Abstract
Background:
Cardiovascular disease (CVD) risk is an important health concern among breast cancer survivors. However, few studies have examined whether trajectories of CVD risk and major risk factors are worse among women with a breast cancer diagnosis than those without.
Methods:
We compared changes in weight, body mass index (BMI), waist circumference, systolic blood pressure, and 10-year CVD risk between women with (N=813) and without (N=1049) an incident breast cancer diagnosis while enrolled in the Sister Study cohort. Blood pressure and adiposity measures were collected by trained examiners at an enrollment visit (≥1 year before breast cancer diagnosis) and a second home visit 4–11 years later (≥1 year after breast cancer diagnosis). The non-laboratory-based Framingham risk score, a measure of 10-year general CVD risk, was calculated at both the enrollment and second visits. All analyses were stratified by menopausal status at enrollment.
Results:
Women who were premenopausal at enrollment experienced moderate increases in weight, waist circumference, systolic blood pressure, and CVD risk over the study period. Those who were postmenopausal at enrollment had little change in weight, but increases in waist circumference, systolic blood pressure, and CVD risk. In both groups, changes over time did not differ significantly according to breast cancer status. Neither chemotherapy nor endocrine therapy were associated with greater increases in CVD risk or risk factors.
Conclusions:
In our cohort, changes over time in CVD risk, adiposity measures, and blood pressure were similar between women who developed an incident breast cancer and those who did not.
Keywords: breast cancer, cardiovascular disease, blood pressure, body mass index, waist circumference
Precis
Cardiovascular disease (CVD) is an important long-term health concern among breast cancer survivors. In this study, changes in traditional CVD risk factors over time did not significantly differ between women with and without an incident breast cancer diagnosis, suggesting that changes in common risk factors may not explain reported increased CVD mortality in breast cancer survivors.
Introduction
Breast cancer mortality rates have fallen by an average of 1.8% per year in the past decade, due largely to improvements in treatment and screening.1 Currently, there are >3.5 million breast cancer survivors living in the U.S, and by the year 2026, this number is projected to surpass 4.5 million.2 Thus any unique long-term health concerns of this growing population are increasingly a research priority.
Cardiovascular disease (CVD) is a key contributor to mortality among women with breast cancer, and is the leading cause of death for women with ductal carcinoma in situ or stage I disease, and for women aged 80 years and older with stage II disease.3–5 Recent evidence also supports a higher risk for CVD mortality among women with a breast cancer history compared to their cancer-free peers.6 Cardiotoxic cancer treatments, including anthracycline-based chemotherapy and trastuzumab, have been identified as contributors to CVD risk among breast cancer survivors.7 However, a higher burden of traditional CVD risk factors such as obesity and hypertension could also play an important role. Understanding trajectories of CVD risk and major risk factors among women with breast cancer may aide in the design of appropriately timed and targeted interventions to prevent CVD events in this population. Yet few studies to date have examined longitudinal patterns of CVD risk among women with breast cancer, or have compared changes over time with those of a breast cancer-free comparison group.
In this study, we evaluated changes in CVD risk factors and estimated 10-year CVD risk from pre- to post-diagnosis among women with an incident breast cancer in the National Institute of Environmental Health Sciences (NIEHS) Sister Study cohort, and compared these changes with those of women from the same cohort who remained breast cancer-free over the same time period.
Methods
Study population
The NIEHS Sister Study is a prospective cohort designed to identify genetic and environmental risk factors for breast cancer.8 Between 2003 and 2009, women from the U.S. and Puerto Rico were recruited into the Sister Study through a national multi-media campaign and a network of breast cancer professionals and volunteers. Eligible women were aged 35 to 74 years and free of breast cancer themselves at enrollment, but had a sister who had been diagnosed with breast cancer. Participants completed questionnaires at enrollment for assessment of medical conditions, medication use, and sociodemographic and lifestyle information. For women who developed an incident breast cancer (invasive or ductal carcinoma in situ), medical records were abstracted to collect information on disease stage and treatments received, including chemotherapy and endocrine therapy. If missing from medical records, or if medical records were unavailable, this information was taken from self-reported measures on a questionnaire completed by Sister Study participants approximately six months after their incident breast cancer diagnosis. The study was approved by the Institutional Review Board of the NIEHS, the National Institutes of Health, and the Copernicus Group. All participants provided written informed consent.
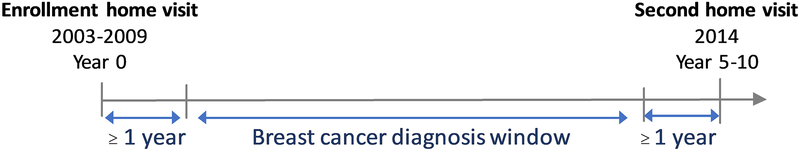
At enrollment, all Sister Study participants completed a home visit for collection of biological samples, blood pressure and anthropometric measures. In 2014, a second home visit was conducted among a subset of Sister Study participants (Figure 1). All women who had developed an incident breast cancer since enrollment were invited to participate (N=1,909), as was a randomly selected 4% subcohort (N=1,828). Of those invited, 1,215 and 1,207 women with and without a breast cancer diagnosis, respectively, completed the second home visit (participation rates: 64% and 66%). For these analyses, we further excluded women with a diagnosis of lobular carcinoma in situ (N=31), a self-reported history of heart attack, angina, heart failure, stroke, or transient ischemic attack at enrollment (N=105), and those missing information on CVD risk and risk factors (N=9). Because the estimated CVD risk measure used in these analyses was originally developed among Framingham Heart Study participants ages 30–74 years,9 we also excluded all women older than 74 years at the time of the second home visit (N=270). Among women with breast cancer, we further excluded those with less than one year between either enrollment and breast cancer diagnosis (N=134) or breast cancer diagnosis and the second home visit (N=7), and those with stage IV disease (N=4).
Figure 1.
Timeline for data collection for women with and without breast cancer in the Sister Study cohort.
CVD risk factor assessment
All anthropometric and blood pressure measures were collected by trained study personnel using the same standardized protocols at both the enrollment and second home visits. Height and weight were measured without shoes, and body mass index was calculated as weight in kilograms divided by height in meters squared (kg/m2). Waist circumference was measured over skin or lightweight clothing at the midpoint between the lowest rib on the right side and the top of the iliac crest. For blood pressure measurement, three readings, approximately 1–2 minutes apart, were taken in a seated position. Measurements were taken from alternating arms, starting with the left arm (Left → Right → Left). If both arms could not be used, three readings were taken from the available arm. The average of the three readings was used in all analyses. For women who reported taking anti-hypertensive medication on questionnaires completed at either enrollment or the second home visit, we added a constant of 15 mmHg to their measured systolic blood pressure from that visit (N=474 at enrollment; N=658 at second visit), to adjust for treatment effects.10 Smoking status and prevalent diabetes were ascertained via questionnaires completed at the enrollment and second home visits.
For each home visit, we calculated the non-laboratory-based version of the Framingham risk measure, a multivariable risk factor algorithm used to assess 10-year risk of general CVD, defined in the Framingham Heart Study as a composite of coronary heart disease, cerebrovascular events, peripheral artery disease, and heart failure.9 This risk measure incorporates information on age, diabetes, smoking, treated and untreated systolic blood pressure, and BMI, and has good discrimination relative to the full, laboratory-based Framingham risk model.9
Statistical analysis
Outcomes included changes in weight, BMI, waist circumference, systolic blood pressure, and 10-year CVD risk, calculated as the difference between the second home visit and enrollment measures. General linear models, with change as the outcome, were used to compare CVD risk and risk factor trajectories between women with and without breast cancer. All models were adjusted for the enrollment measure, age at enrollment, and time between the enrollment and second home visits. Due to evidence of differing trajectories between pre- and postmenopausal women, all analyses were stratified by menopausal status at Sister Study enrollment. We then conducted further analyses stratified by BMI at enrollment and, among women premenopausal at enrollment, by menopausal status at the second home visit. To evaluate associations between chemotherapy and/or endocrine therapy and changes in CVD risk and risk factors, we performed subgroup analyses restricting the breast cancer group to only women who had received these therapies. Among women who were premenopausal at enrollment, we also examined change in CVD risk and risk factors according to menopausal status at diagnosis (i.e. pre- or post-menopausal breast cancer). In sensitivity analyses, we excluded women who reported a diagnosis of angina, heart failure, heart attack, transient ischemic attack, or stroke between enrollment and the second home visit (N=71). We also performed sensitivity analyses using measured systolic blood pressure values that were not corrected for anti-hypertensive medication use.
Results
The average ages at enrollment among participants with and without an incident breast cancer were 47 and 46, respectively, among women who were premenopausal at enrollment, and 59 and 58, respectively, among women who were postmenopausal at enrollment (Table 1). Overall, the median time between the enrollment and second home visits was 7.8 years (IQR=6.5–8.7; range=4.4–10.8). Regardless of enrollment menopausal status or incident breast cancer status, the majority of participants were Non-Hispanic white, had a Bachelor’s degree or higher, and were never smokers.
Table 1.
Participants characteristics at Sister Study enrollment
| Premenopausal at enrollment | Postmenopausal at enrollment | |||
|---|---|---|---|---|
| Breast cancer (n=296) | No breast cancer (n=394) | Breast cancer (N=517) | No breast cancer (N=655) | |
| N(%)a | N(%)a | N(%)a | N(%)a | |
| Age (years), mean (SD) | 47.6 (5.0) | 46.6 (5.1) | 59.2 (5.1) | 58.3 (5.4) |
| Race/ethnicity | ||||
| Non-Hispanic white | 269 (91) | 333 (85) | 467 (91) | 584 (89) |
| Non-Hispanic black | 12 (4) | 36 (9) | 23 (4) | 36 (6) |
| Hispanic | 8 (3) | 20 (5) | 14 (3) | 24 (4) |
| Other | 7 (2) | 5 (1) | 12 (2) | 11 (2) |
| Education | ||||
| High school or less | 30 (10) | 44 (11) | 61 (12) | 98 (15) |
| Some college | 74 (25) | 123 (31) | 158 (31) | 205 (31) |
| Bachelor’s degree or higher | 192 (65) | 227 (58) | 297 (58) | 352 (54) |
| Household income | ||||
| Less than $50,000 | 33 (11) | 59 (15) | 95 (19) | 150 (24) |
| $50,000 to $99,999 | 113 (39) | 170 (44) | 219 (44) | 255 (40) |
| $100,000 or more | 143 (49) | 158 (41) | 183 (37) | 229 (36) |
| Smoking status | ||||
| Never | 184 (62) | 241 (61) | 268 (52) | 348 (53) |
| Former | 99 (33) | 120 (30) | 216 (42) | 263 (40) |
| Current | 13 (4) | 33 (8) | 33 (6) | 44 (7) |
| Ever diagnosed with diabetes | ||||
| Yes | 5 (2) | 11 (3) | 24 (5) | 56 (9) |
| No | 287 (97) | 373 (95) | 472 (91) | 579 (88) |
| Borderline | 4 (1) | 10 (3) | 21 (4) | 20 (3) |
| Ever diagnosed with hypertension | ||||
| Yes | 33 (11) | 46 (12) | 152 (29) | 180 (27) |
| No | 254 (86) | 338 (86) | 336 (65) | 437 (67) |
| Borderline | 9 (3) | 10 (3) | 29 (6) | 38 (6) |
| Ever diagnosed with high cholesterol | ||||
| Yes | 59 (20) | 72 (18) | 200 (39) | 258 (39) |
| No | 204 (69) | 277 (70) | 241 (47) | 315 (48) |
| Borderline | 33 (11) | 45 (11) | 75 (15) | 81 (12) |
| Age at breast cancer diagnosis, mean (SD) | 51.6 (5.3) | 62.9 (5.2) | ||
| Stage | ||||
| 0 | 75 (25) | 123 (24) | ||
| II | 135 (46) | 270 (52) | ||
| II | 67 (23) | 108 (21) | ||
| III | 19 (6) | 13 (3) | ||
| Treatment | ||||
| No chemotherapy, no endocrine therapy | 49 (17) | 85 (17) | ||
| Chemotherapy, no endocrine therapy | 37 (13) | 44 (9) | ||
| Endocrine therapy, no chemotherapy | 120 (41) | 264 (52) | ||
| Chemotherapy and endocrine therapy | 88 (30) | 115 (23) | ||
a Numbers may not sum to total due to missing
Among women who were premenopausal at enrollment, neither CVD risk nor any of the risk factors measured differed substantially at either the enrollment or second home visits between women who did and did not develop breast cancer during the study period (Supplementary Table 1). Waist circumference measured at enrollment appeared somewhat larger among postmenopausal women who went on to develop breast cancer than among those who did not (87.4 vs 85.7 cm), but no other measures differed substantially between groups at either time point.
Among women who were premenopausal at enrollment, 10-year CVD risk increased by an average of 2.7% and 2.8% among those who did and did not go on to develop breast cancer, respectively (p=0.867) (Table 2). Changes in weight, BMI, waist circumference, and systolic blood pressure were also similar between groups. No substantial differences in CVD risk or risk factor changes were observed between women with and without breast cancer in analyses stratified by either enrollment BMI or menopausal status at the second home visit, in analyses restricted to cases treated with chemotherapy and/or endocrine therapy, or in analyses according to menopausal status at diagnosis. Changes according to incident breast cancer status were also generally similar among women who were postmenopausal at enrollment, although the increase in systolic blood pressure was smaller among women with breast cancer treated with chemotherapy without endocrine therapy than among women without breast cancer (0.3 mmHg vs 4.8 mmHg; p=0.036) (Table 3). Interpretations were unchanged when women with a diagnosis of angina, heart failure, heart attack, transient ischemic attack, or stroke were excluded, and when uncorrected systolic blood pressure values were used in analyses (data not shown).
Table 2.
Adjusted mean change (95% CI) in CVD risk and risk factors between enrollment and the second home visit among women premenopausal at enrollment a
| N | 10-year CVD risk (%) | Weight (kg) | BMI (kg/m2) | Waist (cm) | Systolic BP (mmHg) | |
|---|---|---|---|---|---|---|
| All | ||||||
| BC | 296 | 2.7 (2.3, 3.1) | 1.9 (1.0, 2.8) | 0.9 (0.5, 1.2) | 4.5 (3.4, 5.5) | 4.4 (3.0, 5.7) |
| No BC | 394 | 2.8 (2.4, 3.1) | 1.6 (0.8, 2.4) | 0.8 (0.5, 1.0) | 3.7 (2.8, 4.6) | 5.6 (4.4, 6.7) |
| P-value | 0.867 | 0.648 | 0.616 | 0.248 | 0.193 | |
| BMI<25 at enrollment | ||||||
| BC | 142 | 1.8 (1.6, 2.1) | 2.3 (1.5, 3.2) | 0.9 (0.6, 1.3) | 4.9 (3.6, 6.1) | 3.8 (1.9, 5.7) |
| No BC | 193 | 1.8 (1.6, 2.0) | 2.1 (1.4, 2.9) | 0.9 (0.7, 1.2) | 4.0 (3.0, 5.1) | 5.3 (3.7, 7.0) |
| P-value | 0.992 | 0.714 | 0.995 | 0.320 | 0.236 | |
| BMI 25.0–29.9 at enrollment | ||||||
| BC | 86 | 2.7 (2.1, 3.3) | 1.5 (−0.2, 3.1) | 0.7 (0.1, 1.4) | 4.7 (3.0, 6.5) | 4.9 (2.4, 7.3) |
| No BC | 103 | 2.6 (2.1, 3.2) | 2.5 (1.0, 4.0) | 1.0 (0.5, 1.6) | 4.1 (2.5, 5.6) | 5.5 (3.3, 7.7) |
| P-value | 0.807 | 0.361 | 0.500 | 0.577 | 0.690 | |
| BMI 30+ at enrollment | ||||||
| BC | 68 | 4.6 (3.2, 6.0) | 1.4 (−1.4, 4.3) | 0.8 (−0.2, 1.9) | 3.7 (1.0, 6.4) | 5.0 (2.0, 8.0) |
| No BC | 98 | 4.9 (3.8, 6.1) | −0.3 (−2.7, 2.0) | 0.2 (−0.7, 1.0) | 2.2 (−0.0, 4.5) | 5.9 (3.5, 8.3) |
| P-value | 0.714 | 0.361 | 0.325 | 0.429 | 0.661 | |
| Premenopausal at enrollment and second visit | ||||||
| BC | 52 | 1.8 (1.3, 2.3) | 1.8 (−0.2, 3.8) | 0.7 (−0.1, 1.4) | 3.6 (1.0, 6.2) | 5.2 (2.4, 8.0) |
| No BC | 142 | 1.9 (1.6, 2.2) | 3.0 (1.7, 4.2) | 1.2 (0.7, 1.6) | 4.2 (2.6, 5.7) | 4.8 (3.1, 6.4) |
| P-value | 0.596 | 0.334 | 0.245 | 0.710 | 0.791 | |
| Premenopausal at enrollment and postmenopausal at second visit | ||||||
| BC | 243 | 3.1 (2.6, 3.6) | 1.7 (0.7, 2.8) | 0.9 (0.5, 1.2) | 4.7 (3.6, 5.8) | 4.3 (2.7, 5.8) |
| No BC | 249 | 3.1 (2.6, 3.6) | 1.0 (0.0, 2.0) | 0.6 (0.2, 0.9) | 3.4 (2.3, 4.5) | 6.0 (4.4, 7.5) |
| P-value | 0.952 | 0.298 | 0.276 | 0.097 | 0.129 | |
| Premenopausal at diagnosis | ||||||
| BC | 187 | 2.4 (2.0, 2.9) | 2.0 (0.8, 3.1) | 0.8 (0.4, 1.3) | 4.5 (3.1, 5.8) | 4.3 (2.5, 6.0) |
| No BC | 394 | 2.6 (2.3, 2.9) | 1.7 (1.0, 2.5) | 0.8 (0.5, 1.1) | 3.7 (2.8, 4.6) | 5.6 (4.4, 6.7) |
| P-value | 0.484 | 0.725 | 0.842 | 0.375 | 0.212 | |
| Postmenopausal at diagnosis | ||||||
| BC | 108 | 3.1 (2.4, 3.8) | 2.1 (0.4, 3.7) | 1.0 (0.4, 1.6) | 4.8 (3.0, 6.7) | 4.7 (2.3, 7.0) |
| No BC | 394 | 2.9 (2.5, 3.2) | 1.4 (0.6, 2.2) | 0.7 (0.4, 1.0) | 3.4 (2.5, 4.3) | 5.3 (4.1, 6.5) |
| P-value | 0.591 | 0.492 | 0.313 | 0.195 | 0.643 | |
| Chemotherapy, no endocrine therapy | ||||||
| BC | 37 | 2.0 (1.0, 3.1) | 1.1 (−1.5, 3.7) | 0.7 (−0.2, 1.7) | 4.5 (1.6, 7.5) | 2.5 (−1.4, 6.3) |
| No BC | 394 | 2.7 (2.4, 3.0) | 1.6 (0.8, 2.4) | 0.8 (0.5, 1.0) | 3.6 (2.7, 4.5) | 5.3 (4.2, 6.5) |
| P-value | 0.241 | 0.711 | 0.961 | 0.542 | 0.161 | |
| Endocrine therapy, no chemotherapy | ||||||
| BC | 120 | 2.5 (1.9, 3.1) | 2.4 (0.9, 3.9) | 1.0 (0.5, 1.6) | 4.8 (3.1, 6.4) | 3.6 (1.5, 5.8) |
| No BC | 394 | 2.7 (2.4, 3.0) | 1.6 (0.8, 2.4) | 0.8 (0.5, 1.1) | 3.6 (2.7, 4.5) | 5.5 (4.3, 6.7) |
| P-value | 0.517 | 0.350 | 0.435 | 0.239 | 0.135 | |
| Chemotherapy and endocrine therapy | ||||||
| BC | 88 | 3.0 (2.3, 3.7) | 1.5 (−0.2, 3.2) | 0.7 (0.1, 1.3) | 4.7 (2.7, 6.6) | 5.6 (3.1, 8.1) |
| No BC | 394 | 2.7 (2.4, 3.1) | 1.6 (0.8, 2.4) | 0.7 (0.5, 1.0) | 3.5 (2.6, 4.4) | 5.4 (4.3, 6.6) |
| P-value | 0.548 | 0.957 | 0.918 | 0.297 | 0.918 | |
Abbreviations: CVD, cardiovascular disease; BC, breast cancer
Adjusted for age at enrollment, time between enrollment and second visit, and enrollment measure
Table 3.
Adjusted mean change (95% CI) in CVD risk and risk factors between enrollment and the second home visit among women postmenopausal at enrollment a
| N | 10-year CVD risk | Weight (kg) | BMI (kg/m2) | Waist (cm) | Systolic BP (mmHg) | |
|---|---|---|---|---|---|---|
| All | ||||||
| BC | 517 | 4.0 (3.5, 4.5) | −0.8 (−1.4, −0.2) | −0.0 (−0.3, 0.2) | 3.1 (2.3, 3.9) | 4.5 (3.4, 5.7) |
| No BC | 655 | 4.5 (4.0, 4.9) | −0.6 (−1.1, −0.0) | 0.1 (−0.1, 0.3) | 3.4 (2.7, 4.1) | 4.9 (3.9, 6.0) |
| P-value | 0.161 | 0.600 | 0.431 | 0.547 | 0.590 | |
| BMI<25 at enrollment | ||||||
| BC | 183 | 2.9 (2.4, 3.4) | 0.7 (−0.0, 1.4) | 0.5 (0.2, 0.8) | 4.5 (3.4, 5.6) | 4.1 (2.3, 5.9) |
| No BC | 249 | 3.4 (3.0, 3.8) | 0.6 (−0.1, 1.2) | 0.4 (0.2, 0.7) | 3.7 (2.8, 4.7) | 5.2 (3.7, 6.7) |
| P-value | 0.128 | 0.781 | 0.635 | 0.295 | 0.377 | |
| BMI 25.0–29.9 at enrollment | ||||||
| BC | 183 | 4.1 (3.3, 4.8) | 0.1 (−0.9, 1.2) | 0.4 (0.0, 0.8) | 3.1 (1.9, 4.4) | 5.5 (3.6, 7.5) |
| No BC | 227 | 4.6 (4.0, 5.3) | 0.5 (−0.4, 1.4) | 0.5 (0.1, 0.8) | 4.3 (3.2, 5.5) | 6.2 (4.4, 7.9) |
| P-value | 0.266 | 0.574 | 0.801 | 0.176 | 0.642 | |
| BMI 30+ at enrollment | ||||||
| BC | 151 | 5.2 (3.9, 6.4) | −4.2 (−5.7, −2.6) | −1.3 (−1.9, −0.8) | 1.4 (−0.3, 3.0) | 3.4 (1.2, 5.7) |
| No BC | 179 | 5.9 (4.7, 7.0) | −3.1 (−4.6, −1.7) | −0.6 (−1.1, −0.1) | 1.8 (0.3, 3.3) | 3.4 (1.4, 5.5) |
| P-value | 0.416 | 0.351 | 0.073 | 0.729 | 0.997 | |
| Chemotherapy, no endocrine therapy | ||||||
| BC | 44 | 3.2 (1.5, 4.9) | −0.4 (−2.6, 1.8) | 0.0 (−0.8, 0.8) | 4.9 (2.3, 7.6) | 0.3 (−3.8, 4.4) |
| No BC | 655 | 4.3 (3.9, 4.8) | −0.4 (−1.0, 0.1) | 0.1 (−0.1, 0.3) | 3.5 (2.8, 4.1) | 4.8 (3.8, 5.9) |
| P-value | 0.212 | 0.954 | 0.735 | 0.293 | 0.036 | |
| Endocrine therapy, no chemotherapy | ||||||
| BC | 264 | 4.3 (3.6, 5.0) | −0.5 (−1.4, 0.4) | 0.1 (−0.2, 0.5) | 3.3 (2.2, 4.4) | 5.7 (4.1, 7.4) |
| No BC | 655 | 4.4 (4.0, 4.9) | −0.6 (−1.1, 0.0) | 0.1 (−0.1, 0.3) | 3.4 (2.8, 4.1) | 4.9 (3.8, 5.9) |
| P-value | 0.791 | 0.926 | 0.993 | 0.836 | 0.396 | |
| Chemotherapy and endocrine therapy | ||||||
| BC | 115 | 3.3 (2.3, 4.3) | −1.2 (−2.6, 0.2) | −0.2 (−0.7, 0.3) | 2.6 (1.0, 4.3) | 3.8 (1.3, 6.3) |
| No BC | 655 | 4.3 (3.9, 4.8) | −0.5 (−1.0, 0.1) | 0.1 (−0.1, 0.4) | 3.5 (2.8, 4.2) | 5.1 (4.1, 6.2) |
| P-value | 0.068 | 0.331 | 0.225 | 0.362 | 0.325 | |
Abbreviations: CVD, cardiovascular disease; BC, breast cancer
Adjusted for age at enrollment, time between enrollment and second visit, and enrollment measure
Discussion
In this of study of nearly 2,000 women enrolled in the prospective Sister Study cohort, pre- to post-diagnosis changes in CVD risk and risk factors among women with an incident breast cancer diagnosis did not differ substantially from changes among similarly aged women who remained free of breast cancer over the same time period. Regardless of incident breast cancer status, women who were premenopausal at enrollment experienced, on average, modest gains in CVD risk, weight, waist circumference, and blood pressure over the 4- to 11-year period. Among women who were postmenopausal at enrollment, weight remained relatively stable, while waist circumference, systolic blood pressure, and CVD risk increased to a similar extent among women with and without breast cancer. These patterns held in analyses limited to cases who received either chemotherapy or endocrine therapy.
With improvements in breast cancer survival in the past few decades, cardiovascular disease risk has increasingly become a priority health concern among breast cancer survivors. A recent systematic review examined the risk of CVD mortality following breast cancer, concluding that 2–10% of women with breast cancer die of CVD, and that CVD mortality is elevated among women with breast cancer compared to women without a breast cancer history.6 Similar to women in the general population, traditional cardiovascular disease risk factors, such as hypertension and excess adiposity, have been associated with CVD incidence and mortality among breast cancer survivors.11–13 However, whether breast cancer and its treatment exacerbate these risk factors, contributing to greater increases in CVD risk over time than among women without breast cancer, has not been well-established.
In our analyses, we used the non-laboratory-based Framingham risk measure, an estimate of 10-year general CVD risk that integrates information on age, diabetes, smoking, BMI, and treated and untreated systolic blood pressure, to compare changes in risk according to breast cancer status. Though this risk score has not been validated among women with breast cancer, and may underestimate the absolute risk in this population since it does not incorporate information on a woman’s history of cardiotoxic cancer treatments,14 it is useful as a summary measure of traditional risk factors that may increase CVD risk in both cancer and noncancer groups. To our knowledge, ours is the first study among breast cancer survivors to utilize the non-laboratory-based version of the Framingham risk score, which, unlike the full Framingham risk model, uses BMI rather than lipids in the estimation of CVD risk. Using the full risk model, a small, clinic-based study found that more women with breast cancer were considered ‘high-risk’ (10-year CVD risk > 20%) than were women without breast cancer in cross-sectional analyses.15 Breast cancer cases in their study were selected from a cardio-oncology clinic, while comparison women were selected from an Obstetrics and Gynecology clinic. In contrast, in our results, from women with and without an incident breast cancer diagnosis selected from the same parent study cohort, we did not observe evidence of substantial differences in the non-laboratory-based Framingham risk score according to breast cancer status, in either cross-sectional or longitudinal analyses.
Numerous studies have found that weight gain and adverse body composition changes are common after a breast cancer diagnosis,16 and some have speculated that unfavorable changes in these measures experienced by breast cancer survivors may exceed those experienced in the course of normal aging, with potential implications for future CVD risk. This is thought to be particularly true for women treated with chemotherapy, though recent reviews suggest that the magnitude of weight gain after chemotherapy among breast cancer patients has decreased in more recent years.16, 17 Some studies have also identified endocrine therapy as a predictor of weight gain in breast cancer survivors,18, 19 while others have not found this association.20–22 Though the consequences of weight gain for CVD among women with breast cancer remain unclear, and could depend on the timing of weight gain relative to breast cancer diagnosis, excess adiposity measured at a single time point has been positively associated with CVD incidence and mortality after breast cancer.12, 13 Thus weight, BMI, and other adiposity measures remain important outcomes to monitor in women with a breast cancer history.
While we examined changes in weight from pre- to post-diagnosis in women with an incident breast cancer diagnosis, prior studies have recruited women with a prevalent breast cancer diagnosis, and focused their analyses on weight changes occurring in the post-diagnosis period. In the Breast and Ovarian Surveillance Service (BOSS) study, a prospective cohort of individuals with a familial risk of breast and/or ovarian cancer, significantly greater gains in self-reported weight were observed in breast cancer survivors (N=303) than age-matched women without breast cancer (N=307) from the same cohort.23 However, other studies, using either self-reported24 or standardized measured weight,25 have reported no significant differences in post-diagnosis weight gain between breast cancer survivors and age-matched women without breast cancer. These findings, along with those of the current study, suggest that weight trajectories among women with breast cancer may not greatly differ from those among comparable women without a breast cancer history.
To our knowledge, our study is the first to examine pre- to post-diagnosis changes in blood pressure and CVD risk among women with an incident breast cancer. Ours is also the largest study to date to compare changes in weight among women with breast cancer to those in a comparable group of women without breast cancer. A limitation is that we lacked information on lipid profiles and blood glucose, and therefore could not evaluate changes in these measures. We also lacked information on blood pressure and anthropometric measures from around the time of breast cancer diagnosis. Therefore we could not determine whether any observed changes in weight and other factors in the breast cancer group occurred before or after diagnosis. However, our results suggest that, over a similar period, including the time surrounding both diagnosis and treatment among women with breast cancer, long-term changes in CVD risk factors do not substantially differ according to breast cancer status. The moderate participation rates among Sister Study participants invited for a second home visit are also a limitation, though participation rates were similar between women with and without breast cancer, and most enrollment characteristics that we evaluated did not meaningfully differ between women who did and did not choose to participate in the second visit (data not shown).
Among women with a breast cancer diagnosis, CVD risk is an important long-term health concern. In our study, changes over time in 10-year CVD risk, adiposity measures, and blood pressure were similar between women who developed an incident breast cancer and those who did not, suggesting that changes in common risk factors may not explain reported increased CVD mortality in breast cancer survivors.
Supplementary Material
Acknowledgments
Funding: This research was supported in part by the Intramural Research Program of the National Institutes of Health, the National Institute of Environmental Health Sciences (Z01-ES044005). C.A. was supported by the UNC Lineberger Cancer Control Education Program (T32 CA057726).
Footnotes
Conflicts of interest: None
References
- 1.American Cancer Society. Cancer Facts & Figures 2017. Atlanta: American Cancer Society; 2017. [Google Scholar]
- 2.American Cancer Society. Cancer Treatment & Survivorship Facts & Figures 2016–2017. Atlanta: American Cancer Society; 2016. [Google Scholar]
- 3.Patnaik JL, Byers T, DiGuiseppi C, Dabelea D, Denberg TD. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res. 2011;13: R64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patnaik JL, Byers T, Diguiseppi C, Denberg TD, Dabelea D. The influence of comorbidities on overall survival among older women diagnosed with breast cancer. J Natl Cancer Inst. 2011;103: 1101–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schonberg MA, Marcantonio ER, Ngo L, Li D, Silliman RA, McCarthy EP. Causes of death and relative survival of older women after a breast cancer diagnosis. J Clin Oncol. 2011;29: 1570–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gernaat SAM, Ho PJ, Rijnberg N, et al. Risk of death from cardiovascular disease following breast cancer: a systematic review. Breast Cancer Res Treat. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Accordino MK, Neugut AI, Hershman DL. Cardiac effects of anticancer therapy in the elderly. J Clin Oncol. 2014;32: 2654–2661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sandler DP, Hodgson ME, Deming-Halverson SL, et al. The Sister Study Cohort: Baseline Methods and Participant Characteristics. Environ Health Perspect. 2017;125: 127003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D’Agostino RB Sr., Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117: 743–753. [DOI] [PubMed] [Google Scholar]
- 10.Tobin MD, Sheehan NA, Scurrah KJ, Burton PR. Adjusting for treatment effects in studies of quantitative traits: antihypertensive therapy and systolic blood pressure. Stat Med. 2005;24: 2911–2935. [DOI] [PubMed] [Google Scholar]
- 11.Park NJ, Chang Y, Bender C, et al. Cardiovascular disease and mortality after breast cancer in postmenopausal women: Results from the Women’s Health Initiative. PLoS One. 2017;12: e0184174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simon MS, Beebe-Dimmer JL, Hastert TA, et al. Cardiometabolic risk factors and survival after breast cancer in the Women’s Health Initiative. Cancer. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cespedes Feliciano EM, Kwan ML, Kushi LH, Weltzien EK, Castillo AL, Caan BJ. Adiposity, post-diagnosis weight change, and risk of cardiovascular events among early-stage breast cancer survivors. Breast Cancer Res Treat. 2017;162: 549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Law W, Johnson C, Rushton M, Dent S. The Framingham risk score underestimates the risk of cardiovascular events in the HER2-positive breast cancer population. Curr Oncol. 2017;24: e348–e353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shum K, Solivan A, Parto P, Polin N, Jahangir E. Cardiovascular Risk and Level of Statin Use Among Women With Breast Cancer in a Cardio-Oncology Clinic. Ochsner J. 2016;16: 217–224. [PMC free article] [PubMed] [Google Scholar]
- 16.Vance V, Mourtzakis M, McCargar L, Hanning R. Weight gain in breast cancer survivors: prevalence, pattern and health consequences. Obes Rev. 2011;12: 282–294. [DOI] [PubMed] [Google Scholar]
- 17.van den Berg MM, Winkels RM, de Kruif JT, et al. Weight change during chemotherapy in breast cancer patients: a meta-analysis. BMC Cancer. 2017;17: 259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mortimer J, Behrendt CE. Severe menopausal symptoms are widespread among survivors of breast cancer treatment regardless of time since diagnosis. J Palliat Med. 2013;16: 1130–1134. [DOI] [PubMed] [Google Scholar]
- 19.Sadim M, Xu Y, Selig K, et al. A prospective evaluation of clinical and genetic predictors of weight changes in breast cancer survivors. Cancer. 2017;123: 2413–2421. [DOI] [PubMed] [Google Scholar]
- 20.Makari-Judson G, Judson CH, Mertens WC. Longitudinal patterns of weight gain after breast cancer diagnosis: observations beyond the first year. Breast J. 2007;13: 258–265. [DOI] [PubMed] [Google Scholar]
- 21.Vagenas D, DiSipio T, Battistutta D, et al. Weight and weight change following breast cancer: evidence from a prospective, population-based, breast cancer cohort study. BMC Cancer. 2015;15: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sestak I, Harvie M, Howell A, Forbes JF, Dowsett M, Cuzick J. Weight change associated with anastrozole and tamoxifen treatment in postmenopausal women with or at high risk of developing breast cancer. Breast Cancer Res Treat. 2012;134: 727–734. [DOI] [PubMed] [Google Scholar]
- 23.Gross AL, May BJ, Axilbund JE, Armstrong DK, Roden RB, Visvanathan K. Weight change in breast cancer survivors compared to cancer-free women: a prospective study in women at familial risk of breast cancer. Cancer Epidemiol Biomarkers Prev. 2015;24: 1262–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sedjo RL, Hines LM, Byers T, et al. Long-term weight gain among Hispanic and non-Hispanic White women with and without breast cancer. Nutr Cancer. 2013;65: 34–42. [DOI] [PubMed] [Google Scholar]
- 25.Freedman RJ, Aziz N, Albanes D, et al. Weight and body composition changes during and after adjuvant chemotherapy in women with breast cancer. J Clin Endocrinol Metab. 2004;89: 2248–2253. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.