Abstract
Background:
There is an increasing interest in using digitized whole-slide imaging (WSI) for routine surgical pathology diagnoses. Screencasts are digital recordings of computer screen output with advanced interactive features that allow for the preparation of videos. Screencasts that include hyperlinks to WSIs could help teach pathology residents how to become familiar with technologies that they are likely to use in their future career.
Materials and Methods:
Twenty screencasts were prepared with Camtasia 2.0 software (TechSmith, Okemos, MI, USA). They included clinical history, videos of chest X-rays and/or chest computed tomography images, links to WSI digitized with an Aperio Turbo AT scanner (Leica Biosystems, Buffalo Grove, IL, USA), pre- and posttests, and faculty-narrated videos of the WSI in a manner closely resembling a slide seminar and other educational materials. Screencasts were saved in a hospital network, Screencast.com, YouTube.com, and Vimeo.com. The screencasts were viewed by 12 pathology residents and fellows who made diagnoses, answered the quizzes, and took a survey with questions designed to evaluate their perception of the quality of this technology. Quiz results were automatically e-mailed to faculty. Pre- and posttest results were compared using a paired t-test.
Results:
Screencasts can be viewed with Windows PC and Mac operating systems and mobile devices; only videos saved in our network and screencast.com could be used to generate quizzes. Participants’ feedback was very favorable with average scores ranging from 4.5 to 4.8 (on a scale of 5). Mean posttest scores (87.0% [±21.6%]) were significantly improved over those in the pretest quizzes (48.5% [±31.2%]) (P < 0.0001).
Conclusion:
Screencasts with WSI that allow residents and fellows to diagnose cases using digital microscopy may prove to be a useful technology to enhance the pathology education. Future studies with larger numbers of screencasts and participants are needed to optimize various teaching strategies.
Keywords: Digital microscopy, screencasts, teaching surgical pathology, whole-slide imaging
INTRODUCTION
Pathology is undergoing significant changes with the incorporation of molecular pathology techniques into routine reporting and the increasing use of digital imaging and other digital technologies in daily practice.[1,2,3,4,5,6,7] In the near future, pathology graduates are likely to practice in an environment that leverages digital pathology systems and robotics to improve efficiency, reduce cost, and potentially improve the quality of medical care.[2,4,5,6,8,9,10,11,12,13,14,15,16] Recently, digital pathology vendors such as Leica-Aperio, Philips, and Roche-Ventana have incorporated a common Digital Imaging and Communications in Medicine (DICOM) standard file format and network protocol into their products.[4,17,18,19] The use of a common DICOM standard can facilitate the wide distribution and viewing of whole-slide imaging (WSI) prepared with different systems and is likely to stimulate the adoption of digital pathology systems for routine surgical pathology work in an increasing number of hospitals and other pathology practices. One such digital pathology system from the Philips Medical Systems has been approved by the Food and Drug Administration in April 2017 for routine diagnostic work. We expect similar vendors incorporating this technology to receive approval for their digital pathology systems in the near future.[1,2,4,17]
These technological advances raise questions regarding how well we prepare our residents for the use of digital microscopy and other digital technologies in future diagnostic work. Our department has purchased whole-slide digital scanners and digitized a large number of cases of interest from various subspecialties that are available for “voluntary review” by residents. These are periodically used by faculty in “unknown case” conferences. However, it is our impression that residents and fellows are often too busy or lack the motivation to take advantage from these learning materials on their own time.
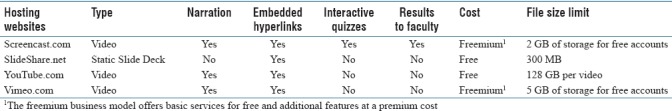
Screencasts are digital recordings of computer screen output with advanced interactive features that allow for the preparation of videos that capture real-time activities on a computer screen. Multiple commercially available applications are currently available for the preparation of screencasts. There are also multiple hosting websites that allow for the storage and sharing of these video-based lectures and/or slide-based lectures, as shown in Table 1.
Table 1.
List of hosting website options
Camtasia (TechSmith, Okemos, Michigan, https://www.techsmith.com/video-editor.html) is all-in-one software that acts as a screen recorder as well as a video editor to edit, trim, and split video clips. It provides interactive features that include quizzes with results automatically e-mailed to faculty, bookmarks to specific points of the video, as well as hyperlinks to outside sources such as journal articles. Camtasia software also includes many motion graphic features such as animations, transitions, and annotations. The screencasts can, therefore, include PowerPoint presentations (Microsoft, Redmond, WA, USA), audio narrations, quizzes, and hyperlinks to various materials and be made available on a local network or the internet. To our knowledge, there has been limited interest in the development of teaching strategies specifically designed to train pathology residents to use digital microscopy for the routine diagnosis of surgical pathology cases.[13,20] Several applications and digital image repositories that incorporate annotated text and WSI have been developed including PathPresenter (https://www.pathpresenter.net), the digital pathology association (https://digitalpathologyassociation.org/whole-slide-imaging-repository), PathoBin (https://pathobin.com), and Philips pathology education tutor (http://www.pathxl.com/pathology-education-tutor), but to our knowledge, there is no information or data in the pathology literature regarding their acceptance as educational tools.
We report the results of a pilot study evaluating the use of screencasts designed to teach residents how to diagnose pulmonary pathology cases using digital microscopy. The screencasts contain hyperlinks to WSI that can be viewed on a computer or mobile device using readily available viewer software, narrated slide descriptions that closely simulate a traditional slide seminar, narrated short lectures, and hyperlinks to journal articles and other documents. Brief clinical histories, images, and WSI did not contain any information that could identify actual patients at Cedars-Sinai Medical Center and were exempted from the institutional review board. The screencasts provide a supervised rather than a “voluntary” teaching environment, as they include pre- and post-test quizzes that the residents are expected to answer as they study the materials; the answers to these quizzes are automatically distributed to faculty by e-mail.
MATERIALS AND METHODS
Twenty “virtual pathology cases” were selected from neoplastic and nonneoplastic lung cases available in our pathology archives. Pulmonary pathology was chosen as the subject for the pilot use of screencast technology because residents generally get limited and intermittent exposure to interesting cases during their bi-weekly rotations at our institution. Pulmonary pathology is also the subspecialty of interest to two of the authors (AM, SK). The selected neoplastic and nonneoplastic lung cases included infectious diseases (Mycobacteria, Aspergillus spp., Coccidioides spp., Pneumocystis jiroveci, Cryptococcus spp., and Histoplasma spp.), acute lung injury (aspiration pneumonia), chronic diffuse lung injury (usual interstitial pneumonia, nonspecific interstitial pneumonia, hypersensitivity pneumonitis, and sarcoidosis), lung transplantation pathology (acute cellular rejection), lymphomas (mantle cell lymphoma and intravascular lymphoma), neoplasms (lung adenocarcinoma, epithelioid mesothelioma, and Langerhans cell histiocytosis), and other rare lung lesions (pulmonary alveolar proteinosis, amyloidosis, and mesothelial hyperplasia). The cases were anonymized by replacing the slide labels with patient information with labels showing only arbitrary teaching slide numbers. WSI of these cases was prepared at ×20 original magnification using an Aperio AT Turbo scanner (Leica Biosystems, Buffalo Grove, IL, USA) and stored in a shared drive available in our hospital's network.
Each virtual pathology case was prepared using PowerPoint software (Microsoft, Redmond, WA, USA) and Camtasia Studio 8® (TechSmith, Okemos, MI, USA). After the slides were scanned in, each screencast took approximately 1–2 h to produce and was structured to provide teaching materials in the following sequence: brief clinical history, imaging studies, hyperlink to WSI, pretest quiz asking for diagnosis and other questions pertinent to the case, and a faculty-narrated video describing the WSI. The faculty explains the case as it would have been done in a traditional slide seminar using a multiheaded microscope, with salient points of the pathologic entity being illustrated and a final quiz [Figure 1]. The clinical history is shown in one or more PowerPoint slides [Figure 1a]. The videos with imaging information were recorded with Camtasia software of the chest computed tomography scans and/or chest X-rays using a desktop computer and the picture archiving and communication system available in our electronic medical records [Figure 1b]. Videos were also recorded of narrated descriptions and brief lectures of the entity being discussed by a faculty member of the same Aperio slides that were previously viewed by the trainee. These videos were saved in TREC and CAMPROJ file formats.
Figure 1.
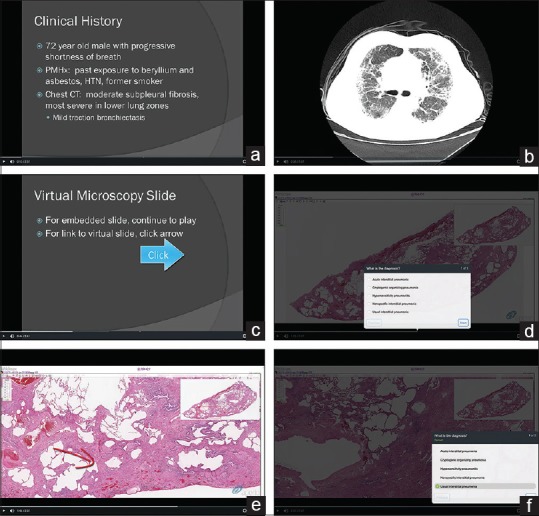
Components of screencasts: brief clinical history (a), imaging studies (b), options of viewing embedded video of whole-slide image and/or manual viewing of whole-slide image (c), pretest (d), annotations in faculty-narrated segments (e), and posttest with subsequent answers provided (f)
Once all the materials necessary to prepare a virtual pathology case were created, PowerPoint files and recorded videos were imported into the Camtasia software and organized with ease in the sequence listed in the previous paragraph by simply dragging each file in the desired order. Interactive features such as hyperlinks to the location of the Aperio slides [Figure 1c] and quizzes [Figure 1d] were then added to the screencasts. Arrows, text boxes, and other various geometric shapes were used to annotate and highlight features in the faculty-narrated segments [Figure 1e]. A posttest was included to assess whether the users learned from the teaching materials [Figure 1f]. The screencasts were saved as CAMPROJ files in the departmental shared drive and uploaded to Screencast.com. Files were also saved as a digital multimedia container file format (MP4), which were uploaded to YouTube.com and Vimeo.com.
These screencasts can be viewed with personal computers using Windows 7 or higher operating system, MacOS 10.10 or higher operating system, and/or mobile devices using iOS® (Apple, Cupertino, CA, USA) or Android® (Alphabet, Mountain View, CA, USA) software. The WSI can be viewed using ImageScope software or WebScope web-based software (Aperio, Leica Biosystems, Buffalo Grove, Illinois, USA) from the hospital's hosting options. Both ImageScope and WebScope enable the adjustment of the WSIs from low to high magnifications [Figure 2]. Videos without narrations that recorded the observation of the WSI at various magnifications can alternatively be viewed from nonlocal hosting sites. The quiz results included in the screencasts are automatically e-mailed to a selected faculty member, who is able to confirm that the resident studied the materials and demonstrated mastery of the materials by comparing the pre- and post-test scores.
Figure 2.
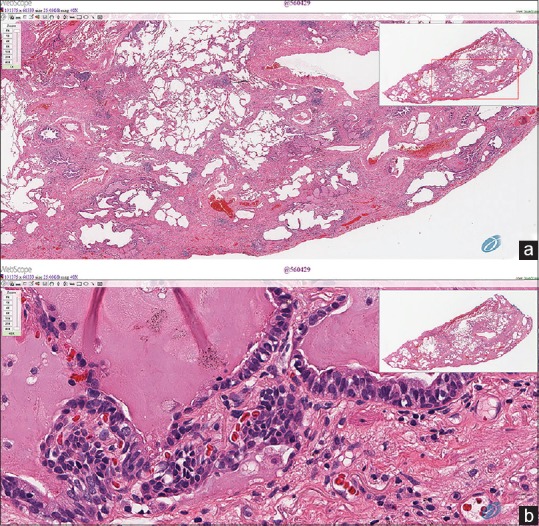
WebScope software (Leica Biosystems) enables the adjustment of the whole-slide images from low (a) to high (b) magnifications
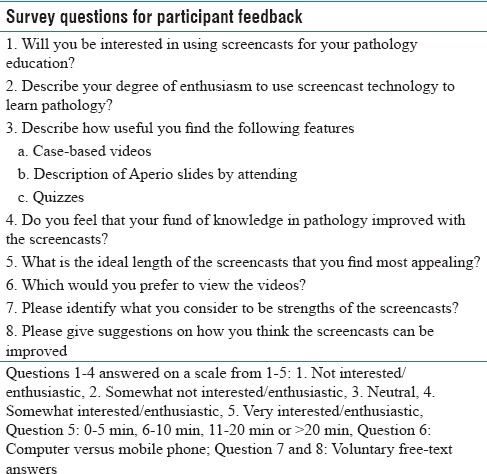
Ten pathology residents (3 PGY-1's, 3 PGY-2's, 2 PGY-3's, and 2 PGY-4's) and two fellows (2 PGY-5's) were asked to view the screencasts and provide feedback by answering a survey containing several questions. All responses by participants were collected anonymously. The initial sections of the screencasts showed the “virtual pathology cases,” including hyperlinks to the WSI. The residents and fellows were asked to diagnose the cases using digital microscopy and to provide their diagnostic assessment by answering the pretest quizzes. After completing these tasks, they were able to view and listen to a discussion of the case, akin to a slide seminar discussion, by faculty. At the end of the exercise, they were asked to answer posttest questions that “certified” that they had studied the materials using the screencasts. The survey questions were designed to get participant feedback regarding the quality of the teaching materials, the evaluation of the technical quality of screencasts on a 1–5 scale, the interest in using screencasts for their education, and the enthusiasm about the usefulness of this teaching format shown in Table 2. The survey also included questions regarding the ideal length of the screencasts and preferences in the platform to view the screencasts and allowed for voluntary free-text answers regarding strengths and weaknesses in the screencasts and suggestions for improvement. The results of the pre- and post-tests were compared using a paired t-test.
Table 2.
List of survey questions for participant's feedback
RESULTS
Screencast files were relatively small, up to 100 MB for videos lasting up to 10 min. Screencasts could be adequately viewed using the departmental intranet, YouTube.com, Vimeo.com, and screencast.com using desktop computers, laptop computers, and iOS® or Android® mobile devices. Screencast.com has a limit of 2 GB of storage upload per month free of charge. YouTube.com offers unlimited uploads, restricts each video size to no more than 128 GB, and does not support interactive capabilities. Vimeo.com does not support interactive capabilities and has weekly limits of storage upload. The three internet companies offer different payment plans with various storage and other additional options. Of these options, only files saved in the departmental intranet and/or screencast.com provided the ability to answer quizzes and automatically e-mail the results to an attending pathologist. These sites were used by the residents to study the materials and answer the quizzes.
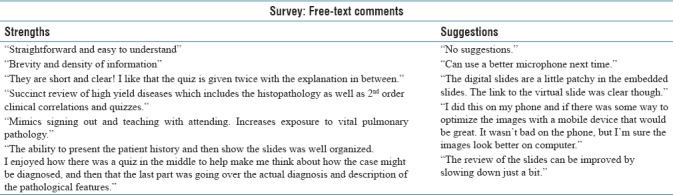
Feedback by participants was very encouraging as shown by average score answers to the various survey questions ranging from 4.5 to 4.8 [Figure 3]. Free-text responses to the survey included favorable comments by several residents who found that the screencasts were fun to use and a valuable learning tool. Additional free-text comments are included in Table 3. Participants significantly improved the number of correct answers in posttests (mean = 87.0% [±21.6%]; median = 100.0%) from those in the pretests (mean = 48.5% [±31.2%]; median = 33.3%) (P < 0.0001).
Figure 3.
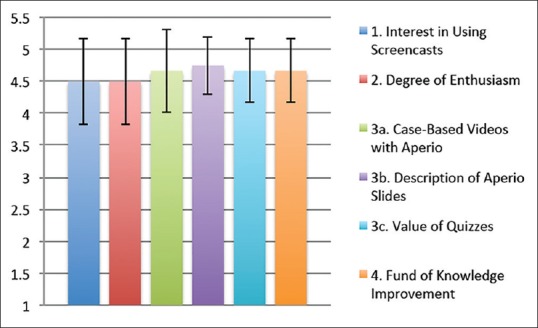
Feedback from participants to survey questions is favorable with mean values of 4.5–4.8 higher on a scale of 1–5 (n = 12). The bar graph shows mean values and standard deviations
Table 3.
Free-text comments from survey
DISCUSSION
Our pilot project shows that screencasts containing “virtual pathology cases,” digitized slide seminars, and other learning materials can be readily prepared by pathology staff and house staff without the need for specialized technical support. The screencasts were well received by our residents and fellows and appear to provide a useful learning tool that could stimulate them to become familiar with the use of digital microscopy for routine diagnosis, while exposing them to a collection of interesting surgical pathology cases that may not be readily encountered during their relatively brief rotations through various subspecialties. This manuscript mainly focuses on the use of screencasts to teach surgical pathology using digital pathology, but the technology can also be used to teach gross pathology and the performance of various techniques such as the preparation of frozen sections, preparation of samples for lymphoma workup, and other tasks. Although there is vast content demonstrating its widespread use in higher education environments, there is limited information in the pathology literature illustrating the use of screencasts for educational activities. Literature search only showed that Mills et al. described the use of screencasts containing “sound bites” as a tool to teach cytopathology.[21] These “sound bites” included PowerPoint-based lectures with voice narration and multiple choice checkpoints.[21]
Multiple studies in our laboratory and others have shown that similar diagnoses can be obtained using digital and light microscopy and that digital microscopy can be effectively used for primary surgical pathology diagnosis, telepathology, teaching, and other applications.[22,23,24,25,26,27,28,29,30] Digital pathology systems offer a variety of logistical advantages, as they can streamline the flow and storage of cases, help reduce clerical errors, shorten turnaround time, and provide other operational efficiencies. These have stimulated an increasing interest in using them to replace the time-tested method of distributing glass slides throughout a laboratory for examination with light microscopes.[10,14,20]
Digital microscopy has already proven to be a practical alternative to conventional microscopy in pathology education and has replaced traditional microscope laboratories in many medical and dental schools.[13,31,32,33,34] It has also been used to provide a large number of interesting cases over the internet.[35,36,37,38] The potential advantages of digital microscopy include the ability to store and distribute cases, integrate the scans with the electronic medical records for review, disseminate imaging studies, and facilitate second opinion consults by pathologists inside or outside the hospital system anywhere in the world. The use of digital microscopy will also probably stimulate the development of various image analysis methods that use deep learning algorithms and other artificial intelligence methods as diagnostic aids.[39,40,41,42,43] In our view, it is likely that digital pathology systems will rapidly improve their capabilities and decrease their cost as other computer-based technologies have done in the past. Thus, while the use of screencasts will increase pathology trainees’ exposure to pulmonary pathology, it will also give them exposure to digital microscopy in a manner that encourages them to become comfortable with the use of this technology for primary diagnosis in this advancing technological landscape. These educational efforts need to include a frank discussion of some of the current limitations of digital microscopy for cytologic diagnosis, where there is a need to focus the images in multiple planes, and evaluation of small structures such as mycobacteria that may be difficult to view on WSI prepared with current technology.
CONCLUSIONS
Screencasts offer practical teaching tools to familiarize residents and fellows to digital microscopy by having them diagnose actual “virtual cases” and to provide them with instructional videos that complement the diagnostic activity. Indeed, at a time, when YouTube and other websites have thousands of educational videos showing how to perform a variety of tasks, including how to learn pathology, it is a little surprising that screencasts or other videos have not been used more frequently to train residents, fellows, technologists, and other laboratory personnel. Although our pilot study has had positive feedback and results with our trainees, future studies where the potential of screencasts as a tool to teach pathology is evaluated with a larger number of digital pathology cases and a larger cohort of pathology trainees are needed to promote the use of this technology.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Available FREE in open access from: http://www.jpathinformatics.org/text.asp?2018/9/1/39/245401
REFERENCES
- 1.Flotte TJ, Bell DA. Anatomical pathology is at a crossroads. Pathology. 2018;50:373–4. doi: 10.1016/j.pathol.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Glassy EF. Digital pathology: Quo vadis? Pathology. 2018;50:375–6. doi: 10.1016/j.pathol.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Scimeca M, Urbano N, Bonfiglio R, Schillaci O, Bonanno E. Management of oncological patients in the digital era: Anatomic pathology and nuclear medicine teamwork. Future Oncol. 2018;14:1013–5. doi: 10.2217/fon-2017-0698. [DOI] [PubMed] [Google Scholar]
- 4.Clunie D, Hosseinzadeh D, Wintell M, De Mena D, Lajara N, Garcia-Rojo M, et al. Digital imaging and communications in medicine whole slide imaging connectathon at digital pathology association pathology visions 2017. J Pathol Inform. 2018;9:6. doi: 10.4103/jpi.jpi_1_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fraggetta F, Rossi ED, Pantanowitz L. Advocating a laboratory information system-centric approach to digital pathology. Arch Pathol Lab Med. 2018;142:434. doi: 10.5858/arpa.2017-0487-LE. [DOI] [PubMed] [Google Scholar]
- 6.Williams BJ, Bottoms D, Clark D, Treanor D. Future-proofing pathology part 2: Building a business case for digital pathology. J Clin Pathol 2018. doi: 10.1136/jclinpath-2017-204926. pii: jclinpath-2017-204926. [DOI] [PubMed] [Google Scholar]
- 7.Gru AA, Kim J, Pulitzer M, Guitart J, Battistella M, Wood GS, et al. The use of central pathology review with digital slide scanning in advanced-stage mycosis fungoides and sézary syndrome: A multi-institutional and international pathology study. Am J Surg Pathol. 2018;42:726–34. doi: 10.1097/PAS.0000000000001041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vergani A, Regis B, Jocollé G, Patetta R, Rossi G. Noninferiority diagnostic value, but also economic and turnaround time advantages from digital pathology. Am J Surg Pathol. 2018;42:841–2. doi: 10.1097/PAS.0000000000001035. [DOI] [PubMed] [Google Scholar]
- 9.Acs B, Rimm DL. Not just digital pathology, intelligent digital pathology. JAMA Oncol. 2018;4:403–4. doi: 10.1001/jamaoncol.2017.5449. [DOI] [PubMed] [Google Scholar]
- 10.Williams BJ, Hanby A, Millican-Slater R, Nijhawan A, Verghese E, Treanor D. Digital pathology for the primary diagnosis of breast histopathological specimens: An innovative validation and concordance study on digital pathology validation and training. Histopathology. 2018;72:662–71. doi: 10.1111/his.13403. [DOI] [PubMed] [Google Scholar]
- 11.Volynskaya Z, Chow H, Evans A, Wolff A, Lagmay-Traya C, Asa SL. Integrated pathology informatics enables high-quality personalized and precision medicine: Digital pathology and beyond. Arch Pathol Lab Med. 2018;142:369–82. doi: 10.5858/arpa.2017-0139-OA. [DOI] [PubMed] [Google Scholar]
- 12.Fraggetta F, Garozzo S, Zannoni GF, Pantanowitz L, Rossi ED. Routine digital pathology workflow: The Catania experience. J Pathol Inform. 2017;8:51. doi: 10.4103/jpi.jpi_58_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mea VD, Carbone A, Di Loreto C, Bueno G, De Paoli P, García-Rojo M, et al. Teaching digital pathology: The international school of digital pathology and proposed syllabus. J Pathol Inform. 2017;8:27. doi: 10.4103/jpi.jpi_17_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams BJ, Bottoms D, Treanor D. Future-proofing pathology: The case for clinical adoption of digital pathology. J Clin Pathol. 2017;70:1010–8. doi: 10.1136/jclinpath-2017-204644. [DOI] [PubMed] [Google Scholar]
- 15.Bengtsson E, Danielsen H, Treanor D, Gurcan MN, MacAulay C, Molnár B. Computer-aided diagnostics in digital pathology. Cytometry A. 2017;91:551–4. doi: 10.1002/cyto.a.23151. [DOI] [PubMed] [Google Scholar]
- 16.Juneja S, Juneja M. Virtual digital pathology: The future is near. Indian J Pathol Microbiol. 2017;60:306–7. doi: 10.4103/IJPM.IJPM_324_16. [DOI] [PubMed] [Google Scholar]
- 17.Marques Godinho T, Lebre R, Silva LB, Costa C. An efficient architecture to support digital pathology in standard medical imaging repositories. J Biomed Inform. 2017;71:190–7. doi: 10.1016/j.jbi.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 18.Kalinski T, Zwönitzer R, Roßner M, Hofmann H, Roessner A, Guenther T, et al. Digital imaging and communications in medicine (DICOM) as standard in digital pathology. Histopathology. 2012;61:132–4. doi: 10.1111/j.1365-2559.2012.04243.x. [DOI] [PubMed] [Google Scholar]
- 19.Singh R, Chubb L, Pantanowitz L, Parwani A. Standardization in digital pathology: Supplement 145 of the DICOM standards. J Pathol Inform. 2011;2:23. doi: 10.4103/2153-3539.80719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Williams BJ, Lee J, Oien KA, Treanor D. Digital pathology access and usage in the UK: Results from a national survey on behalf of the National Cancer Research Institute's CM-path initiative. J Clin Pathol. 2018;71:463–6. doi: 10.1136/jclinpath-2017-204808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mills AN, Meyes-Needham M, LeGallo RD, Boyd JC, Cathro HP, Haverstick DM, et al. From slide sets to sound bites: Teaching and learning pathology in the digital age. J Am Soc Cytopathol. 2014;3:183–7. doi: 10.1016/j.jasc.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Marchevsky AM, Dulbandzhyan R, Seely K, Carey S, Duncan RG. Storage and distribution of pathology digital images using integrated web-based viewing systems. Arch Pathol Lab Med. 2002;126:533–9. doi: 10.5858/2002-126-0533-SADOPD. [DOI] [PubMed] [Google Scholar]
- 23.Marchevsky AM, Lau SK, Khanafshar E, Lockhart C, Phan A, Michaels PJ, et al. Internet teleconferencing method for telepathology consultations from lung and heart transplant patients. Hum Pathol. 2002;33:410–4. doi: 10.1053/hupa.2002.124722. [DOI] [PubMed] [Google Scholar]
- 24.Strauss JS, Felten CL, Okada DH, Marchevsky AM. Virtual microscopy and public-key cryptography for internet telepathology. J Telemed Telecare. 1999;5:105–10. doi: 10.1258/1357633991933404. [DOI] [PubMed] [Google Scholar]
- 25.Okada DH, Binder SW, Felten CL, Strauss JS, Marchevsky AM. “Virtual microscopy” and the internet as telepathology consultation tools: Diagnostic accuracy in evaluating melanocytic skin lesions. Am J Dermatopathol. 1999;21:525–31. doi: 10.1097/00000372-199912000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Singson RP, Natarajan S, Greenson JK, Marchevsky AM. Virtual microscopy and the internet as telepathology consultation tools. A study of gastrointestinal biopsy specimens. Am J Clin Pathol. 1999;111:792–5. doi: 10.1093/ajcp/111.6.792. [DOI] [PubMed] [Google Scholar]
- 27.Dessauvagie BF, Lee AH, Meehan K, Nijhawan A, Tan PH, Thomas J, et al. Interobserver variation in the diagnosis of fibroepithelial lesions of the breast: A multicentre audit by digital pathology. J Clin Pathol. 2018;71:672–9. doi: 10.1136/jclinpath-2017-204977. [DOI] [PubMed] [Google Scholar]
- 28.Rhoads DD, Habib-Bein NF, Hariri RS, Hartman DJ, Monaco SE, Lesniak A, et al. Comparison of the diagnostic utility of digital pathology systems for telemicrobiology. J Pathol Inform. 2016;7:10. doi: 10.4103/2153-3539.177687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Houghton JP, Smoller BR, Leonard N, Stevenson MR, Dornan T. Diagnostic performance on briefly presented digital pathology images. J Pathol Inform. 2015;6:56. doi: 10.4103/2153-3539.168517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Houghton JP, Ervine AJ, Kenny SL, Kelly PJ, Napier SS, McCluggage WG, et al. Concordance between digital pathology and light microscopy in general surgical pathology: A pilot study of 100 cases. J Clin Pathol. 2014;67:1052–5. doi: 10.1136/jclinpath-2014-202491. [DOI] [PubMed] [Google Scholar]
- 31.Williams BJ, Treanor D. A novel leadership fellowship in digital pathology. J Pathol Inform. 2016;7:39. doi: 10.4103/2153-3539.189704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ameisen D, Deroulers C, Perrier V, Bouhidel F, Battistella M, Legrès L, et al. Towards better digital pathology workflows: Programming libraries for high-speed sharpness assessment of whole slide images. Diagn Pathol. 2014;9(Suppl 1):S3. doi: 10.1186/1746-1596-9-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Diaz-Perez JA, Raju S, Echeverri JH. Evaluation of a teaching strategy based on integration of clinical subjects, virtual autopsy, pathology museum, and digital microscopy for medical students. J Pathol Inform. 2014;5:25. doi: 10.4103/2153-3539.137729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sivamalai S, Murthy SV, Gupta TS, Woolley T. Teaching pathology via online digital microscopy: Positive learning outcomes for rurally based medical students. Aust J Rural Health. 2011;19:45–51. doi: 10.1111/j.1440-1584.2010.01176.x. [DOI] [PubMed] [Google Scholar]
- 35.Higgins C. Applications and challenges of digital pathology and whole slide imaging. Biotech Histochem. 2015;90:341–7. doi: 10.3109/10520295.2015.1044566. [DOI] [PubMed] [Google Scholar]
- 36.Vodovnik A. Distance reporting in digital pathology: A study on 950 cases. J Pathol Inform. 2015;6:18. doi: 10.4103/2153-3539.156168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Khvatkov V, Harris E. Pathology: The last digital frontier of biomedical imaging. MLO Med Lab Obs. 2013;45:28–9. [PubMed] [Google Scholar]
- 38.Gutman DA, Cobb J, Somanna D, Park Y, Wang F, Kurc T, et al. Cancer digital slide archive: An informatics resource to support integrated in silico analysis of TCGA pathology data. J Am Med Inform Assoc. 2013;20:1091–8. doi: 10.1136/amiajnl-2012-001469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Robertson S, Azizpour H, Smith K, Hartman J. Digital image analysis in breast pathology-from image processing techniques to artificial intelligence. Transl Res. 2018;194:19–35. doi: 10.1016/j.trsl.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 40.Janowczyk A, Doyle S, Gilmore H, Madabhushi A. A resolution adaptive deep hierarchical (RADHicaL) learning scheme applied to nuclear segmentation of digital pathology images. Comput Methods Biomech Biomed Eng Imaging Vis. 2018;6:270–6. doi: 10.1080/21681163.2016.1141063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Qiu JX, Yoon HJ, Fearn PA, Tourassi GD. Deep learning for automated extraction of primary sites from cancer pathology reports. IEEE J Biomed Health Inform. 2018;22:244–51. doi: 10.1109/JBHI.2017.2700722. [DOI] [PubMed] [Google Scholar]
- 42.Janowczyk A, Madabhushi A. Deep learning for digital pathology image analysis: A comprehensive tutorial with selected use cases. J Pathol Inform. 2016;7:29. doi: 10.4103/2153-3539.186902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ertosun MG, Rubin DL. Automated grading of gliomas using deep learning in digital pathology images: A modular approach with ensemble of convolutional neural networks. AMIA Annu Symp Proc 2015. 2015:1899–908. [PMC free article] [PubMed] [Google Scholar]


