Abstract
OBJECTIVES:
To prospectively investigate associations of sarcopenia, obesity, and sarcopenic obesity with the incidence of falls in a racially and ethnically diverse cohort of healthy postmenopausal women from the Women’s Health Initiative (WHI).
DESIGN:
Prospective cohort study.
SETTING:
Three WHI clinical centers (Tucson-Phoenix, AZ; Pittsburgh, PA; Birmingham, AL).
PARTICIPANTS:
Postmenopausal women aged 50–79 years enrolled in the WHI who received bone and body composition scans by Dual-Energy X-ray Absorptiometry (DXA) at baseline (n=11,020).
MEASUREMENTS:
Sarcopenia was defined as the lowest 20th percentile of appendicular lean mass, correcting for height and body fat. Obesity was defined as a body fat percentage above 42%. Sarcopenic obesity was defined as the co-occurrence of sarcopenia and obesity. Fall outcome was defined as participants who reported falling 2 or more times in any year during 7 years of follow-up. The relative risk (RR) and 95% confidence interval (95% CI) for falls associated with sarcopenic obesity status were analyzed with log binomial regression models stratified by age and race/ethnicity.
RESULTS:
Sarcopenic obesity was associated with an increased risk of falls among women aged 50 – 64 years (RR=1.35, 95% CI: 1.17, 1.56), and those aged 65–79 years (RR=1.21, 95% CI: 1.05, 1.39). Sarcopenic obesity related fall risk among Hispanic/Latina women was higher than Non-Hispanic White women (RR=2.40, 95% CI: 1.56, 3.67 and RR=1.24, 95% CI: 1.11, 1.39, respectively).
CONCLUSION:
In a multiethnic cohort of postmenopausal women, sarcopenic obesity related fall risk was elevated among women aged less than 65 years and women 65 years and over. Sarcopenic obesity posed the highest risk for falls in Hispanic/Latina women. The findings support identification of causal factors and health disparities in sarcopenic obesity to better tailor fall prevention strategies and ameliorate this significant public health burden.
Keywords: Falls, Obesity, Race, Sarcopenia, Women’s Health Initiative
INTRODUCTION
The US population is aging rapidly; 1 in 5 Americans is projected to be age 65 and older by 2030.1 Falls and associated health complications rise steadily in older adults.2 It is estimated that about two-thirds of all hospital costs ($34 billion) are directly or indirectly associated with unintended falls among older adults who undergo hospitalization after a fall.3 Fall-related injuries mainly consist of fractures.2 Costs associated with fractures are projected to increase disproportionately in non-White groups with an increase in costs of 175% in Latinos compared to 37% increase in Whites by 2025.4 A better understanding of health disparities in fall risk is imperative to lessen the increasing fracture burden in non-White groups, and in a rapidly aging population.
The accumulating burden of obesity and sarcopenia in the aging population is an important factor driving healthcare needs related to falls and fractures.5 Sarcopenia is characterized as progressive, age-associated declines in skeletal muscle mass, diminished muscle strength and function. Current estimates posit that 5% to 13% of adults over 60 years of age are considered sarcopenic, with prevalence rates expected to be as high as 50% in adults aged 80 years and older.6 Concomitant to the age-related declines in skeletal muscle mass, gains in adiposity, and consequently obesity may further influence the relationship between sarcopenia and falls risk. Obesity is a growing epidemic with over one third of adults 65 years and older considered obese in 2010.7 The presence of sarcopenia and obesity, coined “sarcopenic obesity” has been associated with declining physical function and mobility, and increased risk of fractures.8,9,10 Studies with differing populations and inconsistent definitions of sarcopenic obesity have produced a wide range of prevalence estimates (0%−41%).11
Clinically, sarcopenia may be masked and go undiagnosed in older adults, particularly if total body weight or BMI are classified as above normal.12 The convergence of the national obesity epidemic coupled with sarcopenia in an aging population has created a circumstance wherein fall risk factors are increasing and suggests a need to recognize sarcopenic obesity as a public health priority. Identifying those at greatest risk for sarcopenic obesity related falls is critical to target intervention strategies, such as diet and exercise programs that have been shown to reduce loss of muscle mass during weight loss.13
Few studies have prospectively investigated the association between sarcopenic obesity and falls, and this association has not been examined in women.10 Additionally, most studies evaluate falls and predisposing factors, such as loss of muscle mass, in adults over 65 years of age. The Women’s Health Initiative (WHI) cohort affords an opportunity to prospectively evaluate fall risk in a multi-ethnic cohort across a broader age range than is typically available in the literature and to robustly evaluate the contributions of obesity, sarcopenia and the combination of the two in women. The primary objectives of this study were to evaluate prospective associations between 1) sarcopenia alone, obesity alone, and concurrent sarcopenic obesity with occurrence of self-reported falls among postmenopausal women; 2) whether sarcopenic obesity with fall risk differs by age; and 3) whether sarcopenic obesity with fall risk differs by race/ethnicity. We hypothesized sarcopenic obesity was associated with increased falls compared to sarcopenia alone, obesity alone or neither. Further, we hypothesized that sarcopenic obesity associated falls would differ across race/ethnic and across age groups.
METHODS
Study Participants
The WHI is a prospective study composed of three clinical trials (CT) (including low-fat diet patterns, hormone replacement therapy, and vitamin D and calcium supplementation) and an observational study (OS).14 A racially and ethnically diverse cohort of postmenopausal women was recruited from 40 clinic centers throughout the US between 1993 and 1998 using mass mailings as the primary recruitment method. The WHI enrolled 161,808 multiethnic postmenopausal women aged 50–79 at baseline with a predicted survival of 3 years or more.15 Additional eligibility criteria included ability and an agreement to reside in the area for at least 3 years after enrollment. All WHI participants were provided written informed consent, and the institutional review board at each clinic site approved the study. The WHI study design and recruitment have been previously described.14,15 This study includes 11,020 participants (comprised of CT: n=4,655 and OS: n=6,365) from Tucson-Phoenix, AZ; Pittsburgh, PA; and Birmingham, AL. who completed Dual-Energy X-ray Absorptiometry (DXA) scans at baseline. We excluded participants with missing sarcopenia data and those missing greater than 50% of fall data in 7 years of follow-up.
Sarcopenia and Obesity
The primary exposure variable had the following categories defined at baseline: sarcopenic only, obese only, both sarcopenic and obese, or neither sarcopenic nor obese. Obesity and sarcopenia were measured by trained technicians using whole-body DXA scans (QDR2000, 2000+, or 4500W; Hologic Inc, Bedford, MA). Obesity was classified as body fat percentage equal to or greater than 42%, as recommended for women 60–79 years old, the category most closely corresponding to the WHI population.16 Following a previous WHI study, we defined sarcopenia using the residual method because it has shown strong correlations with lower extremity function.17,18 Sarcopenia was defined as the lowest 20th percentile of appendicular lean mass accounting for height and body fat. Height was measured to the nearest 0.1 cm using a wall-mounted stadiometer.
Covariates
Covariates including age, race/ethnicity, smoking status, alcohol use, income, weekly physical activity, general health, hormone use, and number of falls in the last 12 months were collected by self-reported questionnaires at baseline.15 Missing covariate data were assessed for type of missingness and imputed using the mean. A sensitivity analysis was used to evaluate if imputed covariate data changed the results of the analysis.
Falls
Falls were assessed using a self-report medical history questionnaire collected annually in OS participants and semi-annually in CT participants with the question: “During the past 12 months, how many times did you fall and land on the floor or ground (do not include falls due to sports activities such as snow- or water-skiing or horseback riding)?”19 Possible answers included none, one time, two times, and three or more times. Falls were included from the follow-up period years 1 through 7. Fall history defined as 2 or more falls per year is a strong predictor of fall risk, and consistent with prior WHI studies.20,21,22 Therefore, we categorized falls as a binary variable: non-faller with no more than 1 fall in any year of follow-up, or faller with 2 or more falls occurring in any year of follow-up.
Statistical Approach
Baseline characteristics were compared according to fall status (i.e. faller versus non-faller). Categorical variables were compared using chi-square test, and continuous variable means were compared using Student’s T-test. We analyzed body composition (sarcopenic, obese, sarcopenic obese, and neither sarcopenic nor obese) as the independent variable in log binomial regression models to estimate relative risks (RR) and 95% confidence intervals (95% CI) for falls. Adjustment for covariates were considered for any measures or characteristics, or reported clinical or medical factor present at baseline, that may potentially confound the relationship between sarcopenia and falls as supported by the literature (age, race/ethnicity, smoking status, alcohol use, income, weekly physical activity, general self-reported health, hormone replacement therapy use, number of falls in 12 months prior to baseline, clinical trial arm, and DXA serial number) and added to the model by purposeful selection.23 Model covariates were retained if considered important in the literature, or their addition resulted in a change in the relative risk of at least 10%. Models were subsequently stratified to examine potential effect modification by age or race/ethnicity, defined as a 10% or greater difference in stratified RR values. We stratified age at 65 years old at baseline to be consistent with fall literature showing that adults 65 and over are at higher risk for falls.2 The most parsimonious model is presented. Two-sided P-values less than 0.05 were considered significant. Statistical analyses were performed using SAS, version 9.4 (SAS Institute, Inc., Cary, NC).
RESULTS
Baseline characteristics
The analytical sample consisted of 9,924 women after excluding 436 with missing sarcopenia data and 660 missing greater than 50% of fall data in 7 years of follow-up (Figure 1). Missing covariate data were imputed with the mean. Women age 65–79 years old at baseline were more likely to fall than those aged 50–64 years old at baseline (Table 1). Fallers were more likely to be Non-Hispanic White and Native American or Alaskan Native than Black or Hispanic/Latina. Fallers had greater whole body fat and lower levels of physical activity, and were more likely to report 2 or more falls in the 12 months prior to baseline.
Figure 1.
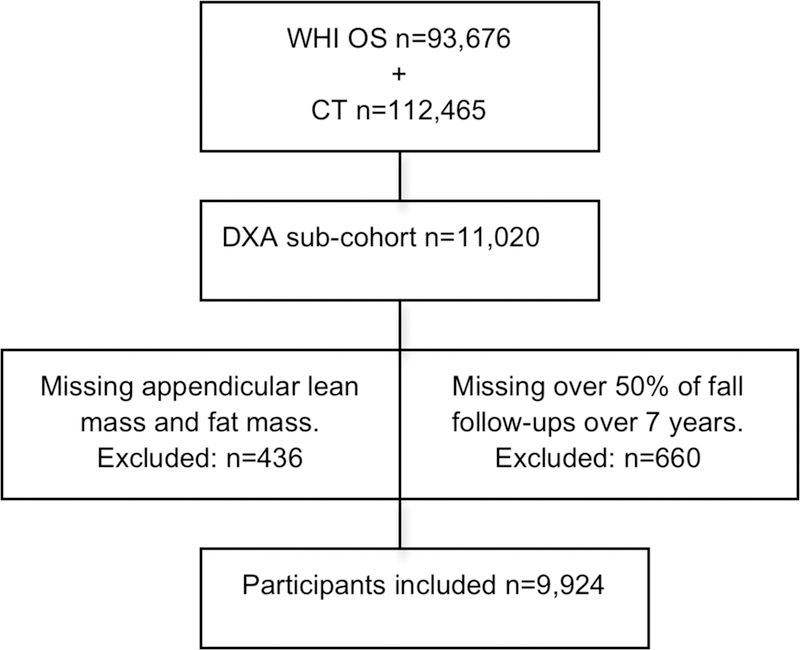
Participants included in the study
Table 1.
Characteristics of postmenopausal women by fall status (N=9,924)
| Non-Faller | Faller | |
|---|---|---|
| n, (%) | 7,415 (74.7) | 2,509 (25.3) |
| Age, n (%)* | ||
| 50 – 64 years | 4,301 (58.0) | 1,309 (52.2) |
| 65 – 79 years | 3,114 (42.0) | 1,200 (47.8) |
| Ethnicity, n (%)* | ||
| White, non-Hispanic | 5,752 (77.6) | 1,970 (78.5) |
| Black or African American | 1,067 (14.4) | 326 (13.0) |
| Hispanic/Latino | 467 (6.3) | 149 (5.9) |
| Native American or Alaska Native | 67 (0.9) | 38 (1.5) |
| Other | 53 (0.72) | 23 (0.92) |
| Missing Data | 9 (0.1) | 3 (0.1) |
| Income ($), n (%)* | ||
| < 20,000 | 1,739 (23.5) | 697 (27.8) |
| 20,000–49,999 | 3,303 (44.6) | 1,039 (41.4) |
| 50,000–99,999 | 1,513 (20.4) | 478 (19.1) |
| > 100,000 | 353 (4.8) | 113 (4.5) |
| Missing or “don’t know” | 208 (2.8) | 68 (2.7) |
| Smoking, pack years, mean (SD) | 8.9 (17.3) | 9.4 (18.0) |
| Alcohol Use, n (%) | ||
| Non drinker | 1,227 (16.6) | 405 (16.1) |
| Past drinker | 1,543 (20.8) | 596 (23.8) |
| <1 drink per month | 974 (13.1) | 322 (12.8) |
| <1 drink per week | 1,461 (19.7) | 473 (18.9) |
| 1–6 drinks per week | 1,532 (20.7) | 495 (19.7) |
| >7 drinks per week | 614 (8.2) | 194 (7.7) |
| Missing data | 64 (0.9) | 24 (1.0) |
| Hormone replacement use, n (%) | ||
| Never | 3,495 (47.1) | 1,163 (46.4) |
| Past | 1,205 (16.3) | 411 (16.4) |
| Current | 2,711 (36.6) | 934 (37.2) |
| Missing data | 4 (0.1) | 1 (0.0) |
| Recreational Physical Activity (minutes/week), mean (SD)* | 172.4 (172.1) | 161.7 (165.4) |
| Appendicular Lean Mass Index (kg/m2), mean (SD) | 5.6 (1.0) | 5.7 (1.0) |
| Whole body fat %, mean (SD)* | 43.5 (7.2) | 44.6 (7.4) |
| Body composition, n (%)* | ||
| Neither | 2,669 (36.0) | 753 (30.0) |
| Sarcopenic | 235 (3.17) | 84 (3.4) |
| Obese | 3,329 (44.9) | 1,178 (47.0) |
| Sarcopenic Obese | 1,182 (15.9) | 494 (19.7) |
| Falls in 12 months prior to baseline, n (%)* | ||
| Yes | 1,762 (23.8) | 1,205 (48.0) |
| No | 4,791 (64.6) | 1,116 (44.5) |
| Missing data | 862 (11.6) | 188 (7.5) |
P < 0.05
The prevalence of sarcopenia was similar among Non-Hispanic White, Hispanic/Latina, and Native American/Alaska Native women (4%, 3%, and 3%, respectively [Figure 2]). Black women had the lowest prevalence of sarcopenia at 0.3%, but the highest prevalence of obesity at 65%. Prevalence of sarcopenic obesity was highest in Native American or Alaska Native women (30%), lowest in Black women (7%), and with similar prevalence rates observed in Non-Hispanic White (19%) and Hispanic/Latina women (18%).
Figure 2:
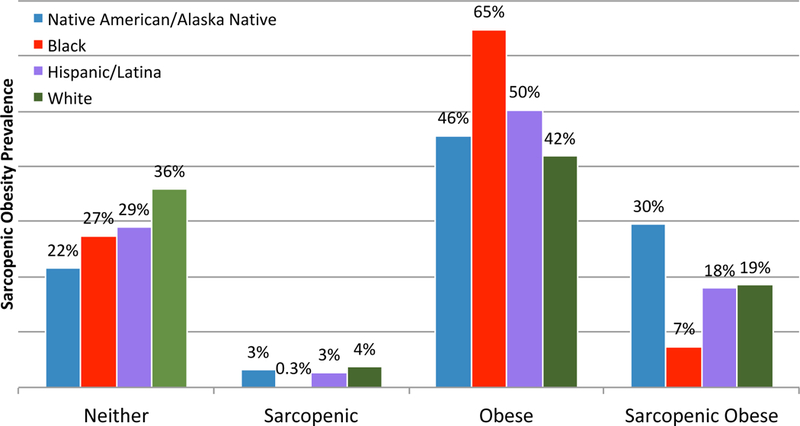
Sarcopenic obesity prevalence by race/ethnicity
Age findings
Age and race/ethnicity were effect modifiers in the association of body composition with falls; therefore, analyses were stratified by these factors. Table 2 presents the crude and adjusted RR and 95% CI for the association between falls and each body composition measure (sarcopenia, obesity, and sarcopenic obesity) compared to the reference group (neither sarcopenic nor obese), stratified by age at baseline. Among women aged 50–64 year old at baseline, all body composition categories were associated with increased risk of falling compared with women who were not sarcopenic or obese. Among women aged 65–79 years old at baseline, obesity and sarcopenic obesity, but not sarcopenia alone, were associated with increased risk of falling. Fall risk associated with sarcopenic obesity was stronger among the younger age group (RR=1.35, 95% CI: 1.17, 1.56) compared with the older age group (RR=1.21, 95% CI: 1.05, 1.39).
Table 2.
Association of body composition with falls, stratified by age
| Crude Models | Adjusted Models* | |||
|---|---|---|---|---|
| 50–64 years old n=5,610 |
65–79 years old n=4,314 |
50–64 years old n=5,393 |
65–79 years old n=4,130 |
|
| Sarcopenia, RR (95% CI) | 1.29 (0.98–1.69) | 1.10 (0.83–1.45) | 1.32 (1.01–1.74) | 1.07 (0.81–1.43) |
| Obesity | 1.22 (1.09–1.37) | 1.16 (1.03–1.30) | 1.22 (1.08–1.37) | 1.16 (1.03–1.30) |
| Sarcopenic Obesity | 1.40 (1.22–1.60) | 1.27 (1.11–1.45) | 1.35 (1.17–1.56) | 1.21 (1.05–1.39) |
Reference category is neither sarcopenic nor obese
Adjusted for race/ethnicity, smoking status, alcohol use, physical activity, and hormone use
Race/ethnicity findings
Table 3 presents the crude and adjusted RR and 95% CI for the association of body composition with falls stratified by race/ethnicity. After adjusting for age, smoking status, alcohol use, physical activity, and hormone use, sarcopenia alone was not a significant predictor of falls in any race/ethnic group (Table 3). Sarcopenia could not be evaluated for Black women because it was far less prevalent at 0.3% (Figure 2). Obesity in Black women was associated with 1.19 (95% CI: 0.95, 1.50) times the risk of falling compared to patients with neither condition. Obesity was a statistically significant predictor of falls in Non-Hispanic White women (RR=1.17, 95% CI: 1.07, 1.29) and Hispanic/Latina women (RR=1.57, 95% CI: 1.06, 2.34). Sarcopenic obesity was a significant predictor of falls in both Hispanic/Latina and Non-Hispanic White women, and the association was stronger among Hispanic/Latina women (RR=2.40, 95% CI: 1.56, 3.67) compared with Non-Hispanic White women (RR=1.24, 95% CI: 1.11, 1.39).
Table 3.
Association of body composition with falls, stratified by race/ethnicity
| Crude Models | Black n=1,389 |
Hispanic/Latina n=616 |
Non-Hispanic White n=7,722 |
Native American/ Alaskan Native n=105 |
|---|---|---|---|---|
| Sarcopenia, RR (95% CI) | - | 1.37 (0.55–3.41) | 1.16 (0.95–1.43) | 1.50 (0.48–4.65) |
| Obesity | 1.19 (0.95–1.49) | 1.41 (0.97–2.04) | 1.19 (1.09–1.30) | 1.13 (0.57–2.21) |
| Sarcopenic Obesity | 1.06 (0.70–1.60) | 2.12 (1.42–3.17) | 1.31 (1.18–1.46) | 1.03 (0.49–2.20) |
| Adjusted Models* | n=1,352 | n=564 | n=7,441 | n=91 |
| Sarcopenia, RR (95% CI) | - | 1.44 (0.59–3.58) | 1.16 (0.94–1.42) | 1.74 (0.37–8.16) |
| Obesity | 1.19 (0.95–1.50) | 1.57 (1.06–2.34) | 1.17 (1.07–1.29) | 1.59 (0.72–3.52) |
| Sarcopenic Obesity | 1.10 (0.73–1.66) | 2.40 (1.56–3.67) | 1.24 (1.11–1.39) | 1.25 (0.58–2.68) |
Reference category is neither sarcopenic nor obese
Adjusted for age, smoking status, alcohol use, physical activity, and hormone use
DISCUSSION
Race/ethnicity findings
This is the first study to our knowledge to assess differences in sarcopenic obesity related falls by race/ethnicity. Race represents the embodiment of a social classification system “structuring opportunity and assigning value based on phenotype”.24,25 Ethnicity reflects social classification within a shared culture, Hispanic or Non-Hispanic.26 The results of this study indicate sarcopenic obesity may result in significantly greater risk of falling in Hispanic/Latina compared with Non-Hispanic White postmenopausal women. Sarcopenic obesity was the strongest risk factor for falls, suggesting the co-occurrence elevates fall risk compared to each condition separately. This result is consistent with a prior study among White older women in the New Mexico Aging Process Study, which found that sarcopenic obesity increased the risk for falls compared with either condition alone and neither condition.5 In contrast, a study in a Tasmanian cohort that found dynapenic (low muscle strength) obesity but not sarcopenic (low muscle mass) obesity was associated with an increased fall risk score.27
Obesity alone increased the risk of falls in Hispanic/Latina and Non-Hispanic White women. However, sarcopenia in non-obese women was not associated with falls among any race/ethnic group. The low prevalence of sarcopenia in non-obese women reported in our study is consistent with cross-sectional results from the National Health and Nutrition Examination Surveys (NHANES) cohort which investigators also noted that sarcopenia alone was associated with physical limitations in older adults.28
Among the Black and Native American or Alaskan Native women, results of our study showed no statistically significant difference in falls across body composition groups. Black women had the lowest prevalence of sarcopenia and sarcopenic obesity, in agreement with the weighted prevalence from the NHANES cohort.28,29 Native American or Alaskan Native women, of whom are traditionally excluded from other large cohort studies, had the highest prevalence of sarcopenic obesity and falls. Nonetheless, we acknowledge the small sample sizes of these race/ethnic groups in our study, and hence insufficient power warrants further investigation.
Obesity may be a mechanism promoting sarcopenia and increasing fall risk through balance destabilization.30 A recent study showed sarcopenic obese individuals have increased risk factors for falls and fractures including poor balance, high levels of serum parathyroid hormone and lower vitamin D levels.31 Visceral fat in the abdominal region has been shown to degrade bone by increasing proinflammatory factors.32 The deleterious effects of visceral fat related inflammation simultaneously promotes sarcopenia through muscle degradation.33 Race/ethnic differences in fall risk from sarcopenic obesity may relate to differences in the abdominal versus general obesity as Latina women are more likely to accumulate abdominal fat distribution than White women.34,35
Overall, this study is consistent with prior literature indicating the synergistic effect of low muscle mass and obesity is associated with falls, and contributes to a race/ethnic specific analysis of this association.31,10 Determining fall risk factors specific to Hispanic/Latino, Black, and Native American or Alaskan Native women in the US is critical to addressing the disproportionately increasing burden of fractures in these communities.36 Fracture rates are higher in Whites, but rates are quickly increasing in non-Whites with an expected increase from 12% in 2012 to 21% in 2025.4 Additionally, mortality rates following hip fractures are higher in non-White groups and may be related to treatment disparities such as delayed preoperative wait time to surgery following hip fractures in Blacks and Latinos.37,38 Evaluating and treating sarcopenic obesity is imperative to reduce falls, as a leading cause of fractures, particularly in Hispanic/Latina women.39 Our study suggests that clinical evaluation of sarcopenia in postmenopausal women is particularly important in fall prevention for obese Latinas. More research is needed to understand racial/ethnic differences in sarcopenic obesity related fall risk, particularly in Native American or Alaskan Natives.
Age findings
Adults 65 and over are at higher risk for falls, and most research on sarcopenic obesity has focused on subjects over 60 years old.2,11 This study shows that, among women 50–64 years old at baseline, sarcopenia and sarcopenic obesity were associated with fall risk within 7 years of follow-up. The prevalence of sarcopenic obesity increased with age, in agreement with NHANES data among adults 60 and over.28 Nevertheless, the younger age group had a slightly higher risk of falls associated with sarcopenic obesity and sarcopenia, despite a higher overall fall rate in the older age group. Fall risk increases with accumulating number of predictors, thus falls in the older age group may be better explained with a model accounting for a cluster of aging related conditions including sarcopenic obesity combined with other comorbid conditions such as decline in visual and sensory and motor functions.40 One such measure is frailty, which considers sarcopenia and age associated cumulative decline of multiple systems.41 A previous WHI study found frailty was more likely in the 70–79 years old age group compared with 65–69 year old group.42 Nonetheless, future research should be directed at identifying those at high risk for falls including adults age less than 65 years, as prior research reports 25% fall prevalence over two years in this age group.43 The current study suggests sarcopenic obesity should be evaluated in adults less than 65 years old to mitigate fall risk.
Strengths and limitations
Results should be taken with caution as the WHI cohort represents relatively healthy community-dwelling participants, and thus those most at risk for falls are not represented. The WHI exclusion criteria included institutionalization and dementia, which are each significant risk factors for falls in older adults.15 Healthy volunteer bias may underestimate sarcopenic obesity associated fall risk disproportionately in the 65–79 year old population, least likely to be represented in this cohort. Though strength or physical function have been included in definitions of sarcopenia in recent years, the present study used an historical definition of sarcopenia, as the combination of mass and function definitions did not exist during the primary WHI study period and therefore, strength measures were unavailable for this population. Even so the residual method is a strong predictor of lower extremity function.18 Falls were self-reported by participants and may be underreported due to recall bias especially among the older age stratum. Data on fall related injuries were not available. Lastly, the WHI defined race/ethnicity with the census definition of self-identified categories that may serve as proxy measurements for cultural affinity, social stratification, or ancestral origin.44 Future research using refined measurements should investigate the underlying causal risk factors for race/ethnic differences. Strengths of this study include a longitudinal study design assessing sarcopenic obesity status prior to prospectively evaluated fall outcomes. It contributes to the understanding of sarcopenic obesity related fall risk by providing race/ethnic and age specific results, and evaluating a large cohort of post-menopausal women.
Conclusion
In conclusion, sarcopenic obesity posed the highest risk of falls among Hispanic/Latina postmenopausal women. Postmenopausal women younger than 65 years were at elevated risk for sarcopenic obesity related falls. As the population ages, the growing prevalence of each condition, independently, and even more so in synergy, may place many older adults at high risk for falls. Efforts to understand changing body composition following menopause will help inform potential interventions to reduce falls. The results of this study warrant more in-depth research to elucidate race/ethnicity and age specific sarcopenic obesity prevention strategies to lessen falls as a significant public health threat.
|
Elements of
Financial/ Personal Conflicts |
*Shawna
Follis |
Alan
Cook |
Jennifer
W. Bea |
Scott B.
Going |
Deepika
Laddu |
Jane
Cauley |
Marcia
Stefanick |
Aladdin
Shadyab |
Zhao
Chen |
|||||||||
| Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation |
x | X | X | X | X | X | X | X | X | |||||||||
| Grants/Funds | x | X | X | X | X | X | X | X | X | |||||||||
| Honoraria | x | X | X | X | X | X | X | X | X | |||||||||
| Speaker Forum |
x | X | X | X | X | X | X | X | X | |||||||||
| Consultant | x | X | X | X | X | X | X | X | X | |||||||||
| Stocks | x | X | X | X | X | X | X | X | X | |||||||||
| Royalties | x | X | X | X | X | X | X | X | X | |||||||||
| Expert Testimony |
x | X | X | X | X | X | X | X | X | |||||||||
| Board Member |
x | X | X | X | X | X | X | X | X | |||||||||
| Patents | x | X | X | X | X | X | X | X | X | |||||||||
| Personal Relationship |
x | X | X | X | X | X | X | X | X | |||||||||
IMPACT Statement:
We certify that this work is novel.
The potential impact of this research on clinical care or health policy includes the following: The findings of this study aid in examining the potential impact of sarcopenic obesity on falls among race/ethnic and age groups. We expand on research in older adults to show sarcopenia and sarcopenic obesity associations with risk of falls among women are not limited to those >65 years old. The results inform fall prevention strategies tailored to race/ethnicity and age towards ameliorating this significant public health burden
ACKNOWLEDGMENTS
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201600018C, HHSN268201600001C, HHSN268201600002C, HHSN268201600003C, and HHSN268201600004C.
Funding sources: This work was supported by the Women’s Health Initiative (WHI), which is funded by the National Heart, Lung, and Blood Institute through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C.
Footnotes
Conflict of Interest Disclosures: Below is a checklist for all authors to complete and attach to their papers during submission.
REFERENCES
- 1.United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing 2015 2015;(ST/ESA/SER.A/390). doi:ST/ESA/SER.A/390
- 2.Bergen G, Stevens MR, Burns ER. Falls and Fall Injuries Among Adults Aged ≥65 Years — United States, 2014. Morb Mortal Wkly Rep 2016;65(37):993–998. doi:10.15585/mmwr.mm6537a2 [DOI] [PubMed] [Google Scholar]
- 3.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev 2006;12(5):290–295. doi:10.1136/ip.2005.011015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 2007;22(3):465–475. doi:10.1359/jbmr.061113 [DOI] [PubMed] [Google Scholar]
- 5.Baumgartner RN. Body composition in healthy aging. Ann N Y Acad Sci 2000;904:437–448. doi:10.1111/j.1749-6632.2000.tb06498.x [DOI] [PubMed] [Google Scholar]
- 6.von Haehling S, Morley JE, Anker SD. An overview of sarcopenia: facts and numbers on prevalence and clinical impact. J Cachexia Sarcopenia Muscle 2010;1(2):129–133. doi:10.1007/s13539-010-0014-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fakhouri THI, Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity among older adults in the United States, 2007–2010. NCHS Data Brief 2012;(No. 106):1–8. https://www.cdc.gov/nchs/products/databriefs/db106.htm. Accessed October 17, 2017. [PubMed] [Google Scholar]
- 8.Baumgartner RN, Wayne SJ, Waters DL, et al. Sarcopenic obesity predicts instrumental activities of daily living disability in the elderly. Obes Res 2004;12(12):1995–2004. doi:10.1038/oby.2004.250 [DOI] [PubMed] [Google Scholar]
- 9.Dufour AB, Hannan MT, Murabito JM, Kiel DP, McLean RR. Sarcopenia definitions considering body size and fat mass are associated with mobility limitations: The framingham study. Journals Gerontol - Ser A Biol Sci Med Sci 2013;68(2):168–174. doi:10.1093/gerona/gls109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scott D, Seibel M, Cumming R, et al. Sarcopenic Obesity and Its Temporal Associations With Changes in Bone Mineral Density, Incident Falls, and Fractures in Older Men: The Concord Health and Ageing in Men Project. J Bone Miner Res 2017;32(3):575–583. doi:10.1002/jbmr.3016 [DOI] [PubMed] [Google Scholar]
- 11.Cauley JA. An Overview of Sarcopenic Obesity. J Clin Densitom 2015;18(4):499–505. doi:10.1016/j.jocd.2015.04.013 [DOI] [PubMed] [Google Scholar]
- 12.Gallagher D, Ruts E, Visser M, et al. Weight stability masks sarcopenia in elderly men and women. Am J Physiol Endocrinol Metab 2000;279(2):E366–75. doi:10.1093/gerona/50a.special_issue.1 [DOI] [PubMed] [Google Scholar]
- 13.Frimel TN, Sinacore DR, Villareal DT. Exercise attenuates the weight-loss-induced reduction in muscle mass in frail obese older adults. Med Sci Sports Exerc 2008;40(7):1213–1219. doi:10.1249/MSS.0b013e31816a85ce [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The Women’s Health Initiative Study Group. Design of the Women’s Health Initiative Clinical Trial and Observational Study. Control Clin Trials 1998;19(1):61–109. doi:http://dx.doi.org/10.1016/S0197-2456(97)00078-0 [DOI] [PubMed] [Google Scholar]
- 15.Hays J, Hunt JR, Hubbell FA, et al. The women’s health initiative recruitment methods and results. Ann Epidemiol 2003;13(9):S18–S77. doi:10.1016/S1047-2797(03)00042-5 [DOI] [PubMed] [Google Scholar]
- 16.Gallagher D, Heymsfield SB, Heo M, et al. Healthy percentage body fat ranges : an approach for developing guidelines based on body mass index 1 – 3. Am J Clin Nutr 2000;72:694–701. doi:10.3945/ajcn.2009.28141.Am [DOI] [PubMed] [Google Scholar]
- 17.Harris R, Chang Y, Beavers K, et al. Risk of Fracture in Women with Sarcopenia, Low Bone Mass, or Both. J Am Geriatr Soc 2017;65(12):2673–2678. doi:10.1111/jgs.15050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newman AB, Kupelian V, Visser M, et al. Sarcopenia: Alternative Definitions and Associations with Lower Extremity Function. J Am Geriatr Soc 2003;51(11):1602–1609. doi:10.1046/j.1532-5415.2003.51534.x [DOI] [PubMed] [Google Scholar]
- 19.Anderson GL, Manson J, Wallace R, et al. Implementation of the women’s health initiative study design. Ann Epidemiol 2003;13(9):S5–S17. doi:10.1016/S1047-2797(03)00043-7 [DOI] [PubMed] [Google Scholar]
- 20.Stalenhoef PA, Diederiks JPM, Knottnerus JA, Kester ADM, Crebolder HFJM. A risk model for the prediction of recurrent falls in community-dwelling elderly: A prospective cohort study. J Clin Epidemiol 2002;55(11):1088–1094. doi:10.1016/S0895-4356(02)00502-4 [DOI] [PubMed] [Google Scholar]
- 21.Bea JW, Thomson CA, Wallace RB, et al. Changes in Physical Activity, Sedentary Time, and Risk of Falling: The Women’s Health Initiative Observational Study. Prev Med (Baltim) 2016;95:103–109. doi:10.1016/j.ypmed.2016.11.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Haring B, Pettinger M, Bea JW, et al. Laxative use and incident falls, fractures and change in bone mineral density in postmenopausal women: Results from the Women’s Health Initiative. BMC Geriatr 2013;13(1). doi:10.1186/1471-2318-13-38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hosmer DW, Lemeshow S. Applied Logistic Regression Hoboken, NJ, USA: John Wiley & Sons, Inc.; 2000. doi:10.1002/0471722146 [Google Scholar]
- 24.Jones CP. Confronting Institutionalized Racism. Phylon 2002;50(1/2):7. doi:10.2307/4149999 [Google Scholar]
- 25.Krieger N. Discrimination and health. Int J Heal Serv 2014;44(4):643–710. doi:10.2190/HS.44.4.b [DOI] [PubMed] [Google Scholar]
- 26.Ford CL, Harawa NT. A new conceptualization of ethnicity for social epidemiologic and health equity research. Soc Sci Med 2010;71(2):251–258. doi:10.1016/j.socscimed.2010.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scott D, Sanders KM, Aitken D, et al. Sarcopenic obesity and dynapenic obesity: 5-year associations with falls risk in middle-aged and older adults. Obesity 2014;22(6):1568–1574. doi:10.1002/oby.20734 [DOI] [PubMed] [Google Scholar]
- 28.Batsis JA, Mackenzie TA, Lopez-Jimenez F, Bartels SJ. Sarcopenia, sarcopenic obesity, and functional impairments in older adults: National Health and Nutrition Examination Surveys 1999–2004. Nutr Res 2015;35(12):1031–1039. doi:10.1016/j.nutres.2015.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Batsis JA, Barre LK, Mackenzie TA, et al. Variation in the prevalence of sarcopenia and sarcopenic obesity in older adults associated with different research definitions: Dual-energy X-ray absorptiometry data from the National Health and Nutrition Examination Survey 1999–2004. J Am Geriatr Soc 2013;61(6):974–980. doi:10.1111/jgs.12260 [DOI] [PubMed] [Google Scholar]
- 30.Hita-Contreras F, Martínez-Amat A, Lomas-Vega R, et al. Relationship of body mass index and body fat distribution with postural balance and risk of falls in Spanish postmenopausal women. Menopause J North Am Menopause Soc 2012;20(2):202–208. doi:10.1097/gme.0b013e318261f242 [DOI] [PubMed] [Google Scholar]
- 31.Huo YR, Suriyaarachchi P, Gomez F, et al. Phenotype of sarcopenic obesity in older individuals with a history of falling. Arch Gerontol Geriatr 2016;65:255–259. doi:10.1016/j.archger.2016.04.003 [DOI] [PubMed] [Google Scholar]
- 32.Machado LG, Domiciano DS, Figueiredo CP, et al. Visceral fat measured by DXA is associated with increased risk of non-spine fractures in nonobese elderly women: a population-based prospective cohort analysis from the Sao Paulo Ageing & Health (SPAH) Study. Osteoporos Int 2016;27(12):3525–3533. doi:10.1007/s00198-016-3682-8 [DOI] [PubMed] [Google Scholar]
- 33.Buch A, Carmeli E, Boker LK, et al. Muscle function and fat content in relation to sarcopenia, obesity and frailty of old age — An overview. Exp Gerontol 2016;76:25–32. doi:10.1016/j.exger.2016.01.008 [DOI] [PubMed] [Google Scholar]
- 34.Gonnelli S, Caffarelli C, Alessi C, Nuti R. Divergent effects of obesity on fragility fractures. Clin Interv Aging 2014;9:1629. doi:10.2147/CIA.S64625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Himes CL, Reynolds SL. Effect of obesity on falls, injury, and disability. J Am Geriatr Soc 2012;60(1):124–129. doi:10.1111/j.1532-5415.2011.03767.x [DOI] [PubMed] [Google Scholar]
- 36.Cauley JA. Defining ethnic and racial differences in osteoporosis and fragility fractures. Clin Orthop Relat Res 2011;469(7):1891–1899. doi:10.1007/s11999-011-1863-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Penrod JD, Litke A, Hawkes WG, et al. The association of race, gender, and comorbidity with mortality and function after hip fracture. J Gerontol A Biol Sci Med Sci 2008;63(8):867–872. doi:10.1109/TMI.2012.2196707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nguyen-Oghalai TU, Kuo Y, Wu H, et al. The Impact of Race/Ethnicity on Preoperative Time to Hip Stabilization Procedure after Hip Fracture. South Med J 2010;103(5):414–418. doi:10.1097/SMJ.0b013e3181d7ba2f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zingmond DS, Melton LJ, Silverman SL. Increasing hip fracture incidence in California Hispanics, 1983 to 2000. Osteoporos Int 2004;15(8):603–610. doi:10.1007/s00198-004-1592-7 [DOI] [PubMed] [Google Scholar]
- 40.Tinetti ME, Williams TF, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. Am J Med 1986;80:429–434. [DOI] [PubMed] [Google Scholar]
- 41.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001;56(3):M146–56. http://www.ncbi.nlm.nih.gov/pubmed/11253156. [DOI] [PubMed] [Google Scholar]
- 42.Fugate Woods N, LaCroix AZ, Gray SL, et al. Frailty: Emergence and Consequences in Women Aged 65 and Older in the Women’s Health Initiative Observational Study. J Am Geriatr Soc 2005;53(8):1321–1330. doi:10.1111/j.1532-5415.2005.53405.x [DOI] [PubMed] [Google Scholar]
- 43.Talbot LA, Musiol RJ, Witham EK, Metter EJ. Falls in young, middle-aged and older community dwelling adults: perceived cause, environmental factors and injury. BMC Public Health 2005;5(1):86. doi:10.1186/1471-2458-5-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harawa NT, Ford CL. The foundation of modern racial categories and implications for research on black/white disparities in health. Ethn Dis 2009;19(2):209–217. http://www.ncbi.nlm.nih.gov/pubmed/19537235. Accessed May 1, 2018. [PubMed] [Google Scholar]


