Abstract
Introduction
Ameloblastoma is a locally destructive tumor with a propensity for recurrence if not entirely excised. Management of ameloblastoma poses a challenge for all involved in the field of head and neck surgery because successful treatment requires not only adequate resection but also a functional and aesthetically acceptable reconstruction of the residual defect.
Methods
Patients who had histologically proven ameloblastoma between 1991 and 2009 were identified from the database of Aga Khan University Hospital. A review of all medical records, radiological images, operative reports and pathology reports was undertaken.
Results
A total of 15 patients with histologically confirmed ameloblastoma were identified. Out of 15 patients nine were males and six were females with age range from 20 to 60 years (mean age 43 years). The most common symptom found in our patient group was painless facial swelling. In 13 patients the origin of tumor was mandible and in the remaining two the tumor originated from maxilla. Eleven out of 15 patients underwent segmental mandibulectomy, two had maxillectomy and two had enucleation. All patients who underwent segmental mandibulectomy required reconstruction. Reconstruction was done with microsurgical free tissue transfer in eight patients, non-vascularized iliac crest bone graft was used in one patient and two had plating only. All free flaps survived with no evidence of flap loss. The mean follow-up was eight years. There was no evidence of graft failure which was used in one patient. Complication was seen in only one of our patients in the form of plate exposure. Recurrence was seen in two of our cases who primarily underwent enucleation. All patients had satisfactory speech, cosmesis and mastication.
Conclusion
The management of ameloblastoma still poses a big challenge in spite of being the most common odontogenic tumor. In our study we have found that segmental mandibulectomy with disease-free margin of around 1 cm and immediate reconstruction with free tissue transfer have shown good results.
Keywords: orthopantomogram, free fibular flap, odontogenic tumor, ameloblastoma, opg, unicystic ameloblastoma, solid ameloblastoma, multicystic ameloblastoma, tumors and cysts of jaw
Introduction
Ameloblastoma is a benign but locally aggressive tumor of epithelial origin that arises from enamel, dental follicle, periodontal ligaments or lining of odontogenic cysts [1, 2]. It is a rare head and neck tumor but it is still the most common odontogenic tumor [3].
The estimation of annual incidence of ameloblastoma is 0.5 per million population. This accounts for more or less 1% of tumors and cysts involving jaw and 10% of tumors of dental origin. Although ameloblastoma involves all age groups, peak incidence is documented in the second and sixth decade [4, 5]. The third and fourth decade is also mentioned for the peek incidence by others [6]. There is significant difference among racial groups. In Blacks more cases are seen in third decade whereas Caucasians have peak incidence during the fourth decade. The disease is most often found posteriorly in the angle of mandible and ascending ramus but can occur anywhere in the mandible or maxilla. Overall 80% of all ameloblastomas occur in the mandible and 20% in the maxilla.
The tumor is usually asymptomatic and presents itself as a slowly enlarging facial swelling. Ameloblastoma is a locally destructive tumor with a propensity for recurrence if not entirely excised. Radiological investigations are helpful in diagnosis. The orthopantomogram (OPG) is a useful first-line investigation and shows well-demarcated unilocular or multilocular expansile lucencies with a so-called ‘soap bubble’ appearance [7, 8]. Computed tomography (CT) is useful in the assessment of the extent of the tumor and cortical destruction of bone [9].
There are six histopathologic subtypes of ameloblastoma that include the follicular, plexiform, acanthomatous, granular cell, basal cell, and desmoplastic types [10, 11]. These subtypes can exist singly or in combination. The tumor is also subdivided into four variants, based on its overall histologic architecture. These include the solid, multicystic, multicystic plus solid, and unicystic types [12, 13].
Management of ameloblastoma poses a challenge for all involved in the field of head and neck surgery because successful treatment requires not only adequate resection but also a functional and aesthetically acceptable reconstruction of the residual defect. Resection with wide margins and reconstruction in the same sitting is currently accepted as the treatment of choice in most cases. Idea of conservative surgery is no longer entertained since it is associated with higher recurrence rate [14, 15].
This work was done to review a management outcome of patients of ameloblastoma who were managed at Aga Khan University Hospital, a tertiary care institute in the city of Karachi, Pakistan.
Materials and methods
Patients who had histologically proven ameloblastoma between 1991 and 2009 were identified from the database of Aga Khan University Hospital. A review of all medical records, radiological images, operative reports and pathology reports was undertaken.
All patients had preoperative radiological investigations including OPG and CT scan of head and neck. Lower limb angiography was also performed in a few cases for those who underwent mandibular reconstruction with the free fibular flap.
In all of our cases resection of tumor was carried out followed by reconstruction. Reconstructions of the mandibular defects were achieved by free tissue transfer with the free fibular flap. The free fibular flaps were raised in the standard fashion as described in the literature. Intra-operatively, a nasogastric tube was inserted in all cases to facilitate early post-operative feeding and to avoid potential contamination of the healing oral wounds.
The multidisciplinary team involved in preoperative and post-operative care and rehabilitation included surgical, nursing, physiotherapy, dietitian and dental staff. All patients were followed up with interval imaging to assess for recurrence.
Results
A total of 15 patients with histologically confirmed ameloblastoma were identified from data base of health information system of Aga Khan University Hospital. Out of 15 patients nine were males and six were females with age range from 20 to 60 years (mean age 43 years). The most common symptom found in our patient group was painless facial swelling. In 13 patients the origin of tumor was mandible and in the remaining two the tumor originated from maxilla. These clinical details of individual patients are shown in Table 1.
Table 1. Clinical presentation of all patients.
| Patient | Age (Years) | Sex | Symptom | Site |
| 1 | 32 | M | Facial swelling | Mandible |
| 2 | 46 | F | Facial swelling | Mandible |
| 3 | 56 | M | Facial swelling | Mandible |
| 4 | 55 | M | Facial swelling | Mandible |
| 5 | 21 | F | Intraoral swelling | Mandible |
| 6 | 20 | M | Facial swelling and trismus | Mandible |
| 7 | 60 | M | Facial swelling | Maxilla |
| 8 | 55 | M | Facial swelling | Mandible |
| 9 | 45 | F | Facial swelling | Maxilla |
| 10 | 51 | F | Facial swelling | Mandible |
| 11 | 31 | M | Facial swelling | Mandible |
| 12 | 45 | F | Facial swelling | Mandible |
| 13 | 46 | F | Facial swelling | Mandible |
| 14 | 38 | M | Facial and intraoral swelling | Mandible |
| 15 | 49 | M | Intraoral swelling | Mandible |
Eleven out of 15 patients underwent segmental mandibulectomy, two had maxillectomy and two had enucleation. All patients who underwent segmental mandibulectomy required reconstruction. Reconstruction was done with microsurgical free tissue transfer in eight patients, non-vascularized iliac crest bone graft was used in one patient and two had AO plating without free tissue transfer. All free flaps survived with no evidence of flap loss. The mean follow-up was eight years. There was no evidence of graft failure; the iliac crest bone graft was used in only one patient. Complication was seen in only one of the two patients who had reconstruction with AO plating without free tissue transfer. Recurrence was seen in two of our cases within one year of follow-up who primarily underwent enucleation; they were later operated with wide resection and AO plating. Surgical detail and outcome of individual patients are shown in Table 2.
Table 2. Surgical details and outcome.
| Patient | Surgery | Reconstruction | Complications | Follow Up (Years) | Recurrence |
| 1 | Segmental mandibulectomy | Free fibula flap | No | 5 | No |
| 2 | Segmental mandibulectomy | Free fibula flap | No | 6 | No |
| 3 | Segmental mandibulectomy | Free fibula flap | No | 8 | No |
| 4 | Segmental mandibulectomy | Plating | No | 11 | No |
| 5 | Segmental mandibulectomy | Free fibula flap | No | 4 | No |
| 6 | Segmental mandibulectomy | Free fibula flap | No | 9 | No |
| 7 | Maxillectomy | No reconstruction | No | 10 | No |
| 8 | Segmental mandibulectomy | Iliac crest grafting | No | 9 | No |
| 9 | Maxillectomy | No reconstruction | No | 6 | No |
| 10 | Enucleation | No reconstruction | No | 8 | Yes |
| 11 | Segmental mandibulectomy | Free fibula flap | No | 5 | No |
| 12 | Segmental mandibulectomy | Plating | Plate exposure | 11 | No |
| 13 | Segmental mandibulectomy | Free fibula flap | No | 6 | No |
| 14 | Segmental mandibulectomy | Free fibula flap | No | 7 | No |
| 15 | Enucleation | No reconstruction | No | 9 | Yes |
The average total operative time for patients requiring reconstruction by free tissue transfer was nine hours and 30 minutes. The average total operative time for patients reconstructed with bone graft or plating was three hours and 45 minutes. All patients had satisfactory speech, cosmesis and mastication.
Discussion
Ameloblastoma is a benign but locally invasive tumor with high rate of recurrence if not resected adequately. They rarely show metastasis. There are available case reports listing metastatic ameloblastoma and ameloblastic carcinoma [16, 17]. Metastatic ameloblastoma refers to a lesion which metastasizes but the histology of both primary and metastatic tissues are benign. However, ameloblastic carcinoma on the other hand has histological features of a carcinoma.
There are various methods of treatment of ameloblastoma which are broadly divided into two types that include a conservative approach such as enucleation and a radical approach with wide local excision and reconstruction. Recurrence is well known complication associated with inadequate treatment of ameloblastoma [18]. Considering lesser aggressiveness of this tumor, enucleation had been reported as adequate treatment for unicystic type of lesions and recurrence rate had been reported low [19]. However, it should be noted that a variant of unicystic ameloblastoma in which there is mural infiltration by epithelial cells is associated with higher recurrence rate and needs wide excision of lesion for adequate treatment [20, 21].
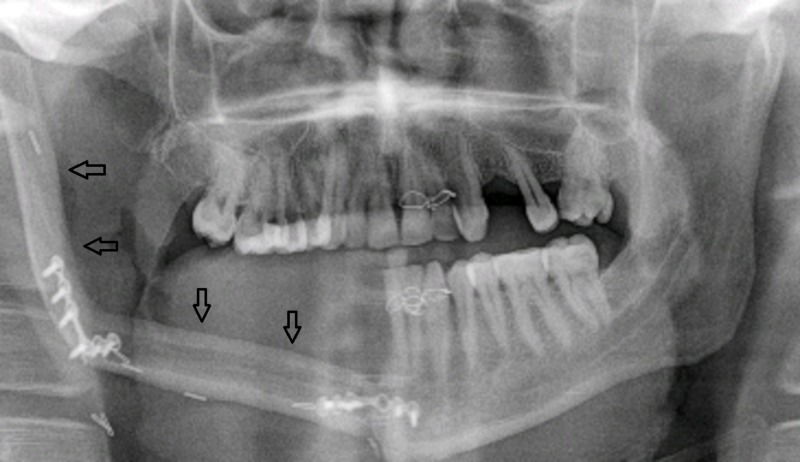
In contrast to unicystic variant, multicystic ameloblastomas have shown high incidence of recurrence. In literature, reported recurrence rates of such variant are considerably higher [22]. Preoperative OPG of a patient with multicystic ameloblastoma is shown in Figure 1.
Figure 1. Patient 14. A 38-year-old male with right-sided facial swelling. Preoperative orthopantomogram revealed multilocular lucencies (arrows) on the right side.
Segmental mandibulectomy with removal of 1-2 cm disease-free bone with immediate reconstruction is considered as an ideal treatment for ameloblastoma. This gives good cosmetic results and also addresses speech and eating problems [23]. Immediate reconstruction with use of plating is shown in Figure 2.
Figure 2. Patient 4. A 55-year-old male with left-sided facial swelling. Postoperative orthopantomogram shows reconstruction of mandible with plating (arrows).
The revolutions in the field of reconstructive microsurgery made free tissue transfer the method of choice for reconstruction of bony defect. In addition to covering large composite bony defects the free fibular flap also gives good aesthetic and functional outcomes with options for dental rehabilitation. Reconstruction of a mandibular defect with free fibular flap is shown in Figure 3.
Figure 3. Patient 11. A 31-year-old male. Postoperative orthopantomogram shows position of free fibular flap (arrows).
Conclusions
The management of ameloblastoma still poses a big challenge in spite of being the most common odontogenic tumor. In our study, we have found that segmental mandibulectomy with disease-free margin of around 1 cm and immediate reconstruction with free tissue transfer have shown good results.
Acknowledgments
I would like to express my deep gratitude to the following: Professor Mukhtar Ahmed Rajput, Muniba Siddiqui, Arsalan Ahmed Rajput, Muhammad Salar-e-Azam Rajput, Mariha Rajput
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Ameloblastoma. Mendenhall WM, Werning JW, Fernandes R, Malyapa RS, Mendenhall NP. Am J Clin Oncol. 2007;30:645–648. doi: 10.1097/COC.0b013e3181573e59. [DOI] [PubMed] [Google Scholar]
- 2.Ameloblastoma. Thompson LD. https://www.ncbi.nlm.nih.gov/m/pubmed/12610896/ Ear Nose Throat J. 2003;82:19. [PubMed] [Google Scholar]
- 3.Frequency of odontogenic cysts and tumors: a systematic review. Johnson NR, Gannon OM, Savage NW, Batstone MD. J Investig Clin Dent. 2014;5:9–14. doi: 10.1111/jicd.12044. [DOI] [PubMed] [Google Scholar]
- 4.Epidemiology of ameloblastomas of the jaws; a report from the Netherlands. Oomens MA, van der Waal I. Med Oral Patol Oral Cir Bucal. 2014;19:0. doi: 10.4317/medoral.20316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Immediate mandibular reconstruction with microsurgical fibula flap transfer following wide resection for ameloblastoma. Gerzenshtein J, Zhang F, Caplan J, Anand V, Lineaweaver W. J Craniofac Surg. 2006;17:178–182. doi: 10.1097/01.scs.0000190350.37978.2c. [DOI] [PubMed] [Google Scholar]
- 6.Recurrent ameloblastoma of the maxillo-facial region: clinical features and treatment. Adekeye EO, Lavery KM. J Maxillofac Surg. 1986;14:153–157. doi: 10.1016/s0301-0503(86)80282-x. [DOI] [PubMed] [Google Scholar]
- 7.Ameloblastoma—a locally destructive and invasive tumour—review of literature. Ruquaya M, Singh VP. Int J Otolaryngol Head Neck Surg. 2014;3:216–222. [Google Scholar]
- 8.Radiologic findings of diseases involving the maxilla and mandible. Underhill TE, Katz JO, Pope TL, Dunlap CL. AJR Am J Roentgenol. 1992;159:345–350. doi: 10.2214/ajr.159.2.1632353. [DOI] [PubMed] [Google Scholar]
- 9.Imaging of maxillomandibular ameloblastoma. Drevelengas A, Eleftheriadis J, Kalaitzoglou I, Palladas P, Lazaridis N. Eur Radiol. 1994;4:203–210. [Google Scholar]
- 10.Ameloblastomas with pronounced desmoplasia. Eversole LR, Leider AS, Hansen LS. http://www.ncbi.nlm.nih.gov/pubmed/6593446. J Oral Maxillofac Surg. 1984;42:735–740. doi: 10.1016/0278-2391(84)90423-3. [DOI] [PubMed] [Google Scholar]
- 11.Histopathology of ameloblastomas. Aisenberg MS. Oral Surg Oral Med Oral Pathol. 1953;6:1111–1128. doi: 10.1016/0030-4220(53)90223-0. [DOI] [PubMed] [Google Scholar]
- 12.Ameloblastoma: a clinical review and trends in management. McClary AC, West RB, McClary AC, et al. Eur Arch Otorhinolaryngol. 2016;273:1649–1661. doi: 10.1007/s00405-015-3631-8. [DOI] [PubMed] [Google Scholar]
- 13.Ameloblastoma in children and adolescents. Zhang J, Gu Z, Jiang L, Zhao J, Tian M, Zhou J, Duan Y. Br J Oral Maxillofac Surg. 2010;48:549–554. doi: 10.1016/j.bjoms.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 14.Recurrence rate following treatment for primary multicystic ameloblastoma: systematic review and meta-analysis. Almeida RA, Andrade ES, Barbalho JC, Vajgel A, Vasconcelos BC. Int J Oral Maxillofac Surg. 2016;45:359–367. doi: 10.1016/j.ijom.2015.12.016. [DOI] [PubMed] [Google Scholar]
- 15.Ameloblastoma of the jaws: a critical reappraisal based on a 40-years single institution experience. Hertog D, van der Waal I. Oral Oncol. 2010;46:61–64. doi: 10.1016/j.oraloncology.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 16.Ameloblastic carcinoma. Gunaratne DA, Coleman HG, Lim L, Morgan GJ. Am J Case Rep. 2015;16:415–419. doi: 10.12659/AJCR.893918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ameloblastic carcinoma of the maxilla: case report and review of the literature. Benlyazid A, Lacroix-Triki M, Aziza R, Gomez-Brouchet A, Guichard M, Sarini J. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:0. doi: 10.1016/j.tripleo.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 18.Mandibular ameloblastoma: a 28-years retrospective study of the surgical treatment results. Tamme T, Tiigimäe J, Leibur E. https://www.ncbi.nlm.nih.gov/pubmed/21217628. Minerva Stomatol. 2010;59:637–643. [PubMed] [Google Scholar]
- 19.Plexiform unicystic ameloblastoma. A variant of ameloblastoma with a low-recurrence rate after enucleation. Gardner DG, Corio RL. Cancer. 1984;53:1730–1735. doi: 10.1002/1097-0142(19840415)53:8<1730::aid-cncr2820530819>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 20.Establishing the natural history and growth rate of ameloblastoma with implications for management: systematic review and meta-analysis. Chae MP, Smoll NR, Hunter-Smith DJ, Rozen WM. PLoS One. 2015;10:0. doi: 10.1371/journal.pone.0117241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Unicystic ameloblastoma: a clinicopathologic study of 33 Chinese patients. Li TJ, Wu YT, Yu SF, Yu GY. https://www.ncbi.nlm.nih.gov/pubmed/11023100. Am J Surg Pathol. 2000;24:1385–1392. doi: 10.1097/00000478-200010000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Recurrence rates of intraosseous ameloblastomas of the jaws: a systematic review of conservative versus aggressive treatment approaches and meta-analysis of non-randomized studies. Antonoglou GN, Sándor GK. J Craniomaxillofac Surg. 2015;43:149–157. doi: 10.1016/j.jcms.2014.10.027. [DOI] [PubMed] [Google Scholar]
- 23.Oromandibular reconstruction using microvascular composite flaps: report of 210 cases. Urken ML, Buchbinder D, Costantino PD, Sinha U, Okay D, Lawson W, Biller HF. Arch Otolaryngol Head Neck Surg. 1998;124:46–55. doi: 10.1001/archotol.124.1.46. [DOI] [PubMed] [Google Scholar]