Abstract
Objectives
To test a patient-centered, tablet-based bedside educational intervention in the hospital and to evaluate the efficacy of this intervention to increase patient engagement with their patient portals during hospitalization and after discharge.
Materials and Methods
We conducted a randomized controlled trial of adult patients admitted to the hospitalist service in one large, academic medical center. All participants were supplied with a tablet computer for 1 day during their inpatient stay and assistance with portal registration and initial login as needed. Additionally, intervention group patients received a focused bedside education to demonstrate key functions of the portal and explain the importance of these functions to their upcoming transition to post-discharge care. Our primary outcomes were proportion of patients who logged into the portal and completed specific tasks after discharge. Secondary outcomes were observed ability to navigate the portal before discharge and self-reported patient satisfaction with bedside tablet use to access the portal.
Results
We enrolled 97 participants (50 intervention; 47 control); overall 57% logged into their portals ≥1 time within 7 days of discharge (58% intervention vs. 55% control). Mean number of logins was higher for the intervention group (3.48 vs. 2.94 control), and mean number of specific portal tasks performed was higher in the intervention group; however, no individual comparison reached statistical significance. Observed ability to login and navigate the portal in the hospital was higher for the intervention group (64% vs. 60% control), but only 1 specific portal task was significant (view provider messaging tab: 92% vs. 77% control, P = .04). Time needed to deliver the intervention was brief (<15 min for 80%), and satisfaction with the bedside tablet to access the portal was high in the intervention group (88% satisfied/very satisfied).
Conclusion
Our intervention was highly feasible and acceptable to patients, and we found a highly consistent, but statistically non-significant, trend towards higher inpatient engagement and post-discharge use of key portal functions among patients in the intervention group.
Keywords: portals, patient engagement, transitions of care, hospitalization
BACKGROUND AND SIGNIFICANCE
Increased patient engagement in care is both one of the greatest opportunities and greatest challenges for the “digital era” of healthcare.1–3 One of the top priorities for Center for Medicare and Medicaid Service’s (CMS’s) incentive program for Meaningful Use of Electronic Health Records (EHRs) is to “engage patients and families” to result in “empowered individuals.”4 Many of these objectives will be met through increased use of personal health records (PHR) or patient portals. Allowing patients’ access to information such as laboratory results, information about medications, patient-specific education resources, and secure messaging to their providers has the potential to engage patients in their healthcare leading to improve quality, safety, and outcomes.5 Although consensus is emerging around key issues to facilitate portal use in acute care settings,6,7 patient engagement with portals in the acute and post-acute setting still trails far behind use in outpatient settings, and evidence for successful implementation of inpatient portals remains very limited.
Most recent studies of portal use in hospital settings have been qualitative or exploratory in nature with notable exceptions.8,9 For example, a study by Wollen and colleagues noted that following bedside training, hospitalized patients responded favorably to accessing their clinical information and reported high levels of satisfaction at accessing information about medications and patient education materials.10 Another study by O’Leary et al found that inpatients who were orientated to their patient portals were significantly more likely to correctly name their physicians and understand their physicians’ roles.11 Similarly, previous work by our group has demonstrated the feasibility of teaching patients to use their portals during hospitalization12 and has suggested that hospitalized patients are eager to use technology to engage in their care13 and that bedside training can improve portal engagement among non-users.14,15 To our knowledge, there are no studies that have examined the role of portals to engage patients during transitions from acute care and after hospital discharge, although several are ongoing.16,17
Engagement during care transitions from the hospital is especially important because of high stakes for patients as well as high costs for the system. Furthermore, recent Meaningful Use objectives also focus on coordination of care, suggesting opportunities to use leverage portals to engage patients’ during their care transitions.4 To explore this opportunity and address gaps in the literature around portal use and transitions of care, we conducted a pilot randomized controlled clinical trial focused on bedside engagement of hospitalized patients to use their patient portals during and after hospital discharge. We hypothesized that patients who received a patient-centered, tablet-based bedside educational intervention on portal use focused on accomplishing key post-discharge tasks (outpatient provider messaging, view results, view medications, and view appointments) would have higher rates of post-discharge portal use than a control group that was provided the same access (bedside tablet computer) but no education.
METHODS
Study design, participants, and setting
We conducted a prospective, randomized controlled trial (RCT) embedded within a larger, observational study of patient engagement in discharge planning.18 We approached patients on either their first or second day of hospitalization, which is aligned with clinical practice at our institution and a widely held maxim of hospital medicine that “discharge planning begins on the day of admission.”19 Participants were eligible for inclusion if they were admitted to the medical service, English speaking, and over age 18 years of age. (Supplementary Appendix: Study Protocol). Participants were ineligible if they were blind, deaf, cognitively impaired by the assessment of their medical team, or involuntarily hospitalized due to incarceration or major psychiatric illness. Participants did not have to be currently enrolled in the University of California San Francisco’s (UCSF’s) portal platform to be eligible to participate, however, were required to have access to a personal tablet or home computer when discharged. Patients could elect to participate in the larger, observational discharge planning study but not the RCT. In such cases, the participant was not assigned to an intervention group, and pre-screening allocation established by the randomization procedure (see below) remained concealed and applied to the next patient who agreed to participate in the RCT. The study took place on the Medicine Service at UCSF, a tertiary referral academic medical center. This study was approved by the UCSF Institutional Review Board and registered as a clinical trial at www.clinicaltrials.gov (identifier NCT02109601).
Randomization and power calculations
We used a block randomization procedure to assign patients to intervention or control groups. Prior to screening or approaching patients, research assistants (RAs) used a random number generator to create blocks of 10 with random ordering of repeated numbers (1 = intervention, 2 = control). Due to the nature of the intervention, participants or study personnel were not blinded following random assignment. We calculated 100 patients were needed to enable detection of a 25% absolute difference in ability to perform at least 1 post-discharge portal task (80% power, 2-sided alpha 0.05).
Intervention and control group descriptions
To ensure that device access and portal login were not barriers to pre-discharge portal access, we provided all patients with tablet computers (iPad® 16 GB 3rd generation Model A1430) and in-person login assistance. The portal used at our institution (MyChart by Epic Systems) is mobile friendly and easily accessible via web browsers commonly used on tablets, desktops, laptops, or smartphones. Control patients received a tablet computer and limited assistance registering and logging in if they were first-time users of our portal; no other assistance or instruction on how to use the portal was offered or delivered to control patients. Intervention patients received an extensive bedside, structured education by trained RAs in the hospital, which guides patients through key functions of the portal, including how to verify personal information (eg, address, phone number, email), view medications and request refills, view test results (labs and radiology), view current appointments and request changes, and how to view and send secure messages to outpatient providers. To enhance patient engagement in the intervention arm, we explained the relevance of these tasks and gave explicit examples for how the portal could be useful to them after leaving the hospital, eg, checking (or changing) appointments made during hospitalization that they may wish to change after discharge, checking for new medications prescribed in the hospital (or requesting refills), and reviewing test results (especially those pending at the time of discharge). While this tutorial provides uniform basic content for all patients, it was designed to be adaptive enough to allow RAs to “speed up” or “slow down” or otherwise tailor the depth of explanation to the needs of each individual patient. All patients were approached before noon, and they were encouraged to use the tablet on their own for the rest of the day. The RA returned to re-collect the device approximately 5 hours later and complete a debrief interview (Supplementary Appendix: Study Protocol).
Data collection and sources of data
Following enrollment and consent, RAs administered a brief pre-study survey to assess baseline technology use. This survey, which was previously used by our group,12 assessed device ownership, internet use, and any pre-admission portal activities (defined as use of any online portal, not just our institutional portal, to access health information or accomplish tasks such as refilling prescription). At the end of the day, the RAs performed a debrief interview in which participants were asked to independently demonstrate ability to perform key portal tasks (the same ones addressed in the structured tutorial). The RA recorded which tasks (if any) were able to be accomplished independently and/or whether the RA provided additional assistance. To assess portal access and use to accomplish post-discharge tasks (defined as login, outpatient provider messaging, view results, view medications, and view appointments), we accessed searchable databases of our EHR via Epic Systems Clarity clinical databases (Verona WI). Patient demographic and clinical information was also obtained from the EHR. For clinical severity specifically, we used the used Severity of Illness classification developed by the CMS, which categorizes all patients with a given Diagnosis-Related Group into 1 of 4 classes of severity (minor, moderate, major, and extreme).
Primary and secondary outcomes
Primary outcomes were the proportion of patients who logged in to the portal and completed specific tasks after discharge: login, outpatient provider messaging, view results, view medications, and view appointments. Secondary outcomes were the RA-observed ability to navigate the portal before discharge (login, view medications, view med refills, view appointments, view lab results, view messages) and patient satisfaction (overall satisfaction using the tablet in the hospital and using the tablet specifically to access and navigate the portal in hospital).
Data analysis
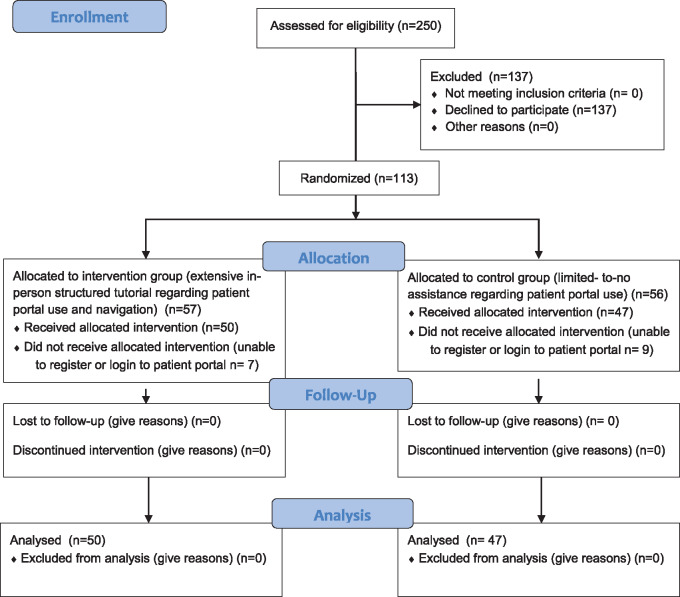
Two-hundred-fifty patients were eligible for the study and were approached as described in our CONSORT Flow Diagram (Figure 1). Of these, 163 were enrolled in a larger observational study of patient engagement in discharge planning, and 113 of these also agreed to participate in the randomized trial. Of 113 who agreed to enroll in the trial and were randomized, 97 completed were able to register/log in successfully to MyChart and willing to allow monitoring of their post-discharge portal use. Given that the outcome of interest was post-discharge portal use, we could not use an intention-to-treat analysis to include the 16 patients who initially agreed to participate but were ultimately unable to log in or would not allow post-discharge data access, as these patients did not have the primary outcome of interest (post-discharge portal usage). Most of these patients had existing accounts but could not remember their login information and were unable to reset their password or were locked out after multiple attempts at the time of study enrollment. Although our team was able to register participants for new accounts, we were unable to reset or unlock existing accounts if the participant could not remember details needed to restore or reset his or her account (such as the correct email used to originally register the account). Therefore, we used a per-protocol approach to data analysis and present results from the 97 participants who were able to register/log in successfully and allow access to their post-discharge portal data. Patient demographic and clinical information was summarized using descriptive statistics. To assess the rigor of randomization, we compared these characteristics by intervention and control group using t tests and chi-square tests. We summed and averaged the total number of logins to the portal and number of clicks in different domains of the portal (medications, labs, appointments). We used logistic regression to adjust for age and previous portal use, as well as functional impairment given our prior work suggesting negative effects on both transitions20 and internet access at home.21 For logistic regressions, we constructed our dichotomous outcome variables as “ever” or “at least once” events, eg, a patient who logged in once or performed a certain task (ex: viewing medications) would be categorized the same as one who logged in (or performed a certain task) many times. Those who logged in or completed tasks at least once were compared to patients who never logged in or never completed the specified tasks. Analyses were conducted in SAS.
Figure 1.
CONSORT flow diagram.
RESULTS
Patient characteristics (Table 1)
Table 1.
Participant characteristics
| Total | Overall N (%) | Intervention n (%) | Control n (%) |
|---|---|---|---|
| 97 | 50 (52%) | 47 (48%) | |
| Demographics | |||
| Age | |||
| 18–49 | 48 (49) | 20 (40) | 28 (60) |
| 50–60 | 41 (42) | 24 (48) | 17 (36) |
| ≥70 | 8 (8) | 6 (12) | 2 (4) |
| Gender | |||
| Female | 53 (55) | 28 (58) | 25 (55) |
| Race/ethnicity | |||
| White | 53 (55) | 26 (52) | 27 (57) |
| Black | 19 (20) | 9 (18) | 10 (21) |
| Hispanic | 9 (9) | 5 (10) | 4 (9) |
| Asian | 7 (7) | 5 (10) | 2 (4) |
| Other/Unknown | 9 (9) | 5 (10) | 4 (9) |
| Married/Living as married | 47 (48) | 22 (44) | 25 (55) |
| Payer | |||
| Medicaid | 23 (24) | 10 (20) | 13 (28) |
| Medicare | 22 (23) | 13 (26) | 9 (19) |
| Private | 26 (47) | 24 (50) | 22 (47) |
| Self-pay/Uninsured | 6 (6) | 3 (6) | 3 (6) |
| UCSF primary care provider | 43 (44) | 25 (50) | 18 (38) |
| Clinical Characteristics | |||
| Clinical severity of illness | |||
| Minor or moderate | 29 (30) | 14 (28) | 15 (32) |
| Major | 55 (57) | 27 (54) | 28 (60) |
| Extreme | 13 (13) | 9 (18) | 4 (9) |
| Length of stay | Mean 6.4 (13.5 STD) | Mean 5.1 (STD 4.7) | Mean 7.7 (STD 18.8) |
| Technology use characteristics | |||
| Device ownership | |||
| Own desktop computer | 51 (53) | 25 (50) | 26 (55) |
| Own laptop computer | 67 (69) | 36 (72) | 31 (66) |
| Own smartphone | 57 (59) | 26 (52) | 31 (66) |
| Own tablet computer | 48 (49) | 26 (52) | 22 (47) |
| Doesn’t own a device | 6 (6) | 3 (6) | 3 (6) |
| Internet use | |||
| Internet use daily | 79 (81) | 39 (78) | 40 (85) |
| Internet use several times a week | 7 (7) | 4 (8) | 3 (6) |
| Internet use once a week or less | 6 (6) | 2 (4) | 4 (9) |
| Pre-study online health tasks (any platform) | |||
| Looked up health information | 78 (80) | 40 (80) | 38 (81) |
| Communicated with provider | 55 (57) | 30 (60) | 25 (55) |
| Scheduled medical appointment | 39 (41) | 23 (46) | 16 (34) |
| Refilled prescription | 34 (35) | 25 (50) | 9 (19) |
| None of these | 10 (10) | 3 (6) | 7 (15) |
Although our study arms were not powered to detect small differences in patient characteristics, overall demographics appear very similar between groups, and prior technology use rates were comparable between groups in terms of device ownership, internet use, and pre-study online health tasks. Notably, the one area of difference between the 2 groups that was significant was prior MyChart registration: 34 participants in the intervention group (68%) were previously registered vs. 18 (38%) in the control group (P < .01). Thus, 16 patients in the intervention group and 29 in the control group were registered for new MyChart accounts at the time of their enrollment in the study. This difference notwithstanding, our key measure for feasibility, time needed for basic orientation to use of the portal on the tablets, was not different by intervention group. Most participants required less than 15 minutes (40 or 80% intervention; 40 or 85% control) and a few required 15–30 minutes (4 or 8% intervention; 3 or 6% control) or over 30 minutes (6 or 12% intervention; 4 or 9% control).
Inpatient portal use and satisfaction
All 97 participants included in the analysis were able to login and navigate within their portals during their inpatient stay. When study tablets were collected at the end of the day by the RA, however, only 60 (62%) participants were able to demonstrate ability to log in independently as part of the debrief interview; the remaining 37 (38%) were able to log in with assistance (Table 2). Once logged in, participants were able to accomplish other tasks as part of this debrief interview with varying frequency. For all tasks, we observed a higher percentage of success in accomplishing the task independently in the intervention group (range 46%–92% intervention vs. 32%–79% control), although this reached statistical significance only for the task of navigating to the outpatient provider messaging tab (46 or 92% intervention; 36 or 77% control, P = .04). With respect to participant satisfaction, overall satisfaction was high for using the tablet during hospitalization in general (78 or 80% were “satisfied” or “very satisfied”) and for using the tablet to access and navigate their portals specifically (83 or 86% “satisfied” or “very satisfied”). Again we observed higher rates in the intervention group vs. control, but these did reach statistical significance (Table 2).
Table 2.
Inpatient portal tasks accomplished independently and patient satisfaction
| Tasks Accomplished | Overall N (%) | Intervention n (%) | Control n (%) | P-value |
|---|---|---|---|---|
| Login | 60 (62) | 32 (64) | 28 (60) | .65 |
| View provider messaging | 82 (86) | 46 (92) | 36 (77) | .04 |
| View lab results | 79 (81) | 43 (86) | 36 (77) | .23 |
| View medications | 74 (76) | 41 (82) | 33 (70) | .17 |
| View appointments | 82 (86) | 45 (90) | 37 (79) | .12 |
| Patient satisfaction | ||||
| Overall satisfaction using tablet in the hospital | 78 (80) | 43 (86) | 35 (74) | .15 |
| Satisfaction with tablet to access and navigate portal | 83 (86) | 44 (88) | 39 (83) | .48 |
Post-discharge patterns of portal use
Just over half of all participants logged into their portals at least once within 7 days of discharge: 55 or 57% overall, 29 (58%) for intervention; 26 (55%) for control (Table 3). Mean number of total logins was higher for the intervention group (3.48 vs. 2.94 for control) but not statistically significant. The percentage of participants who performed specific tasks once logged in to the portal ranged from 20%–48% for the intervention group and 10%–38% for control. Mean number of tasks performed was higher for the intervention group in every area measured; however, no individual comparison reached statistical significance. The most frequently performed (highest means) for both groups were outpatient provider messaging (5.98 intervention, 3.98 control), lab results (5.68 intervention, 4.36 control), and appointment review (2.14 intervention, 2.04 control).
Table 3.
Post-discharge portal tasks accomplished by patients
| Clicked at least once |
Mean number of clicks |
||||||
|---|---|---|---|---|---|---|---|
| Task | All N (%) | Intervention n (%) | Control n (%) | P-value (ChiSq) | Intervention | Control | P-value (Wilcoxon) |
| Login | 55 (57) | 29 (58) | 26 (55) | .86 | 3.48 | 2.94 | .60 |
| Provider messaging | 42 (43) | 24 (48) | 18 (38) | .55 | 5.98 | 3.98 | .33 |
| Lab results | 40 (41) | 22 (44) | 18 (38) | .59 | 5.68 | 4.36 | .49 |
| View medications | 33 (34) | 17 (34) | 16 (34) | .53 | 1.24 | 1.23 | .78 |
| Appointment review | 34 (35) | 21 (42) | 13 (28) | .41 | 2.14 | 2.04 | .23 |
Finally, we performed logistic regression analysis to determine if odds of post-discharge portal access were higher among intervention participants. Given the differences observed between intervention and control groups in terms of age (non-significant) and prior MyChart use (significant), we performed logistic regression analyses adjusted for these variables to predict login or performance of any single task listed in Table 3. Although unadjusted odds ratios were higher (>1.0) for each task when modeled for the intervention group, this did not achieve statistical significance. Similarly, adding age and prior MyChart use to the model as adjustor variables did not result in any statistically significant result (all confidence intervals crossed 1.0, results not shown).
DISCUSSION
We found that a patient-centered, tablet-based bedside educational intervention focused on portal training for hospitalized patients produced a trend towards higher overall use of and engagement with the portal among intervention patients, specifically in their observed ability to login and navigate the portal before discharge, satisfaction with portal use on tablets in the hospital, and frequency of portal use after discharge. Our approach differs from previous hospital-based EHR interventions that have focused on engaging providers to increase the completion and accuracy of key transition tasks such as scheduling appointments, communicating with providers, and completing medication reconciliation.22–24 There are few studies that have examined the potential for portals to improve patient engagement in these tasks during transitions of care. Recent systematic reviews of this area have highlighted that existing studies have largely been qualitative or exploratory in nature8,9; ours is the first randomized clinical trial to rigorously test an interventional approach to increase patient engagement with their portals in the hospital and post-discharge settings.
While the positive trend towards greater engagement in tasks for our intervention group was very consistent, only 1 area (outpatient provider messaging) was statistically significant. There are several factors that could explain this result. First, it is possible that providing patients with tablets to access their portals could be a more powerful intervention than we anticipated and could have overshadowed the educational intervention. To explore this question, we created a virtual cohort of 400 active users of our institutional portal who were hospitalized around the same time as patients in the current study but did not receive any device during their stay.14 We compared portal use in this virtual cohort to patients in the current study as part of our published study protocol. Virtual cohort patients had a similar number of logins, but patients in our study who received tablets were more likely to use the portal to check their medications during hospitalization, even after adjustment for prior portal use. Second, although we anticipated a modest effect and set our enrollment targets accordingly, our intervention effect was even smaller than anticipated. Our previous work using a 12-hospital quality and research network showed that few patients (20%–30%) had ever used the internet for post-discharge tasks related to medications, appointments, or provider communication.25 In the current study, however, most patients reported they had used the internet for these tasks in the past, and our observed use of the portal for these post-discharge tasks among all study participants ranged from 35%–57% overall. Thus, it is possible that a secular trend towards greater portal use effectively elevated the pre-study baseline we had previously observed and used to set our targets.
Although a secular trend towards greater portal use would be good news, the larger literature on patient perceptions and experiences using inpatient portals suggests plenty of room for improvement in the hospital to increase engagement.8,9 Indeed, our qualitative work with patients admitted at 12 hospitals across the United States,26 as well as more in-depth interviews with a subset of patients who used iPad tablets to access their portal at our hospital10 and others,27 suggests educational barriers are among the most important—and addressable—challenges to inpatient and post-discharge use of portals.28,29 While the trend we observed in this study toward greater portal engagement among intervention patients who received adaptive educational training in portal use adds validity to this hypothesis, the limited (non-statistically significant) effect may also be due to broad enrollment criteria, which allowed a wide range of experience and aptitude. Future studies should focus interventions to patients with observed inability to perform certain tasks as inclusion criteria or those at highest risk of poor transitions. Future studies should ultimately measure success in terms of outcomes such as fewer missed follow-up appointments or unfilled medications, as these seem plausibly modifiable through better portal engagement to view or change appointments and refill medications. Furthermore, future educational interventions could leverage more sophisticated approaches to enhance patient self-efficacy. As one example, a “teach to goal” approach has recently been deployed in the hospital to achieve more consistent and effective use of inhalers after discharge in patients with respiratory conditions such as asthma.30,31 In this approach, patients must independently demonstrate competency in a series of small tasks to complete the intervention (eg, remove cap from inhaler, attach spacer to inhaler, depress inhaler correct number of times for intended dose, inhale and hold breath for 5 seconds, exhale slowly). If the patient performs any of these tasks incorrectly, the provider reviews those steps until the patient can reach the goal of completing all tasks correctly and independently. This teach to goal approach could be applied to hospital-based portal training to ensure higher self-efficacy in portal use, particularly in patients with limited baseline portal skills or at higher risk for poor transitions of care. Finally, while we did not explore the abilities of family members or other caregivers to engage in portal tasks on the patient’s behalf, several studies of parental portal use during pediatric hospitalization demonstrated high engagement and can serve as examples for future work in this area with adult inpatients.32,33
Another step towards greater patient efficacy in portal engagement could be to teach patients to access the portal on their own devices. We provided tablet computers at bedside to ensure a uniform portal experience for participants, but many patients now bring their own mobile devices to the hospital with them. Indeed, in a separate study, we found about 2 in 3 patients at our hospital brought and used at least 1 mobile device during their hospitalization (rates were as high as 80% in some units such as oncology).13 As the movement towards “bring your own device” (BYOD) gains momentum for patient engagement with the EHR and other health-related platforms (eg, diet, activity, and medication logs or other health-related apps), there is tremendous opportunity for patients in acute and post-acute phases of care. For example, we are currently studying a BYOD approach to engaging patients in mobility during and after hospitalization using accelerometers and patients’ own smartphones to provide feedback as they strive to achieve walking goals (steps per day) to promote recovery.34 Finally, there may be certain pragmatic advantages to a BYOD approach to portal engagement. In our study, we found that only 62% of all patients were able to log in independently but, once logged in, ability to accomplish other tasks independently was notably higher (76%–86%). While there may be a number of factors at play, one compelling hypothesis is that patients had a difficult time getting to the login page and entering their credentials on an unfamiliar device. Future studies could explore whether a BYOD approach could facilitate stored credentials or even use biometrics (fingerprint of facial recognition), as these are becoming standard for most mobile devices.
We believe our results and experience have important implications for policy and practice regarding the use of portals in the hospital and immediately after discharge. First and foremost, more studies of portal use in the hospital are needed, especially given that most hospitals have not yet deployed this feature of EHR, and Meaningful Use will require higher use in the near future,4 suggesting an impending implementation boom—more evidence is needed to guide this process. Furthermore, future implementation work will need to anticipate and study the effect of portals that are unique to the inpatient environment, such as MyChart Bedside—we used a single portal that reflected actual practice at UCSF. While there may be certain advantages to an inpatient-only mode for portals, there may be tradeoffs as well, such as having to “re-learn” how to navigate a different layout and set of functionalities after discharge. Studies of this platform to date have focused on provider experience35 or patient satisfaction,36 but have not yet examined patient usage or outcomes. Indeed, while national data are lacking, our experience networking with peer institutions suggests that most are still using a single portal designed primarily for outpatient use without a separate inpatient version or adaptive portal that has an inpatient view (such as MyChart Bedside). Finally, our portal (MyChart) is “tethered” to our EHR (Epic), which means there is limited ability to share information between among in different systems with different EHR systems. Future studies should examine how patients who receive care in multiple systems may leverage the portal differently after discharge.
While our study brings insights into the use of portals in the hospital, it also has limitations. We studied patients at 1 hospital only on a general medicine service; patients at other medical centers or different services may have different experiences and abilities using portals. Second, we were unable to follow an intention-to-treat analysis because some patients with existing MyChart accounts were unable to log in or unlock their accounts after randomization. Thus, these patients did not have the opportunity to contribute to the study outcomes (frequency of login and frequency of MyChart task completion) and could not be analyzed together with patients who were able to successfully log in; however, our analysis did include all other patients who were enrolled (there was no loss to follow-up and inability to login was the one and only cause for exclusion from final analysis). Third, although we used a rigorous randomization process and found no differences in virtually every category of clinical/demographic features or technology use, we did observe far higher rates of prior MyChart use in the intervention group. Nonetheless, this did not appear to be a significant predictor of engagement in our analyses that adjusted for prior MyChart use.
CONCLUSIONS
We conducted a randomized trial of a bedside tablet-based educational intervention to improve post-discharge use of our institutional patient portal and found consistent but statistically non-significant trends towards higher post-discharge use in the intervention group. As demand for patient access to electronic medical records increases from key stakeholders including patients/caregivers, government and private payers, as well as healthcare providers, more evidence from rigorous studies will be needed to guide successful implementation and operationalization of patient portals during and after acute care.
FUNDING
This research was supported by the National Institutes of Health (NIH), National Institute of Aging (NIA) through the Claude D. Pepper Older Americans Independence Center, grant number P30AG021342, and a Career Development Award, grant number K23AG045338-05 (Dr Greysen). This research was also sponsored by an intramural grant for Digital Health by the University of California, San Francisco (no grant number, Dr Greysen, PI). No sponsor had any role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
CONTRIBUTION STATEMENT
SRG: conception of the work; acquisition, analysis, and interpretation of data; drafting of the manuscript and revisions for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
JDH: analysis and interpretation of data; drafting of the manuscript and revisions for important intellectual content; final approval of the version to be published.
CR: analysis and interpretation of data; revisions to the manuscript for important intellectual content; final approval of the version to be published.
YM: acquisition, analysis, and interpretation of data; drafting of the manuscript and revisions for important intellectual content; final approval of the version to be published.
NH: analysis and interpretation of data; revisions to the manuscript for important intellectual content; final approval of the version to be published.
JR: acquisition, analysis, and interpretation of data; revisions to the manuscript for important intellectual content; final approval of the version to be published.
ADA: conception of the work and interpretation of data; revisions to the manuscript for important intellectual content; final approval of the version to be published.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Conflict of interest statement. All authors have no competing interests to declare.
Supplementary Material
ACKNOWLEDGMENTS
Preliminary results from this project were presented as part of a panel presentation at the 2015 Annual Meeting of the American Medical Informatics Association and as a research poster presentation at the 2015 Annual Meeting of the Society for Hospital Medicine.
REFERENCES
- 1. Laurance J, Henderson S, Howitt PJ, et al. Patient engagement: four case studies that highlight the potential for improved health outcomes and reduced costs. Health Aff (Millwood) 2014; 33 (9): 1627–34. [DOI] [PubMed] [Google Scholar]
- 2. Irizarry T, DeVito Dabbs A, Curran CR.. Patient portals and patient engagement: a state of the science review. J Med Internet Res 2015; 17 (6): e148.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kruse CS, Argueta DA, Lopez L, Nair A.. Patient and provider attitudes toward the use of patient portals for the management of chronic disease: a systematic review. J Med Internet Res 2015; 17 (2): e40.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.EHR Incentives and Certification: Meaningful Use Definitions and Objectives. https://www.healthit.gov/providers-professionals/meaningful-use-definition-objectives. Accessed March 22, 2018.
- 5. Kruse CS, Bolton K, Freriks G.. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res 2015; 17 (2): e44.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Collins SA, Rozenblum R, Leung WY, et al. Acute care patient portals: a qualitative study of stakeholder perspectives on current practices. J Am Med Inform Assoc 2017; 24(e1): e9–e17. [Epub ahead of print] PubMed PMID: 27357830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grossman LV, Choi SW, Collins S, et al. Implementation of acute care patient portals: recommendations on utility and use from six early adopters. J Am Med Inform Assoc 2018; 25(4): 370–9. [Epub ahead of print] PubMed PMID: 29040634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Inform Assoc 2014; 21 (4): 742–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kelly MM, Coller RJ, Hoonakker PL.. Inpatient portals for hospitalized patients and caregivers: a systematic review . J Hosp Med 2017; doi:10.12788/jhm.2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Woollen J, Prey J, Wilcox L, et al. Patient experiences using an inpatient personal health record. Appl Clin Inform 2016; 7 (2): 446–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. O’Leary KJ, Lohman ME, Culver E, et al. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. J Am Med Inform Assoc 2016; 23 (1): 159–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Greysen SR, Khanna RR, Jacolbia R, Lee HM, Auerbach AD.. Tablet computers for hospitalized patients: a pilot study to improve inpatient engagement. J Hosp Med 2014; 9 (6): 396–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ludwin S, Greysen SR.. Use of smartphones and mobile devices in hospitalized patients: untapped opportunities for inpatient engagement. J Hosp Med 2015; 10 (7): 459–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Greysen SR, Magan Mendoza Y, Rosenthal J, et al. Using tablet computers to increase patient engagement with electronic personal health records: protocol for a prospective, randomized interventional study. JMIR Res Protoc 2016; 5 (3): e176.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Greysen SR, Rajkomar A, Ritchie CR, Auerbach AD.. Improving engagement of older, hospitalized adults through bedside use of personal health records [abstract]. J Hosp Med 9 (Suppl 2): 147. [Google Scholar]
- 16. McAlearney AS, Sieck CJ, Hefner JL, et al. High touch and high tech (HT2) proposal: transforming patient engagement throughout the continuum of care by engaging patients with portal technology at the bedside. JMIR Res Protoc 2016; 5 (4): e221.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Masterson Creber R, Prey J, Ryan B, et al. Engaging hospitalized patients in clinical care: study protocol for a pragmatic randomized controlled trial. Contemp Clin Trials 2016; 47: 165–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harrison JD, Greysen SR, Jacolbia R, et al. Not ready, not set…discharge: patient-reported barriers to discharge readiness at an academic medical center. J Hosp Med 2016; 11 (9): 610–4. [DOI] [PubMed] [Google Scholar]
- 19. Goodman DM, Burke AE, Livingston EH.. Discharge planning. JAMA 2013; 309 (4): 406.. [DOI] [PubMed] [Google Scholar]
- 20. Greysen SR, Stijacic Cenzer I, Auerbach AD, Covinsky KE.. Functional impairment and hospital readmission in Medicare seniors. JAMA Intern Med 2015; 175 (4): 559–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Greysen SR, Chin Garcia C, Sudore RL, Cenzer IS, Covinsky KE.. Functional impairment and internet use among older adults: implications for meaningful use of patient portals. JAMA Intern Med 2014; 174 (7): 1188–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schnipper JL, Liang CL, Hamann C, et al. Development of a tool within the electronic medical record to facilitate medication reconciliation after hospital discharge. J Am Med Inform Assoc 2011; 18 (3): 309–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med 2009; 169 (8): 771–80. [DOI] [PubMed] [Google Scholar]
- 24. Turchin A, Hamann C, Schnipper JL, et al. Evaluation of an inpatient computerized medication reconciliation system. J Am Med Inform Assoc 2008; 15 (4): 449–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Greysen S, Metlay J, Kripalani S, Sarkar U, Robinson E, Auerbach A.. Internet use for postdischarge health care tasks among readmitted patients: preliminary results from the homerun transitions of care study [abstract]. J Hosp Med 2013; 8 (suppl 2) https://www.shmabstracts.com/abstract/internet-use-for-postdischarge-health-care-tasks-among-readmitted-patients-preliminary-results-from-the-homerun-transitions-of-care-study/. Accessed October 3, 2018. [Google Scholar]
- 26. Greysen SR, Harrison JD, Kripalani S, et al. Understanding patient-centred readmission factors: a multi-site, mixed-methods study. BMJ Qual Saf 2017; 26 (1): 33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. O’Leary KJ, Sharma RK, Killarney A, et al. Patients’ and healthcare providers’ perceptions of a mobile portal application for hospitalized patients. BMC Med Inform Decis Mak 2016; 16 (1)123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Prey JE, Restaino S, Vawdrey DK.. Providing hospital patients with access to their medical records. AMIA Annu Symp Proc 2014; 2014: 1884–93. [PMC free article] [PubMed] [Google Scholar]
- 29. Davis SE, Osborn CY, Kripalani S, et al. Health literacy, education levels, and patient portal usage during hospitalizations. AMIA Annu Symp Proc 2015; 2015: 1871–80. [PMC free article] [PubMed] [Google Scholar]
- 30. Press VG, Arora VM, Shah LM, et al. Teaching the use of respiratory inhalers to hospitalized patients with asthma or COPD: a randomized trial. J Gen Intern Med 2012; 27 (10): 1317–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Press VG, Kelly CA, Kim JJ, et al. Virtual Teach-To-Goal™ adaptive learning of inhaler technique for inpatients with asthma or COPD. J Allergy Clin Immunol Pract 2017; 5 (4): 1032–9.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kaziunas E, Hanauer DA, Ackerman MS, Choi SW.. Identifying unmet informational needs in the inpatient setting to increase patient and caregiver engagement in the context of pediatric hematopoietic stem cell transplantation. J Am Med Inform Assoc 2016; 23 (1): 94–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kelly MM, Hoonakker PL, Dean SM.. Using an inpatient portal to engage families in pediatric hospital care. J Am Med Inform Assoc 2017; 24 (1): 153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mobility Optimization Via Engagement with Interactive Technology – The MOVE-IT Randomized Trial. https://clinicaltrials.gov/ct2/show/NCT03321279. Accessed April 3, 2018.
- 35. Hefner JL, Sieck CJ, Walker DM, et al. System-wide inpatient portal implementation: survey of health care team perceptions. JMIR Med Inform 2017; 5 (3): e31.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Winstanley EL, Burtchin M, Zhang Y, et al. Inpatient experiences with MyChart bedside. Telemed J E Health 2017; 23 (8): 691–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.