Abstract
Introduction:
Early detection is crucial for prompt management of acute kidney injury (AKI) patients in emergency department (ED). This study aimed to investigate the usefulness of hyperchloremic metabolic acidosis (HCMA) levels in this regard.
Methods:
In this retrospective observational study, > 18 years old critically ill patients presenting to ED of Marcianise Hospital, Italy, were divided into non-AKI and AKI group according to KDIGO guideline. The level of HCMA ((arterial pH x bicarbonate)/chloride) was compared between groups and correlation of HCMA with estimated glomerular filtration rate (e-GFR) in ARF patients was evaluated.
Results:
134 patients with the mean age of 76.5 ± 3.1 years were enrolled (64 non-AKI and 70 AKI; 64% female). Two groups were similar regarding mean age (p = 0.251), sex (p = 0.091), APACHII score (p = 0.215), Charlson Comorbidity Index (p= 0.187), and body mass index (p = 0.129). The mean HCMA level was 1.98 ± 0.09 in the non-AKI group and 1.56 ± 0.07 in the AKI group (p=0.039). There was a positive correlation between HCMA and e-GFR levels in AKI group (r: 0.467, p=0.0092).
Conclusions:
If confirmed and validated in a future study, ABG derived formula for HCMA may be a useful tool for early detection of AKI patients in emergency department.
Key Words: Acute kidney injury, hyperchloremic metabolic acidosis, emergency department, renal function
Introduction:
Acute kidney injury (AKI) is a frequent and potentially life-threatening syndrome, with high costs for patients and the healthcare systems (1). Overall, 5.5% of all emergency department patients had acute kidney injury in one study (2). AKI is defined as a rise in creatinine, 50% from its baseline value, and/or a fall in the glomerular filtration rate (GFR) by 25%, and/or a decrease in urine output reaching less than 0.5 ml/kg/h for 6 h or more (3). AKI in patients is associated with higher mortality. Patients with severe sepsis and septic shock exhibit a complex metabolic acidosis upon intensive care unit admission, caused predominantly by hyperchloremic acidosis, which is more pronounced in non-survivors (4). Normally, the major renal defense against metabolic acidosis is the net urinary excretion of strong anions, such as chloride, and the retention of strong cations (5). This mechanism becomes impaired in AKI patients. An early diagnosis is crucial for prompt management of AKI to anticipate acute renal dysfunction. The purpose of this study was to investigate the usefulness of hypercloremic metabolic acidosis (HCMA) levels evaluated, using an arterial blood gas (ABG) analysis derived formula, for early suspicion of AKI in emergency department (ED).
Methods:
Study design and setting
In the present retrospective observational study, eligible patients who were admitted to University Hospital of Marcianise, Italy, from January 2017 to March 2017, were evaluated regarding HCMA level and its’ correlation with renal function. Ethical Committee of North Campania approved the protocol of the present study and all researchers adhered to the principles of the Helsinki declaration during the study period. Additionally, a consent form was obtained from patients.
Participants
Adult (>18 years old) critically ill patients (Acute Physiology and Chronic Health Evaluation (APACHE II) index >18) in emergency department were subdivided in the non-AKI (with normal creatinine levels and GFR > 90 ml/min/1.73 m2) and the AKI group according to KDIGO guideline. AKI patients were defined as patients whose serum creatinine had increased to ≥ 0.3 mg/dl (26.5 micrmol/L) within 48 hours or 1.5-fold from the baseline, which was known or presumed to have occurred in the preceding 7 days, with decrease in urine output, according KDIGO guidelines (3,8).
Adults with chronic kidney disease or need for renal replacement therapy, those not giving consent, less than 18 years of age, history of acute gastrointestinal and post-operative patients were excluded. The Acute Physiology and Chronic Health Evaluation (APACHE II) score and Charlson Comorbidity Index (CCI) (6, 7) were calculated from the patient charts.
Data gathering and measurements
Demographic and clinical characteristics, patient diagnoses, procedures (e.g. laboratory tests), treatments/interventions and patient outcomes were extracted from patients’ profiles by an emergency medicine specialist who was responsible for data gathering and patients were enrolled using random sampling method.
Glomerular filtration rate (GFR) was evaluated via CKD-EPIdemiology Collaboration (CKD-EPI) equation (8). Serum levels of albumin, creatinine and various electrolytes, including Na, K, Ca, Mg, Cl and HPO4, were recorded for each patient. Blood pH and the partial pressures of oxygen and carbon dioxide in the blood (PaO2 and PaCO2) were measured using a RapidLab Blood Gas Analyzer (GEMrPremiertm 4000 plus). HCMA was evaluated in emergency department, using the following formula: ((pH x HCO3-) / Cl-), where pH is the arterial pH, HCO3- is the arterial bicarbonate concentration and Cl- is the arterial chloride concentration, as reported by ABG analysis, on admission to the Emergency Department.
Statistical Analysis
Data analyses were performed using SPSS, Version 19.0 (IBM Corp, Armonk, NY). Statistical significance was set at p<0.05 for all procedures. Analyses of ABG were made using a non-parametric U-test by Mann-Whitney for independent sample. Data are presented as percentage and mean ± standard error (SE).
Results:
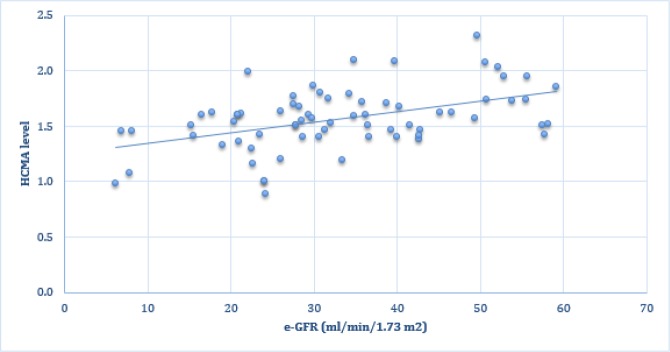
134 patients with the mean age of 76.5 ± 3.1 (68-85) years were enrolled (64 non-AKI and 70 AKI; 64% female). Baseline characteristics of studied patients are reported in table 1. Two groups were similar regarding mean age (p = 0.251), sex (p = 0.091), APACHII score (p = 0.215), Charlson Comorbidity Index (p= 0.187), and body mass index (p = 0.129). Table 2 summarizes the ABG, electrolyte findings of studied patients. The mean HCMA level was 1.98 ± 0.09 in the non-AKI group and 1.56 ± 0.07 in the AKI group (p=0.039). Figure 1 shows the correlation of HCMA and e-GFR levels in AKI patients. There was a positive correlation between HCMA and e-GFR levels in AKI group (r: 0.467, p=0.0092).
Table 1.
Baseline characteristics of studied patients
| Variables | non-AKI (n=64) | AKI (n=70) | P value |
|---|---|---|---|
| Sex | |||
| Male | 22 (34.3) | 26 (37.1) | 0.091 |
| Female | 42 (65.7) | 44 (62.9) | |
| Age (years) | |||
| Mean± SE | 75±4 | 77±3 | 0.251 |
| APACHE II score | |||
| Mean± SE | 22±3 | 24±4 | 0.215 |
| Charlson Comorbidity Index | |||
| Mean± SE | 4.0 ±1.8 | 4.0 ±1.3 | 0.187 |
| BMI (Kg/m 2 ) | |||
| Mean± SE | 21.2 ± 6.0 | 22.3 ± 5.0 | 0.129 |
| Serum Creatinine (mg/dl) | |||
| Mean± SE | 0.79 ± 0.02 | 2.06 ± 0.01 | 0.0091 |
| e-GFR (ml/min/1.73 m 2 ) | |||
| Mean± SE | 91.3 ± 0.45 | 33.4 ± 0.25 | 0.0087 |
| Comorbid disease | |||
| Diabetes | 22 (31) | 33 (47) | 0.041 |
| Hypertension | 44 (59) | 35 (50) | 0.101 |
| Cirrhosis | 2 (3) | 5 (10) | 0.037 |
| COPD | 6 (10) | 8 (11) | 0.180 |
| Heart Failure | 11 (17) | 15 (21) | 0.140 |
Data are presented as mean ± standard error (SE) or number (%). APACHE: Acute Physiology and Chronic Health Evaluation; BMI: Body Mass Index; COPD: Chronic Obstructive Pulmonary Disease.
Table 2.
Laboratory findings of studied patients
| Variables | non-AKI (n=64) | AKI (n=70) | P value |
|---|---|---|---|
| Arterial blood gas parameters | |||
| pH | 7.44 (7.43-7.46) | 7.35 (7.35-7.41) | 0.131 |
| pCO2 | 43 (41-44) | 45 (42-44) | 0.110 |
| pO2 | 65 (61-70) | 60 (62-71) | 0.197 |
| HCO3- | 25.4 (24.5-26.3) | 22.5 (21.3-23.7) | 0.021 |
| Serum electrolyte | |||
| Na+ | 136 (135-139) | 137 (135-140) | 0.199 |
| K+ | 4.5 (4.1-5.1) | 5.0 (4.5-5.3) | 0.213 |
| Cl- | 95.3 (90.6-102.1) | 106.4 (104.2-108.8) | 0.046 |
| (pH x HCO3 - ) / Cl - | |||
| HCMA | 1.98 (1.73-2.08) | 1.56 (1.48-1.65) | 0.039 |
Data are presented with 95% confidence interval. HCMA: hyperchloremic metabolic acidosis level.
Figure 1.
Linear positive correlation between hyperchloremic metabolic acidosis (HCMA) and estimated glomerular filtration rate (e-GFR) levels in AKI group (r: 0.467, p=0.0092).
Discussion:
In this paper we reported the differences of HCMA levels in non-AKI and AKI patients in the emergency department. In AKI patients a significant association between ABG derived hyperchloremic metabolic acidosis state and e-GFR was found.
AKI is associated with higher mortality in emergency patients (9, 10). It has been reported that hyperchloremic acidosis due to the intraoperative chloride load also has an important role in deterioration of renal function (11). Thus, early identification of AKI patients is crucial for their prompt management. Acute kidney injury can lead to hyperchloremic metabolic acidosis especially when the glomerular filtration rate is between 30 to 59 mL/min (stage III) (12, 13). HCMA has been reported in AKI patients (4). In fact, to maintain normal pH, the kidneys have to perform two physiological functions. The first is to reabsorb all the filtered HCO3-. The second is to excrete the daily H+ load (14). In particular, during the early phases of AKI, progressive hyperammonemia results in hyperchloremic metabolic acidosis because of impairment in renal ammonia excretion (15). In the course of AKI there are no classic physical signs and symptoms in the early stage to alert the clinician of ongoing injury. Identifying individuals with suspicion for developing AKI in the ED is of increasing interest. In fact, the present data suggest that the ABG derived formula, for evaluation of HCMA state, may have a potential to be used as a screening test, for early diagnosis of AKI in emergency patients. These data are crucial, because actually the diagnosis of AKI is usually based on changes in serum creatinine. In this regard, serum creatinine is a less rapid indicator of acute renal dysfunction and it may lead to a delay in the diagnosis of AKI. On this note, we found a linear positive correlation between the levels of HCMA, as evaluated by the ABG derived formula, and the impairment of renal function (e-GFR). This is the first study that shows such an association in AKI patients in ED. If confirmed and validated in a future study, the use of ABG derived formula for HCMA may represent a useful tool for early detection of AKI in the emergency department. It seems that HCMA level may be a useful tool for the early detection of AKI within the first few hours of admission.
Limitations
Limitations of the present study are mainly represented by the retrospective study design. In this regard, a future large prospective study may be needed to confirm the present findings.
Conclusion:
This is the first report that shows an association between HCMA level and AKI in emergency department patients. If confirmed and validated in a future study, the use of ABG derived formula for HCMA may represent a useful tool for early detection of AKI patients in emergency department.
Acknowledgements
None.
Author contribution
Mauro Giordano and Tiziana Ciarambino designed the study. Pietro Castellino, Lorenzo Malatino, Giuseppe Signoriello, Giuseppe Paolisso, Luigi Elio Adinolfi participated in acquisition and management of data. All authors approved final version of the manuscript to be published and are accountable for all aspects of the work.
Funding/Support
This research has not been supported.
Conflict of interest
The authors declare no conflicts of interest.
References
- 1.Li PKT, Burdmann EA, Mehta RL. Acute kidney injury: global health alert. Arab journal of nephrology and transplantation. 2013;6(2):75–81. [PubMed] [Google Scholar]
- 2.Scheuermeyer FX, Grafstein E, Rowe B, Cheyne J, Grunau B, Bradford A, et al. The clinical epidemiology and 30-day outcomes of emergency department patients with acute kidney injury. Canadian journal of kidney health and disease. 2017;4:2054358117703985. doi: 10.1177/2054358117703985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kellum JA, Lameire N, Aspelin P, Barsoum RS, Burdmann EA, Goldstein SL, et al. Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group KDIGO clinical practice guideline for acute kidney injury. Kidney international supplements. 2012;2(1):1–138. [Google Scholar]
- 4.Noritomi DT, Soriano FG, Kellum JA, Cappi SB, Biselli PJ, Libório AB, et al. Metabolic acidosis in patients with severe sepsis and septic shock: a longitudinal quantitative study. Critical care medicine. 2009;37(10):2733–9. doi: 10.1097/ccm.0b013e3181a59165. [DOI] [PubMed] [Google Scholar]
- 5.Stewart PA. Modern quantitative acid–base chemistry. Canadian journal of physiology and pharmacology. 1983;61(12):1444–61. doi: 10.1139/y83-207. [DOI] [PubMed] [Google Scholar]
- 6.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 7.Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Critical care medicine. 2006;34(5):1297–310. doi: 10.1097/01.CCM.0000215112.84523.F0. [DOI] [PubMed] [Google Scholar]
- 8.Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. Jama. 2015;313(8):837–46. doi: 10.1001/jama.2015.0602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hoste EA, Bagshaw SM, Bellomo R, Cely CM, Colman R, Cruz DN, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive care medicine. 2015;41(8):1411–23. doi: 10.1007/s00134-015-3934-7. [DOI] [PubMed] [Google Scholar]
- 10.Bouchard J, Acharya A, Cerda J, Maccariello ER, Madarasu RC, Tolwani AJ, et al. A prospective international multicenter study of AKI in the intensive care unit. Clinical Journal of the American Society of Nephrology. 2015;CJN:04360514. doi: 10.2215/CJN.04360514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Toyonaga Y, Kikura M. Hyperchloremic acidosis is associated with acute kidney injury after abdominal surgery. Nephrology. 2017;22(9):720–7. doi: 10.1111/nep.12840. [DOI] [PubMed] [Google Scholar]
- 12.Bockenkamp B, Vyas H. Understanding and managing acute fluid and electrolyte disturbances. Current Paediatrics. 2003;13(7):520–8. [Google Scholar]
- 13.Relman AS, Lennon EJ, Lemann J. Endogenous production of fixed acid and the measurement of the net balance of acid in normal subjects. The Journal of clinical investigation. 1961;40(9):1621–30. doi: 10.1172/JCI104384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Widmer B, Gerhardt RE, Harrington JT, Cohen JJ. Serum electrolyte and acid base composition: the influence of graded degrees of chronic renal failure. Archives of internal medicine. 1979;139(10):1099–102. [PubMed] [Google Scholar]
- 15.Wright G, Noiret L, Damink SWO, Jalan R. Interorgan ammonia metabolism in liver failure: the basis of current and future therapies. Liver International. 2011;31(2):163–75. doi: 10.1111/j.1478-3231.2010.02302.x. [DOI] [PubMed] [Google Scholar]