Abstract
Background/Objectives:
Among married couples, the death of one’s spouse can influence perceptions of health services available at the end-of-life (EOL). However, it is unknown if one spouse’s EOL experience is associated with the widowed spouse’s uptake of health services or advance care planning (ACP). We determine if EOL experiences in the first spouse are associated with EOL experiences in the second spouse.
Design:
Nationally-representative, longitudinal survey.
Setting:
Health and Retirement Study, Waves 1992–2012 linked to Medicare claims
Participants:
4,558 community-dwelling older adults who died, representing 2,279 male-female married couples.
Measurements:
We examined three EOL experiences: 1) enrollment in hospice for >3 days before death; 2) lack of ACP prior to death; and 3) Intensive care unit (ICU) use during the last 30 days of life. We used multiple logistic regression to determine if the EOL experience of the first spouse was a significant predictor of the EOL experience in the second spouse after adjusting for demographics, socioeconomic status, health status, and time between the first and second spouses’ death.
Results:
First spouses who died were on average 80 years old and 62% male, and second spouses were on average 85 years old and 62% female. After adjustment, second spouses were more likely to use hospice if the first spouse used hospice services (OR=1.68, 95% CI: 1.29–2.20). Second spouses were less likely to have ACP when the first spouse did not have ACP prior to death (OR=2.91, 95% CI: 2.02–4.21). Hospice and ACP associations were stronger when deaths were closer in time to one another (p-value for interaction <0.05). Second spouses were more likely to use ICU services if the first spouse was in the ICU prior to death (OR=1.80, 95% CI: 1.27–2.55).
Conclusions:
The EOL experiences of older spouses are strongly associated, which may be relevant when framing ACP discussions.
Keywords: Marriage, Intensive Care Unit, Hospice, Advance Care Planning, Older adults
INTRODUCTION
Among married couples, spouses often play a critical role in caregiving and decision making at the end of their partner’s life.1–3 This experience and the eventual loss of one’s partner can influence their perceptions of health care services available at the end of life. Medically intense deaths, such as those involving hospitalizations or intensive care unit (ICU) stays, for example, can be associated with post-traumatic stress or depression in family members and poorer perceived management of distressing symptoms like pain and dyspnea.4–8 Witnessing family members on hospice, on the other hand, is often associated with positive perceptions of quality of life and symptom management.6, 9, 10 One might expect, therefore, that the end-of-life experience of one’s marital partner is associated with how the surviving spouse perceives and eventually approaches their own end-of-life decisions and advance care planning.
A substantial literature documents the concordance among spouses across a wide spectrum of health behaviors and health risk factors.9, 11–15 To date, however, there are no studies directly examining whether there is concordance in end-of-life experiences among married couples, including advance care planning, hospice use, or ICU use prior to death. There are several hypotheses on mechanisms for spousal concordance, which may be relevant to end-of-life experiences. The shared resources hypothesis, for example, suggests that shared environments and resources among married couples can lead to similar health outcomes.16 Alternatively, interdependence theory suggests that couples work to achieve health goals that are in the interest of the relationship, and recognizes the influence one spouse can have on the other’s health preferences.17 The importance of the marital relationship may factor into how couples complete advance care directives or whether individuals prioritize end-of-life interventions that place less caregiving burden on partners or family members. In addition, one theory suggests that a person’s end-of-life treatment intensity can impact the downstream health care utilization of caregivers due to the perceived impact on symptoms, financial burdens of costs, and shared social networks.18A better understanding of whether spousal concordance exists in end-of-life experiences could inform how providers engage married couples and widowed spouses in advance care planning.
In this study, we used the US nationally-representative Health and Retirement Study (HRS) to examine end-of-life experiences among older married couples, including hospice use, an ICU stay in the last 30 days of life, and lack of advance care planning prior to death. Our goal was to determine if these end-of-life experiences in the first spouse were associated with the end-of-life experiences in the second spouse. We utilize the theoretical framework developed by Ornstein et al. (2015) on downstream effects of end-of-life treatment intensity on caregivers to posit three a priori hypotheses related to each measured end-of-life experience: 1) that the second spouse is more likely to utilize hospice services if the first spouse received hospice care; 2) that the second spouse is less likely to utilize ICU services if the first spouse was in the ICU at the end of life; and 3) that the second spouse less likely to have documented advance care planning if the first spouse had no advance care planning before death.17,18
METHODS
Sample
The Health and Retirement Study (HRS) is a nationally-representative sample of US community-dwelling adults 50 years or older. Using a household sampling strategy, HRS includes co-resident partners and spouses providing a national sample of married couples. Respondents were interviewed starting in 1992 and every subsequent two years, with additional participants added every six years. After participant deaths, next-of-kin provided information about the end-of-life period in an exit interview. The Institutional Review Board at the University of Michigan and the University of San Francisco, California approved this study. Further details on the sample design and study are available online at the HRS website (http://hrsonline.isr.umich.edu/).
We examined waves 1992–2012 of HRS and included married couples where both spouses died between August, 1992 and December, 2013. From the total HRS sample of 29,648 respondents (14,824 couples), we excluded couples if both spouses did not die within the specified timeframe (n = 24,548), had the same date of death (n = 10), or at least one spouse was not age-eligible for all waves of HRS or resided in a nursing home (n = 532). This yielded a sample of 4,558 community-dwelling older adults representing 2,279 couples. For simplicity, we use the term “first spouse” to refer to the spouse who dies first in a married couple and “second spouse” to refer to the spouse who dies second in a married couple.
End-of-life Experiences
We studied three characteristics of the spouses’ end-of-life experience: 1) hospice services for more than three days prior to death, 2) ICU level care in the last 30 days of life, and 3) lack of advance care planning prior to death. The ICU and hospice outcomes were both derived from Medicare claims data and defined based on prior literature demonstrating these time cutoffs as quality indicators for end-of-life care.19–21 For hospice we included HRS decedent spouses who agreed to a Medicare linkage, as Medicare claims capture hospice use for persons with either Fee-for-Service or Medicare Managed Care. For ICU use we included HRS decedent spouses enrolled in Medicare Fee-for-Service in the last 30 days of life. The number of couples with information from both spouses on hospice and ICU use was 1,803 and 1,353, respectively. Having no Advance Care Planning (ACP) prior to death is a known quality indicator that can predispose individuals to a number of poor end-of-life outcomes.22 Lack of Advance Care Planning (ACP) was defined as having no advance directive, durable power of attorney (DPOA) or prior discussed preferences for end-of-life care with a next-of-kin.23 ACP was determined from HRS asking proxies during the exit interview whether the decedent subject had engaged in ACP discussions prior to death. For years 1992, 1993, 1994, and 1998 questions about advance directives, DPOA, or discussed preferences for end-of-life care with a next-of-kin were not asked. The number of couples with information on ACP for both spouses was 1,402 couples.
Covariates
Based on prior literature, we included several variables that are predictors of end-of-life care and advance care planning.24–26 We included age at the time of death, gender, race/ethnicity (“White/Caucasian,” “Black/African American,” “Hispanic,” or “Other”), and education (less than high school/GED or greater than high school/GED). Socioeconomic status was measured using net worth in quartiles,27 and the presence of living children at death was determined from exit interviews with next-of-kin. The importance of religion was measured prior to death. Cognition prior to death was determined using the dementia probability score and composite memory scores previously described in the HRS sample.28 We established the date of death and months between deaths of each spouse using the National Death Index (NDI) dataset, the RAND HRS dataset, and information from exit interviews. We determined the presence of several comorbidities prior to death, including hypertension, diabetes, non-skin cancers, lung disease, prior stroke, or heart disease. Functional status was measured based on Activities of Daily Living (ADLs) (toileting, dressing, eating, getting in and out of bed, and bathing) with individuals defined as having “no ADL dependence” if they could do all activities independently, or “any ADL dependence” if they required help with any of the activities.29
Statistical Analysis
We first examined the associations of end-of-life outcomes between each spouse using Pearson Chi-square tests. We then fit separate logistic regression models to determine if the first spouse’s end-of-life outcomes predicted each outcome variable for the second spouse after adjusting for select covariates of the second spouse. In each model, we tested for two interactions: 1) between first spouse end-of-life outcomes and months between spousal deaths, and 2) between first spouse end-of-life outcomes and gender of the second spouse. We report statistically significant (p<0.05) interaction terms. Odds ratios are reported as are 95% confidence intervals. All analyses were performed with SAS 9.4 and Stata 15 statistical packages and utilized sampling weights accounting for the complex sample design to ensure national representativeness.30
RESULTS
Characteristics of each spouse in our sample appear in Table 1. The first spouses who died were 62% male with a median age of 80 years old at death. The second spouses were 62% female with a median age of 85 years old at death. First and second spouses had similar use of ICU in the last 30 days of life (26.5% and 26.0%, respectively). The first spouse had lower hospice use compared to the second spouse (22.4% vs 31.9%, p<0.001), and more frequently had no ACP prior to death (28.4% vs 16.4%.%, p<0.001).
Table 1.
Weighted sample characteristics prior to death by spouse in HRS and Medicare datasets from 1992–2012 (N=2,279 dyads)
| Characteristics | First Spouse (%) | Second Spouse (%) | |
|---|---|---|---|
| Sociodemographics | |||
| Age at death, median (IQR) | 80.1 (74.5–85.7) | 84.8 (78.5–90.2) | |
| Year of Death, median (IQR) | 2001 (1997–2005) | 2008 (2004–2010) | |
| Months between deaths, median (IQR) | - | 59 (26–104) | |
| Gender | Male | 61.5 | 38.5 |
| Female | 38.5 | 61.5 | |
| Race/Ethnicity | White/Caucasian | 87.5 | 86.9 |
| Black/AA | 7.4 | 7.4 | |
| Hispanic | 4.0 | 4.7 | |
| Other | 1.2 | 1.0 | |
| Educationa | <HS or GED | 41.4 | 38.8 |
| Net Worth($) | <6,000 | 10.6 | 15.6 |
| 6,000–<81,000 | 27.3 | 26.7 | |
| 81,000–<239,000 | 30.2 | 27.0 | |
| >=239,000 | 31.9 | 30.8 | |
| Has Living Children | 93.4 | 93.1 | |
| Importance of Religion | Very Important | 60.7 | 65.0 |
| Somewhat important | 24.8 | 23.1 | |
| Not important | 14.6 | 11.9 | |
| Health status | |||
| Comorbiditiesa | Cancer | 25.9 | 24.5 |
| Hypertension | 58.5 | 67.0 | |
| Diabetes mellitus | 22.9 | 23.8 | |
| Lung disease | 21.6 | 18.5 | |
| Stroke | 21.2 | 20.7 | |
| Heart Disease | 46.9 | 46.6 | |
| Any ADL Dependencea | 26.8 | 25.1 | |
| End of life outcomes | |||
| Hospice use > 3 daysb | 22.4 | 31.9 | |
| ICU stay in last 30 days of lifec | 26.5 | 26.0 | |
| Advance care planningd | 71.6 | 83.6 | |
Abbreviations: HRS - Health and Retirement Study, SD - Standard Deviation, IQR - interquartile range, HS - High school, ADL - activities of daily living, ICU - intensive care unit
Reports percentage responding yes or having the condition, column may not add up to 100%
Available for n=2,040 first spouses and n=1,954 second spouses
Available for n=1,677 first spouses and n=1,533 second spouses
Advance care planning includes having an advance directive, durable power of attorney (DPOA) or having discussed preferences for end-of-life care with a next-of-kin. Data was not available for 1992, 1993, 1994, and 1998 waves. Available for n=1,703 first spouses and n=1791 second spouses.
Table 2 presents weighted percentages and unadjusted odds ratios between end-of-life variables from each spouse. In addition, Table 2 presents adjusted odds ratios from separate logistic regression models which use end-of-life variables in the first spouse as a predictor of outcomes in the second spouse (Figure 1). After adjustment, second spouses were more likely to use hospice if the first spouse used hospice services (aOR=1.68, 95% CI: 1.29–2.20). When first spouses had no ACP prior to death, second spouses had nearly three times the odds of having no ACP prior to death (aOR=2.91, 95% CI: 2.02–4.21). Second spouses were more likely to use ICU services in the last 30 days of life if the first spouse was in the ICU prior to death (aOR=1.80, 95% CI: 1.27–2.55), but less likely to use the ICU if the first spouse received hospice services (aOR=0.65, 95% CI: 0.47–0.91). In addition, individuals whose spouses used the ICU were less likely to receive hospice services (aOR=0.72, 95% CI: 0.53–0.99), and more likely to have advance care planning (aOR=1.52, 95% CI: 1.04–2.23).
Table 2.
Association of End-of-Life Outcomes Among Married Couples, HRS and Medicare datasets from 1992–2012
| Predictors: End of Life Experiences in 1st Spouse | Outcomes: End of Life Experiences in 2nd Spouse | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospice use >3 days | ICU stay in last 30 days | Advance care planning | ||||||||||
| n | No | Yes | p-value | n | No | Yes | p-value | n | No | Yes | p-value | |
| Hospice use >3 days | ||||||||||||
| No(%) | 1,803 | 70.05 | 29.95 | <0.001 | 1,442 | 72.6 | 27.4 | 0.01 | 1,624 | 16.3 | 83.7 | 0.15 |
| Yes(%) | 58.22 | 41.78 | 80.0 | 20.0 | 12.9 | 87.1 | ||||||
| OR(95%CI) | 1.67 | (1.27–2.20) | 0.67 | (0.49–0.91) | 1.31 | (0.90–1.92) | ||||||
| aOR(95%CI) | 1.68 | (1.29–2.20) | <0.001 | 0.65 | (0.47–0.91) | 0.01 | 1.04 | (0.72–1.52) | 0.82 | |||
| ICU stay in last 30 days of life | ||||||||||||
| No(%) | 1,497 | 66.7 | 33.3 | 0.05 | 1,353 | 77.8 | 22.2 | <0.001 | 1,347 | 16.4 | 83.6 | 0.19 |
| Yes(%) | 72.5 | 27.5 | 64.3 | 35.7 | 13.6 | 86.4 | ||||||
| OR(95%CI) | 0.76 | (0.57–0.99) | 1.94 | (1.38–2.74) | 1.25 | (0.88–1.77) | ||||||
| aOR(95%CI) | 0.72 | (0.53–0.99) | 0.04 | 1.80 | (1.27–2.55) | 0.001 | 1.52 | (1.04–2.23) | 0.03 | |||
| Advance care planning | ||||||||||||
| No(%) | 1,474 | 72.7 | 27.3 | 0.02 | 1,151 | 71.9 | 28.1 | 0.98 | 1,402 | 29.4 | 70.6 | <0.001 |
| Yes(%) | 65.6 | 34.4 | 72.0 | 28.0 | 10.0 | 90.0 | ||||||
| OR(95%CI) | 1.40 | (1.05–1.84) | 0.99 | (0.72–1.37) | 3.72 | (2.73–5.06) | ||||||
| aOR(95%CI) | 1.24 | (0.90–1.72) | 0.18 | 1.03 | (0.72–1.49) | 0.86 | 2.91 | (2.02–4.21) | <0.001 | |||
Abbreviations: HRS - Health and Retirement Study, ICU - Intensive Care Unit, OR - Odds Ratio, aOR - adjusted Odds Ratio
“1st spouse” refers to the spouse who dies first in a married couple,”2nd spouse” refers to the spouse that dies second in a married couple
Percentages included in the table are row percentages
Chi-square tests are used to determine the significance of unadjusted odds ratios
Adjusted odds ratios adjust for: Age at death, Months between 1st spouse’s death and 2nd spouse’s death, Year of death, Gender, Race/Ethnicity, Comorbidities (Cancer,Hypertension,Diabetes mellitus, Lung disease, Stroke, Heart Disease),Any ADL dependence, Education less than high school or have GED, Net worth, Importance of Religion, and Presence of Children
Figure1.
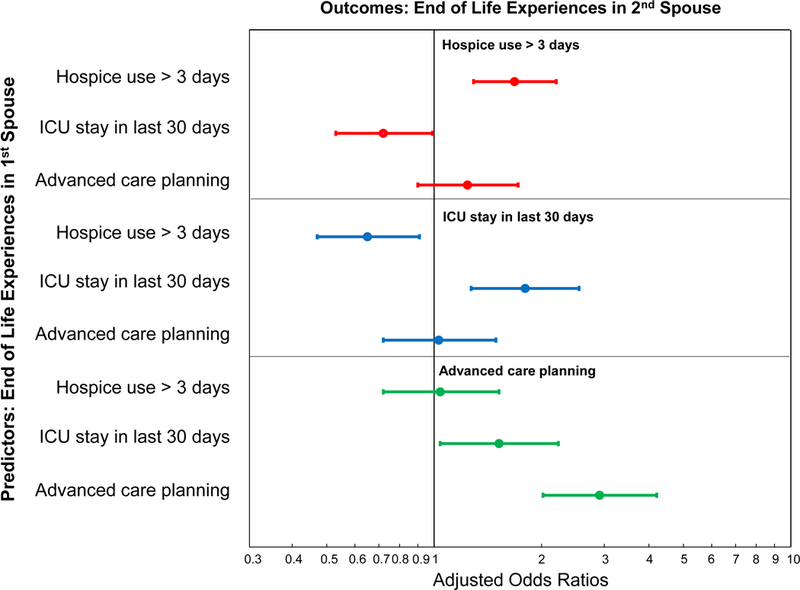
Association of End-of-Life Outcomes Among Married Couples. Figure presents the adjusted odds ratios derived from separate logistic regression models. Models adjust for: Months between 1st spouse’s death and 2nd spouse’s death and the following covariates for the 2nd spouse: Age at death, Year of death, Gender, Race/Ethnicity, Comorbidities (Cancer, Hypertension, Diabetes mellitus, Lung disease, Stroke, Heart Disease), Any ADL dependence, Education less than high school or have GED, Net worth, Importance of Religion, and Presence of Children. “1st spouse” refers to the spouse who dies first in a married couple, “2nd spouse” refers to the spouse that dies second in a married couple. Bars represent 95% Confidence Intervals.
We next determined whether associations between the first and second spouse’s end-of-life outcomes varied with the time between deaths. When deaths were closer in time to one another, spouses were more likely to have similar hospice utilization behavior (p-value for interaction=0.034, Figure 2) and a similar lack of ACP (p-value for interaction=0.036, Figure 3). As deaths became further separated in time, the first spouse’s hospice or ACP use had less of an association with the second spouse’s hospice or ACP use (Figure 2 and Figure 3). Time between death did not modify the association of ICU use among spouses. We determined whether associations between the first and second spouse’s end-of-life outcomes differed based on the gender of the first spouse who died. This analysis revealed no signification interaction effects by gender (Supplementary Tables 1 and 2).
Figure2.
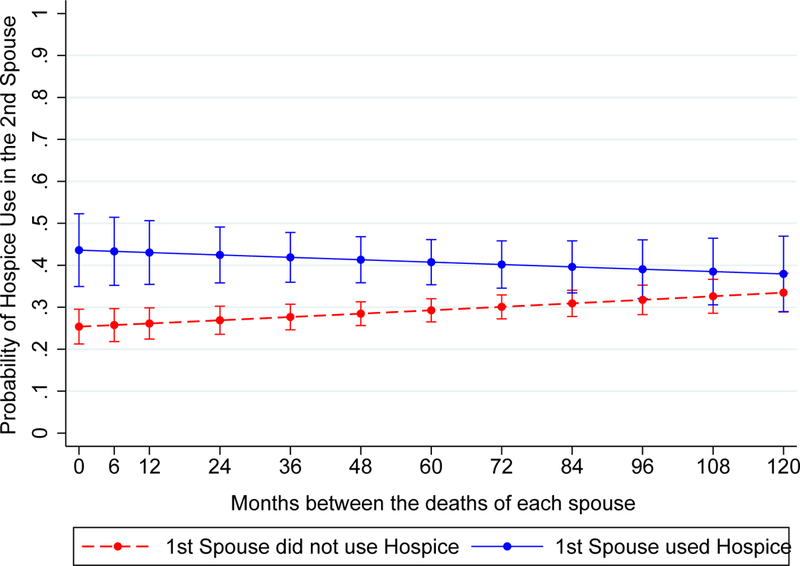
Adjusted marginal probability of hospice use for second spouses by first hospice use status. Figure presents the marginal probabilities derived from a logistic regression model. Model adjusts for: Months between 1st spouse’s death and 2nd spouse’s death and the following covariates for the 2nd spouse: Age at death, Year of death, Gender, Race/Ethnicity, Comorbidities (Cancer, Hypertension, Diabetes mellitus, Lung disease, Stroke, Heart Disease), Any ADL dependence, Education less than high school or have GED, Net worth, Importance of Religion, and Presence of Children. “1st spouse” refers to the spouse who dies first in a married couple, “2nd spouse” refers to the spouse that dies second in a married couple. Bars represent 95% Confidence Intervals.
Figure3.
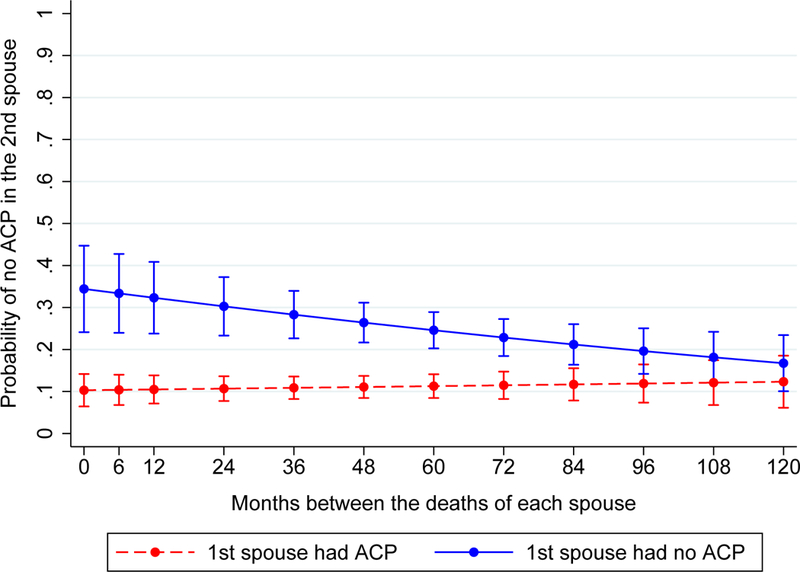
Adjusted marginal probability of no advance care planning (ACP) for second spouses by first spouse ACP status. Figure presents the marginal probabilities derived from a logistic regression model. Model adjusts for: Months between 1st spouse’s death and 2nd spouse’s death and the following covariates for the 2nd spouse: Age at death, Year of death, Gender, Race/Ethnicity, Comorbidities (Cancer, Hypertension, Diabetes mellitus, Lung disease, Stroke, Heart Disease), Any ADL dependence, Education less than high school or have GED, Net worth, Importance of Religion, and Presence of Children. “1st spouse” refers to the spouse who dies first in a married couple, “2nd spouse” refers to the spouse that dies second in a married couple. Bars represent 95% Confidence Intervals.
DISCUSSION
In a nationally-representative sample of older married couples, we are the first to examine the similarities in their end-of-life experiences. We found a similar pattern in hospice use and lack of ACP between spouses, and that these associations were stronger the closer in time the deaths occurred. In addition, spouses had similar tendencies to use the ICU prior to death such that if the first spouse used the ICU the second spouse had nearly twice the odds of ICU use. We discuss how clinicians might incorporate this information into advance care planning below.
As hypothesized, when the first spouse engaged in hospice or had no ACP, the second spouse to die was more likely to engage in hospice or have no ACP. Results contribute to growing literature showing that married couples act similarly on a range of health behaviors,11–14 and studies showing that spouses are more likely to have ACP if their partner has engaged in ACP,9, 31 or if their partner has died.32–36 We expand on our understanding of spousal concordance related to ACP and hospice use through two additional findings. First, spouses who died first had approximately 10 percentage point lower rates of hospice use and ACP engagement compared to second spouses. Additionally, when deaths were closer in time to one another second spouses were more likely to have similar hospice use and lack of ACP to the first spouses. Based on our conceptual framework, we speculate that hospice use and ACP are in part co-dependent or learned behaviors.17, 18 Individuals who did not witness a spouse engage in these activities may have had lower initial familiarity which may have had a larger impact on spouses who died shortly after their partners. Additionally, shared characteristics, values and exposures within a married couple may play a role in the explanation for these associations. For example, in order to access home hospice services both spouses may have had similar caregiver or family resources to allow them to remain at home. Similar resources would be particularly important for widowed spouses.
Our study is the first to show concordant tendencies among married couples to use the ICU at the end-of life; second spouses had nearly twice the odds of using the ICU if first spouses utilized ICU services at the end-of-life. These results were unexpected given prior literature demonstrating individuals’ stated intentions to avoid aggressive care witnessed in spouses,9 poorer perceived end-of-life symptom management in the ICU,6, 37 and the impact of ICU care on psychological health of caregivers..4, 5, 7 One potential explanation is shared traits or exposures to the health system among married couples which increase the likelihood of ICU use. These may include a lack of ACP,38 health seeking behaviors, and geographic exposures to high intensity health care systems.39, 40 In addition, children and caregivers may make similar decisions for each spouse at the end-of-life in critical illness through a surrogate role. In summary, despite qualitative studies showing spouses’ stated intentions to avoid similar ICU experiences,41 surviving spouses actual uptake of ICU services remains similar.
Notably, we found no significant difference in spousal concordance for end-of-life experiences depending on the gender of the first spouse to die, despite prior literature often showing a different impact of marriage on health based on gender.42 This was relevant to our sample since second spouses were on average older and more often female. We hypothesize that end-of-life experiences are less subject to gender relationships due to complex interactions with the health system and other caregivers who may be involved with decisions. Alternatively, the study was underpowered to detect differences by gender.
Taken together, results suggest that investigating an individual’s experience with spousal death can meaningfully inform advance care planning. Inquiry could be as simple as asking individuals, “can you tell me about your prior experience with serious illness in a loved one or your spouse?” Clinicians might gain from this knowledge in two ways. First, if the second spouse wishes to have a different end-of-life experience than the first spouse, this might warrant explicit discussion and advance care planning. Second, the end-of-life experience of one’s spouse may lead to more familiarity with hospice and advance care planning. Interventions aimed at improving advance care planning and appropriate hospice use may be particularly effective in the years shortly after the death of one’s spouse. In addition, results suggest that interventions to improve end-of-life experiences might target households and leverage dyadic decision making by discussing advance care planning as a couple rather than as individuals. Recognizing end-of-life decisions as relevant to marital or family relationships (i.e. “our” medical issue) rather than only about the individual (i.e. “my” medical issue) could make counseling more effective and have cascading effects to spouses.17,18
We acknowledge several limitations. First, as with most studies of married couples, we were unable to measure many shared traits, preferences, and exposures, which may introduce bias into our adjusted estimates. In addition to controlling for common confounders, we examined whether shared traits at the couple-level (for example, both spouses being religious, both having college-level educations, or both having certain comorbidities) predicted end-of-life experiences and found no significant effects in regression models. Second, we do not study the role of other family members in end-of-life experiences who may take on more responsibilities of surrogate decision making in widowed spouses. Including a covariate for presence of children in our regression models did not alter study results, however, there may be residual confounding. Future studies might examine the role of the broader social network. Third, we did not remove couples that may have divorced during the study period. However, we would expect divorced couples to have less concordance in end-of-life experiences, so findings may represent more conservative estimates. A sensitivity analysis removing couples where one spouse had more than one partner in their lifetime (n = 158) revealed similar results. Fourth, results are only generalizable to heterosexual couples included in HRS as same-sex couples were not specifically sampled.
In conclusion, this study shows that spouses have similar end-of-life experiences with respect to hospice use, ICU use, and lack of advance care planning. Associations for hospice use and advance care planning were stronger the closer the deaths occurred. Results may be relevant to how clinicians frame advance care planning discussions, potential interventions, and the timing of these discussions.
Supplementary Material
Supplementary Table 1. Association of End-of-Life Outcomes Among Married Couples when the Male Dies First, HRS and Medicare datasets from 1992–2012.
Supplementary Table 2. Association of End-of-Life Outcomes Among Married Couples when the Female Dies First, HRS and Medicare datasets from 1992–2012
IMPACT statement:
We certify that this research is novel. In a nationally-representative survey we are the first to show that married couples have similar end-of-life experiences related to the use of hospice services, the intensive care unit, and advance care planning, and that certain associations are more similar the closer in time the deaths occur. Results are relevant to how we understand and approach advance care planning in older adults.
ACKNOWLEDGEMENTS
The National Institute on Aging provided support for Dr. Alex Smith (R01AG047897) and Dr. Katherine Ornstein (K01AG047923).
Funding:
The National Institute on Aging provided support for Dr. Alex Smith (R01AG047897) and Dr. Katherine Ornstein (K01AG047923).
Footnotes
Conflicts of Interest:
All authors report no conflicts of interest.
Sponsor’s Role:
The sponsor had no role in the design, methods, data collection, analysis, or preparation of the paper.
REFERENCES
- 1.Rabow MW, Hauser JM, Adams J. Supporting family caregivers at the end of life: They don’t know what they don’t know. Jama. 2004;291(4):483–491. [DOI] [PubMed] [Google Scholar]
- 2.Fried T, Zenoni M, Iannone L. A dyadic perspective on engagement in advance care planning. Journal of the American Geriatrics Society. 2017;65(1):172–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jo S, Brazil K, Lohfeld L, Willison K. Caregiving at the end of life: perspectives from spousal caregivers and care recipients. Palliative & Supportive Care. 2007;5(1):11–17. [DOI] [PubMed] [Google Scholar]
- 4.Azoulay E, Pochard F, Kentish-Barnes N, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. American journal of respiratory and critical care medicine. 2005;171(9):987–994. [DOI] [PubMed] [Google Scholar]
- 5.Jones C, Skirrow P, Griffiths RD, et al. Post-traumatic stress disorder-related symptoms in relatives of patients following intensive care. Intensive care medicine. 2004;30(3):456–460. [DOI] [PubMed] [Google Scholar]
- 6.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. Jama. 2004;291(1):88–93. [DOI] [PubMed] [Google Scholar]
- 7.Ornstein KA, Aldridge MD, Garrido MM, et al. The Use of Life-Sustaining Procedures in the Last Month of Life Is Associated With More Depressive Symptoms in Surviving Spouses. Journal of pain and symptom management. 2017;53(2):178–187. e171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petrinec AB, Martin BR. Post-intensive care syndrome symptoms and health-related quality of life in family decision-makers of critically ill patients. Palliative & Supportive Care. 2017:1–6. [DOI] [PubMed] [Google Scholar]
- 9.Carr D “I don’t want to die like that…”: The impact of significant others’ death quality on advance care planning. The Gerontologist. 2012;52(6):770–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ornstein KA, Aldridge MD, Garrido MM, Gorges R, Meier DE, Kelley AS. Association between hospice use and depressive symptoms in surviving spouses. JAMA internal medicine. 2015;175(7):1138–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Franks MM, Shields CG, Lim E, Sands LP, Mobley S, Boushey CJ. I Will If You Will Similarity in Married Partners’ Readiness to Change Health Risk Behaviors. Health Education & Behavior. 2012;39(3):324–331. [DOI] [PubMed] [Google Scholar]
- 12.Falba TA, Sindelar JL. Spousal concordance in health behavior change. Health services research. 2008;43(1p1):96–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pai C-W, Godboldo-Brooks A, Edington DW. Spousal concordance for overall health risk status and preventive service compliance. Annals of epidemiology. 2010;20(7):539–546. [DOI] [PubMed] [Google Scholar]
- 14.Kotwal AA, Lauderdale DS, Waite LJ, Dale W. Differences between husbands and wives in colonoscopy use: results from a national sample of married couples. Preventive medicine. 2016;88:46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meyler D, Stimpson JP, Peek MK. Health concordance within couples: a systematic review. Social science & medicine. 2007;64(11):2297–2310. [DOI] [PubMed] [Google Scholar]
- 16.Smith KR, Zick CD. Linked lives, dependent demise? Survival analysis of husbands and wives. Demography. 1994;31(1):81–93. [PubMed] [Google Scholar]
- 17.Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, Emmons KM. Understanding health behavior change among couples: An interdependence and communal coping approach. Social science & medicine. 2006;62(6):1369–1380. [DOI] [PubMed] [Google Scholar]
- 18.Ornstein KA, Boerner K, Siu AL, Schulz R. Downstream effects of end-of-life care for older adults with serious illness on health care utilization of family caregivers. Journal of palliative medicine. 2015;18(9):736–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Earle CC, Park ER, Lai B, Weeks JC, Ayanian JZ, Block S. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. Journal of Clinical Oncology. 2003;21(6):1133–1138. [DOI] [PubMed] [Google Scholar]
- 20.Grunfeld E, Urquhart R, Mykhalovskiy E, et al. Toward population‐based indicators of quality end‐of‐life care. Cancer. 2008;112(10):2301–2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the aggressiveness of cancer care near the end of life. Journal of Clinical Oncology. 2004;22(2):315–321. [DOI] [PubMed] [Google Scholar]
- 22.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end‐of‐life care: A national study. Journal of the American Geriatrics Society. 2007;55(2):189–194. [DOI] [PubMed] [Google Scholar]
- 23.Bischoff KE, Sudore R, Miao Y, Boscardin WJ, Smith AK. Advance care planning and the quality of end‐of‐life care in older adults. Journal of the American Geriatrics Society. 2013;61(2):209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bravo G, Dubois M-F, Paquet M. Advance directives for health care and research: Prevalence and correlates. Alzheimer Disease & Associated Disorders. 2003;17(4):215–222. [DOI] [PubMed] [Google Scholar]
- 25.Alano GJ, Pekmezaris R, Tai JY, et al. Factors influencing older adults to complete advance directives. Palliative & Supportive Care. 2010;8(3):267–275. [DOI] [PubMed] [Google Scholar]
- 26.Locher JL, Kilgore ML, Morrisey MA, Ritchie CS. Patterns and predictors of home health and hospice use by older adults with cancer. Journal of the American Geriatrics Society. 2006;54(8):1206–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith JP. Wealth inequality among older Americans. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 1997;52(Special Issue):74–81. [DOI] [PubMed] [Google Scholar]
- 28.Wu Q, Tchetgen EJT, Osypuk TL, White K, Mujahid M, Glymour MM. Combining direct and proxy assessments to reduce attrition bias in a longitudinal study. Alzheimer disease and associated disorders. 2013;27(3):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Katz S Assessing self‐maintenance: activities of daily living, mobility, and instrumental activities of daily living. Journal of the American Geriatrics Society. 1983;31(12):721–727. [DOI] [PubMed] [Google Scholar]
- 30.Stata Statistical Software: Release 15 [computer program]. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 31.Koss CS. Beyond the Individual: The Interdependence of Advance Directive Completion by Older Married Adults. Journal of the American Geriatrics Society. 2017. [DOI] [PubMed] [Google Scholar]
- 32.Amjad H, Towle V, Fried T. Association of Experience with Illness and End‐of‐life Care with Advance Care Planning in Older Adults. Journal of the American Geriatrics Society. 2014;62(7):1304–1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carr D, Khodyakov D. End-of-life health care planning among young-old adults: An assessment of psychosocial influences. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2007;62(2):S135–S141. [DOI] [PubMed] [Google Scholar]
- 34.Morrison RS, Meier DE. High rates of advance care planning in New York City’s elderly population. Archives of Internal Medicine. 2004;164(22):2421–2426. [DOI] [PubMed] [Google Scholar]
- 35.Ruff H, Jacobs RJ, Fernandez MI, Bowen GS, Gerber H. Factors associated with favorable attitudes toward end-of-life planning. American Journal of Hospice and Palliative Medicine®. 2011;28(3):176–182. [DOI] [PubMed] [Google Scholar]
- 36.Fried TR, Bullock K, Iannone L, O’leary JR. Understanding advance care planning as a process of health behavior change. Journal of the American Geriatrics Society. 2009;57(9):1547–1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Teno JM, Mor V, Ward N, et al. Bereaved Family Member Perceptions of Quality of End‐of‐Life Care in US Regions with High and Low Usage of Intensive Care Unit Care. Journal of the American Geriatrics Society. 2005;53(11):1905–1911. [DOI] [PubMed] [Google Scholar]
- 38.Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. Jama. 2008;300(14):1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Welch WP, Miller ME, Welch HG, Fisher ES, Wennberg JE. Geographic variation in expenditures for physicians’ services in the United States. New England journal of medicine. 1993;328(9):621–627. [DOI] [PubMed] [Google Scholar]
- 40.Tschirhart EC, Du Q, Kelley AS. Factors influencing the use of intensive procedures at the end of life. Journal of the American Geriatrics Society. 2014;62(11):2088–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences?: A Study of the US Medicare Population. Medical care. 2007;45(5):386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gender Umberson D., marital status and the social control of health behavior. Social science & medicine. 1992;34(8):907–917. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1. Association of End-of-Life Outcomes Among Married Couples when the Male Dies First, HRS and Medicare datasets from 1992–2012.
Supplementary Table 2. Association of End-of-Life Outcomes Among Married Couples when the Female Dies First, HRS and Medicare datasets from 1992–2012


