Abstract
Breast cancer is the leading cause of cancer-related death for women, and multidrug resistance (MDR) is the major obstacle faced by chemotherapy for breast cancer. We have previously synthesized a doxorubicin (DOX) derivative by conjugating DOX with triphenylphosphonium (TPP) to achieve mitochondrial delivery, which induced higher cytotoxicity in drug-resistant breast cancer cells than DOX itself. Due to its amphiphilicity, TPP-DOX is difficult to physically entrap in nanocarriers. Thus, we linked it to hyaluronic acid (HA) by a novel ionic bond utilizing the specific bromide ion of TPP to form supra-molecular self-assembled structures (HA-ionic-TPP-DOX). The product was analyzed uisng 1H-NMR, 13C-NMR and mass spectrometry. The HA nanocarriers (HA-ionic-TPP-DOX) were shown to self-assemble into spherical nanoparticles, and sensitive to acidic pH in terms of morphology and drug release. Compared with free DOX, HA-ionic-TPP-DOX produced much greater intracellular DOX accumulation and mitochondrial localization, leading to increased ROS production, slightly decreased mitochondrial membrane potential, increased cytotoxicity in MCF-7/ADR cells and enhanced tumor targeting in vivo. In xenotransplant zebrafish model with the MCF-7/ADR cell line, both TPP-DOX and HA-ionic-TPP-DOX inhibited tumor cell proliferation without inducing significant side effects compared with free DOX. In addition, we observed a better anti-tumor effect of HA-ionic-TPP-DOX on MCF-7/ADR cells in zebrafish than that of TPP-DOX treatment. Furthermore, HA-ionic-DOX-TPP exhibited favorable biocompatibility and anti-tumor effects in MCF-7/ADR tumor-bearing nude mice in comparison with the effects of TPP-DOX and DOX, suggesting the potential of HA-ionic-TPP-DOX for the targeted delivery and controlled release of TPP-DOX, which can lead to the sensitization of resistant breast tumors.
Keywords: breast cancer, doxorubicin, drug resistance, TPP-DOX, mitochondrial target, hyaluronic acid, ionic bond, nanocarriersl zebrafish
Introduction
Breast cancer is the most common type of cancer in women around the world, and chemotherapy is the major form of breast cancer therapy. However, the clinical benefits of chemotherapy are hampered by multidrug resistance (MDR). Several mechanisms may be involved in MDR, including the overexpression of efflux pumps such as P-glycoprotein (P-gp)1, decreased drug uptake, altered intracellular drug localization, enhanced repair of drug-induced DNA damage and hindered apoptotic pathways2.
To overcome the drug resistance of cancer, many approaches have been reported. In this context, perhaps the most researched target has been the overexpression of efflux transporters, an important mechanism for the resistance of breast cancer cells to common chemotherapy agents, such as doxorubicin and paclitaxel. Various nano-carriers have been developed to overcome efflux-mediated resistance either by evading the interaction of chemotherapeutic drugs with transporters or by co-delivering inhibitors of drug efflux pumps to tumors along with anti-cancer drugs. Some nano-carriers could simultaneously deliver genes3 that affect cellular MDR pathways, such as siBcl-24,5, siP-gp6,7, and sisurvivin8. Many chemotherapy drugs have targeted particular subcellular compartments. The accessibility of these subcellular drug targets to DOX may become limited in MDR cells. For example, the action of DOX in the cell nucleus leads to DNA damage by inhibiting topoisomerase enzymes9. However, MDR tumor cells will discharge DOX from the cell nucleus and minimize its access to topoisomerase enzymes. Mitochondria are another subcellular target of DOX. Mitochondria are essential intracellular organelles that ensure cell survival and regulate cell apoptosis10,11. Research has revealed a relationship between mitochondrial dysfunction and diseases such as cancer, Alzheimer's12, diabetes13, ischemia-reperfusion injury and many more. The delivery of chemotherapy drugs to the mitochondria can be achieved by taking advantage of the high membrane potential14 and protein import machinery or the mitochondria targeting sequence (MTS)15,16. It has been reported that lipophilic cations17 can readily cross mitochondrial membranes and accumulate within mitochondria. Triphenylphosphonium (TPP)18,19 has commonly been used for this purpose. For instance, TPP has been used to modify the surface of paclitaxel liposomes20 and to create triphenylphosphine-chitosan-graft-PEI-lonidamine/siRNA/poly(acrylic acid)-polyethylene glycol-folic acid nanoparticles21, CoQ10/poly(ethylene glycol)-polycaprolactone-triphenylphosphonium bromide micelles22, and G4-PAMAM–poly(ethylene glycol)-triphenylphosphonium23. However, the surface charges of nanoparticles that were modified by TPP were shown to be positive, resulting in off-target in vivo effects. In addition, the large particle size of these nanoparticles is disadvantageous for intracellular mitochondria targeting24.
Previously, we have reported on the development of a small molecular mitochondriotropic doxorubicin derivative (TPP-DOX25). To form that derivative, TPP is directly conjugated to DOX by an amide bond to achieve mitochondrial targeting. TPP-DOX was confirmed to target mitochondria and enhance the toxicity of DOX to MDA-MB-435/DOX-resistant cancer cells. In this study, we linked TPP-DOX to water-soluble HA by an ionic bond to form supra-molecular self-assembled structures (Figure 1). Meanwhile, an MCF-7/ADR-(CM-Dil) xenograft bearing zebrafish model was used to evaluate the in vivo anti-tumor activity of the HA-ionic-TPP-DOX due to the homology of the zebrafish genome to the human genome and of zebrafish tissues to comparable human tissue types26,27.
Figure 1.
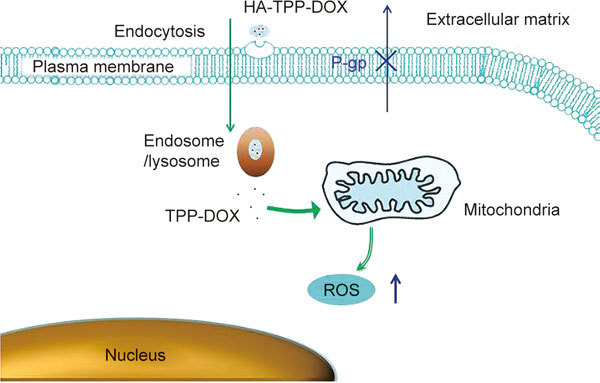
Proposed scheme for the interaction of HA-ionic-TPP-DOX (shown as HA-TPP-DOX) with MDR cancer cells.
Materials and methods
Materials
MCF-7/ADR cells were purchased from Nanjing KeyGen Biotech Co, Ltd (Nanjing, China). N-hydroxysuccinimide (NHS), N,N′-dicyclohexylcarbodiimide (DCC) and (3-carboxypropyl)triphenylphosphonium bromide (TPP) were purchased from Sigma-Aldrich (St Louis, MO). Silver nitrate was purchased from Aladdin (China). Doxorubicin hydrochlorid was obtained from Zhejiang Provincial People's Hospital (Zhejiang, China). Sodium salt hyaluronic acid (HA, Mw 48 kDa) was purchased from Zhengda Freda Co (Jinan, China). All other chemicals were of analytical grade.
Synthesis of TPP-DOX
The synthesis of TPP-DOX was carried out as described previously25. Briefly, TPP (9.3 mmol), DCC (12 mmol) and NHS (12 mmol) were dissolved in DMF (10 mL). The reaction mixture was stirred with a magnetic stirrer at room temperature for 3 h. Triethylamine (9.3 mmol) was added to a solution of DOX (9.3 mmol) in DMF(10 mL) and stirred for 0.5 h to alkalify DOX. Subsequently, the alkaline DOX solution was added dropwise to the activated TPP solution. This reaction was carried out at 0 °C for 45 min and then at room temperature overnight. The crude product was obtained by precipitation with a large amount of diethyl ether. The precipitate was dissolved in trichloromethane. After evaporation, it was extracted with deionized water to remove impurities. Finally, the product was purified on a silica gel plate (CHCl3/MeOH=4/1, 0.5% triethylamine).
Preparation of HA-ionic-TPP-DOX
TPP-DOX was conjugated to HA by using silver nitrate as an activating reagent. HA (35 mg) and silver nitrate (8 mg) were dissolved in distilled water (10 mL) with the pH adjusted to 7.5 and then reacted for 2 h to form HA-(COO-Ag+). After free Ag+ was removed from HA-(COO-Ag+) by dialysis against water, 10 mL of TPP-DOX solution (4 mg/mL) was added to the HA-(COO-Ag+) solution dropwise. HA-ionic-TPP-DOX was obtained after insoluble silver bromide formed by the reaction between bromide ion in TPP-DOX and Ag+ in HA-(COO-Ag+) was removed by high-speed centrifugation (15 000 r/min, 10 min). After the reaction proceeded with stirring overnight, the solution was poured into a dialysis bag (MWCO 8000–14000) and dialyzed against a large excess amount of deionized water to remove impurities, and then, the product in the dialysis bag was collected.
The product was analyzed by mass spectrometry (Agilent 1290 HPLC-6224 Time-of-Flight Mass Spectrometer) and 1H and 13C nuclear magnetic resonance (NMR) (Bruker AVIII500M, USA). D2O was purchased from Tenglong Weibo Technology Co, Ltd (Qingdao, China) as an NMR solvent.
Particle size and transmission electron microscopy (TEM)
The particle size and zeta potential were measured by using a Zetasizer Nano-S90 (Malvern Instruments, Ltd, UK). To investigate the role of TPP-DOX in the self-assembly behavior of HA-ionic-TPP-DOX, the morphologies of HA-ionic-TPP-DOX were observed by transmission electron microscopy (JEM1200EX, Japan) after dialysis against excess PBS (pH 4.0) to remove TPP-DOX.
In vitro release studies
Release experiments were performed at pH 7.4 and pH 5.0. For each release study, 0.2 mg of HA-ionic-TPP-DOX was added to 1 mL of H2O, and the solution was placed in a dialysis tube (MWCO: 8000–14000 Da). Then, the dialysis tube was immersed directly in 25 mL of 0.2 mol/L phosphate buffer solution (pH=7.4 or 5.0) and shaken at 37 °C in a thermostatic oscillator. The concentration of the released TPP-DOX from HA-ionic-TPP-DOX was determined on the basis of the fluorescence intensity at 570 nm in reference to the standard calibration curve.
Cell culture
MCF-7/ADR cells were cultured in RPMI-1640 medium supplemented with 100 U/mL penicillin, 100 mg/mL streptomycin, and 10% fetal bovine serum (Gibco Life Technologies Co., Carlsbad, USA ) at 37 °C in a humidified 5% CO2 incubator (HF151UV, Heal Force, HK).
Uptake of and DOX
MCF-7/ADR cells were seeded into 6-well plates at a density of 106 cells/well. After 24 h, the cells were incubated with free DOX solution, TPP-DOX or HA-ionic-TPP-DOX in RPMI-1640 medium for 1 h at equivalent DOX concentrations (8.6 and 17.2 μmol/L). The cells were then washed twice with ice-cold PBS, digested with trypsin and finally examined by flow cytometric analysis (FC500MCL, Beckman Coulter, USA) to determine DOX uptake.
Cytotoxicity assay in vitro
The in vitro cytotoxicity was evaluated by the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. Briefly, MCF-7/ADR cells were seeded at a density of 5000 cells/well into 96-well culture plates and cultured for 24 h. Cells were then exposed to various concentrations of free DOX, TPP-DOX or HA-ionic-TPP-DOX. Untreated cells were used as blank controls.
After incubation for 48 h, the medium was exchanged with fresh culture medium containing MTT solution (0.5 mg/mL), and incubation was continued at 37 °C for 4 h. Then, the medium was discarded, and DMSO was added to dissolve the formazan crystals formed by living cells. The absorbance was measured at 570 nm with a microplate reader. Finally, the relative cell viability was calculated as follows: cell viability(%)=(OD 570 samples-OD 570 blank)/(OD 570 control-OD 570 blank)×100.
Assessment of mitochondrial targeting by confocal laser scanning microscopy (CLSM)
A confocal laser scanning fluorescence microscope (Nikon, Japan) was used to observe the co-localization of DOX in mitochondria. Briefly, MCF-7/ADR cells were seeded into glass-bottomed dishes at a density of 2×105 cells/well and cultured for 24 h. After 24 h of incubation, the cells were treated with free DOX, TPP-DOX solution and HA-ionic-TPP-DOX and further cultured for 4 h under the same conditions. The final concentration of DOX was 8.6 μmol/L. After the incubation, the cells were washed twice with cold PBS and stained with Hoechst 33342 (Life Technologies Co, Carlsbad, CA, USA) for 20 min, then stained with Mito-tracker Green FM (Life Technologies Co. Carlsbad, CA, USA) for 40 min. The concentration of Mito-tracker was 140 nmol/L. The cells were washed twice with PBS and observed by confocal microscopy. Composite images were made by overlapping the images of the individual channels.
Reactive oxygen species (ROS) measurements
Intracellular ROS production was measured by using the Reactive Oxygen Species Assay Kit (Beyotime Biotech Co, Ltd, Shanghai, China). After treatment with 8.6 μmol/L of free DOX, TPP-DOX solution or HA-ionic-TPP-DOX for different times (4 h, 12 h, 24 h), the cells were washed twice with PBS and then loaded with DCFH-DA in serum-free medium and incubated at 37 °C for 20 min. The ROS production of the MCF-7/ADR cells was evaluated by using a flow cytometer (FC500MCL, Beckman Coulter, USA).
Measurement of mitochondrial membrane potential
The changes in mitochondrial membrane potential after incubation with free DOX, TPP-DOX solution and HA-ionic-TPP-DOX at an equivalent 3 μg/mL DOX concentration were evaluated by a Mitochondrial Membrane Potential Assay Kit with JC-1 (Beyotime Biotech Co, Ltd, Shanghai, China), which contained JC-1 dye specific to mitochondria and able to indicate the mitochondrial membrane potential by the fluorescent ratio of green and red colors. After incubation for 24 h, the cells were washed and stained with freshly prepared JC-1 at 37 °C for 20 min in the dark, according to the manufacturer's protocol. Then, the cells were collected and evaluated by flow cytometry.
Biodistribution
To investigate the distribution and tumor accumulation ability of the HA-ionic-TPP-DOX, nude female mice (4 weeks old) were administered a subcutaneous injection of 0.1 mL of MCF-7/ADR cancer cell suspension containing 7×106 cells. After the tumors had grown to 100 cm3, the nude mice were intravenously injected with free DOX, TPP-DOX or HA-ionic-TPP-DOX individually (equivalent DOX, 5 mg/kg). The mice were euthanized at 48 h, and the tumor and organs (heart, liver, spleen, lung, and kidney) were harvested and then imaged with the MaestroTM in vivo imaging system (Cambridge Research and Instrumentation, USA). Meanwhile, tumor slices (5 μm) were cut after freezing in OCT medium for the further determination of DOX localization in tumors by fluorescence microscopy. All care and handling of animals was performed according to the guidelines of the Animal Ethics Committee of Zhejiang University (HangZhou, China).
Anti-tumor activities in transgenic zebrafish models
The transgenic zebrafish model is widely used for drug evaluation and to investigate the anti-tumor activity of drugs in the xenograft tumor model. Tg(fli1a:eGFP)+/− transgenic zebrafish were raised by standard methods27. Fertilization was performed by photo induced spawning over green plants and culturing at 28.5 °C in filtered tap water.
MCF-7/ADR cells labeled with the red fluorescent dye CM-DiI were used in the zebrafish tumor xenograft model to allow the observation of anti-tumor effects. In brief, MCF-7/ADR cells were incubated with CM-DiI for 4 min at 37 °C, followed by 15 min at 4 °C, then centrifuged and rinsed to remove unincorporated dye. Then, 200 trypsinized MCF-7/ADR cells were injected into the perivitelline space of dechorionized 48 hpf tg(fli1a:eGFP)+/− transgenic zebrafish by a standard micro-injection method after the zebrafish had been anaesthetized with 1.85 mmol/L tricaine. After implantation, the zebrafish were maintained at 33°C in Holt-Buffer solution (60 mmol/L NaCl, 2.4 mmol/L NaHCO3, 0.9 mmol/L CaCl2, 0.67 mmol/L KCl). At 24 h after implantation, 1 nL of free DOX, TPP-DOX or HA-ionic-TPP-DOX was injected into the zebrafish at an equivalent DOX concentration of 1 mg/mL.
At 4 days post-inoculation (4 dpi), the zebrafish were anaesthetized with 0.62 mmol/L tricaine and then imaged by a camera (Nikon DS-Ri1)) with a microscope system (Nikon SMZ18) for live imaging. All experimental procedures were conducted in compliance with the directives of the animal welfare committee of Zhejiang University.
In vivo anti-tumor assays in mouse model
Nude female BALB/c mice (4 weeks old) received a subcutaneous injection of 0.1 mL of MCF-7/ADR cancer cell suspension containing 107 cells in the right forelimb. When the tumor volume was greater than 50 mm3, the tumor-bearing mice were intravenously administered saline, DOX solution, TPP-DOX or HA-ionic-TPP-DOX (equivalent DOX dose, 4 mg/kg) every 2 days. Each group contained six mice. After treatment, the body weight and tumor dimensions were recorded. The tumor volume was calculated using the equation volume=(width2×length)/2. After the end of the experiment, the tumor tissues of the nude mice were taken and fixed for 48 h in 4% formaldehyde solution in paraffin sections and detected by TUNEL immunohistochemical staining.
Statistics
Data represent the mean and standard deviation in each experiment, repeated at least three times. Differences between the mean values were analyzed by the two-sided unpaired Student's t test or one-way ANOVA, and results were considered statistically significant at P<0.05.
Results and discussion
MASS and NMR spectra
The structural characterization of TPP-DOX and HA-ionic-TPP-DOX were confirmed by 1H NMR in D2O. The signals ranging from 7.5 to 8.0 ppm (d) belong to the protons of the phenyl rings of TPP (Figure 2A), and the peaks at 3.2 ppm (c), 2.5 ppm (a) and 1.9 ppm (b) were attributed to the CH2CH 2P, CH2CH 2COOH and CH2CH 2CH2 protons of TPP, respectively. For DOX (Figure 2B), the peaks at 1.2 ppm (f') and 4.8 ppm (c') were attributed to CH 3 and OCHO in daunosamine, and the peaks at 3.6 ppm (e'), 3.8 ppm (d'), 7.3–7.6 ppm (a', b') belonged to the signals of COCH 2OH, OCH 3, and aromatic protons in naphthacenequinone, respectively. For HA, the peaks at 1.9 ppm (n) and 3.2–4.5 ppm (m) correspond to the methyl group (NHCOCH 3) and the methenyl group (Figure 2C). The peaks for aromatic protons in TPP and DOX were also observed in TPP-DOX 1H NMR, ranging from 7.0 to 8.0 ppm (Figure 2D), which proved the formation of the TPP-DOX conjugate.
Figure 2.
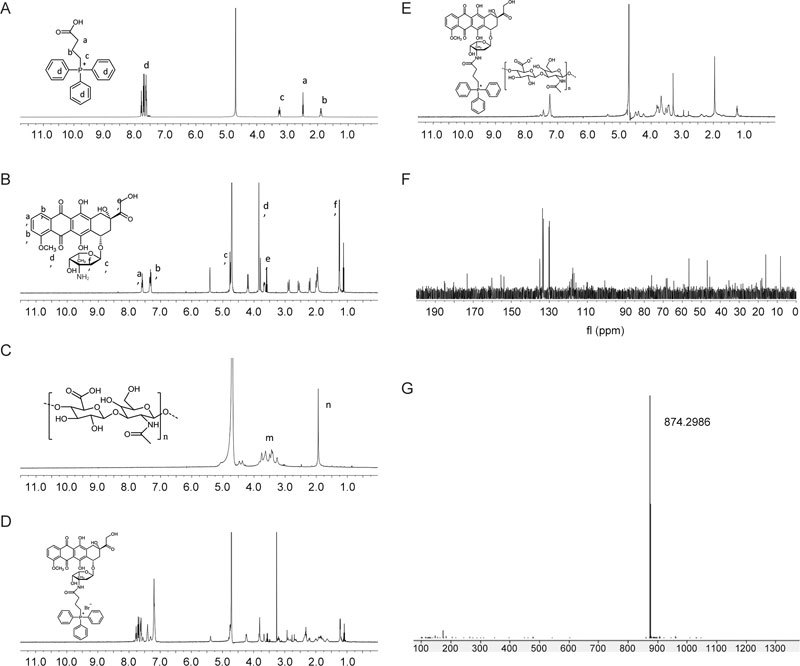
1H nuclear magnetic resonance (1H-NMR) spectra of TPP (A), DOX (B), HA (C), TPP-DOX (D), and HA-ionic-TPP-DOX (E). 13C nuclear magnetic resonance (13C-NMR) (F) and mass spectrometry (G) of TPP-DOX.
The peaks for the aromatic protons (7.0–7.6 ppm) and the methyl group (1.2 ppm) in TPP-DOX, together with the characteristic peaks of HA, were observed in HA-ionic-TPP-DOX 1H NMR (Figure 2E), which proved the conjugation between HA and TPP-DOX. The 13C NMR spectra confirmed the aromatic peaks ranging from 120 to 140 ppm related to TPP and the DOX carbons of aromatic rings (Figure 2F), and mass spectrometry was also used to confirm the structure of TPP-DOX with a molecular weight of 874 (Figure 2G).
Particle size and TEM analysis of HA-ionic-TPP-DOX
The morphology of HA-ionic-DOX-TPP is spheroidal and monodisperse (PDI=0.096) in water with an average particle size of 257 nm (Figure 3A) and a zeta potential of -24.1 mV (Figure 3B). Our further study proved that HA-ionic-DOX-TPP could self-assemble into a spherical structure with TPP-DOX as its hydrophobic kernel. In a pH 4.0 dialysis solution, the TPP-DOX electrostatically adhering to HA was replaced by hydrogen ions, resulting in changes to the structure. After losing its hydrophobic TPP-DOX kernel, the spherical structure became hydrophilic long chains intertwining with each other in the water with an average size of 490 nm (Figure 3C) and a zeta potential of -21.6 mV (Figure 3D). Thus, the structure formed by HA-ionic-TPP-DOX was stable and conducive to intravenous injection. Taking advantage of the long-term systemic circulation of HA and the selectivity of HA for tumors that over-express CD44, TPP-DOX was more effectively transferred into tumor tissues.
Figure 3.
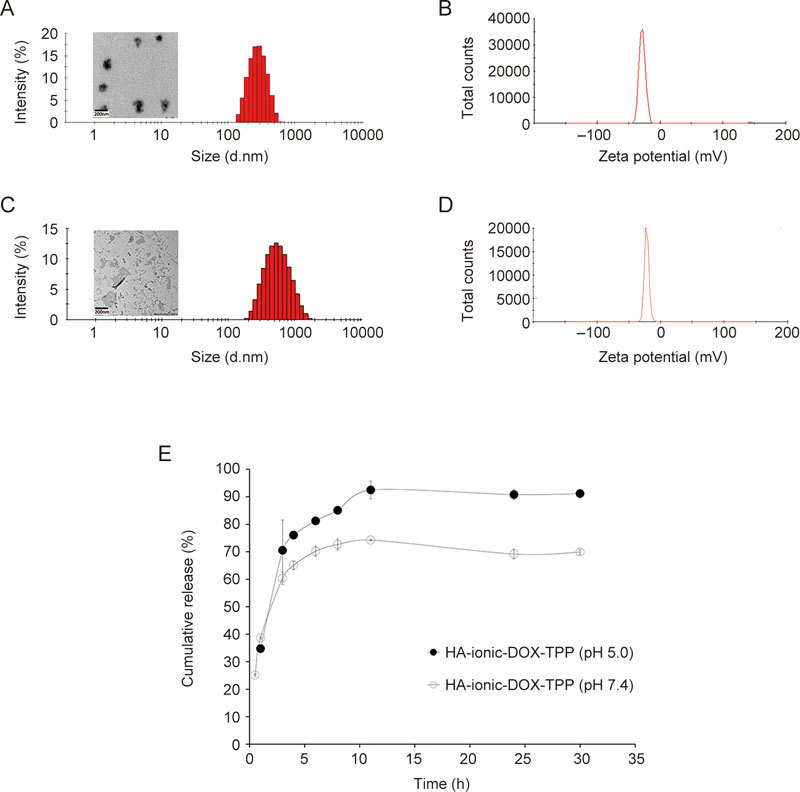
Characterization of HA-ionic-TPP-DOX. The morphology was observed under a transmission electron microscope (TEM), and the particle size was determined by dynamic light scattering (DLS) (A), together with the zeta potential of HA-ionic-TPP-DOX (B). After HA-ionic-TPP-DOX was dialyzed against excess PBS (pH 4.0) to remove TPP-DOX, its morphology and particle size (C), and zeta potential (D) were observed again. Meanwhile, In vitro release profiles of TPP-DOX from HA-ionic-TPP-DOX in the release media at pH 7.4 or 5.0 (E).
In vitro release
The content of TPP-DOX within the HA-ionic-TPP-DOX carrier was measured to be 31.4%, and the solubility of TPP-DOX was 33.87 mg/mL in water and 113.96 mg/mL in chloroform, which suggested that TPP-DOX was amphiphilic. There, it was difficult to entrap physically. Silver nitrate could react with the carboxyl group in HA to produce silver carbonate, and then the bromide ion in TPP-DOX could substitute the silver ion of silver carbonate in HA, leading to the precipitation of silver bromide. Consequently, TPP-DOX was conjugated to the carboxyl group of HA by an ionic bond, which could improve the drug loading and stability of the preparation.
To test the release characteristics of TPP-DOX from the HA nano-complex, dialysis was used28. In addition, HA-CDDP formed by ionic interaction has been reported to show a pH-sensitive release profile29. Therefore, the TPP-DOX release profile was evaluated in phosphate buffer with different pH values: pH 5.0 and 7.4 were used to simulate the endosomal acidic pH and physiological pH, respectively. The HA-ionic-DOX-TPP exhibited faster release at pH 5.0 than at pH 7.4. At 30 h, 91% of TPP-DOX was released at pH 5.0, while only 69% was released at pH 7.4. The pK a value of HA is approximately 3.030. Both curves showed a burst release of TPP-DOX of up to 25% at pH 5.0 and 34% at pH 7.4 in 0.5 h, reflecting that TPP-DOX could adsorb onto the surface of HA by electrostatic interaction (Figure 3E).
Cell uptake of DOX
The cell uptake was measured by flow cytometric analysis (Figure 4). The cell uptake levels of both TPP-DOX and HA-ionic-TPP-DOX were significantly higher than that of free DOX, which might be because the modification of DOX with TPP results in the avoidance of P-gp recognition and efflux. Furthermore, TPP-DOX showed the highest cell uptake, and the positive charge of TPP-DOX may contribute to its cell uptake and subsequent cytotoxicity.
Figure 4.
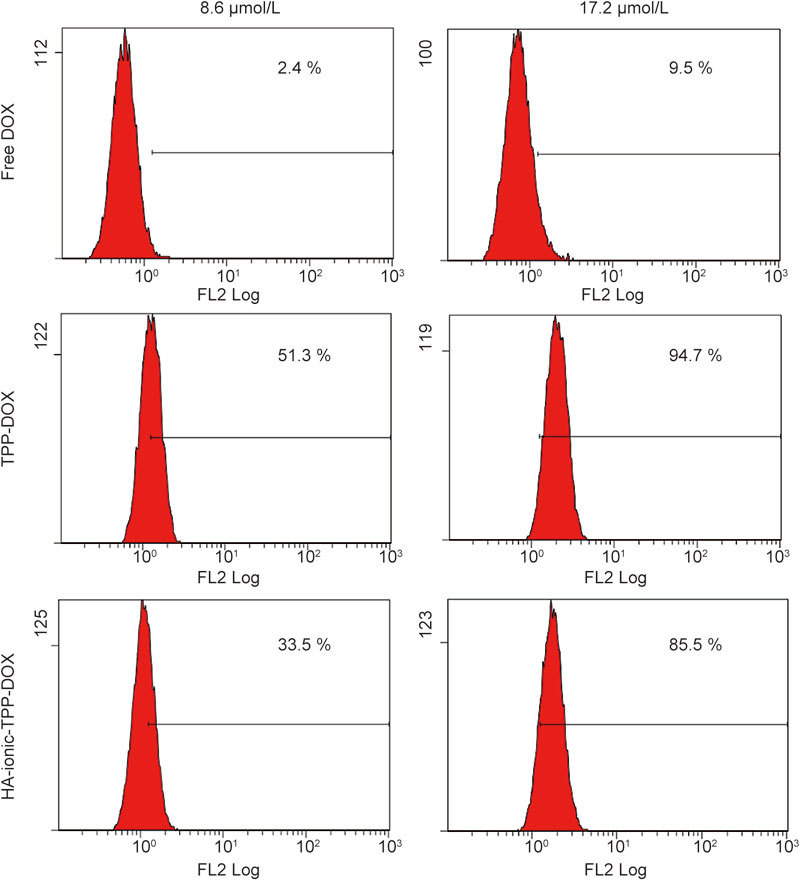
Cellular uptake of HA-ionic-TPP-DOX into MCF-7/ADR cells. MCF-7/ADR cells were seeded into 6-well plates at a density of 1×105 cells/well and cultured for 24 h, then incubated with free DOX, TPP-DOX, or HA-ionic-TPP-DOX for 1 h at equivalent DOX concentrations. The cells were then washed twice with ice-cold PBS, digested with trypsin and finally examined by flow cytometric analysis (FC500MCL, Beckman Coulter, USA) to determine the DOX uptake.
Cytotoxicity assay in vitro
The cytotoxicity levels of free DOX, TPP-DOX, and HA-ionic-TPP-DOX were estimated in MCF-7/ADR cells for 48 h. Figure 5 illustrated that all three showed concentration-dependent toxicity. TPP-DOX showed much higher toxicity than free DOX: the IC50 of TPP-DOX was 4.87 μmol/L, which was far less than the IC50 of free DOX (80.6 μmol/L). The high toxicity of TPP-DOX was attributed to inducing apoptosis by achieving mitochondrial co-location. In addition, another reason may be that TPP-DOX was positively charged, which could enhance the cell uptake. The IC50 of HA-ionic-TPP-DOX (57.7 μmol/L) was slightly lower that of free DOX but much higher than that of TPP-DOX. It is also reported that the HA nano-complex could prolong circulation in the blood and increase the drug distribution in tumors by the enhanced permeability and retention (EPR) effect7.
Figure 5.
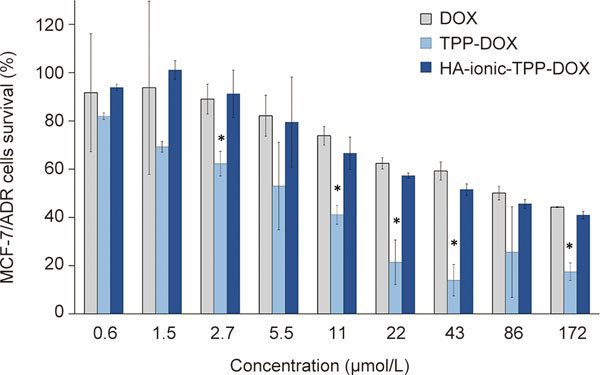
Cytotoxicity of DOX, TPP-DOX, and HA-ionic-TPP-DOX in drug-resistant MCF-7/ADR cells in vitro. * P<0.05 represents a significant difference from the DOX group.
Assessment of mitochondrial targeting by confocal laser scanning microscopy (CLSM)
The intracellular distribution of DOX was observed by confocal laser scanning microscopy. After 1 h of incubation, little DOX could be observed in MCF-7/ADR cells as a result of the drug-resistance of the tumor cells, while much more TPP-DOX and HA-ionic-TPP-DOX could accumulate in the cells, which is consistent with the cell uptake results mentioned above. However, none of them could be localized in the mitochondria, as the 1 h incubation time is not sufficient for transport to the mitochondria (Figure 6A).
Figure 6.

Intracellular distributions of DOX, TPP−DOX and HA-ionic-TPP-DOX in MCF-7/ADR cells. Cells were exposed to DOX, TPP−DOX or HA-ionic-TPP-DOX solution at 37 °C for 1 h (A) and 4 h (B), and the mitochondria were stained with Mito-tracker Green FM, while the nuclei were stained with Hoechst 33342. The overlay between the fluorescence of TPP-DOX (red) and Mito-tracker (green) appears as yellow.
The confocal fluorescence images of MCF-7/ADR cells incubated with free DOX, TPP-DOX and HA-ionic-TPP-DOX for 4 h are illustrated (Figure 6B). Bright yellow fluorescence, a combination of red and green fluorescence, was used to indicate the co-localization of DOX with the mitochondria. According to the images, both TPP-DOX and HA-ionic-TPP-DOX exhibited punctate distribution, indicating that both TPP-DOX and HA-ionic-TPP-DOX selectively accumulated in the mitochondria of MCF-7/ADR cells. However, after the addition of free DOX solution, no bright yellow fluorescence could be observed. Free DOX seemed to be localized in the form of dots, perhaps indicating its sequestration in endosomes in the MCF/7 ADR cells, while TPP-DOX and HA-ionic-TPP-DOX were more evenly distributed in the cells. The CSLM images show that the TPP-DOX released from HA-ionic-TPP-DOX might have been able to target mitochondria. Many studies have reported that the surface modification of nanoparticles with TPP or MTS led to a tendency to accumulate in the mitochondria. However, because the size of these nanoparticles ranges from 50 nm to 200 nm31,32,33, they were too large to target the mitochondria because of obstruction by the components of the cytoplasm. Meanwhile, the molecular weight of TPP-DOX is only 874 Da, which is smaller and allows more flexible movement in the cytoplasm.
Reactive oxygen species (ROS) measurements
Reactive oxygen species (ROS) play an important role in the induction of apoptosis under both physiological and pathological conditions. Interestingly, mitochondria are both the source and target of ROS, which can be harmful to the cell if produced excessively. Cytochrome c is released from mitochondria and triggers caspase activation. It appears to be largely mediated by direct or indirect ROS action34.
DOX, TPP-DOX and HA-ionic-TPP-DOX showed no difference in the production of ROS from MCF/ADR cells after exposure for 4 h. However, when the incubation time was increased to 12 h, the ROS production of TPP-DOX was significantly increased and continued increasing with time until 24 h). Compared with that of free DOX, the ROS production of TPP-DOX was twice as high after 12 h, and four times as high after 24 h. HA-ionic-TPP-DOX could induce five times as much ROS production in cells as free DOX at the 24 h incubation time point (Figure 7).
Figure 7.
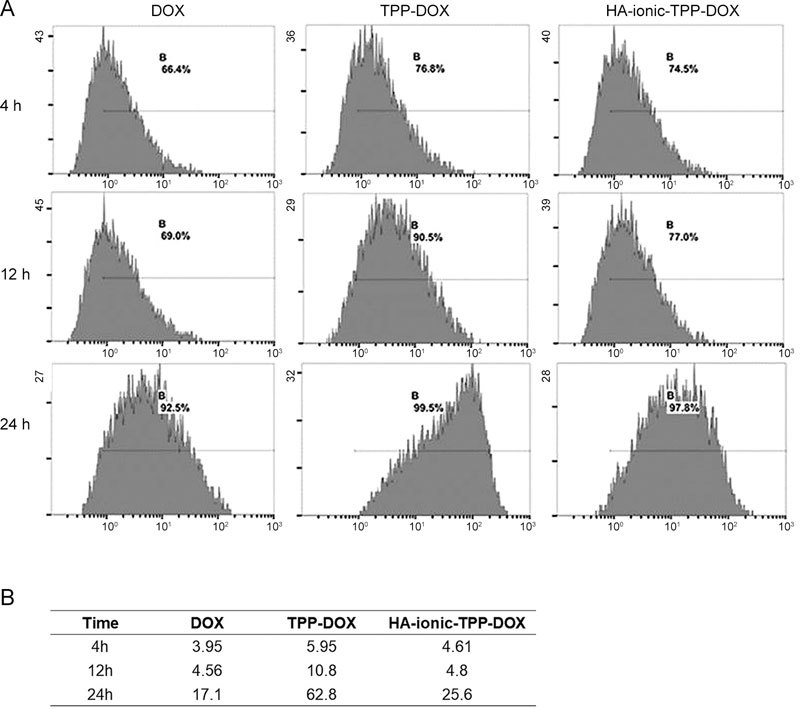
Effects of DOX, TPP-DOX and HA-ionic-TPP-DOX on ROS production in MCF-7/ADR cells. MCF-7/ADR cells were treated with DOX,TPP-DOX and HA-ionic-TPP-DOX at a DOX concentration of 8.6 μmol/L and then stained with H2DCF-DA at different intervals, followed by flow cytometry analysis. The image is shown in (A) and the fluorescence value in (B). Normal MCF-7/ADR cells without treatment served as controls.
Evaluation of mitochondrial membrane integrity by JC-1 uptake
To test whether the uptake of TPP-DOX and HA-ionic-TPP-DOX into mitochondria could alter the mitochondrial membrane potential, JC-1 was used as an indicator of mitochondrial membrane potential change in MCF-7/ADR cells. The results showed that TPP-DOX had a significant impact on the mitochondrial membrane potential after incubation for 24 h (Figure 8). Compared with those of free DOX and HA-ionic-TPP-DOX, the JC-1 monomer/aggregate values were higher for TPP-DOX, reflecting the rapid accumulation of TPP-DOX in mitochondria. HA-ionic-TPP-DOX showed a suboptimal effect in decreasing the mitochondrial membrane potential (Figure 8).
Figure 8.
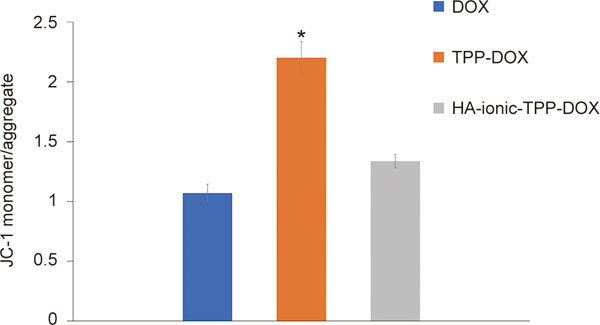
Effects of DOX, TPP-DOX and HA-ionic-TPP-DOX on the mitochondrial membrane potential of MCF-7/ADR cells. MCF-7/ADR cells were treated with 3 μg/mL equivalent concentrations of doxorubicin for 24 h and then stained with JC-1, followed by flow cytometry analysis. The height of the column shows the ratio of JC-1 aggregates and JC-1 monomer in the mitochondrial membrane and cytoplasm, and * P<0.05 represents a significant difference from the MCF-7/ADR cells treated with DOX solution.
In vivo distribution
The distributions of DOX solution, TPP-DOX solution and HA-ionic-TPP-DOX group were assessed after intravenous administration (Figure 9).
Figure 9.
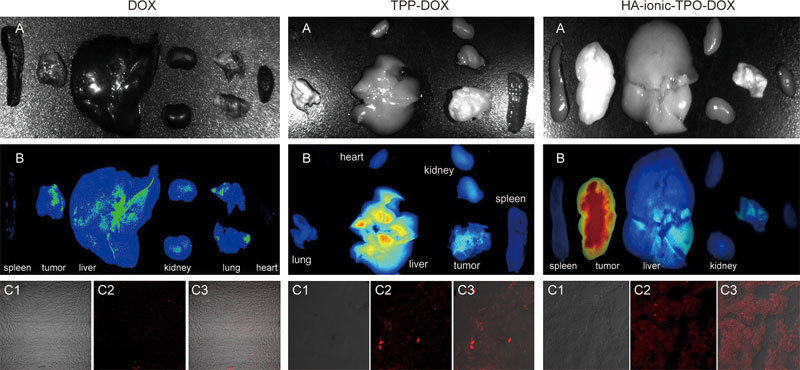
Distribution of DOX, TPP-DOX and HA-ionic-TPP-DOX in nude mice bearing MCF-7/ADR tumors. After the intravenous administration of free DOX solution, TPP-DOX and HA-ionic-TPP-DOX (4 mg/kg) for 24 h, nude mice bearing MCF-7/ADR tumors were sacrificed, and the major organs were collected and DOX fluorescence was observed by the in vivo imaging system (A, B). Furthermore, frozen sections of tumors were harvested, followed by observation by confocal laser scanning microscopy (OLYMPUS IX83-FV3000-OSR, Japan) to evaluate the accumulation of DOX (C2, red fluorescence) in the tumors. The sections observed under visible light (C1) were used as controls and overlapped with the DOX fluorescence (C3).
Compared with TPP-DOX and HA-ionic-TPP-DOX groups, little DOX could be observed in the tumor and organs in the DOX group after 24 h intravenous administration, suggesting the rapid elimination and off-target effects of free DOX.
Many tumor cells over-express HA-binding receptors such as CD44, and correspondingly, nano-carriers based on HA, in addition to the enhanced permeability and retention (EPR) effect, may be responsible for the stronger DOX fluorescence at both ex vivo tumor sites and in vitro tumor slices in the HA-ionic-TPP-DOX group than in the TPP-DOX solution group) in the nude mouse model bearing MCF-7/ADR tumors. The tumor-targeting property of HA-ionic-TPP-DOX would be favorable for in vivo therapy.
In vivo anti-tumor assays in a Tg(fli1a:eGFP)+/− transgenic zebrafish model
To investigate the toxicity of DOX toward MCF-7/ADR cells in vivo, a zebrafish xenograft experiment was employed because it offers a rapid and efficient approach for assessing drug effects on human cancer cells at various stages of tumorigenesis, resulting from its in vivo visualization of cell migration and cell mass formation and the interaction between human cancer and zebrafish cells in the transparent animal under microscopic observation35,36. Therefore, MCF-7/ADR cells were labeled with a fluorescent tracking dye (CM-DiI) and injected into the zebrafish perivitelline space, whereupon they proliferated and formed masses primarily in the regions surrounding the intestine, pancreas and liver (1 dpi). After drug treatment for three days (4 dpi), anti-tumor effects were observed in the free DOX, TPP-DOX and HA-ionic-TPP-DOX groups, in contrast to the control group, which had not been treated with the drug. Solid tumors formed in the control and free DOX groups, whereas tumor growth was significantly inhibited in both the TPP-DOX and the HA-ionic-TPP-DOX groups (Figure 10A). In addition, HA-ionic-TPP-DOX resulted in the most significant inhibition of tumor growth, which may be due to the targeted delivery and controlled release of HA-ionic-TPP-DOX (Figure 10A). Therefore, HA-ionic-TPP-DOX suppressed tumor growth in the MCF-7/ADR tumor model more effectively than free DOX and TPP-DOX.
Figure 10.
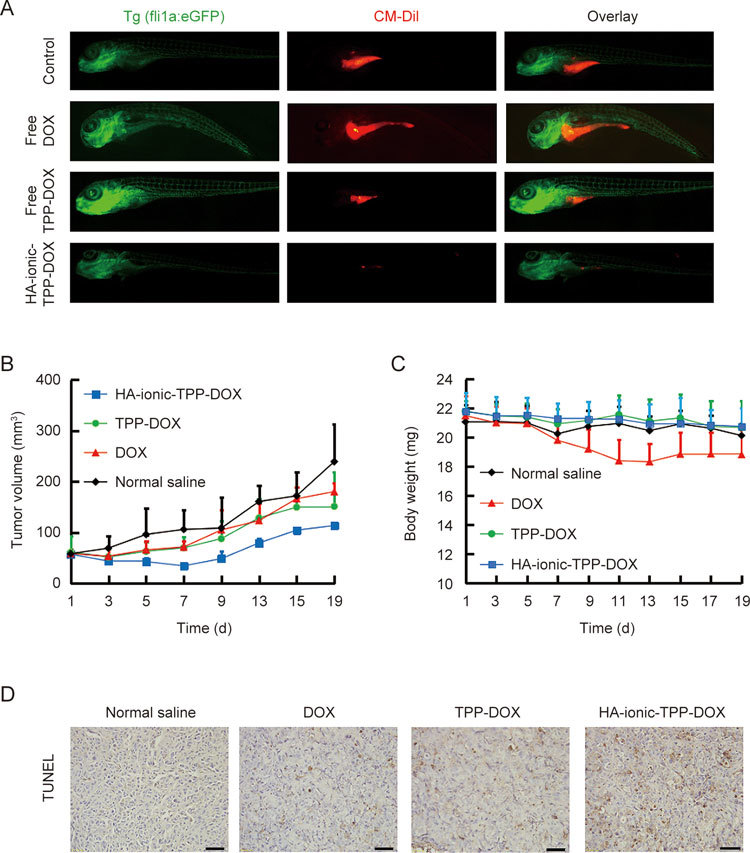
Images showing the anti-tumor effects of free DOX, TPP-DOX and HA-ionic-TPP-DOX in the tg(fli1a:eGFP)+/− transgenic zebrafish MCF-7/ADR tumor model (A). MCF-7/ADR cells were injected into the perivitelline space of dechorionized 48 hpf zebrafish. After 24 h, 1 nL of free DOX or HA-ionic-TPP-DOX was injected into the zebrafish at an equivalent DOX at concentration of 1 mg/mL. The zebrafish were imaged at 4 days post-inoculation (4 dpi), and green and red indicate vasculature and cancer cells, respectively (n=20). Tumor volume (B), body weight (C), and apoptosis (D) of nude mice after free DOX, TPP-DOX and HA-ionic-TPP-DOX treatment.
Meanwhile, the morphology of the zebrafish was imaged by fluorescence microscopy, and a clearly increased ventricle volume, together with body distortion, could be observed in the DOX solution group, indicating cardiotoxicity mediated by DOX. Meanwhile, HA-ionic-TPP-DOX may decrease the side effects, i.e., cardiotoxicity, as no significant difference in the ventricle volume and morphology of zebrafish resulted from the sustained release of the drug.
Anti-tumor effect in vivo
The tumor volumes and body weights were recorded to evaluate the in vivo anti-tumor efficacy of HA-ionic-DOX-TPP in nude mice bearing MCF-7/ADR tumors (Figure 10B,C). Tumors in mice receiving HA-ionic-DOX-TPP grew to 113.4 mm3 and were smaller than those in mice that received free DOX solution (180.1 mm3) or TPP-DOX solution (151.1 mm3), while the tumor volume was as large as 239.1 mm3 in the control group (saline group), demonstrating that HA-ionic-DOX-TPP exhibited a favorable anti-tumor effect in vivo. In addition, the body weights decreased in the free DOX group, while no significant decrease in body weights was observed for other treatments. In addition, immunohistochemical staining was performed by the TUNEL assay to investigate the apoptosis at the tumor site. TUNEL is widely used in the detection of apoptosis because it reflects the breakdown of DNA in cells. In TUNEL immunohistochemistry, the nuclei of the apoptotic cells were stained brown, and the HA-ionic-TPP-DOX group had more apoptotic cells than the DOX group ((Figure 10D).
Conclusion
In this study, TPP-DOX was conjugated by an ionic bond to the water-soluble polysaccharide HA, which has good biocompatibility and tumor targeting ability, as a framework material to form spherical nanoparticles by self-assembly. HA on the surface of the nanoparticle prolonged the circulation time in the blood and achieved tumor targeting by the CD44 receptor while bearing TPP-DOX in the core hydrophobic region. The suitable particle size and surface negative charge of HA-ionic-DOX-TPP was also beneficial for bio-distribution in the tumor by the EPR effect. The small molecule TPP-DOX exhibited excellent ability to target the mitochondria, compared with that of traditional TPP-modified nanoparticles. The cytotoxicity of HA-ionic-TPP-DOX was slightly better than that of free DOX, and it significantly inhibited tumor growth and prolonged the survival of tumor-bearing zebrafish compared with free DOX, suggesting potential prospects for in vivo use in the future.
Author contribution
Min HAN and Jian-qing GAO designed research; Hui-Na LIU, Ning-ning GUO, Wang-wei GUO, and Ming-yi HUANG-FU performed research; Wang-wei GUO, Ming-yi HUANG-FU, and Mohammad REZA VAKILI contributed new analyical tools and reagents; Jie-jian CHEN, Wen-hong XU, and Qi-chun WEI analyzed data; Hui-na LIU and Afsaneh LAVASANIFAR wrote the paper.
Acknowledgements
This study was supported by the National Basic Research Program of China (No 2014CB931901), the National Natural Science Foundation of China (No 81373346, 81102392, 81572952, 81673022), the Zhejiang Provincial Natural Science Foundation of China (No LY15H300001), the Fundamental Research Funds for the Central Universities (No 2017XZZX011-04), the Zhejiang Medical and Health Science and Technology Plan Project (No 2016KYB109), and the Zhejiang Provincial Natural Science Foundation of China (No LY17H160013).
Contributor Information
Min Han, Email: hanmin@zju.edu.cn.
Afsaneh Lavasanifar, Email: afsaneh@ualberta.ca.
References
- 1.Higgins CF. Multiple molecular mechanisms for multidrug resistance transporters. Nature. 2007;446:749–57. doi: 10.1038/nature05630. [DOI] [PubMed] [Google Scholar]
- 2.Kapse-Mistry S, Govender T, Srivastava R, Yergeri M. Nanodrug delivery in reversing multidrug resistance in cancer cells. Front Pharmacol. 2014;5:159. doi: 10.3389/fphar.2014.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giljohann DA, Seferos DS, Prigodich AE, Patel PC, Mirkin CA. Gene regulation with polyvalent siRNA-nanoparticle conjugates. J Am Chem Soc. 2009;131:2072–3. doi: 10.1021/ja808719p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.He C, Liu D, Lin W. Self-assembled nanoscale coordination polymers carrying siRNAs and cisplatin for effective treatment of resistant ovarian cancer. Biomaterials. 2015;36:124–33. doi: 10.1016/j.biomaterials.2014.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakamura K, Abu Lila AS, Matsunaga M, Doi Y, Ishida T, Kiwada H. A double-modulation strategy in cancer treatment with a chemotherapeutic agent and siRNA. Mol Ther. 2011;19:2040–7. doi: 10.1038/mt.2011.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Creixell M, Peppas NA. Co-delivery of siRNA and therapeutic agents using nanocarriers to overcome cancer resistance. Nano Today. 2012;7:367–79. doi: 10.1016/j.nantod.2012.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen K, Emmanuel R, Kisin-Finfer E, Shabat D, Peer D. Modulation of drug resistance in ovarian adenocarcinoma using chemotherapy entrapped in hyaluronan-grafted nanoparticle clusters. Acs Nano. 2014;8:2183–95. doi: 10.1021/nn500205b. [DOI] [PubMed] [Google Scholar]
- 8.He CB, Poon C, Chan C, Yamada SD, Lin WB. Nanoscale coordination polymers codeliver chemotherapeutics and sirnas to eradicate tumors of cisplatin-resistant ovarian cancer. J Am Chem Society. 2016;138:6010–9. doi: 10.1021/jacs.6b02486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gewirtz DA. A critical evaluation of the mechanisms of action proposed for the antitumor effects of the anthracycline antibiotics Adriamycin and daunorubicin. Biochem Pharmacol. 1999;57:727–41. doi: 10.1016/S0006-2952(98)00307-4. [DOI] [PubMed] [Google Scholar]
- 10.Green DR, Reed JC. Mitochondria and apoptosis. Science. 1998;281:1309–12. doi: 10.1126/science.281.5381.1309. [DOI] [PubMed] [Google Scholar]
- 11.Gulbins E, Dreschers S, Bock J. Role of mitochondria in apoptosis. Exp Physiol. 2003;88:85–90. doi: 10.1113/eph8802503. [DOI] [PubMed] [Google Scholar]
- 12.Nishikawa T, Edelstein D, Du XL, Yamagishi S, Matsumura T, Kaneda Y, et al. Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature. 2000;404:787–90. doi: 10.1038/35008121. [DOI] [PubMed] [Google Scholar]
- 13.Morino K, Petersen KF, Dufour S, Befroy D, Frattini J, Shatzkes N, et al. Reduced mitochondrial density and increased IRS-1 serine phosphorylation in muscle of insulin-resistant offspring of type 2 diabetic parents. J Clin Invest. 2005;115:3587–93. doi: 10.1172/JCI25151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen LB. Mitochondrial membrane potential in living cells. Annu Rev Cell Biol. 1988;4:155–81. doi: 10.1146/annurev.cb.04.110188.001103. [DOI] [PubMed] [Google Scholar]
- 15.Neupert W, Herrmann JM. Translocation of proteins into mitochondria. Annu Rev Biochem. 2007;76:723–49. doi: 10.1146/annurev.biochem.76.052705.163409. [DOI] [PubMed] [Google Scholar]
- 16.Kawamura E, Yamada Y, Yasuzaki Y, Hyodo M, Harashima H. Intracellular observation of nanocarriers modified with a mitochondrial targeting signal peptide. J Biosci Bioeng. 2013;116:634–7. doi: 10.1016/j.jbiosc.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Murphy MP. Selective targeting of bioactive compounds to mitochondria. Trends Biotechnol. 1997;15:326–30. doi: 10.1016/S0167-7799(97)01068-8. [DOI] [PubMed] [Google Scholar]
- 18.Murphy MP. Targeting lipophilic cations to mitochondria. Biochim Biophys Acta. 2008;1777:1028–31. doi: 10.1016/j.bbabio.2008.03.029. [DOI] [PubMed] [Google Scholar]
- 19.Murphy MP, Smith RAJ. Targeting antioxidants to mitochondria by conjugation to lipophilic cations. Annu Rev Pharmacol. 2007;47:629–56. doi: 10.1146/annurev.pharmtox.47.120505.105110. [DOI] [PubMed] [Google Scholar]
- 20.Zhou J, Zhao WY, Ma X, Ju RJ, Li XY, Li N, et al. The anticancer efficacy of paclitaxel liposomes modified with mitochondrial targeting conjugate in resistant lung cancer. Biomaterials. 2013;34:3626–38. doi: 10.1016/j.biomaterials.2013.01.078. [DOI] [PubMed] [Google Scholar]
- 21.Zhang BF, Xing L, Cui PF, Wang FZ, Xie RL, Zhang JL, et al. Mitochondria apoptosis pathway synergistically activated by hierarchical targeted nanoparticles co-delivering siRNA and lonidamine. Biomaterials. 2015;61:178–89. doi: 10.1016/j.biomaterials.2015.05.027. [DOI] [PubMed] [Google Scholar]
- 22.Sharma A, Soliman GM, Al-Hajaj N, Sharma R, Maysinger D, Kakkar A. Design and evaluation of multifunctional nanocarriers for selective delivery of coenzyme q10 to mitochondria. Biomacromolecules. 2012;13:239–52. doi: 10.1021/bm201538j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bielski ER, Zhong Q, Brown M, da Rocha SRP. Effect of the Conjugation Density of Triphenylphosphonium cation on the mitochondrial targeting of poly(amidoamine) dendrimers. Mol Pharm. 2015;12:3043–53. doi: 10.1021/acs.molpharmaceut.5b00320. [DOI] [PubMed] [Google Scholar]
- 24.Malhi SS, Murthy RS. Delivery to mitochondria: a narrower approach for broader therapeutics. Expert Opin Drug Deliv. 2012;9:909–35. doi: 10.1517/17425247.2012.694864. [DOI] [PubMed] [Google Scholar]
- 25.Han M, Vakili MR, Abyaneh HS, Molavi O, Lai R, Lavasanifar A. Mitochondrial delivery of doxorubicin via triphenylphosphine modification for overcoming drug resistance in MDA-MB-435/DOX cells. Mol Pharm. 2014;11:2640–9. doi: 10.1021/mp500038g. [DOI] [PubMed] [Google Scholar]
- 26.Bar-Ilan O, Albrecht RM, Fako VE, Furgeson DY. Toxicity assessments of multisized gold and silver nanoparticles in zebrafish embryos. Small. 2009;5:1897–910. doi: 10.1002/smll.200801716. [DOI] [PubMed] [Google Scholar]
- 27.Yang J, Shimada Y, Olsthoorn RC, Snaar-Jagalska BE, Spaink HP, Kros A. Application of coiled coil peptides in liposomal anticancer drug delivery using a zebrafish xenograft model. Acs Nano. 2016;10:7428–35. doi: 10.1021/acsnano.6b01410. [DOI] [PubMed] [Google Scholar]
- 28.Cai S, Xie YM, Bagby TR, Cohen MS, Forrest ML. Intralymphatic chemotherapy using a hyaluronan-cisplatin conjugate. J Surg Res. 2008;147:247–52. doi: 10.1016/j.jss.2008.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fan X, Zhao X, Qu X, Fang J. pH sensitive polymeric complex of cisplatin with hyaluronic acid exhibits tumor-targeted delivery and improved in vivo antitumor effect. Int J Pharm. 2015;496:644–53. doi: 10.1016/j.ijpharm.2015.10.066. [DOI] [PubMed] [Google Scholar]
- 30.Brown MB, Jones SA. Hyaluronic acid: a unique topical vehicle for the localized delivery of drugs to the skin. J Eur Acad Dermatol. 2005;19:308–18. doi: 10.1111/j.1468-3083.2004.01180.x. [DOI] [PubMed] [Google Scholar]
- 31.Boddapati SV, D'Souza GGM, Erdogan S, Torchilin VP, Weissig V. Organelle-targeted nanocarriers: specific delivery of liposomal ceramide to mitochondria enhances its cytotoxicity in vitro and in vivo. Nano Lett. 2008;8:2559–63. doi: 10.1021/nl801908y. [DOI] [PubMed] [Google Scholar]
- 32.Theodossiou TA, Sideratou Z, Katsarou ME, Tsiourvas D. Mitochondrial delivery of doxorubicin by triphenylphosphonium-functionalized hyperbranched nanocarriers results in rapid and severe cytotoxicity. Pharm Res. 2013;30:2832–42. doi: 10.1007/s11095-013-1111-7. [DOI] [PubMed] [Google Scholar]
- 33.Biswas S, Dodwadkar NS, Deshpande PP, Torchilin VP. Liposomes loaded with paclitaxel and modified with novel triphenylphosphonium-PEG-PE conjugate possess low toxicity, target mitochondria and demonstrate enhanced antitumor effects in vitro and in vivo. J Control Release. 2012;159:393–402. doi: 10.1016/j.jconrel.2012.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simon HU, Haj-Yehia A, Levi-Schaffer F. Role of reactive oxygen species (ROS) in apoptosis induction. Apoptosis. 2000;5:415–8. doi: 10.1023/A:1009616228304. [DOI] [PubMed] [Google Scholar]
- 35.Haldi M, Ton C, Seng WL, Mcgrath P. Human melanoma cells transplanted into zebrafish proliferate, migrate, produce melanin, form masses and stimulate angiogenesis in zebrafish. Angiogenesis. 2006;9:139–51. doi: 10.1007/s10456-006-9040-2. [DOI] [PubMed] [Google Scholar]
- 36.Gao X, Wang S, Wang B, Deng S, Liu X, Zhang X, et al. Improving the anti-ovarian cancer activity of docetaxel with biodegradable self-assembly micelles through various evaluations. Biomaterials. 2015;53:646–58. doi: 10.1016/j.biomaterials.2015.02.108. [DOI] [PubMed] [Google Scholar]


