANKH expression (Fig. 4c, d). Inclusion of cycloheximide (CHX) in the media over 24 h also abolished effects of bFGF, strongly suggesting that protein translation is required as an intermediate step for the effects of bFGF on ALPL and ANKH (Fig. 4c, d).
Fig. 4.
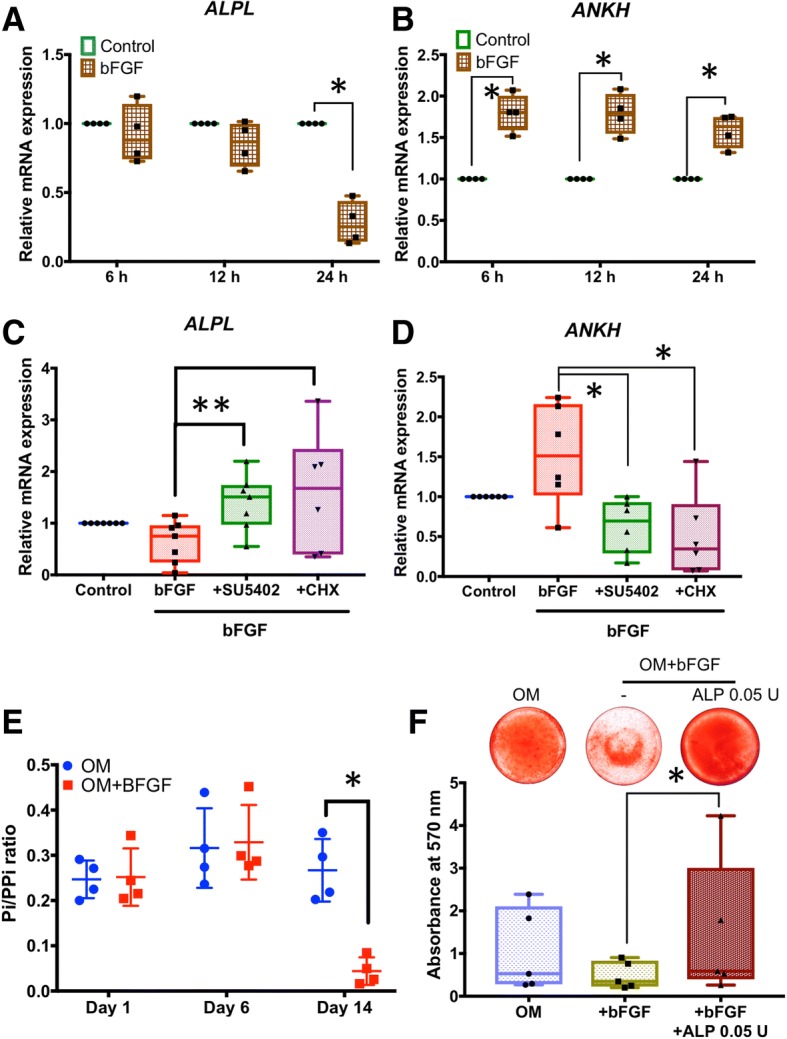
Regulation of ALPL and ANKH expression by bFGF in SHEDs. Cells were maintained in normal growth medium in the presence or absence of 10 ng/mL bFGF for 6, 12, or 24 h. a Addition of bFGF significantly inhibits ALPL mRNA by 24 h. b The induction of ANKH mRNA by bFGF is observed at 6, 12, and 24 h. c, d For both ALPL and ANKH, inclusion of 20 mM FGFR inhibitor (SU5402) in growth medium abolishes effects of bFGF at 24 h. Addition of 1 μg/ml cyclohexamide (CHX) inhibits effects of bFGF on ALPL and ANKH expression, suggesting that protein translation is required. e In culture medium collected from SHEDs on days 1, 6, and 14 after osteogenic induction, bFGF significantly reduces Pi/PPi ratio by day 14. f Addition of 0.05 U ALP rescues bFGF-attenuated ALP expression and mineral deposition in SHEDs. The Mann-Whitney U test was employed for comparisons of two groups. The Kruskal-Wallis test followed by pairwise comparison was used for comparisons of three or more groups. Bars indicate statistically significant differences (*p < 0.05, **p < 0.01). OM osteogenic induction medium
Culture medium collected on days 1, 6, and 14 after osteo/odontogenic induction revealed bFGF significantly reduced Pi/PPi ratio by day 14 (by about 80%; p < 0.05) (Fig. 4e), confirming a functional effect from reduced ALPL and increased ANKH expression. Addition of 0.05 U ALP rescued bFGF-attenuated mineral deposition (Fig. 4f).
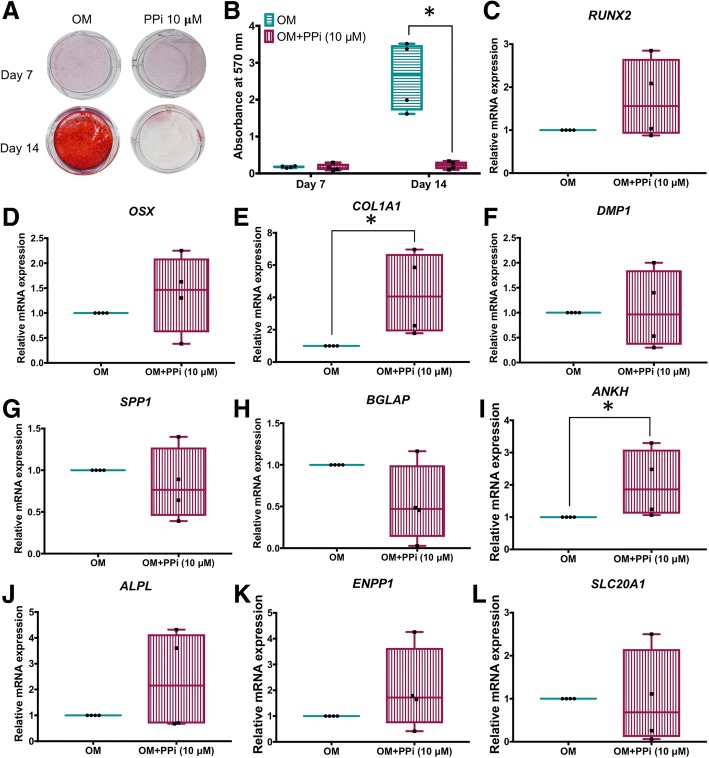
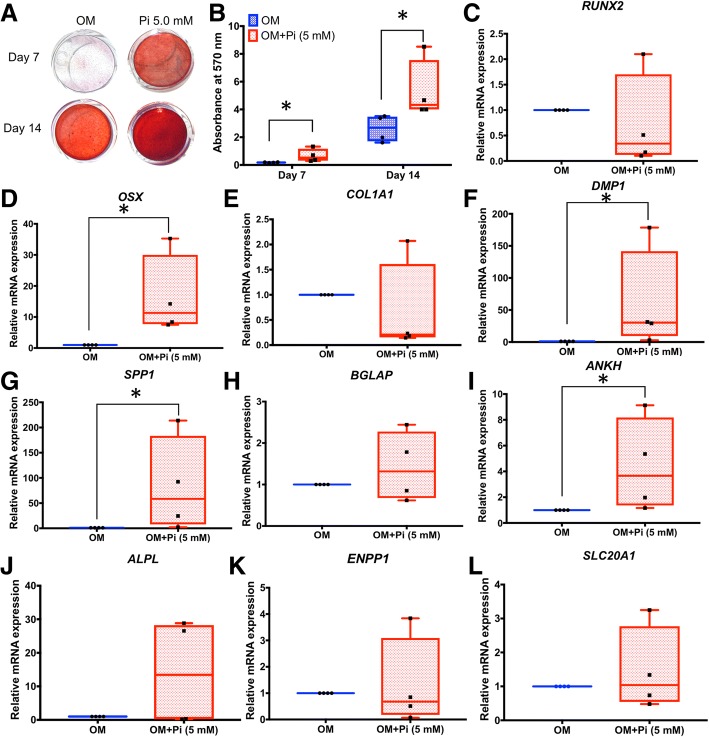
Inorganic phosphate and pyrophosphate regulate mineralization by SHEDs
Effects of exogenous PPi on osteoblast and cementoblast mineralization in vitro have been reported [12, 21]; however, to our knowledge, PPi has not been tested on stem cells, or more specifically on SHEDs. Addition of 10 μM PPi to osteogenic induction medium of SHEDs nearly completely inhibited mineral deposition by 14 days (Fig. 5a, b). At 7 days, inclusion of PPi increased COL1A1 (4-fold; p < 0.05) and ANKH (about 2-fold; p < 0.05), but did not significantly affect a number of other genes associated with mineralization and Pi/PPi regulation, compared to untreated controls (Fig. 5c–l).
Fig. 5.
PPi regulates mineralization and gene expression in SHEDs. a, b Addition of 10 μM PPi to osteogenic induction medium of SHED cells nearly completely inhibits mineral deposition by 14 days. c–l At 7 days, inclusion of PPi increases COL1A1 (p < 0.05) and ANKH (p < 0.05), but does not significantly affect other genes associated with mineralization and Pi/PPi regulation, compared to untreated controls. The Mann-Whitney U test was employed for comparisons of two groups, and bars indicated the statistically significant difference (*p < 0.05). OM osteogenic induction medium
Effects of exogenous Pi on osteoblast, cementoblast, and odontoblast mineralization and expression in vitro have been extensively studied [22–25], and experiments investigating effects of Pi on various types of stem cells have been reported [26, 27]. However, to our knowledge, this relationship has not been explored in SHEDs or other dental stem cells. Addition of 5 mM Pi to osteogenic medium significantly increased mineral deposition by SHEDs at both days 7 and 14 (about 3- and 2-fold, respectively; p < 0.05 for both) (Fig. 6a, b). At 7 days, inclusion of Pi significantly induced OSX (10-fold), DMP1 (25-fold), SPP1 (50-fold), and ANKH (4-fold) mRNA (p < 0.05 for all); however, other genes were unaffected (Fig. 6c–l).
Fig. 6.
Pi regulates mineralization and gene expression in SHEDs. a, b Addition of 5 mM Pi to osteogenic induction medium of SHED cells increases mineral deposition at 7 and 14 days. c–l At 7 days, inclusion of Pi increases OSX, DMP1, SPP1, and ANKH (p < 0.05 for all), but does not significantly affect other genes associated with mineralization and Pi/PPi regulation, compared to untreated controls. The Mann-Whitney U test was employed for comparisons of two groups, and bars indicated the statistically significant difference (*p < 0.05). OM osteogenic induction medium
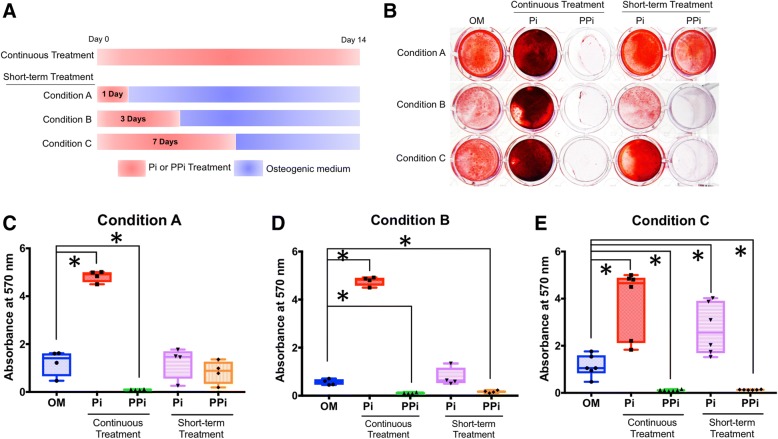
From the above experiments, it was not clear whether Pi or PPi was acting early or late to influence cell mineralization in the 14-day experiment. Therefore, the effect of duration of Pi or PPi treatment was investigated. Continuous administration of 5 mM Pi or 10 μM PPi in osteogenic medium served as the positive control, no added Pi or PPi served as negative control, and conditions A, B, and C incorporated shorter-term Pi or PPi treatments of 1, 3, or 7 days, respectively, followed by completion of the experiment in osteogenic medium (Fig. 7a). Continuous treatment of SHEDs with Pi or PPi resulted in significantly increased (nearly 3-fold; p < 0.05) or decreased (20-fold; p < 0.05) mineral deposition, respectively (Fig. 7b–e). Cells under condition A showed no significant difference in mineralization (Fig. 7b). Cells under condition B exhibited PPi-mediated inhibition of mineralization by 3 days (Fig. 7c). Lastly, cells under condition C showed increased mineralization from Pi treatment (more than 2-fold; p < 0.05), while those receiving PPi treatment significantly reduced mineral deposition (Fig. 7d). These results within the first 7 days suggest that the supplementation of exogenous Pi and PPi not only influences the precipitation and growth of mineral crystals, but may also affect intracellular mechanism(s).
Fig. 7.
Regulation of mineralization in SHEDs by continuous and short-term Pi and PPi treatment. a Cells were treated with 5 mM Pi or 10 μM PPi in osteogenic medium, with no Pi or PPi serving as negative control, and continuous administration of Pi or PPi serving as the positive control, whereas conditions A, B, and C incorporated shorter-term Pi or PPi treatments of 1, 3, or 7 days, respectively, followed by completion of the experiment in osteogenic medium. b Continuous treatment of SHEDs with Pi significantly increases (p < 0.05) mineral deposition while or continuous PPi significantly decreases (p < 0.05) mineral deposition. c Cells under condition A show no significant differences in mineralization from negative controls. d Cells under condition B exhibit PPi-mediated inhibition of mineralization by 3 days (p < 0.05). e Cells under condition C show increased mineralization from Pi treatment (p < 0.05) and decreased mineralization from PPi treatment (p < 0.05). The Mann-Whitney U test was employed for comparisons of three or more groups, and bars indicated the statistically significant difference (*p < 0.05). OM osteogenic induction medium
Discussion
For the first time, we report effects of bFGF on regulation of Pi/PPi and mineralization in SHEDs. Addition of bFGF to SHEDs during in vitro osteo/odontogenic differentiation decreased ALPL mRNA expression and ALP enzyme activity, increased ANKH mRNA, and decreased Pi/PPi ratio and mineral deposition. Effects of bFGF on ALPL and ANKH mRNA expression were detected within 24 h and required FGFR signaling and protein synthesis. Addition of exogenous PPi inhibited mineralization and increased ANKH, COL1A1, and SPP1 mRNA, while addition of exogenous Pi increased mineralization and increased OSX, ANKH, SPP1, and DMP1 mRNA. These effects of PPi and Pi on mineralization could be replicated by short-term 3- and 7-day treatments, suggesting early signaling effects in addition to physical-chemical modulation of mineral deposition. This study reveals the effects of bFGF on Pi/PPi regulators in SHEDs and implicates these factors in how bFGF directs osteo/odontogenic differentiation and mineralization by these cells.
Regulation by bFGF of osteo/odontogenic markers and mineralization in SHED cells
Previous studies demonstrated that bFGF inhibited mineralization in SHEDs and DPSCs [1, 9]. Here, we confirmed this effect of bFGF on mineralization in SHEDs and extended understanding of the underlying mechanisms by examining the influence of bFGF on other osteo/odontogenic markers and Pi/PPi regulators. Type 1 collagen, encoded by COL1A1 and COL1A2 genes, composes 90% of the extracellular matrix (ECM) of the bone, dentin, and cementum. bFGF significantly inhibited COL1A1 expression during osteo/odontogenic differentiation on days 1, 3, and 7. It has been shown that bFGF suppresses COL1 and COL3 while enhancing mRNA expression of matrix metalloproteinases MMP1 and MMP2 in human periodontal ligament (PDL) cells, suggesting a catabolic influence of bFGF on ECM regulation [28]. Similarly, collagen synthesis was reduced by bFGF treatment in rat hair dermal papilla cells [29]. Hence, the bFGF-induced reduction of COL1A1 expression could be beneficial in terms of scar formation during wound healing. On the contrary, in rabbit chondrocytes, bFGF did not influence COL1A1 mRNA levels but suppressed COL2 mRNA expression [30]. Tenocytes overexpressing bFGF increased COL1 and COL3 expression.
We demonstrated that bFGF inhibits RUNX2 and BGLAP mRNA expression on days 1 and 3, respectively. RUNX2 serves a master transcription factor regulating osteo/odontogenic differentiation and function, upstream of numerous key genes [31, 32]. BGLAP encodes OCN, an extracellular matrix protein found in the bone, dentin, and cementum and posited to regulate mineralization as well as perform wider endocrine functions [33, 34]. Previous publications implicated bFGF inhibition of osteo/odontogenic differentiation of SHEDs in part via reduction of RUNX2 and BGLAP mRNA [8]. Similarly, studies on stem cells from apical papilla (SCAP) showed that bFGF treatment during osteo/odontogenic induction decreased BGLAP mRNA levels at early but not late time points [35]. In PDL cells, bFGF inhibited mineralization when added to osteogenic medium, but with no apparent regulation of RUNX2 or BGLAP expression, suggesting alternative mechanisms [36]. However, bFGF induced RUNX2 expression in human periodontal ligament cells which are maintained in growth medium [36]. In mouse osteoblasts, bFGF attenuated RUNX2-induced Alpl expression [37]. The influence of bFGF on RUNX2 and OCN at specific time points during osteo/odontogenic induction of SHEDs and other cells requires further investigation.
These collected data concerning effects of bFGF on COL1A1, RUNX2, and BGLAP suggest cell-type-specific responses to bFGF. The reduction of all three of these osteo/odontogenic markers concomitant with decreased mineral deposition supports a link to attenuation of mineralization; however, additional studies are warranted to explore these relationships further.
Effect of bFGF on Pi and PPi regulators in SHED cells
During osteo/odontogenic differentiation, SHEDs upregulated ALPL expression early, while ANKH, ENPP1, and SLC20A1 mRNA levels were not markedly changed during the differentiation period assayed here. Alpl was induced early in OCCM.30 murine cementoblasts, and Ank, Enpp1, Spp1, and Dmp1 mRNA increased at later times after mineral deposition [38]. In MC3T3.E1 murine pre-osteoblasts, bFGF induced Enpp1 and Ank but inhibited Alpl mRNA expression [19]. In MLO-Y4 murine osteocyte-like cells, bFGF upregulated Ank, Enpp1, Slc20a1, and Dmp1 [39]. Conversely, we showed here that bFGF suppressed ALPL but induced ANKH expression in SHEDs, while ENPP1 expression was not markedly changed by exposure to bFGF. These changes were blocked by addition of an FGFR inhibitor, confirming the requirement of FGF signaling. In addition, the effect of bFGF on ALPL and ANKH expression was attenuated by protein synthesis inhibitor, suggesting the involvement of intermediate factors in the regulation process. Ultimately, the consequence of bFGF-reduced ALPL and increased ANKH in SHEDs was borne out by significantly decreased Pi/PPi ratio, an alteration that likely contributed to reduced mineralization in vitro and would be anticipated to have a potent effect to inhibit ECM mineralization.
Based on inhibition of mineralization and changes in Pi/PPi regulatory genes in response to bFGF, we explored direct effects of exogenous PPi or Pi on SHEDs during osteo/odontogenic differentiation. Addition of exogenous PPi inhibited mineralization and significantly upregulated COL1A1 and ANKH expression in SHEDs. In OCCM.30 cementoblasts, 10–100 μM PPi decreased mineral deposition, and removal of PPi from culture medium during early stages allowed mineral deposition to proceed as normal, suggesting a primarily physicochemical effect on mineral deposition by these cells [12]. In contrast, a dose of 2.5 μM PPi increased Alpl and Ank and decreased Enpp1 in MC3T3.E1 pre-osteoblasts, implicating direct signaling effects [21]. We documented that withdrawal of PPi from medium after 1 day allowed SHEDs to mineralize similar to untreated controls; however, PPi withdrawal after days 3 or 7 did not reverse the inhibitory effect of PPi on mineralization. Because SHEDs largely mineralize between 7 and 14 days in osteogenic medium, these results suggest that PPi not only inhibits mineral precipitation and growth, but may also regulate cells through additional signaling mechanisms, a hypothesis that requires further investigation. In Alpl knockout (Alpl−/−) mice, a model for the hereditary error-in-metabolism, hypophosphatasia (HPP), loss of TNAP function increases PPi and prevents mineralization in the bones and teeth. Severely hypomineralized dentin in Alpl−/− mice was accompanied by loss of expression of Bglap and dentin sialophosphoprotein (Dspp) mRNA by odontoblasts [40], supporting a connection between PPi, mineralization, and altered expression in skeletal/dental cells in vivo.
Addition of 5 mM Pi significantly increased OSX, DMP1, SPP1, and ANKH mRNA in SHEDs. Pi is well established as a potent signal in osteoblasts, cementoblasts, and odontoblasts [22–25, 41]. Spp1/OPN was first identified as a target for Pi signaling in MC3T3.E1 murine pre-osteoblasts, where extracellular signal-regulated kinases (ERK) 1/2 and protein kinase C (PKC) pathways were implicated in its transcription [25, 41]. Subsequently, Pi was found to regulate numerous genes in osteoblasts [41–43]. In OCCM.30 cementoblasts, Pi also induced Spp1/OPN, possibly through a glucocorticoid receptor in the promoter region [22, 44]. OPN is a multifunctional ECM protein involved in cell migration, attachment, differentiation, and also a negative regulator of mineralization proposed to be involved in pathological hypomineralization of dentin in diseases such as HPP and X-linked hypophosphatemia (XLH) [40, 45–47]. Genetic ablation of OPN in Spp1−/− mice resulted in increased mineral content in the bones, increased cortical and trabecular bone parameters in femurs and tibias, and increased dentin and alveolar bone [48–50]. Interestingly, Spp1−/− mice featured defective reparative dentin formation, suggesting the protein is necessary for pulpo-dentinal healing [51].
DMP1 is an ECM protein closely related to OPN that is expressed by odontoblasts, osteoblasts, and osteocytes. Pi induction of Dmp1/DMP1 was previously documented in OCCM.30 murine cementoblasts and human PDL fibroblasts [12, 52]. DMP1 is critical for dentin formation and periodontal development. Dmp knockout (Dmp1−/−) mice exhibit a dentinogenesis imperfecta-like phenotype including thin and hypomineralized dentin and an enlarged pulp cavity in the molars [53]. Additionally, loss-of-function of DMP1 is responsible for autosomal recessive hypophosphatemic rickets, an endocrine disorder marked by low circulating Pi and severe hypomineralization of the bones and teeth [54].
OSX is a transcription factor directing osteoblast and odontoblast differentiation [55, 56]. The upregulation of OSX in SHEDs by Pi observed in the present study paralleled Pi induced Osx expression in rat kidney fibroblast and human vascular smooth muscle cells [57, 58]. In those cells, Pi induced upregulation of Osx occurred via Akt1 and ERK signaling [57].
Addition of Pi to SHEDs increased expression of ANKH mRNA. Induction of Ank was also achieved by addition of 5 mM Pi to OCCM.30 murine cementoblast cells, hypothesized to be a response to pro-mineralization conditions and a sort of negative feedback to compensate the overabundance of extracellular Pi and to balance Pi/PPi ratio, and regulate the pace of mineralization [22]. Loss of function of Ank/ANKH leads to decreased PPi and increased and sometimes ectopic mineralization, and Ank mutant or knockout mice feature skeletal differences and massively increased acellular cementum [12, 14, 17, 59]. These potent effects of ANK/ANKH on mineralized tissue development in vivo justify further investigation of the interactions of bFGF, ANKH, PPi, and mineralization in SHEDs.
Influence of local Pi and PPi regulation on tooth development and regeneration
Pi and PPi participate in tooth development and regeneration. Their roles were demonstrated by the investigation in knockout and mutated mouse models. Alpl mutation, resulting in increased local PPi concentrations, causes delayed tooth eruption, aplasia or hypoplasia of cementum, and defective insertion of Sharpey’s fibers [10, 60]. Conversely, mice lacking Ank or Enpp1 function exhibited hypercementosis with otherwise normal dental and periodontal structure [10, 61]. These data strongly support the significant role of local Pi/PPi ratio via regulation by TNAP, ANK/ANKH, and ENPP1, in directing tooth development and structural formation.
Besides the role of Pi/PPi in tooth development, modulation of this ratio has also been proposed as an alternative approach for regenerative treatment. TNAP immobilized fibrin scaffolds enhanced Pi concentration and osteogenic differentiation in vitro as well as increased calvarial bone regeneration in vivo [62]. Local delivery of polyphosphate led to the increase alveolar bone regeneration around rat molars [63]. Studies of Ank knockout mice demonstrated that decreased PPi promoted more rapid and greater cementum regeneration in a periodontal defect model compared to wild-type mice [64], implying a role for Pi/PPi regulation in periodontal tissue regeneration. However, more work must indeed be done to understand the mechanism(s) and to develop treatment strategies in translational and clinical settings.
Benefit of bFGF in future clinical applications
The present study aimed to investigate regulatory mechanisms whereby bFGF affected SHED differentiation and mineralization. We concluded that continuous bFGF treatment of SHEDs inhibited mineral deposition, in part via regulation of genes controlling Pi/PPi metabolism. However, several reports demonstrated that bFGF pretreatment before osteogenic induction promoted osteogenic potential of various human stem/progenitor cells [65]. Our findings parallel those of Fakhry and colleagues, which indicated that continuous treatment of calvarial osteoblasts with bFGF inhibited osteogenic gene expression and mineralization, while short-term treatment of bFGF stimulated osteogenic differentiation [66]. Moreover, previous publications reported the beneficial utilization of bFGF in hard tissue formation through various approaches. Local application of bFGF enhanced dental implant stability and osseointegration in animal models [67, 68]. In addition, bFGF has been utilized in alveolar bone and periodontal tissue regeneration, i.e., periodontal defect treatment and alveolar ridge preservation [69, 70]. The anabolic effect of bFGF in vivo could result from the brief exposure of local cells to the released proteins, prompting osteogenic differentiation. In addition, bFGF regulates angiogenesis, cell migration, and cell proliferation [71, 72]. Hence, these processes could help to facilitate the healing and formation of hard tissue in vivo.
Another potential use of bFGF in clinical regenerative therapy would be to maintain stemness of stem and progenitor populations in vitro. It has been shown that mesenchymal stem cells isolated from dental tissues lose their stem cell properties and decline in proliferation during long-term culture in vitro [7]. Our previous reports revealed that continuous bFGF treatment in vitro promoted maintenance of stemness in dental tissue-derived mesenchymal stem cells [1, 2, 7]. The bFGF supplementation in long-term culture of SHEDs enhanced colony-forming unit ability and stem cell marker gene expression [7]. Hence, bFGF could be useful to amplify cell number while maintaining stem cell properties in vitro for future regenerative application of SHEDs.
Conclusions
This study reveals the effects of bFGF on osteogenic differentiation ability of SHEDs. In addition, it has been demonstrated that bFGF influences Pi/PPi regulators in SHEDs and implicates these factors in how bFGF directs osteo/odontogenic differentiation and mineralization by these cells.
Additional file
Table S1. Primer sequences for QPCR. (DOCX 18 kb)
Acknowledgements
Authors thank to the Oral Biology Research Center for providing the research facilities. We appreciate the assistance from the Department of Pediatric Dentistry for sample collection.
Funding
This study was supported by the Chulalongkorn Academic Advancement Into Its 2nd Century Project. TO is supported by Thailand Research Fund (RSA6180019). NN is supported by the Ratchadapisek Sompote Fund for Postdoctoral Fellowship, Chulalongkorn University.
Availability of data and materials
Please contact the corresponding author for data requests.
Abbreviations
- Akt
Serine/threonine-specific protein kinase
- ALP
Alkaline phosphatase
- ALPL
Tissue-nonspecific alkaline phosphatase
- ANKH
Progressive ankylosis protein
- BCA
Bicinchoninic acid
- bFGF
Basic fibroblast growth factor
- BGLAP
Bone γ-carboxyglutamate protein
- CD105
Cluster of differentiation 105
- CD44
Cluster of differentiation 44
- CD45
Cluster of differentiation 45
- CD90
Cluster of differentiation 90
- cDNA
Complimentary DNA
- CHX
Cycloheximide
- COL1
Collagen type 1
- COL12
Collagen type 2
- COL1A1
Collagen type 1a1
- COL1A2
Collagen type 1a2
- COL3
Collagen type 3
- DMP1
Dentin matrix protein 1
- DPSCs
Dental pulp stem cells
- Dspp
Dentin sialophosphoprotein
- ECM
Extracellular matrix
- ENPP1
Ectonucleotide pyrophosphatase phosphodiesterase 1
- ERK
Extracellular signal-regulated kinases
- FGFR
Fibroblast growth factor receptor
- HPP
Hypophosphatasia
- IBMX
Isobutylmethylxanthine
- LPL
Lipoprotein lipase
- MMP
Matrix metalloproteinases
- MSCs
Mesenchymal stem cells
- NANOG
Nanog homeobox
- NaOH
Sodium hydroxide
- OCCM.30
Murine cementoblast cell line
- OCN
Osteocalcin
- OCT4
POU class 5 homeobox 1
- OPN
Osteopontin
- OSX
Osterix
- PDL
Periodontal ligament
- Pi
Inorganic phosphate
- PKC
Protein kinase C
- PPARγ
Peroxisome proliferator-activated receptor γ
- PPi
Inorganic pyrophosphate
- REX1
ZFP42 zinc finger protein
- RUNX2
Runt-related transcription factor 2
- SCAP
Stem cells from apical papilla
- SHEDs
Stem cells isolated from human exfoliated deciduous teeth
- SLC20A1
Solute carrier family 20 member 1
- SPP1
Secreted phosphoprotein 1
- SU5402
FGFR inhibitor
- TNAP
Tissue-nonspecific alkaline phosphatase
- XLH
X-linked hypophosphatemia
Authors’ contributions
NN contributed to the experimental design, data acquisition and analysis, and critical manuscript revision. WS contributed to the cell isolation from deciduous teeth, data interpretation, and critical manuscript revision. PP contributed to the data interpretation and critical manuscript revision. BF contributed to the experimental design, data interpretation, and critical manuscript revision. TO contributed to the study conception and experimental design, data analysis and interpretation, and manuscript preparation. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by Human Research Ethics Committee, Faculty of Dentistry, Chulalongkorn University (Approval number 2015-007). The procedure was performed according to the Declaration of Helsinki. Informed consent was obtained from parents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nunthawan Nowwarote, Email: p_now@hotmail.com.
Waleerat Sukarawan, Email: wsukarawan@hotmail.com.
Prasit Pavasant, Email: prasit.pav@chula.ac.th.
Brian L. Foster, Email: foster.1004@osu.edu
Thanaphum Osathanon, Phone: +662-218-8885, Email: thanaphum.o@chula.ac.th.
References
- 1.Osathanon T, Nowwarote N, Pavasant P. Basic fibroblast growth factor inhibits mineralization but induces neuronal differentiation by human dental pulp stem cells through a FGFR and PLCgamma signaling pathway. J Cell Biochem. 2011;112:1807–1816. doi: 10.1002/jcb.23097. [DOI] [PubMed] [Google Scholar]
- 2.Nowwarote N, Sukarawan W, Pavasant P, Osathanon T. Basic fibroblast growth factor regulates REX1 expression via IL-6 in stem cells isolated from human exfoliated deciduous teeth. J Cell Biochem. 2017;118:1480–1488. doi: 10.1002/jcb.25807. [DOI] [PubMed] [Google Scholar]
- 3.Wang G, Zhang H, Zhao Y, Li J, Cai J, Wang P, et al. Noggin and bFGF cooperate to maintain the pluripotency of human embryonic stem cells in the absence of feeder layers. Biochem Biophys Res Commun. 2005;330:934–942. doi: 10.1016/j.bbrc.2005.03.058. [DOI] [PubMed] [Google Scholar]
- 4.Ding VM, Ling L, Natarajan S, Yap MG, Cool SM, Choo AB. FGF-2 modulates Wnt signaling in undifferentiated hESC and iPS cells through activated PI3-K/GSK3beta signaling. J Cell Physiol. 2010;225:417–428. doi: 10.1002/jcp.22214. [DOI] [PubMed] [Google Scholar]
- 5.Miura M, Gronthos S, Zhao M, Lu B, Fisher LW, Robey PG, et al. SHED: stem cells from human exfoliated deciduous teeth. Proc Natl Acad Sci U S A. 2003;100:5807–5812. doi: 10.1073/pnas.0937635100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nowwarote N, Pavasant P, Osathanon T. Role of endogenous basic fibroblast growth factor in stem cells isolated from human exfoliated deciduous teeth. Arch Oral Biol. 2015;60:408–415. doi: 10.1016/j.archoralbio.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 7.Sukarawan W, Nowwarote N, Kerdpon P, Pavasant P, Osathanon T. Effect of basic fibroblast growth factor on pluripotent marker expression and colony forming unit capacity of stem cells isolated from human exfoliated deciduous teeth. Odontology. 2014;102:160–166. doi: 10.1007/s10266-013-0124-3. [DOI] [PubMed] [Google Scholar]
- 8.Li B, Qu C, Chen C, Liu Y, Akiyama K, Yang R, et al. Basic fibroblast growth factor inhibits osteogenic differentiation of stem cells from human exfoliated deciduous teeth through ERK signaling. Oral Dis. 2012;18:285–292. doi: 10.1111/j.1601-0825.2011.01878.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Osathanon T, Nowwarote N, Manokawinchoke J, Pavasant P. bFGF and JAGGED1 regulate alkaline phosphatase expression and mineralization in dental tissue-derived mesenchymal stem cells. J Cell Biochem. 2013;114:2551–2561. doi: 10.1002/jcb.24602. [DOI] [PubMed] [Google Scholar]
- 10.Foster BL, Tompkins KA, Rutherford RB, Zhang H, Chu EY, Fong H, et al. Phosphate: known and potential roles during development and regeneration of teeth and supporting structures. Birth Defects Res C Embryo Today. 2008;84:281–314. doi: 10.1002/bdrc.20136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang YL, Stanford CM, Keller JC. Calcium and phosphate supplementation promotes bone cell mineralization: implications for hydroxyapatite (HA)-enhanced bone formation. J Biomed Mater Res. 2000;52:270–278. doi: 10.1002/1097-4636(200011)52:2<270::AID-JBM5>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 12.Foster BL, Nagatomo KJ, Nociti FH, Jr, Fong H, Dunn D, Tran AB, et al. Central role of pyrophosphate in acellular cementum formation. PLoS One. 2012;7:e38393. doi: 10.1371/journal.pone.0038393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Foster BL, Kuss P, Yadav MC, Kolli TN, Narisawa S, Lukashova L, et al. Conditional Alpl ablation phenocopies dental defects of hypophosphatasia. J Dent Res. 2017;96:81–91. doi: 10.1177/0022034516663633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harmey D, Hessle L, Narisawa S, Johnson KA, Terkeltaub R, Millan JL. Concerted regulation of inorganic pyrophosphate and osteopontin by akp2, enpp1, and ank: an integrated model of the pathogenesis of mineralization disorders. Am J Pathol. 2004;164:1199–1209. doi: 10.1016/S0002-9440(10)63208-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mackenzie NC, Zhu D, Milne EM, van ‘t Hof R, Martin A, Darryl Quarles L, et al. Altered bone development and an increase in FGF-23 expression in Enpp1(−/−) mice. PLoS One. 2012;7:e32177. doi: 10.1371/journal.pone.0032177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dutra EH, Chen IP, Reichenberger EJ. Dental abnormalities in a mouse model for craniometaphyseal dysplasia. J Dent Res. 2013;92:173–179. doi: 10.1177/0022034512468157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ao M, Chavez MB, Chu EY, Hemstreet KC, Yin Y, Yadav MC, et al. Overlapping functions of bone sialoprotein and pyrophosphate regulators in directing cementogenesis. Bone. 2017;105:134–147. doi: 10.1016/j.bone.2017.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thumbigere-Math V, Alqadi A, Chalmers NI, Chavez MB, Chu EY, Collins MT, et al. Hypercementosis associated with ENPP1 mutations and GACI. J Dent Res. 2018;97:432–441. doi: 10.1177/0022034517744773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hatch NE, Nociti F, Swanson E, Bothwell M, Somerman M. FGF2 alters expression of the pyrophosphate/phosphate regulating proteins, PC-1, ANK and TNAP, in the calvarial osteoblastic cell line, MC3T3E1(C4) Connect Tissue Res. 2005;46:184–192. doi: 10.1080/03008200500237203. [DOI] [PubMed] [Google Scholar]
- 20.Nowwarote N, Osathanon T, Jitjaturunt P, Manopattanasoontorn S, Pavasant P. Asiaticoside induces type I collagen synthesis and osteogenic differentiation in human periodontal ligament cells. Phytother Res. 2013;27:457–462. doi: 10.1002/ptr.4742. [DOI] [PubMed] [Google Scholar]
- 21.Addison WN, Azari F, Sorensen ES, Kaartinen MT, McKee MD. Pyrophosphate inhibits mineralization of osteoblast cultures by binding to mineral, up-regulating osteopontin, and inhibiting alkaline phosphatase activity. J Biol Chem. 2007;282:15872–15883. doi: 10.1074/jbc.M701116200. [DOI] [PubMed] [Google Scholar]
- 22.Foster BL, Nociti FH, Jr, Swanson EC, Matsa-Dunn D, Berry JE, Cupp CJ, et al. Regulation of cementoblast gene expression by inorganic phosphate in vitro. Calcif Tissue Int. 2006;78:103–112. doi: 10.1007/s00223-005-0184-7. [DOI] [PubMed] [Google Scholar]
- 23.Rutherford RB, Foster BL, Bammler T, Beyer RP, Sato S, Somerman MJ. Extracellular phosphate alters cementoblast gene expression. J Dent Res. 2006;85:505–509. doi: 10.1177/154405910608500605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chaudhary SC, Kuzynski M, Bottini M, Beniash E, Dokland T, Mobley CG, et al. Phosphate induces formation of matrix vesicles during odontoblast-initiated mineralization in vitro. Matrix Biol. 2016;52-54:284–300. doi: 10.1016/j.matbio.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beck GR, Jr, Zerler B, Moran E. Phosphate is a specific signal for induction of osteopontin gene expression. Proc Natl Acad Sci U S A. 2000;97:8352–8357. doi: 10.1073/pnas.140021997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schack LM, Noack S, Winkler R, Wissmann G, Behrens P, Wellmann M, et al. The phosphate source influences gene expression and quality of mineralization during in vitro osteogenic differentiation of human mesenchymal stem cells. PLoS One. 2013;8:e65943. doi: 10.1371/journal.pone.0065943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu YK, Lu QZ, Pei R, Ji HJ, Zhou GS, Zhao XL, et al. The effect of extracellular calcium and inorganic phosphate on the growth and osteogenic differentiation of mesenchymal stem cells in vitro: implication for bone tissue engineering. Biomed Mater. 2009;4:025004. doi: 10.1088/1748-6041/4/2/025004. [DOI] [PubMed] [Google Scholar]
- 28.Silverio-Ruiz KG, Martinez AE, Garlet GP, Barbosa CF, Silva JS, Cicarelli RM, et al. Opposite effects of bFGF and TGF-beta on collagen metabolism by human periodontal ligament fibroblasts. Cytokine. 2007;39:130–137. doi: 10.1016/j.cyto.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 29.Lachgar S, Charveron M, Bouhaddioui N, Neveux Y, Gall Y, Bonafe JL. Inhibitory effects of bFGF, VEGF and minoxidil on collagen synthesis by cultured hair dermal papilla cells. Arch Dermatol Res. 1996;288:469–473. doi: 10.1007/BF02505237. [DOI] [PubMed] [Google Scholar]
- 30.Nataf V, Tsagris L, Dumontier MF, Bonaventure J, Corvol M. Modulation of sulfated proteoglycan synthesis and collagen gene expression by chondrocytes grown in the presence of bFGF alone or combined with IGF1. Reprod Nutr Dev. 1990;30:331–342. doi: 10.1051/rnd:19900306. [DOI] [PubMed] [Google Scholar]
- 31.Camilleri S, McDonald F. Runx2 and dental development. Eur J Oral Sci. 2006;114:361–373. doi: 10.1111/j.1600-0722.2006.00399.x. [DOI] [PubMed] [Google Scholar]
- 32.Komori T. Signaling networks in RUNX2-dependent bone development. J Cell Biochem. 2011;112:750–755. doi: 10.1002/jcb.22994. [DOI] [PubMed] [Google Scholar]
- 33.Lombardi G, Perego S, Luzi L, Banfi G. A four-season molecule: osteocalcin. Updates in its physiological roles. Endocrine. 2015;48:394–404. doi: 10.1007/s12020-014-0401-0. [DOI] [PubMed] [Google Scholar]
- 34.Karsenty G. Update on the biology of osteocalcin. Endocr Pract. 2017;23:1270–1274. doi: 10.4158/EP171966.RA. [DOI] [PubMed] [Google Scholar]
- 35.Wu J, Huang GT, He W, Wang P, Tong Z, Jia Q, et al. Basic fibroblast growth factor enhances stemness of human stem cells from the apical papilla. J Endod. 2012;38:614–622. doi: 10.1016/j.joen.2012.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.An S, Huang X, Gao Y, Ling J, Huang Y, Xiao Y. FGF-2 induces the proliferation of human periodontal ligament cells and modulates their osteoblastic phenotype by affecting Runx2 expression in the presence and absence of osteogenic inducers. Int J Mol Med. 2015;36:705–711. doi: 10.3892/ijmm.2015.2271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Teplyuk NM, Haupt LM, Ling L, Dombrowski C, Mun FK, Nathan SS, et al. The osteogenic transcription factor Runx2 regulates components of the fibroblast growth factor/proteoglycan signaling axis in osteoblasts. J Cell Biochem. 2009;107:144–154. doi: 10.1002/jcb.22108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zweifler LE, Patel MK, Nociti FH, Jr, Wimer HF, Millan JL, Somerman MJ, et al. Counter-regulatory phosphatases TNAP and NPP1 temporally regulate tooth root cementogenesis. Int J Oral Sci. 2015;7:27–41. doi: 10.1038/ijos.2014.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kyono A, Avishai N, Ouyang Z, Landreth GE, Murakami S. FGF and ERK signaling coordinately regulate mineralization-related genes and play essential roles in osteocyte differentiation. J Bone Miner Metab. 2012;30:19–30. doi: 10.1007/s00774-011-0288-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Foster BL, Nagatomo KJ, Tso HW, Tran AB, Nociti FH, Jr, Narisawa S, et al. Tooth root dentin mineralization defects in a mouse model of hypophosphatasia. J Bone Miner Res. 2013;28:271–282. doi: 10.1002/jbmr.1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beck GR, Jr. Inorganic phosphate as a signaling molecule in osteoblast differentiation. J Cell Biochem 2003;90:234–243. [DOI] [PubMed]
- 42.Conrads KA, Yu LR, Lucas DA, Zhou M, Chan KC, Simpson KA, et al. Quantitative proteomic analysis of inorganic phosphate-induced murine MC3T3-E1 osteoblast cells. Electrophoresis. 2004;25:1342–1352. doi: 10.1002/elps.200405892. [DOI] [PubMed] [Google Scholar]
- 43.Conrads KA, Yi M, Simpson KA, Lucas DA, Camalier CE, Yu LR, et al. A combined proteome and microarray investigation of inorganic phosphate-induced pre-osteoblast cells. Mol Cell Proteomics. 2005;4:1284–1296. doi: 10.1074/mcp.M500082-MCP200. [DOI] [PubMed] [Google Scholar]
- 44.Fatherazi S, Matsa-Dunn D, Foster BL, Rutherford RB, Somerman MJ, Presland RB. Phosphate regulates osteopontin gene transcription. J Dent Res. 2009;88:39–44. doi: 10.1177/0022034508328072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sodek J, Ganss B, McKee MD. Osteopontin. Crit Rev Oral Biol Med. 2000;11:279–303. doi: 10.1177/10454411000110030101. [DOI] [PubMed] [Google Scholar]
- 46.McKee MD, Hoac B, Addison WN, Barros NM, Millan JL, Chaussain C. Extracellular matrix mineralization in periodontal tissues: noncollagenous matrix proteins, enzymes, and relationship to hypophosphatasia and X-linked hypophosphatemia. Periodontol 2000. 2013;63:102–122. doi: 10.1111/prd.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Salmon B, Bardet C, Coyac BR, Baroukh B, Naji J, Rowe PS, et al. Abnormal osteopontin and matrix extracellular phosphoglycoprotein localization, and odontoblast differentiation, in X-linked hypophosphatemic teeth. Connect Tissue Res. 2014;55(Suppl 1):79–82. doi: 10.3109/03008207.2014.923864. [DOI] [PubMed] [Google Scholar]
- 48.Foster BL, Ao M, Salmon CR, Chavez MB, Kolli TN, Tran AB, et al. Osteopontin regulates dentin and alveolar bone development and mineralization. Bone. 2018;107:196–207. doi: 10.1016/j.bone.2017.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Boskey AL, Spevak L, Paschalis E, Doty SB, McKee MD. Osteopontin deficiency increases mineral content and mineral crystallinity in mouse bone. Calcif Tissue Int. 2002;71:145–154. doi: 10.1007/s00223-001-1121-z. [DOI] [PubMed] [Google Scholar]
- 50.Yadav MC, Huesa C, Narisawa S, Hoylaerts MF, Moreau A, Farquharson C, et al. Ablation of osteopontin improves the skeletal phenotype of phospho1(−/−) mice. J Bone Miner Res. 2014;29:2369–2381. doi: 10.1002/jbmr.2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Saito K, Nakatomi M, Ida-Yonemochi H, Ohshima H. Osteopontin is essential for type I collagen secretion in reparative dentin. J Dent Res. 2016;95:1034–1041. doi: 10.1177/0022034516645333. [DOI] [PubMed] [Google Scholar]
- 52.Berendsen AD, Smit TH, Schoenmaker T, Walboomers XF, Harris SE, Everts V, et al. Inorganic phosphate stimulates DMP1 expression in human periodontal ligament fibroblasts embedded in three-dimensional collagen gels. Cells Tissues Organs. 2010;192:116–124. doi: 10.1159/000289585. [DOI] [PubMed] [Google Scholar]
- 53.Ye L, MacDougall M, Zhang S, Xie Y, Zhang J, Li Z, et al. Deletion of dentin matrix protein-1 leads to a partial failure of maturation of predentin into dentin, hypomineralization, and expanded cavities of pulp and root canal during postnatal tooth development. J Biol Chem. 2004;279:19141–19148. doi: 10.1074/jbc.M400490200. [DOI] [PubMed] [Google Scholar]
- 54.Feng JQ, Ward LM, Liu S, Lu Y, Xie Y, Yuan B, et al. Loss of DMP1 causes rickets and osteomalacia and identifies a role for osteocytes in mineral metabolism. Nat Genet. 2006;38:1310–1315. doi: 10.1038/ng1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sinha KM, Zhou X. Genetic and molecular control of osterix in skeletal formation. J Cell Biochem. 2013;114:975–984. doi: 10.1002/jcb.24439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kim TH, Bae CH, Lee JC, Kim JE, Yang X, de Crombrugghe B, et al. Osterix regulates tooth root formation in a site-specific manner. J Dent Res. 2015;94:430–438. doi: 10.1177/0022034514565647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen Z, Chen D, McCarthy TL, Centrella M, Zhang Y, Moeckel GW. Inorganic phosphate stimulates fibronectin expression in renal fibroblasts. Cell Physiol Biochem. 2012;30:151–159. doi: 10.1159/000339054. [DOI] [PubMed] [Google Scholar]
- 58.Mathew S, Tustison KS, Sugatani T, Chaudhary LR, Rifas L, Hruska KA. The mechanism of phosphorus as a cardiovascular risk factor in CKD. J Am Soc Nephrol. 2008;19:1092–1105. doi: 10.1681/ASN.2007070760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gurley KA, Chen H, Guenther C, Nguyen ET, Rountree RB, Schoor M, et al. Mineral formation in joints caused by complete or joint-specific loss of ANK function. J Bone Miner Res. 2006;21:1238–1247. doi: 10.1359/jbmr.060515. [DOI] [PubMed] [Google Scholar]
- 60.Beertsen W, VandenBos T, Everts V. Root development in mice lacking functional tissue non-specific alkaline phosphatase gene: inhibition of acellular cementum formation. J Dent Res. 1999;78:1221–1229. doi: 10.1177/00220345990780060501. [DOI] [PubMed] [Google Scholar]
- 61.Nociti FH, Jr, Berry JE, Foster BL, Gurley KA, Kingsley DM, Takata T, et al. Cementum: a phosphate-sensitive tissue. J Dent Res. 2002;81:817–821. doi: 10.1177/154405910208101204. [DOI] [PubMed] [Google Scholar]
- 62.Osathanon T, Giachelli CM, Somerman MJ. Immobilization of alkaline phosphatase on microporous nanofibrous fibrin scaffolds for bone tissue engineering. Biomaterials. 2009;30:4513–4521. doi: 10.1016/j.biomaterials.2009.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hacchou Y, Uematsu T, Ueda O, Usui Y, Uematsu S, Takahashi M, et al. Inorganic polyphosphate: a possible stimulant of bone formation. J Dent Res. 2007;86:893–897. doi: 10.1177/154405910708600917. [DOI] [PubMed] [Google Scholar]
- 64.Rodrigues TL, Nagatomo KJ, Foster BL, Nociti FH, Somerman MJ. Modulation of phosphate/pyrophosphate metabolism to regenerate the periodontium: a novel in vivo approach. J Periodontol. 2011;82:1757–1766. doi: 10.1902/jop.2011.110103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lee TH, Kim WT, Ryu CJ, Jang YJ. Optimization of treatment with recombinant FGF-2 for proliferation and differentiation of human dental stem cells, mesenchymal stem cells, and osteoblasts. Biochem Cell Biol. 2015;93:298–305. doi: 10.1139/bcb-2014-0140. [DOI] [PubMed] [Google Scholar]
- 66.Fakhry A, Ratisoontorn C, Vedhachalam C, Salhab I, Koyama E, Leboy P, et al. Effects of FGF-2/-9 in calvarial bone cell cultures: differentiation stage-dependent mitogenic effect, inverse regulation of BMP-2 and noggin, and enhancement of osteogenic potential. Bone. 2005;36:254–266. doi: 10.1016/j.bone.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 67.Kartal Y, Ucok C, Ozgul O, Doruk Kocyigit I, Tolga Suer B. Effect of locally applied bFGF on implant stability: biomechanical evaluation of 2 different implant surfaces in rabbits. Implant Dent. 2014;23:463–470. doi: 10.1097/ID.0000000000000104. [DOI] [PubMed] [Google Scholar]
- 68.Zou GK, Song YL, Zhou W, Yu M, Liang LH, Sun DC, et al. Effects of local delivery of bFGF from PLGA microspheres on osseointegration around implants in diabetic rats. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:284–289. doi: 10.1016/j.tripleo.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 69.Li F, Yu F, Xu X, Li C, Huang D, Zhou X, et al. Evaluation of recombinant human FGF-2 and PDGF-BB in periodontal regeneration: a systematic review and meta-analysis. Sci Rep. 2017;7:65. doi: 10.1038/s41598-017-00113-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hoshi S, Akizuki T, Matsuura T, Ikawa T, Kinoshita A, Oda S, et al. Ridge augmentation using recombinant human fibroblast growth factor-2 with biodegradable gelatin sponges incorporating beta-tricalcium phosphate: a preclinical study in dogs. J Periodontal Res. 2016;51:77–85. doi: 10.1111/jre.12285. [DOI] [PubMed] [Google Scholar]
- 71.Chen M, Song K, Rao N, Huang M, Huang Z, Cao Y. Roles of exogenously regulated bFGF expression in angiogenesis and bone regeneration in rat calvarial defects. Int J Mol Med. 2011;27:545–553. doi: 10.3892/ijmm.2011.619. [DOI] [PubMed] [Google Scholar]
- 72.Du M, Zhu T, Duan X, Ge S, Li N, Sun Q, et al. Acellular dermal matrix loading with bFGF achieves similar acceleration of bone regeneration to BMP-2 via differential effects on recruitment, proliferation and sustained osteodifferentiation of mesenchymal stem cells. Mater Sci Eng C Mater Biol Appl. 2017;70:62–70. doi: 10.1016/j.msec.2016.08.049. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Primer sequences for QPCR. (DOCX 18 kb)
Data Availability Statement
Please contact the corresponding author for data requests.