Abstract
Research has shown that children experience increased emotional distress when engaging in emotional caretaking of a parent. The current study is the first to examine this process in families in which the source of the stress is the child’s illness. Prospective associations were tested among mothers’ depressive symptoms near the time of their child’s cancer diagnosis, mothers’ expressed distress and their child’s emotional caretaking during an interaction task, and child anxious/depressed symptoms at one year post diagnosis. Families (N = 78) were recruited from two pediatric hospitals soon after their child’s (ages 5–18) new diagnosis or relapse of cancer. Mothers reported on their own depressive symptoms and their child’s anxious/depressed symptoms near the time of diagnosis or recurrence (Time 1) and one year later (Time 3). At Time 2 (4 months after Time 1) mother-child dyads completed a video-recorded discussion of their experience with cancer that was coded for observed maternal expressed distress (anxiety, sadness) and observed child emotional caretaking. Maternal expressed distress during the interaction was significantly related to more emotional caretaking behaviors by both boys and girls. Results of a moderated mediation model showed that child emotional caretaking at Time 2 significantly mediated the relation between maternal depressive symptoms at Time 1 and child anxious/depressed symptoms at Time 3 for girls, but not for boys. The findings suggest that children’s emotional caretaking behaviors contribute to subsequent anxious/depressed symptoms for girls, but not for boys, with cancer.
Keywords: pediatric cancer, communication, emotional caretaking, emotional distress, depressive symptoms
Over 12,500 children and adolescents are diagnosed with cancer each year in the United States (National Cancer Institute, 2013). Given the five year survival rate of over 80%, research exploring the psychological and interpersonal impact on survivors and their families is a high priority. Cancer diagnosis and treatment are inherently stressful for children and their families who are faced with multiple clinic and hospital visits, invasive and painful treatments, disruptions in family and daily life, and uncertainty about recurrence and long-term health outcomes (e.g., Rodriguez, Dunn, Zuckerman, Vannatta, Gerhardt, & Compas, 2012). Further, the diagnosis can be particularly stressful for parents, due to financial strain, traveling to and from the hospital, difficulties communicating about their child’s cancer diagnosis, and caring for their child (Compas et al., 2015; Cousino & Hazen, 2013; Rodriguez et al., 2012). Consequently, a subset of both children and parents are at an increased risk for emotional distress, including symptoms of anxiety and depression (Pai, Greenley, Lewandwski, Drotar, Youngstrom, & Peterson, 2007; Pinquart & Shen, 2011), which have been shown to be associated with maladaptive coping mechanisms and parent-child communication (Compas et al., 2014, 2015; Murphy et al., 2016).
Symptoms of emotional distress can have important interpersonal consequences, affecting patterns of communication between children with cancer and their parents (e.g., Murphy et al., 2016; Rodriguez et al., 2016). For example, Rodriguez et al. (2016) found that higher maternal depressive symptoms near the time of diagnosis were subsequently related to lower levels of maternal observed positive communication and higher levels of observed withdrawn and harsh communication during a video-recorded interaction task with their child. Further, Murphy et al. (2016) found that maternal posttraumatic stress symptoms near diagnosis predicted harsh communication during an parent-child interaction task three months later. This suggests that maternal distress can have downstream effects on communication with children in this population. Given that a portion of parents experience heightened symptoms of distress, it is possible that they may express their distress during the course of interactions with their child; however, prior research on parent communication in this population has not examined communication patterns related to parents’ anxiety and sadness specifically. There could be a direct relationship between maternal symptoms and child distress through processes of emotional contagion (Field, 1995; Tronick & Gianino, 1986) or parenting (Compas et al., 2010); however, the way a child responds and cares for the parent could also account for this relationship.
One potential correlate of parents’ verbal and nonverbal displays of emotional distress may be a tendency for children to respond with attempts to soothe or care for their parents (Champion et al., 2009). Symptoms of parental emotional distress, such as sadness, anxiety, and irritability, may result in increased soothing or comforting behaviors by children or adolescents in an attempt to care for their parent. In some instances, children may assume responsibility for the emotional needs of their parent or take on the emotional burden of their parent’ s problem. This includes displaying knowledge of parents’ emotional problems, offering solutions, or taking responsibility for these problems. This process is reflected in the concept of emotional caretaking, which refers to instances when a child attends to the emotional needs of the parent. Emotional caretaking is distinct from instrumental caretaking, in which a child assumes age-inappropriate household responsibilities or functionally takes on the role of the parent at home (Champion et al., 2009; Jurkovic, 1997). Other terms related to child caretaking behaviors have been used in the literature, including parentification and the parental child (e.g., Boszormenyi-Nagy & Spark, 1973; Minuchin, Montalvo, Guerney, Rosman, & Schumer; 1967); however, both of these constructs are more closely associated with instrumental rather than emotional caretaking as they highlight an increase in daily chores, hassles, and household responsibilities.
In one of the few empirical investigations of children’s emotional and instrumental caretaking directed at their parents, Champion et al. (2009) examined these processes in children of mothers with and without a history of depression. While children in both groups demonstrated similar levels of caretaking behaviors, caretaking was only associated with children’s symptoms of anxiety and depression for those who had a mother with a history of depression. Results from this study further indicated that emotional caretaking was more strongly associated with adolescents’ symptoms of anxiety and depression than instrumental caretaking, which is consistent with other research (Hooper et al., 2008, 2011; Jurkovic, 1997).
Despite possible differences in the effects of emotional and instrumental caretaking, child caretaking studies related to chronic illness have primarily focused on instrumental caretaking. Further, researchers in this area have primarily investigated these behaviors in families in which a parent has been diagnosed with an illness. For example, with respect to caretaking behaviors in children of parents diagnosed with AIDS, greater AIDS-related illness was associated with higher adolescent parentification and instrumental caretaking, which predicted higher levels of adolescent internalizing and externalizing problems (Stein, Riedel, & Rotheram-Borus, 1999). Child gender did not affect the association between caretaking and their adjustment; however, adolescents reported doing more chores when they had a mother relative to a father with AIDS. In a study of adolescents of parents with cancer, Grant and Compas (1995) studied how adolescents responded to stress related to their parents’ diagnosis and found that girls reported more instrumental caretaking behaviors than boys, and caretaking was associated with anxious/depressed symptoms for girls but not for boys.
Other studies of child emotional caretaking have also found gender differences in the association between caretaking behaviors and internalizing symptoms. Models of gender socialization suggest that girls are socialized to be more caring and nurturing (Wethington, McLeod, & Kessler, 1987), which could have downstream effects on how emotional caretaking is related to their emotional wellbeing. Prior research has shown that females experience a higher cost of parentification and caretaking with respect to internalizing symptoms compared to males (e.g., Jurkovic, 1997; Wethington et al., 1987). Girls are also more likely to be involved in all types of caretaking (e.g., Byng-Hall, 2008; Dearden & Becker, 2004), although a recent study with undergraduate students found that boys reported higher levels of childhood parentification compared to girls (Hooper, Tomek, Bond, & Reif, 2015). Nevertheless, much of the research investigating caretaking behaviors has relied on retrospective self-reports from young adults and college-aged students, examining distress and caretaking concurrently (e.g., Hooper et al., 2015; Jankowski, Hooper, Sandage, & Hannah, 2013). Building on these studies, longitudinal designs and multimethod assessments are important to better understand how child caretaking is associated with later emotional distress and how this association may be moderated by child gender.
While research on child caretaking has been conducted in populations in which the parent has a chronic mental or physical illness (e.g., parents diagnosed with depression, AIDs, and cancer), the emotional caretaking process has yet to be examined in families in which the source of the stress is the child’s illness. It is plausible that child caretaking may also occur in families in which the child is chronically ill. This is especially salient for pediatric cancer, as a child’s cancer diagnosis is associated with increased emotional distress among some parents. If parents express this distress to their child during the course of parent-child interactions, it may pull for emotional caretaking in their children. Given the toll that cancer takes on children’s physical health, instrumental caretaking and other forms of parentification may be less common, but emotional caretaking may still occur. Therefore, emotional caretaking may be a more important construct to assess in this pediatric population.
There are several other factors that could influence the relationship between emotional caretaking and child symptoms in this population. Prior research using this sample has found that children’s use of secondary control coping (i.e., cognitive reappraisal, acceptance, and positive thinking) near the time of diagnosis is related to their anxious/depressed symptoms concurrently and longitudinally (Compas et al., 2014; Compas et al., under review). Additionally, maternal depression and child age have also been found to be related to child symptoms in pediatric cancer and other child and adolescent populations (Compas et al., 2015; Goodman, Rouse, Connell, & Broth, 2011).
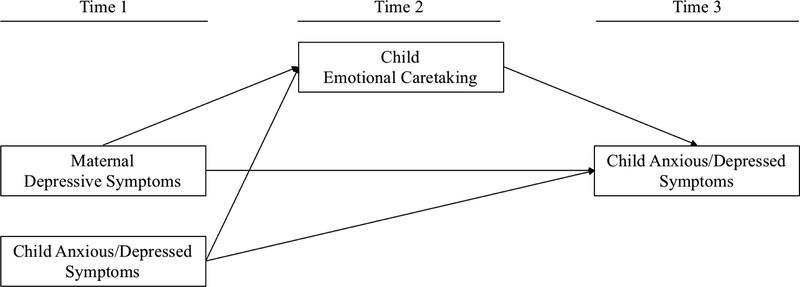
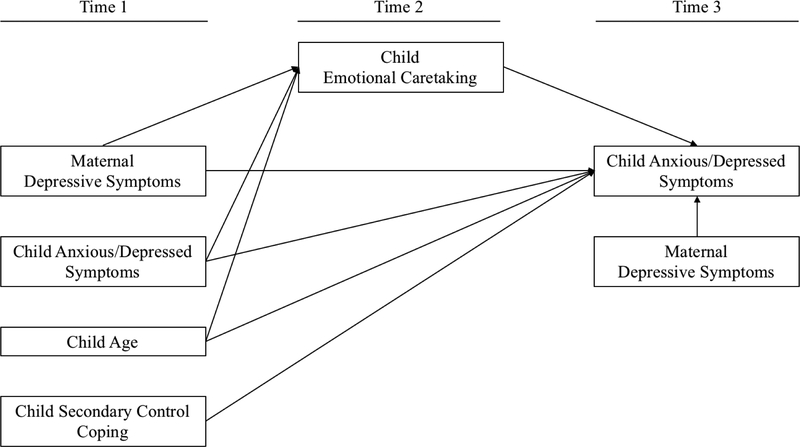
This multi-method prospective study included observations of both expressed maternal distress and child caretaking behaviors during mother-child discussions about the child’s cancer, as well as mothers’ reports of their own and their child’s distress. We focused on mothers because of their higher involvement caring for their children with cancer and the larger association among maternal caregiving and child psychopathology (Connell & Goodman, 2002). Mothers reported on emotional distress an average of two months after the child’s diagnosis or recurrence (Time 1), mothers and children were observed discussing the child’s cancer approximately four months after Time 1 (Time 2), and children self-reported distress approximately 12 months after Time 1 (Time 3). The purpose of this study was to examine the concurrent relation between observations of mothers’ expressed distress and children’s emotional caretaking behaviors during video-recorded mother-child discussions of the child’s cancer, examine mothers’ reported distress at T1 and children’s emotional caretaking at T2 as predictors of children’s distress at T3 and to examine child gender as a moderator of these associations. We hypothesized that: (1) Maternal expressed distress during interactions with their children would be positively related to child emotional caretaking concurrently at T2, indicating that these behaviors co-occur. (2) Maternal depressive symptoms at T1 would be positively related to child emotional distress one year later at T3, and child emotional caretaking at T2 would mediate this association for girls but not for boys. The conceptual model that was tested in both girls and boys is presented in Figure 1a. Additional analyses were conducted to determine if child emotional caretaking remained a moderator after controlling for other variables that have been shown to predict child anxious/depressed symptoms, shown in Figure 1b.
Figure I.
Models of emotional caretaking as a mediator in the relation between maternal depressive symptoms and child anxious/depressed symptoms controlling for (a) child anxious/depressed symptoms at T1, (b) child age at T1, child secondary control coping at T1, and maternal depressive symptoms at T3
Method
Participants
Participants included 78 children diagnosed with cancer and their mothers. Children were on average 10.35 years old (SD = 3.67; range 5 to 17), and 45% were female. Sixty-seven (86%) were European American, 7 (9%) African American, 1 (1%) American Indian, and the remainder reported ‘Other’ for their race. Five children (6.4%) were Hispanic/Latino. Cancer diagnoses included leukemia (44%), lymphoma (18%), brain tumor (6%), and other solid tumor (32%). At one-year follow-up, 34 (43%) were still receiving treatment. Mothers were on average 38.68 years old (SD = 7.52), and education level ranged from high school to graduate school (M = 3 years of college or trade school). Families reported a range of annual household income (24%: $25 000 or less; 23%: $25,001–50,000; 17%: $50,001–75,000; 13%: $75,001–100,000; 22%: $100,001 or above).
Procedure
Families were recruited for a longitudinal study examining family adjustment to childhood cancer from two large pediatric oncology centers in urban areas of the Southern and Midwestern United States. All study procedures were approved by the Institutional Review Boards of the participating academic medical centers. Inclusion criteria required families to have a child: (a) between 5–17 years old (b) with a new cancer diagnosis or recent recurrence, (c) receiving treatment through the oncology division, and (d) with no developmental disability (i.e., intellectual disability), although no participants were excluded for this reason. Eligible families were identified by members of the pediatric oncology medical team, and medical personnel introduced the study to caregivers. After receiving verbal consent to be approached by a member of the research team, families were given additional information and were recruited for participation if interested. Participants provided informed consent/assent for the video-recorded observation, in addition to completing questionnaires near the time of diagnosis or recurrence and approximately one year later.
At T1, 2 months (M = 59.56 days, SD = 43.00 days, Range = 8 to 269 days) after the child’s cancer diagnosis or recurrence, mothers completed self-report questionnaires of emotional distress and mothers completed measures of child distress and reported family demographic characteristics. Four months later (M = 111.44 days after T1, SD = 71.78 days, Range = 7 to 267 days; T2), families were approached to participate in an optional videorecorded observation of a discussion between the mother and child about the child’s diagnosis or recurrence and treatment. At T3, on average 1 year after T1 (M = 349.79 days after T1, SD = 51.52 days, Range = 172 to 497 days), mothers completed the same questionnaires they completed at T1. Days from diagnosis or recurrence to T1, from T1 to T2, and from T2 to T3 were not correlated with any of the variables in the current analysis.
For inclusion in current analyses, mother-child dyads completed assessments at T1 and T3, as well as the observation at T2. 325 mothers completed questionnaire measures at T1 and 219 mothers completed questionnaires at T3. Of the 218 mothers that completed both T1 and T3 questionnaires, 89 mother-child dyads participated in the observation. Reasons for declining the observation included lack of time, not wanting to be video-recorded, and lack of interest. Families were excluded from current analyses if the interaction video and questionnaire measures were completed on the same day (n = 6), or if the follow-up measures were completed more than 1.5 years post-diagnosis or recurrence (n = 5). Families included in the analyses did not significantly differ from those who were excluded on child age, mother age, child race, child ethnicity, child gender, family income, relapse status, maternal distress at either time point, or child anxious/depressed symptoms at T3. Children in families who were included in the analyses, however, had significantly higher anxious/depressed symptoms at T1 (M = 55.04, t(312) = −2.11, p = .035) relative to families who were excluded (T1: M = 53.48). Primary study variables among families who were included in the current analyses did not differ across cancer type or initial diagnosis versus relapse status. Further, study variables were not correlated with mother-reported chance of treatment success.
Observations took place in a private room at the hospital or laboratory space. During the observation, graduate-level research assistants read from a standardized script that told mothers and children that “we are interested in understanding how parents and children talk about cancer and its treatment. We would like you and your child to talk in the way you might talk if you were having a discussion at home or privately in the hospital about your child’s illness and its treatment.” Mothers were given a card with written prompts (e.g., What have we each learned about cancer and how it is treated? What parts of your cancer and its treatment have been the hardest for each of us? What kinds of feelings (or emotions) have we each had since we found out you have cancer? What are the ways we each try to deal with these feelings and emotions?) to help guide the conversation as needed, and the research assistant left the room for the mother-child dyad to complete the discussion. All families used at least one written prompt. The research assistant returned and debriefed the participants to address any potential questions or distress after 15 minutes. In the event that a family expressed severe distress that was not decreased by the briefing process, the research assistant inquired about their desire to seek family counseling to help with talking about difficult topics. Research assistants had access to a resource sheet with contact information on several family counselors in the area, and families were referred to one of these counselors if they expressed interest. Families were compensated with checks or gift cards at each time point.
Measures
Family Demographic Characteristics.
Mothers reported child age and race/ethnicity, and self-reported age, family income, and educational attainment.
Medical Information.
Child cancer diagnoses and treatment information were obtained from medical records.
Maternal Depressive Symptoms.
The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) was completed by all mothers at T1 and T3. The BDI-II has been widely used to assess the typical attitudes and symptoms presented by depressed individuals over the previous two weeks. The BDI-II has been shown to have excellent reliability, with an internal consistency of α = .91 and test-retest reliability of α = .93 (Beck, Steer, & Brown, 1996). In the current sample, internal consistency was α = .93.
Child Anxious-Depressed Symptoms.
The Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001) was completed by mothers to assess their perception of the child’s internalizing problems over the past 6 months. The measure has strong test-retest reliability with coefficients ranging from .78 to .88, and criterion-related validity has been established for children aged 11 to 18 (Achenbach & Rescorla, 2001). In these analyses, we used the Anxious/Depressed syndrome scale as the best representation of child’s anxiety-depression symptoms. This subscale has been used frequently in pediatric cancer to avoid confounding with other scores that include somatic complaints common to treatment for cancer (Pinquart & Shen, 2011). Internal consistency for this scale was α = .74 at T1 and α = .86 at T2.
Observed Maternal Expressed Distress.
The Iowa Family Interaction Scale (IFIRS; Melby & Conger, 2001) is a macro-level system used to code an individual’s verbal and nonverbal communication, behaviors, and emotions from 1 (absent) to 9 (mainly characteristic) throughout an interaction. Intensity, frequency, and contextual or affective nature of the behavior, as well as age of the child are taken into consideration during scoring. Trained graduate and undergraduate research assistants were required to pass a written test of code definitions and clarifications with 90% accuracy and reach 80% reliability on previously coded videos prior to coding new interactions. All videos were double-coded by two coders, who then met to reach consensus. As specified within the IFIRS manual, higher scores were used when ratings differed by a single point, and ratings that differed by more than two points were resolved through discussion. Identical scores from raters and scores that differed by only one-point constituted as agreement. On average, interrater reliability determined prior to rater consensus was 77% (SD = 10.26) across all maternal codes and 76% (SD = 13.04) across child codes.
We used the IFIRS system to code a video-recorded 15-minute conversation between mothers and their children about cancer diagnosis or recurrence and treatment. For this study, an expressed maternal distress composite code was created by averaging two maternal codes (sadness and anxiety). Code definitions and examples are found in Table 1.
Table 1.
Codes, Definitions, and Descriptive Statistics for Maternal Expressed Distress and Child Emotional Caretaking
| Code | Definition | Examples | Mean (SD) | Range | |
|---|---|---|---|---|---|
| Maternal Expressed Distress | |||||
| Anxiety (Macro) | Emotional distress that is conveyed as nervousness, fear, tension, stress, worry, and concern. | Trembling or tense body movements and verbal statements that express fear of the future ‘I’m worried about what will happen if I have to keep leaving work to come to the hospital’ |
4.77 (1.62) | 1–8 | |
| Sadness (Macro) | Emotional distress that is conveyed as sadness, unhappiness, despondency, depression, and regret. | Crying or appearing down and negative verbal statements ‘I’ve been so sad ever since you got sick’ | 4.97 (1.40) | 1–8 | |
| Child Emotional Caretaking | |||||
| Emotional Caretaking (Macro) | The child takes care of the emotional needs of the mother or takes on an emotional burden that may be age-inappropriate. | Lower levels: displays knowledge of the mother’s problems or difficulties; at higher levels: offer solutions for the mother’s emotional problems or take responsibility for the mother’s difficulties. ‘I know staying in the hospital has been really hard on you.’ | 1.55 (1.16) | 1–7 | |
| Backchannels (Micro) | The number of utterances the child makes to acknowledge the mother’s conversational contributions or to prompt her to continue. | Positive affirmations of what the mother is saying, including nodding as well as verbal statements. ‘Mhm’ ; ‘Of course it has’ ; nods | 0.82 (2.42) | 0–13 | |
Note: Macro codes from Iowa Family Interaction Rating Scales (range 1–9), Micro codes from Contingency Coding System (count data).
Observed Child Emotional Caretaking.
For this study, child emotional caretaking was captured with a composite of two codes: a macro-level code based on the IFIRS manual and definitions from previous research on emotional caretaking (Champion et al., 2009; Broszormenyi-Nagy & Spark, 1973; Jurkovic, 1997) and a micro-level code from the Contingency Coding System (CCS; Rodriguez et al., 2013). Using both macro- and micro-level codes allows for sensitivity in coding interactions (Rodriguez et al., 2013; Murphy et al., 2016). The emotional caretaking composite score was created by averaging a macro-code from IFIRS (emotional caretaking) and one micro-code (backchannels) from CCS.
As discussed above, the IFIRS coding system provides measures of verbal and nonverbal communication throughout the entire interaction, and child scores are not contingent on parent behaviors. Children received ratings on the emotional caretaking IFIRS code when they expressed emotional support or concern for their mother regardless of whether or not mom expressed distress. Micro-level coding is based on transcribing and coding individual parent and child utterances. The CCS was developed within a sample of children diagnosed with cancer (e.g., Murphy et al. 2016; Rodriguez et al., 2013). All observations were first transcribed and then coded by trained undergraduate and graduate coders who achieved 90% accuracy on a written test of code definitions and reached 80% reliability during training. Observations were coded using printed transcripts independently by two coders who met to reach consensus. The backchannels code was used as one measure of child emotional caretaking, as it quantifies how children encouraged their mother to disclose their experience and their emotions through both verbal and nonverbal encouragers that were directly contingent on an utterance by the mothers. See Table 1 for code definitions and examples. The distributions for emotional caretaking and backchannels were positively skewed, so each variable was mean-centered and transformed into a z-score prior to creating the composite code.
Data Analyses
Independent samples t-tests were conducted in order to test for gender differences between boys and girls. Bivariate Pearson correlations were conducted as a first step in examining associations among variables. We used AMOS to test a two-group path analytic model to evaluate the hypothesized mediating effect of child emotional caretaking on the association between maternal depressive symptoms and child anxious/depressed symptoms, controlling for symptoms at T1, for boys and girls. The current analyses were conducted with a 95% confidence interval for the indirect effect with 10,000 bootstrap samples. Due to our a priori hypotheses regarding gender differences and the direction of effects, separate conditional indirect effects were assessed for girls and boys and one-tailed tests of significance were used throughout the correlation and path analyses.
Supplemental analyses were also conducted using additional covariates that have been shown to predict child emotional distress cross-sectionally and longitudinally, and may have accounted for additional variance in symptoms in the current analyses. Child secondary control coping at T1, age at T1, and maternal depressive symptoms at T3 were added to the AMOS path analytic models to evaluate if child emotional caretaking remained a significant moderator of the association between maternal depressive symptoms at T1 and child axious/depressed symptoms at T3.
Results
Descriptive Statistics
Descriptive statistics for maternal expressed distress and their associated code definitions are in Table 1. Girls did not significantly differ from boys in their levels of emotional caretaking behaviors (t(76) = .21, p = .837). When examining descriptive statistics for girls and boys separately, mothers’ level of expressed distress during the interaction task did not significantly differ based on child gender (girls, M = 5.06, SD = 1.29; boys, M = 4.72, SD = 1.32; t(76) = 1.13, p = .262).
The mean for maternal depressive symptoms and child anxious/depressed symptoms at both timepoints fell in the mild and moderate ranges, respectively. Means, standard deviations, and results of independent samples t-tests for maternal depressive symptoms and child anxious/depressed symptoms by gender are presented in Table 2. There were no significant differences in maternal depressive symptoms at T1 and child anxious/depressed symptoms at T3 between girls and boys. However, boys had significantly higher anxious/depressed symptoms at T1 relative to girls.
Table 2.
Means and Standard Deviations for Measures of Distress at T1 and T3 with Independent Samples t-Tests comparing girls and boys.
| Girls | Boys | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t(76) | 95% CI | |
| T1 | ||||||
| Maternal Depressive Symptoms | 14.84 | 10.81 | 13.33 | 9.28 | .658 | −3.05 to 6.07 |
| Child Anxious/Depressed Symptoms | 53.34 | 4.58 | 56.56 | 7.33 | −2.29* | −6.09 to −0.35 |
| T3 | ||||||
| Child Anxious/Depressed Symptoms | 54.83 | 6.50 | 56.71 | 9.06 | −1.03 | −5.53 to 1.76 |
p<.05. Maternal Depressive Symptoms are measured with the Beck Depression Inventory-II. Child Anxious-Depressed scores measured with the Child Behavior Checklist are standardize T-scores (M = 50, SD = 10).
T1 occurred about 2 months after diagnosis or recurrence.
T3 occurred about 1 year after T1.
Bivariate Correlations by Gender
Bivariate correlations are shown for boys and girls separately in Table 3. For both girls and boys, mothers’ expressed distress during the interaction was significantly, positively related to their child’s emotional caretaking concurrently during the parent-child interaction task. This indicates that maternal expressed distress and child caretaking co-occurred during the interaction task for both sons and daughters. In addition, depressive symptoms at T1 for mothers of both boys and girls were significantly related to maternal depressive symptoms at T3 and children’s anxious-depressed symptoms at T3. Baseline maternal depressive symptoms, maternal expressed distress, child emotional caretaking, and child anxiety-depressed symptoms were all significantly correlated for girls; whereas only mothers’ depressive symptoms at T1 and child anxious/depressed symptoms were significantly correlated for boys.
Table 3.
Correlation Matrix by the Gender of the Child
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Mothers’ Depressive Symptoms at T1 | -- | .39* | .35* | .71*** | .74*** |
| 2. Mothers’ Expressed Distress at T2 | −.11 | -- | .61*** | .38* | .20 |
| 3. Child Emotional Caretaking at T2 | .15 | .39** | -- | .42** | .12 |
| 4. Child’s Anxious/Depressed Symptoms at T3 | .29* | −.10 | −.02 | -- | .75*** |
| 5. Mothers’ Depressive Symptoms at T3 | .40** | .01 | .04 | .31* | -- |
Correlations for boys (n = 43) are presented below the diagonal; Correlations for girls (n = 35) are presented above the diagonal.
p < .10,
p < .05,
p < .01,
p <.001; with one-tailed tests of significance.
Indirect Effects by Gender
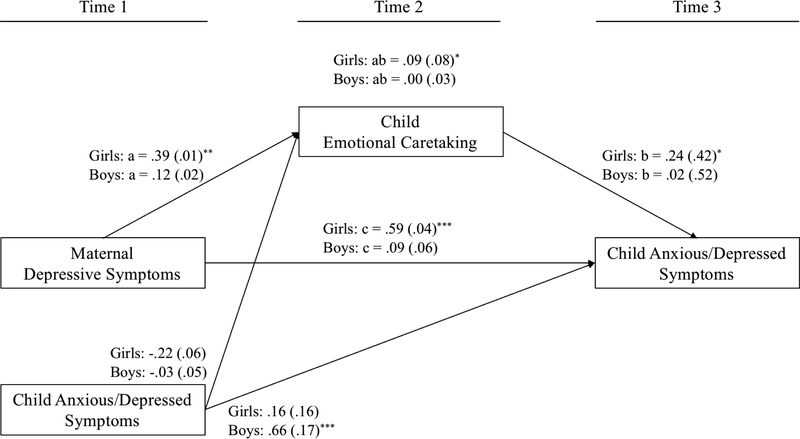
To test the mediation effects of emotional caretaking, we conducted a two-group (male and female) model in which T2 child emotional caretaking mediated the relation between T1 maternal depressive symptoms and T3 child anxious/depressed symptoms, while controlling for T1 child anxious/depressed symptoms. The model and all unstandardized path coefficients are presented in Figure I. For girls (Figure 1a), the path from T1 maternal depressive symptoms to T2 child emotional caretaking was significant (path a). The path coefficient from T2 child emotional caretaking to T3 child distress symptoms was also significant (path b). Further, there was a significant coefficient for the direct effect (path c) from T1 maternal depressive symptoms to T3 child distress at. Further, T1 child anxious/depressed symptoms was not a significant predictor of either emotional caretaking at T2 or anxious/depressed symptoms at T3. Finally, analyses showed that there was a significant indirect effect of T1 maternal distress on girls’ T3 depressive symptoms through T2 child emotional caretaking (path ab).
The model for boys is also described in Figure II. Neither path a, from T1 maternal depressive symptoms to T3 child emotional caretaking; path b, from T2 emotional caretaking to T3 child distress; nor path c, from T1 maternal depressive symptoms to T3 child distress, were significant for boys. Child anxious/depressed symptoms at T1, however, was a significant predictor of symtoms one year later. Although there was a significant mediator effect of emotional caretaking for girls, emotional caretaking did not mediate the relationship between maternal distress and child symptoms for boys (path ab). Model 14 of PROCESSmacro (Hayes, 2013, 2015) was used to test a significant difference in the indirect effect for girls and boys. The index of moderation showed that the test of moderated mediation was not significant (Index unstd. B = −.03, Bootstrap SE = .03, 95% CI −.11, to .00).
Figure II.
Direct and indirect effects of maternal depressive symptoms on child symptoms of anxiety and depression through child emotional caretaking, controlling for child scores on the Anxious/Depressed CBCL syndrome scale at T1 for girls and boys. Standardized regression path coefficients (βs) with standard errors in parentheses. *p < 05; **p < .01; ***p < .001; with one tailed tests of significance.
Supplemental Analyses with Additonal Covariates
Supplemental analyses controlling for additional covariates showed that, for girls, child age did not significantly predict emotional caretaking at T2 (β = .15, SE = .04, p = .162) or child anxious/depressed symptoms at T3 (β = −.05, SE = .08, p = .308), and child secondary control coping at T1 was not a significant predictor of child anxious/depressed symptoms at T3 (β = − .09, SE = 4.78, p = .193) in the presence of the other variables in the model. Maternal depressive symptoms at T3, however, was significantly related to child anxious/depressed symptoms at T3 (β = .65, SE = .03, p < .001) and maternal depressive symptoms at T1 was no longer a significant predictor (c’ path; β = .15, SE = .03, p = .099). Nevertheless, there remained a significant a path from maternal depressive symptoms to child emotional caretaking (β = .39, SE = .01, p = .007), b path from child emotional caretaking to child anxious/depressed symptoms (β = .34, SE = .35, p = .002), and mediator effect of emotional caretaking on the association between maternal and child anxious/depressed symptoms (path ab: β = .13, Bootatrap SE = .09, p = .016).
For boys, the only significant predictor of child anxious/depressed symptoms at T3 was from child anxious/depressed symptoms at T1 (β = .69, SE = .17, p < .001). Child age (β = −.10, SE = .16, p = .192), child secondary control coping at T1 (β = .01, SE = 9.53, p = .471), and maternal depressive symptoms at T3 (β = .09, SE = .06, p = .216) were all nonsignificant predictors of child anxious depressed symptoms at T3. Further, child age at T1 did not significantly predict emotional caretaking behaviors (β = .01, SE = .05, p = .074). Similar to Model 1, child emotional caretaking did not moderate the relation between maternal and child symptoms (path ab: β = .01, Bootatrap SE = .05, p = .332).
Discussion
Pediatric cancer is stressful for children and their caregivers, and this experience can lead to increased emotional distress for some family members near the time of diagnosis or recurrence and into survivorship (Pai et al., 2007; Pinquart & Shen, 2011). This study presents new insight into how maternal depressive symptoms and expressed distress, along with child emotional caretaking, are associated with child emotional distress over time for children with cancer. Similar to previous studies, children and their mothers had mildly to moderately elevated levels of distress near the time of diagnosis (e.g., Compas et al., 2014, 2015). As hypothesized, mothers expressed moderate levels of distress (verbally and/or nonverbally) to their child during the interaction, and mothers’ expression of anxiety and sadness was related to higher levels of child emotional caretaking concurrently. It is striking that despite having cancer, a portion of this sample of children still engaged in emotional caretaking of their mothers. The presence of emotional caretaking may suggest that some children assume responsibility for their mother’s distress, creating a challenge to concurrently juggle efforts to care for their mother alongside their attempts at coping with their own stressors and distress. Maternal depressive symptoms at T1 were also significantly related to maternal expressed distress and child emotional caretaking for girls, but not for boys. These findings suggest that while both boys and girls may respond similarly to content and body language during mother-child communication, girls may be additionally affected by displays of maternal symptoms of depression that were not captured in these interactions.
We tested child emotional caretaking as a mediator in the association between maternal depressive symptoms near the time of diagnosis or recurrence and child emotional distress one year later. Maternal depressive symptoms near the time of child cancer diagnosis were significantly related to child emotional caretaking and anxious/depressed symptoms one year later for girls, but not for boys. Boys and girls did not differ in levels of emotional caretaking during the interaction task; however, there was a differential association between caretaking with their own distress eight months later, such that emotional caretaking was significantly related to child distress for girls only. Findings from the mediation analyses showed that child emotional caretaking significantly mediated the relationship between maternal depression at diagnosis or recurrence and child emotional distress one year later for girls, but not boys. This was true when controlling for children’s anxious/depressed symptoms, secondary control coping, childage at T1, and maternal depressive symptoms at T3; providing a very stringent test of these associations. This finding also suggests that, for boys, child symptoms near diagnosis were more stable predictors of their anxious/depressed symptoms one year later given the other variables in the model. Despite the relatively low mean levels of emotional caretaking behavior during the video-recorded interaction task, these findings indicate that even low levels of caretaking can have significant implications for girls’ wellbeing.
Previous research has suggested that girls are more likely to take on caretaking roles, and they are more likely to be affected by this additional stress and responsibility when the parent is emotionally or physically ill (e.g., Champion et al., 2009; Grant & Compas, 1995; Wethington et al., 1987). Results show that boys and girls with cancer are equally likely to engage in emotional caretaking in response to maternal expressed distress, yet girls may be more adversely affected than boys. This gender difference is consistent with models of gender socialization, such that girls are socialized to be more caring and nurturing (Wethington et al., 1987). Because this is the first study to assess child emotional caretaking in families in which the child has a significant health problem, it is not possible to assess if this pattern is unique to children with cancer relative to other physical or mental health concerns. Future research should evaluate the effect of these behaviors in other populations to better understand how caretaking behavior is related to child distress when the child has an emotional or physical illness.
This study also adds to the emerging literature on communication in families of children with cancer that use direct observation of parent-child interactions. A recent review indicated that family communication in pediatric populations is impaired compared to communication in families with typically developing children (Murphy, Murray, & Compas, 2017). Further, in pediatric cancer, parents have identified communicating with their child about the diagnosis as a significant source of stress (Rodriguez et al., 2011). Prior research has shown that near the time of diagnosis, depressive symptoms in mothers of children with children with cancer are associated with higher levels of negative communication and lower levels of positive communication (Rodriguez et al., 2013), and that mothers’ posttraumatic stress symptoms near diagnosis are associated with more harsh communication (Murphy et al., 2016). Although the given prompts may have shaped the conversation and pulled for emotional caretaking to a degrees, the current study extends these findings by providing evidence of how maternal distress is associated with mother-child dyadic communication and, consequently, child adjustment.
The current study had several methodological strengths. First, we used a longitudinal and multimethod design that included both nationally-standardized questionnaire and observational measures. We were able to conduct a prospective analysis of key variables near the time of diagnosis, during mother-child interactions, and at one year follow-up. Second, this study improves on much of the recent research on emotional caretaking, which focus on college samples using retrospective designs and self-report measures (e.g., Hooper et al., 2011, 2015). Third, research on child emotional caretaking has been predominately limited to families in which a parent has a physical illness or psychiatric diagnosis, whereas this study provides evidence that caretaking behaviors can also occur when the child is ill.
There are several limitations that can be addressed in future research. First, because a portion of the children were too young to complete questionnaires, we used only mothers’ reports on child symptoms of emotional distress near the time of diagnosis and one year later. Maternal distress may influence their perception and reports of their child’s distress. Although the primary study hypotheses were supported when controlling for maternal distress at T2, multi-informant studies are the gold-standard when using questionnaire mesures of internalizing symptoms (Achenbach & Rescorla, 2001). Second, the sample was also predominantly composed of European American mother-child dyads, meaning that the findings of this study may not generalize to families of other racial or ethnic backgrounds. In addition, this study only analyzed mother-child dyads, and we did not assess how children may engage in emotional caretaking with their fathers. Future research would benefit from child self-report measures, a more diverse sample, and the use of father-child dyads. Third, there was considerable variabilty in the length of time between each assessment across the parent-child dyads. Finally, due to the moderate sample size, we did not achieve power to detect differences in boys and girls; a larger sample would provide power to conduct tests of moderated mediation that may be more sensitive to child gender.
In summary, results show that maternal distress near the time of child cancer diagnosis is related to child emotional caretaking four months later and distress one year later, particularly for girls. In addition, child emotional caretaking was concurrently related to maternal expressed distress during the video-recorded interaction. These findings suggest three targets for interventions. First, reducing maternal distress, including symptoms of depression, may have downstream effects of child wellbeing. Further, it may also be important to assist parents in their communication about cancer with their child. This could either have a direct effect on the child’s wellbeing, or it could influence wellbeing by reducing the amount of emotional caretaking that the child assumes. Although emotional caretaking was moderately related to maternal expressed distress, children might still provide these caretaking behaviors in the absence of maternal expressions of emotional distress. Perceived or assumed distress could also encourage children, and particularly girls, to provide emotional caretaking and support. Clinicians chould be encouraged to provide psychoeducation to parents on the differential effect of parental distress on girls and boys’ wellbeing. They could also advise parents to discuss the relative emotional responsibilities with their child throughout their treatment, making it clear that the burden of caring does not fall on the child. Finally, clinicians could consider assessing and targeting child emotional caretaking behaviors, especially in girls. Results from this study may inform future family-based interventions to bolster resilience in response to pediatric cancer by reducing maternal distress, strengthening positive maternal communication, and reducing emotional caretaking behaviors in children.
Acknowledgments
Funding
This work was supported by grants from the National Cancer Institute (R01CA118332; R01CA118332–07), a training grant from the National Institute of Mental Health (T32-MH18921), and a gift from Patricia and Rodes Hart.
References
- Achenbach TM, & Rescorla LA (2001). Manual for the ASEBA school-age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families. [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck Depression Inventory Manual (2nd ed). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Boszormenyi-Nagy I, & Spark GM (1973). Invisible loyalties: Reciprocity in intergenerational family therapy. Hagerstown, MD: Harper & Row. [Google Scholar]
- Byng-Hall J (2002). Relieving parentified children’s burden in families with insecure attachment patterns. Family Process, 41(3), 375–388. [DOI] [PubMed] [Google Scholar]
- Champion JE, Jaser SS, Reeslund KL, Simmons L, Potts JE, Shears AR, & Compas BE (2009). Caretaking behaviors by adolescent children of mothers with and without a history of depression. Journal of Family Psychology, 23(2), 156–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Bemis H, Gerhardt CA, Dunn MJ, Rodriguez EM, Desjardins L, Preacher KJ, Manring S, & Vannatta K (2015). Mothers and fathers coping with their child’s cancer: Individual and interpersonal processes. Health Psychology, 34, 783–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Champion JE, Forehand R, Cole DA, Reeslund KL, Fear J, Hardcastle J, Keller G, Rakow A, Garai E, Merchant MJ, & Roberts L (2010). Coping and Parenting: Mediators of 12-month outcomes of a family group cognitive-behavioral preventive intervention with families of depressed parents. Journal of Consulting and Clinical Psychology, 78(5), 623–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Desjardins L, Vannatta K, Young-Saleme T, Rodriguez EM, Dunn M, Bemis H, Snyder S, & Gerhardt CA (2014). Children and adolescents coping with cancer: Self- and parent-reports of coping and anxiety/depression. Health Psychology, 33, 853–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Vannatta K, Murphy LK, Bemis H, Desjardins L, … & Gerhardt CA (2018). Children and Adolescents Coping with the Stress of Cancer: A Longitudinal Multi-Informant Study. Manuscript under review.
- Connell AM, & Goodman SH (2002). The association between psychopathology in fathers versus mothers and children’s internalizing and externalizing behavior problems: A meta-analysis. Psychological Bulletin, 128(5), 746–773. [DOI] [PubMed] [Google Scholar]
- Cousino MK, & Hazen R. a. (2013). Parenting stress among caregivers of children with chronic illness: A systematic review. Journal of Pediatric Psychology, 38(1465–735X (Electronic)), 809–828. [DOI] [PubMed] [Google Scholar]
- Dearden C, & Becker S (2004). Young carers in the UK: The 2004 report. London: Carers UK. [Google Scholar]
- Dunn MJ, Rodriguez EM, Miller KS, Gerhardt C a, Vannatta K, Saylor M, … Compas BE (2011). Direct Observation of Mother - Child Communication in Pediatric Cancer : Assessment of Verbal and Nonverbal Behavior and Emotion. Journal of Pediatric Psychology, 36(5), 565–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field T (1995). Psychologically depressed parents In Bornstein MH (Ed.), Handbook of parenting: Vol. 4. Applied and practical parenting. Mah- wah, NJ: Erlbaum. [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, & Broth MR (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review, 14(1), 1–27. [DOI] [PubMed] [Google Scholar]
- Grant KE, & Compas BE (1995). Stress and anxious-depressed symptoms among adolescents: searching for mechanisms of risk. Journal of Consulting and Clinical Psychology, 63(6), 1015–1021. [DOI] [PubMed] [Google Scholar]
- Harper FW, Peterson AM, & Uphold H (2013). Longitudinal study of parent caregiving self-efficacy and parent stress reactions with pediatric cancer treatment procedures. PsychoOncology, 22(7), 1658–1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). An introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford Press. [Google Scholar]
- Hayes AF (2015). An index and test of linear moderated mediation. Multivariate Behavioral Research, 50(1), 1–22. [DOI] [PubMed] [Google Scholar]
- Hooper LM, Decoster J, White N, & Voltz ML (2011). Characterizing the magnitude of the relation between self-reported childhood parentification and adult psychopathology: A meta-analysis. Journal of Clinical Psychology, 67(10), 1028–1043. [DOI] [PubMed] [Google Scholar]
- Hooper LM, Tomek S, Bond JM, & Reif MS (2015). Race/ethnicity, gender, parentification, and psychological functioning: Comparisons among a nationwide university sample. The Family Journal, 23(1), 33–48. [Google Scholar]
- Jankowski PJ, Hooper LM, Sandage SJ, & Hannah NJ (2013). Parentification and mental health symptoms: Mediator effects of perceived unfairness and differentiation of self. Journal of Family Therapy, 35(1), 43–65. [Google Scholar]
- Jurkovic GJ (1997). Lost childhoods: The plights of the parentified child. Philadelphia: Brunner/Mazel. [Google Scholar]
- Lim J, Wood BL, & Miller BD (2008). Maternal depression and parenting in relation to child internalizing symptoms and asthma disease activity. Journal of Family Psychology, 22(2), 264. [DOI] [PubMed] [Google Scholar]
- Melby JN, & Conger RD (2001). The Iowa Family Interaction Rating Scales: Instrument Summary. (Kerig PK & Lindahl KM, Eds.). Erlbaun: Mahwah, NJ: Family observational coding systems. [Google Scholar]
- Minuchin S, Montalvo B, Guerney BG, Rosman B, & Schumer F (1967). Families of the slums: An exploration of their structure and treatment. New York: Basic Books. [Google Scholar]
- Monti JD, Winning A, Watson KH, Williams EK, Gerhardt CA, Compas BE, & Vannatta K (2017). Maternal and paternal influences on children’s coping with cancer-related stress. Journal of Child and Family Studies, 26, 2016–2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy LK, Murray CB, & Compas BE (2017). Topical Review: Integrating Findings on Direct Observation of Family Communication in Studies Comparing Pediatric Chronic Illness and Typically Developing Samples. Journal of Pediatric Psychology, 42(1), 95–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy LK, Rodriguez EM, Schwartz L, Bemis H, Desjardins L, Gerhardt CA, … C. BE (2016). Longitudinal association among maternal communication and adolescent posttraumatic stress symptoms after cancer diagnosis. Psycho-Oncology, 25(7), 779–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. (2013). A snapshot of pediatric cancers. Retrieved from http://www.cancer.gov/researchandfunding/snapshots/pdf/Pediatric-Snapshot.pdf
- Pai AL, Greenley RN, Lewandowski A, Drotar D, Youngstrom E, & Peterson CC (2007). A meta-analytic review of the influence of pediatric cancer on parent and family functioning. JFam Psychol, 21(3), 407–415. https://doi.org/10.1037/0893-3200.2L3.407 [DOI] [PubMed] [Google Scholar]
- Pinquart M, & Shen Y (2011). Behavior problems in children and adolescents with chronic physical illness: A meta-analysis. Journal of Pediatric Psychology, 36(4), 375–384. [DOI] [PubMed] [Google Scholar]
- Rodriguez EM, Dunn MJ, Zuckerman T, Hughart L, Vannatta K, Gerhardt CA, … Compas BE (2013). Mother-child communication and maternal depressive symptoms in families of children with cancer: Integrating macro and micro levels of analysis. Journal of Pediatric Psychology, 38(7), 732–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez EM, Dunn MJ, Zuckerman T, Vannatta K, Gerhardt CA, & Compas BE (2012). Cancer-Related Sources of Stress for Children With Cancer and Their Parents. Journal of Pediatric Psychology, 37(2), 185–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez EM, Murphy L, Vannatta K, Gerhardt CA, Young-Saleme T, Saylor M, … Compas BE (2016). Maternal coping and depressive symptoms as predictors of mother-child communication about a child’s cancer. Journal of Pediatric Psychology, 41(3), 329–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothbaum F, & Weisz JR (1994). Parental caregiving and child externalizing behavior in nonclinical samples: A meta-analysis. Psychological Bulletin, 116(1), 55–74. [DOI] [PubMed] [Google Scholar]
- Stein JA, Riedel M, & Rotheram-Borus MJ (1999). Parentification and its impact on adolescent children of parents with AIDS. Family Process, 38(2), 193–208. [DOI] [PubMed] [Google Scholar]
- Tronick EZ, & Gianino A (1986). The transmission of maternal disturbance to the infant In Tronick EZ & Field T (Eds.), Maternal depression and infant disturbance (pp. 61–82). San Francisco, CA: Jossey-Bass. [Google Scholar]
- Wethington E, McLeod JD, & Kessler RC (1987). The importance of life events for explaining sex differences in psychological distress. In & Barnett GKBRC, Biener L (Ed.), Gender and Stress (pp. 144–156). New York: Free Press. [Google Scholar]