Abstract
Background:
Rosacea is a common chronic cutaneous disorder which is characterized by flushing, erythema, papulopustules and telangiectasia. The pathogenesis of the disease is still unknown. A multifaceted approach is necessary to control the disease because of its tendency to relapse. New more effective treatment options are desirable to achieve a complete remission. Aminolevulinic acid–photodynamic therapy (ALA-PDT) is a well-established treatment for non-melanoma skin cancer and precancerous lesions. ALA-PDT can also be used for inflammatory disease, including acne vulgaris. However, little is known about the efficacy and safety of ALA-PDT for rosacea in Chinese patients with Fitzpatrick skin types III and IV.
Objectives:
To investigate the efficacy and safety of ALA-PDT in the treatment of rosacea classified as erythematotelangiectatic type or papulopustular type.
Methods:
Twenty rosacea patients with either erythematotelangiectatic or papulopustular types were enrolled. 5% 5-Aminolevulinic acid in an oil-in-water emulsion was applied to the lesions under occlusion with plastic film for 2h, and the lesions were irradiated with 100 mW/cm2, 80-90 J/cm2, LED red light (635 ± 15 nm) over 15 minutes in each session with four sessions at 10-day intervals. Objective measures (severity of flushing, erythema and telangiectasia, number of inflammatory lesions, VISIA Red Complexion Analysis images), subjective symptoms (including itching, prickling, burning, etc.) were recorded at baseline and at 4, 12 and 24 weeks after the last treatment. Adverse effects were recorded at each treatment and follow-up visit.
Results:
During the follow-up period, all patients showed gradual objective clinical improvement compared with baseline (P<0.01). Clinical inflammatory lesions disappeared completely in all patients after 24 weeks. Subjective symptoms, including flushing, itching, prickling, burning et at, had vanished and did not show any relapse during the follow-up period. The main side effects of ALA-PDT were pain, erythema, swelling and post- inflammatory hyperpigmentation. All side-effects were transient and tolerated by all the patients. No patients were dissatisfied with the therapeutic outcome.
Conclusions:
ALA-PDT is an effective and safe approach for the treatment of rosacea of erythematotelangiectatic or papulopustular types, to control clinical manifestations and reduce subjective symptoms.
Keywords: rosacea, 5-aminolevulinic acid, photodynamic therapy, red light emitting diodes, Chinese skin types, erythemato-telangiectatic or papulopustular types
Introduction
Rosacea is a common inflammatory skin condition, which affects up to 1-20% of the general Population1 with primary features of centrofacial flushing, erythema, papules and pustules, telangiectasia, and a combination of secondary features including edema, dryness, itching, stinging and burning. Rosacea has been divided into four subtypes, erythemato-telangiectatic, papulopustular, phymatous and ocular, each with its own characteristic features 2. Different specific external triggers like hot or cold temperature, UV light exposure, spicy foods, alcohol, exercise and psychological stress may exacerbate flushing and have been blamed for frequent flare-ups3. The intermittent course of the disease and the need for repeated treatment can be frustrating and significantly affect the patient’s quality of life.
The precise pathogenesis of rosacea remains unclear. Systemic medication (including doxycycline hydrochloride, minocycline hydrochloride, isotretinoin, etc) and topical therapies (including metronidazole, azelaic acid, benzoperoxide, calcineurin inhibitors, α-adrenergic receptor agonists, etc) have been used in various combinations for the treatment of rosacea 4. Nevertheless in many patients, standard treatment is still not particularly effective, especially for controlling flushing. Therefore, it is necessary to develop new alternative treatment modalities for rosacea.
Photodynamic therapy (PDT) is a recently adopted modality which employs a harmless photosensitizer and optimum wavelength light, leading to production of singlet oxygen and cytotoxic reactive oxygen species, which can selectively damage target tissue or microorganisms. Topically applied 5-aminolevulinic acid (ALA) or methylaminolevulate (MAL), a precursor in the heme biosynthetic pathway, leads to accumulation of the photosensitizer protoporphyrin IX (PPIX) within the target cells. Illumination destroys target tissue, regulates the local immunological reaction and modulates the chronic inflammatory process. ALA-PDT has been used to treat basal cell carcinoma, actinic keratoses, acne, psoriasis, viral warts, port-wine stains and other dermatological disorders5. The range of indications has expanded recently, and good outcomes have been documented for treatment of rosacea using PDT6. Here we present a pilot study using ALA-PDT to treat 20 Chinese rosacea patients with Fitzpatrick skin types III and IV.
Methods
Patients
We performed a prospective study of patients with rosacea who were admitted to our department between October 2015 to June 2017.All patients were enrolled with a clinical diagnosis of rosacea classified as erythemato-telangiectatic or papulopustular subtype. The clinical manifestations of rosacea were papules, pustules, erythema, edema, and flushing with or without telangiectasia. All patients had previously received various conventional medical treatments, including oral preparations and topical medicines, however, after stopping treatment, the clinical signs returned. These therapies in general only produce a temporary improvement in symptoms without long-term remission. Before receiving PDT, all patients provided informed written consent to the procedure. All the clinical manifestations were recorded including objective and subjective symptoms. The clinical study was approved by the local ethics committee (IRB) of Southwest Hospital, Chongqing, China and was in accord with the Declaration of Helsinki.
Photodynamic therapy
Prior to every treatment and follow-up visit photographs of the rosacea lesions were captured by the VISIA 6.0 Complexion Analysis System (Canfield Scientific Inc, USA). Freshly prepared 5% 5-aminolevulinic acid in an oil-in-water emulsion (Shanghai Fudan- Zhangjiang Bio-Pharmaceutical Co. Ltd, Shanghai, China) was applied to the lesions with a 1-cm margin under occlusion with plastic film for 2h. The lesions were irradiated with 100 mW/cm2, 80-90 J/cm2, LED red light (635 nm ± 15 nm) (Omnilux Revive, Photo Therapeutics, Inc, London, UK) for 15 minutes. All patients received same ALA-PDT treatment regimen delivered four times at 10 day intervals 7 and were followed-up at 4, 12, 24-weeks. All patients received no other medical treatment or conventional therapy during the treatment, just the use of moisturizing cream twice a day (Cetaphil Moisturizing Cream, Galdema Company, France).
Clinical evaluation
The efficacy of the treatment was evaluated by the improvement in both the objective and subjective symptoms of the rosacea patients, as well as the Physician’s Global Assessment (PGA) at each follow-up visit by three external blinded dermatologists. Objective features (including flushing, erythema, telangiectasia) were graded using a scale based on “Standard Grading System for Rosacea” 2: Flushing [0 = none,1 = mild (slight, transient, not obvious), 2 = moderate (worse than 1 and better than 3), 3 = severe (persistent, frequently, obvious)]; Erythema [0 = none,1 = mild (slight, either with restricted central involvement or generalized over the whole face), 2 = moderate (pronounced, centrally restricted or generalized on the face), 3 = severe (severe over the whole face)]; Telangiectasia [0=none,1=mild (fine vessels < 0.2 mm in diameter covering < 10% of the face), 2=moderate (several fine vessels and/or a few large vessels > 0.2mm in diameter covering 10–30% of the face), 3=severe (many fine and/or large vessels covering >30% of the face)]. The numbers of papule/pustules were recorded prior to every treatment and at each follow-up visit. Values of the VISIA Red images were calculated to compare the changes in red/inflamed skin with a decreased score indicating improvement in erythema and telangiectasia. Subjective symptoms (include itching, prickling, burning, etc) were graded on the following scale: 0 = absent; 1 = mild (occasional, slight); 2 = moderate (more obvious, lasting); 3 = severe (significant or persistent, affects daily living). The PGA was performed using a 7-point scale7: 0 = clear, 1 = minimal, 2 = mild, 3 = mild to moderate, 4 =moderate, 5= moderate to severe, and 6= severe. Evaluation criteria: 0=clear (almost no roseacea (ie, no papules and/or pustules; no or residual erythema; mild to moderate degree of telangiectasia may be present); 1=minimal (rare papules and/or pustules; residual to mild erythema; mild to moderate degree of telangiectasia may be present); 2= mild (few papules and/or pustules; mild erythema; mild to moderate degree of telangiectasia may be present); 3=mild to moderate (distinct number of papules and/or pustules; mild to moderate erythema; mild to moderate degree of telangiectasia may be present); 4=moderate (pronounced number of papules and/or pustules; moderate erythema; mild to moderate degree of telangiectasia may be present); 5=moderate to severe (many papules and/or pustules; occasionally with large inflamed lesions, moderate erythema; moderate degree of telangiectasia may be present); 6=severe (numerous papules and/or pustules; occasionally with confluent areas of inflamed lesions, moderate to severe erythema; moderate to severe degree of telangiectasia may be present).
Patients were asked to carry out self-assessment for rosacea symptoms by the Patient’s Global Improvement Assessment. At 4-, 6- and 24 -weeks follow-up visits after the last treatment, patients were requested to grade the improvement of rosacea as 1=good, 2=fair, 3=poor, 4=even worse8. The treatment related pain was recorded using a visual analogue scale (VAS) of 0 to 10 mm (0 = no pain and 10 = extremely painful) during each session of PDT. Patients’ tolerance to treatment and adverse effects were also recorded after each treatment and at subsequent follow-up visits. Patients’ satisfaction for ALA-PDT was rated on a scale of 0 to 3 (dissatisfied=0, somewhat satisfied=1, satisfied=2, very satisfied=3) where a higher score indicated more satisfaction9.
Statistical analysis
Scores of individual symptoms, counts of inflammatory lesions, values of the VISIA Red images and the Physician’s Global Assessment between baseline and follow-up visit were statistically analyzed with Wilcoxon signed rank test, repeated-measures analysis of variance test or Friedman test. Differences of Patient’s Global Improvement Assessment and satisfaction at each visit were assessed using chi-square test. All analyses were performed using Statistical Package for Social Sciences (SPSS) version 13.0. A probability less than 0.05 was considered statistically significant.
Results
20 Patients were enrolled in the study from 2015 to 2017, 20 (18 women and 2 men) with an age range of 19–51 years (mean, 37 y) completed 4 sessions of PDT and the 6-month follow-up visits. The duration of disease ranged from 4 to 120 months (median 22 m).The 20 patients all showed erythema, papules, pustules and presented one or more subjective symptoms. All patients presented with a history of flushing and 7 patients showed fixed erythema on the face. 15 patients had lesions involving the cheeks, 3 patients involved the nose and paranasal area, the other 2 patients involved cheeks and the anterior part of the chest. The features of the participants were in accord with typical characteristics of rosacea patients (Table 1).
Table 1.
Basic information of patients
| Characteristic | Value |
|---|---|
| Age (years), mean±SD | 37 ±10.7 |
| Gender (M/F) | 2/18 |
| Disease history (month), median (range) | 22 (4,120) |
| Physician’s Global Assessment, n (%) | |
| Mild | 0 (0%) |
| Mild to moderate | 1 (5%) |
| Moderate | 7 (35%) |
| Moderate to severe | 9 (45%) |
| Severe | 3 (15%) |
| Skin phototype, n (%) | |
| Ⅲ | 11 (55%) |
| Ⅳ | 9 (45%) |
| Affected areas, n (%) | |
| Cheek | 15 (75%) |
| Nose and paranasal area | 3 (15%) |
| Anterios part of chest | 2 (10%) |
| Manifestation, n (%) | |
| Flushing | 20 (100%) |
| Erythema | 18 (90%) |
| Telangiectasia | 2 (10%) |
| Papulo-pustules | 18 (90%) |
| Subjective symptoms | |
| Burning | 15 (75%) |
| Prickling | 4 (20%) |
| Itching | 18 (90%) |
| Numbers of baseline papules and pustules (mean ± SD/median, range) |
35.9 ±16.3/35 (5, 60) |
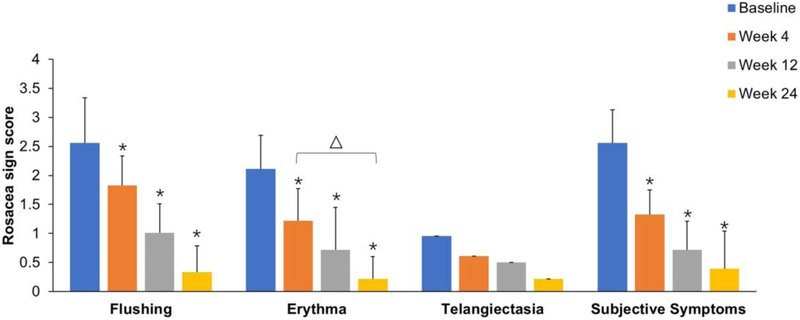
The scores of objective and subjective rosacea symptoms at baseline and post-treatment are presented in Table 1. All patients showed a significant improvement in clinical signs of rosacea after treated by ALA–PDT. At the last follow-up visit, the mean score (±SD) of flushing was reduced from 2.56 ± 0.78 to 0.33 ± 0.49 (P<0.01) compared with the baseline score. There was statistical difference in flushing severity index between a follow-up period of 4 weeks and 12 weeks (P=0.025). The most significant improvements in flushing were detected at week 4 with a reduction from baseline of 87.1%. Overall facial erythema improved significantly during the follow-up visit time. The mean erythema scores (±SD) decreased from 2.11 ± 0.58 at baseline to 0.22 ± 0.43 at week 24 gradually with a 89.5% reduction based on the 4-point scale (P<0.01). There was a statistical difference in erythema between the 1st and 3rd follow-up visit (P=0.008). The scores of telangiectasia were reduced in 4 out of 7 patients at the 1st follow-up visit. But there were no statistically significant decreases between baseline and each follow-up visit (P>0.05) (Fig 1).
Figure 1.
Changes from baseline in flushing, erythema, telangiectasia and subjective symptoms at weeks 4, 12 and 24 after the last treatment. There was a statistically significant difference between baseline and all the time points post-treatment except in the telangiectasia score (P> 0.05). *P< 0.01 vs baseline;ΔP< 0.05.
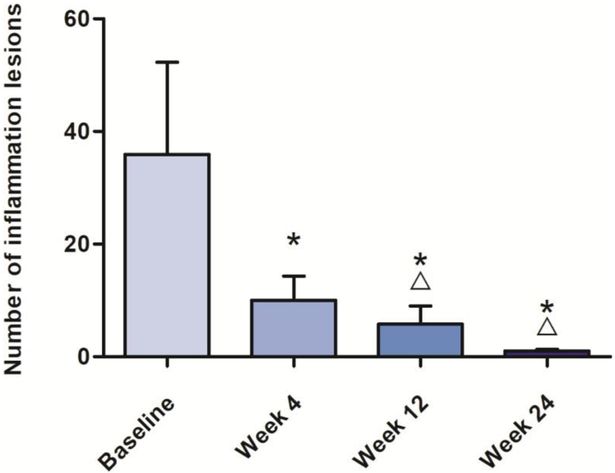
All the 20 patients showed amelioration of the papulopustular symptoms at the follow-up visits. The mean (±SD) number of inflammatory lesions (pustules and papules) decreased from 35.9±16.3 at baseline to 1.0±0.3 at the last follow-up visit (figure 2).The mean percent reduction in inflammatory lesion numbers was 97.2% (P<0.01).
Figure 2.
Mean±SD numbers of inflammatory lesions at baseline and follow-up visits treated with ALA-PDT. *P<0.01 vs baseline. ΔP< 0.05.
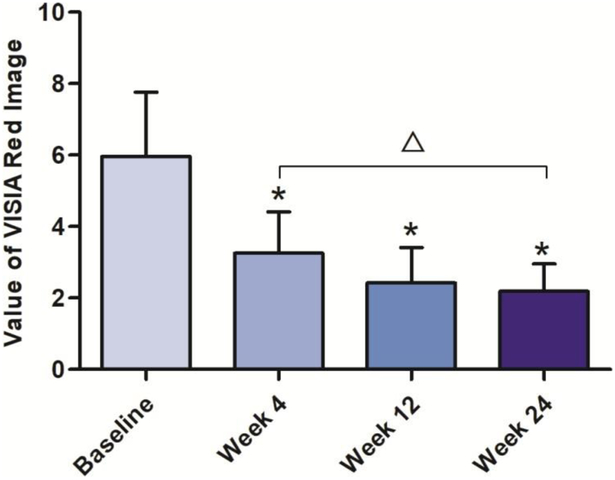
Statistically significant improvements in red/inflamed skin determined by values of the VISIA Red images were detected before and at 4 weeks with mean scores continuing to decline after 12 and 24 weeks. The mean score (±SD) of baseline was 5.96 ± 1.80 which decreased to 2.19±0.77 at week 24. A statistical difference was demonstrated between the beginning and end of the 24-week follow-up (Figure 3).
Figure 3.
Improvement in red/inflamed skin from baseline. *P<0.01 vs baseline; Δ P< 0.05.
15 patients complained of burning symptoms, while 4 patients complained of prickling and 18 patients complained of itching (mild to severe degree) before the ALA-PDT therapy. During the 24-week follow-up visits, the complaints of subjective symptoms disappeared completely in 16 patients, and the other 4 patients experienced only occasional burning less than at baseline. The mean score (±SD) of subjective symptom severity index decreased from 2.58±0.57 to 0.39±0.50 (Figure 1, P<0.01).
The Physician’s Global Assessment (PGA) showed a progressive increase in overal improvement. At baseline, the majority of patients (n=16, 80%) had ratings of "moderate" "moderate to severe" and "severe" on the PGA. After PDT ratings dropped to "clear" in 4 of the total cases, to "minimal" in 12 cases and to "mild" in 2 cases at 24 weeks (Table 2). The difference between baseline and post-treatment was statistically significant (P<0.01).
Table 2.
Physicians’ Global Assessment of the improvement of rosacea after four treatments.
| Clear | Minimal | Mild | Mild to moderate |
Moderate | Moderate to severe |
Severe | |
|---|---|---|---|---|---|---|---|
| Baseline | 0(0.0%) | 0(0.0%) | 1(5.0%) | 1(5.0%) | 7(35.0%) | 8(40.0%) | 3(15.0%) |
| Week 4 | 0(0.0%) | 8(40.0%) | 6(30.0%) | 3(15.0%) | 1(5.0%) | 2(10.0%) | 0(0.0%) |
| Week 12 | 2(10.0%) | 10(50.0%) | 6(30.0%) | 1(5.0%) | 1(5.0%) | 0(0.0%) | 0(0.0%) |
| Week 24 | 4(20.0%) | 12(60.0%) | 3(15.0%) | 1(5.0%) | 0(0.0%) | 0(0.0%) | 0(0.0%) |
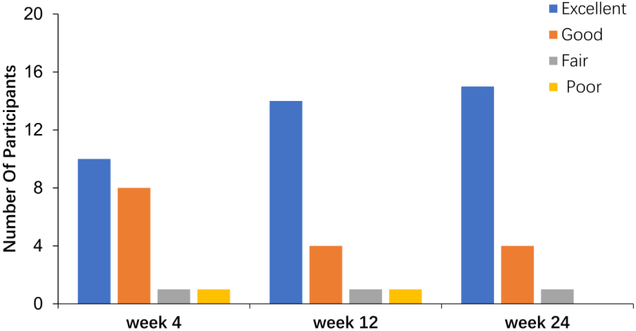
Patient’s Global Improvement Assessment scores at 24 weeks after the last session,15 patients (80%) reported a significant improvement in their signs and symptoms, 4 patients (20%) reported "good" improvement, 1 patient (5%) reported a "fair" improvement. The self-assessment scores for the patients are summarized in figure 4.
Figure 4.
The values of the Patient’s Global Assessment for improvement in overall severity at the follow- up periods. (P>0.05)
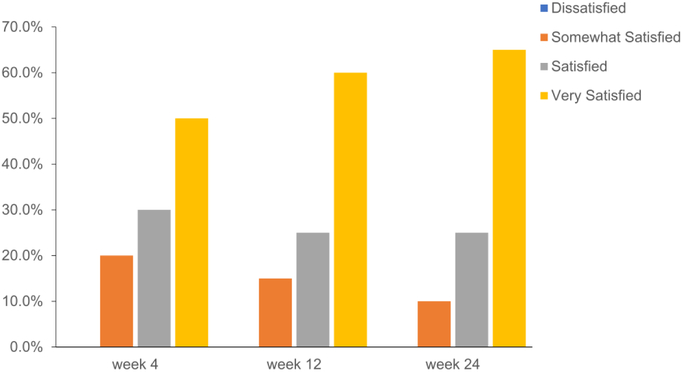
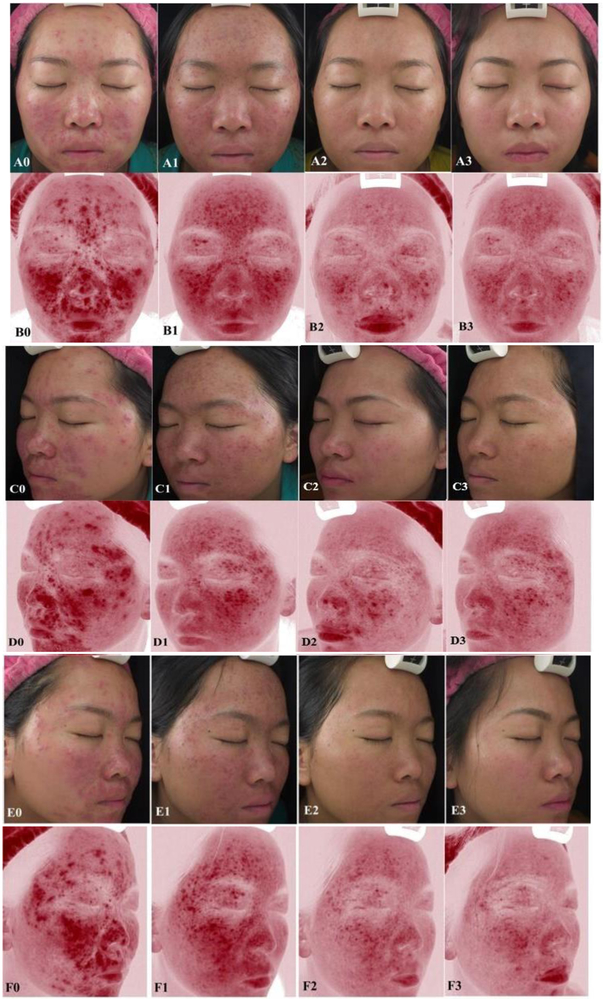
After four ALA-PDT treatments and three follow-up visits, participants rated their satisfaction revealing that 13 (65%) patients were “very satisfied”, 5 (25%) patients were “satisfied” and 2 (10%) was “somewhat satisfied” at the last follow-up visit. No patients were dissatisfied at the clinical response of the treatment (Figure 5). A typical clinical series of photographs are show in Fig 6.
Figure 5.
The satisfaction levels for the overall improvement and safety at weeks 4,12, 24.
Figure 6.
A single typical case originally presenting with moderate erythema and severe papulopustules who showed a significant improvement after 4-treatment sessions of PDT. (front A 0-3), (left side C 0-3), (right side E 0-3), photographs; and (front B 0-3), (left side D 0-3), (right side F 0-3), VISIA Red images. (A0-F0) baseline before treatment, (A1-F1) at the 4 week visit after 4 treatments; (A2-F2) continued improvement at 12 weeks; (A3-F3) at 24 week visit.
Side effects
All 20 participants suffered from transient pain during the treatments especially in the first 5 min. They could all tolerate the pain with the average pain index score being 3.6±1.1. In addition, the most common treatment-related cutaneous adverse events (AEs) were erythema and swelling, lasting up to 2 days. All patients who experienced the side effects described above could tolerate them. 4 patients (20.0%) showed desquamation and post-inflammatory hyperpigmentation classed as “moderate” after the treatment. 3 of these underwent completely recovery in 1 week and the other case showed slight hyperpigmentation lasting more than 3-months. There was no relapse of erythema, papules or pustules during the 24 week period of follow-up.
Discussion
Rosacea has several features in common with acne. Some treatment methods for acne vulgaris and rosacea, such as antibiotics, retinoids, azelaic acid, etc, show overlap in mechanistic rationale and in clinical practice. PDT has been widely accepted as an effective and safe choice to treat acne because of its potential modulatory function on the pilosebaceous unit and amelioration of the local inflammatory environment 7, 10. Results in acne have led more and more investigators to conduct trials to treat rosacea with PDT. A study performed by Nybaek first described that PDT may be useful in selected cases of rosacea 11. Furthermore, Katz reported an efficacious case study using PDT for the treatment of erythema, papules, pustules and severe flushing consistent with rosacea12. Bryld reported an apparent beneficial effect and further assessed the possible benefit of MAL-PDT in a series of rosacea patients13. Our study also showed a gradual decrease of flushing, erythema and inflammatory lesions in 20 erythemato-telangiectatic or papulopustular rosacea patients after receiving PDT. Objective symptoms as well as subjective symptoms were improved significantly without any relapse during the 24-week follow-up visit.
Although the clinical results have proven the efficacy of PDT in the treatment of rosacea, the exact mechanism by which PDT works in rosacea is not entirely clear. There are several factors hypothesized to support the mechanism of PDT in alleviating symptoms. (1) Dysfunction of the innate immune system is proposed to be associated with the pathogenesis of rosacea. PDT could lead to increased TLR expression and downregulation of cytokine secretion 14, PDT could modulate the immune system and induce apoptosis of T cells. Matrix metalloproteinase MMP-1 and MMP-3 are also secreted by fibroblasts in response to PDT15. These factors could explain immunomodulatory effects on rosacea patients. (2) Microbial stimuli, including Bacillus including Bacillus oleronius, Staphylococcus epidermidis, Demodex folliculorum etc. also have been speculated to contribute to the pathophysiology of rosacea16. The photodynamic effect against various microorganisms has already been published in numerous in vitro and in vivo studies including its effectiveness against Demodex infection17. The therapeutic mechanism of PDT in rosacea may have a relationship with the antimicrobial effect reducing inflammatory processes18.
Based on our clinical results, rosacea could be well-controlled by PDT. PDT led to a rapid and noticeable resolution of inflammatory lesions starting at the 1st follow-up visit and lasting for a sustained period. Among the clinical signs and features of rosacea, the greatest degree of improvement was seen in papule-pustules, followed by improvements erythema. This supports the effect of ALA-PDT on inhibition of sebaceous gland function and reduction of inflammation playing an important role in the treatment of rosacea. There were obvious differences in the number of papules and pustules between before treatment and at 24-week follow-up visit. The results of erythema severity index continued to decline during the last two follow-up visits and were consistent with values of VISIA Red images. It confirmed that patients experienced further improvement at week 12 and 24 after the last treatment session. Flushing can be very difficult to control in rosacea. However, PDT was able to control flushing at 4 weeks after treatment. Subjective symptoms (including itching, prickling, burning etc) had almost disappeared without any relapse seen during the follow-up visits. No significant differences were seen when comparing the improvement in telangiectasia. This may be because topically applied ALA could not penetrate into the capillary vessels and accumulate into vascular endothelial cells. Therefore ALA-PDT could not destroy established telangiectasia. Based on our data, PDT seemed to be somewhat more efficient against the papulopustular and inflammatory symptoms than against angiotelectasis. Therefore, PDT may be very suitable for the of papulopustular and erythematotelangiectatic subtypes of rosacea, (since the latter has an elevated inflammatory status) which is not the case for established angiotelectasis.
In our study, 2 patients who rated themselves as “somewhat satisfied” described their improvement as ‘poor’ with remaining mild to moderate erythema, had a few papules or pustules on the nose at the baseline assessment. combined with Fitzpatrick IV type skin. We speculate that the sebaceous glands of the nose which are widely distributed, and the function may return even after having been destroyed by PDT.
Generally, a strong irritant reaction that occurs in the three days after PDT appears to be able to treat inflammatory cutaneous diseases. This may be a case of acute inflammation treating chronic inflammation. However on the other hand, it is known that rosacea is easily aggravated by various physical and environmental triggering factors. At high levels of PDT, it is possible that flares of rosacea might be triggered by an excessive amount of ROS. It is important to choose proper parameters to relieve inflammation, flushing, telangiectasia while avoiding irritating the skin or exacerbating the rosacea symptoms at the same time. We used a moderate-dose of red light combined with 5% ALA-PDT in our study. No aggravation in the severity of the erythema or inflammatory lesions was observed. Friedman et al demonstrated that there was no statistically significant difference in patient-reported efficacy when they applied multiple, sequential light and laser sources in ALA-PDT for rosacea19.The optimum light source and PDT parameters still require further study.
The majority of patients with mild rosacea symptoms can be relieved by pharmaceutical treatment. Most of our patients were graded as moderate-severe, and were resistant to medication or easily relapsed after medication. PDT is an excellent alternative treatment choice for these patients who want to end their reliance on long-term medication. PDT could even control rosacea flares to a certain extent. However, a greater number of cases, including control groups (or a control area on the same patient) should be included to demonstrate the therapeutic effect of PDT on rosacea. Objective and standard assessments are needed with further refinement.
Conclusion
This study suggests that papulopustular rosacea patients obtained the best therapeutic benefit of ALA-PDT among the 4 rosacea subtypes, followed by the erythematotelangiectatic type. The treatment was safe and well tolerated. However, large sample data and controlled clinical trials are necessary for verification.
Highlights.
A clinical trial of ALA-PDT in 20 Chinese patients with rosacea
Four sessions of PDT at 10 day intervals with six months follow up
All patients (100% response rate) showed improvement with no recurrence
Papulopustular and erythematotelangiectatic sub-types showed best response
Side-effects (pain, erythema, edema) were transient and well tolerated
Acknowledgments
Conflict of Interest Disclosures: Dr. Rui Yin received research grant (No. 81571902) from National Natural Science Foundation of China and clinical research grant (SWH2014LC17) from Southwest Hospital, Third Military Medical University for this work. Michael R Hamblin was supported by US NIH grants R01AI050875 and R21AI121700. No authors hold stock, or receive royalties from any companies.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tan J, Berg M. Rosacea: current state of epidemiology. J AM ACAD DERMATOL 2013; 69:S27–35. [DOI] [PubMed] [Google Scholar]
- 2.Wilkin J, Dahl M, Detmar M et al. Standard grading system for rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J AM ACAD DERMATOL 2004; 50: 907–12. [DOI] [PubMed] [Google Scholar]
- 3.Two AM, Wu W, Gallo RL et al. Rosacea Part I. Introduction, categorization, histology, pathogenesis, and risk factors. J AM ACAD DERMATOL 2015; 72: 749–58. [DOI] [PubMed] [Google Scholar]
- 4.Abokwidir M, Feldman SR. Rosacea Management. Skin Appendage Disorders 2016; 2: 26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wen X, Li Y, Hamblin MR. Photodynamic therapy in dermatology beyond non-melanoma cancer: an update. Photodiagnosis Photodyn Ther 2017; 19: 140–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ozog DM, Rkein AM, Fabi SG et al. Photodynamic Therapy: A Clinical Consensus Guide. DERMATOL SURG 2016; 42: 804–27. [DOI] [PubMed] [Google Scholar]
- 7.Yin R, Hao F, Deng J, et al. Investigation of optimal aminolaevulinic acid concentration applied in topical aminolaevulinic acid-photodynamic therapy for treatment of moderate to severe acne: a pilot study in Chinese subjects. Br J Dermatol, 2010, 163:1064–71. [DOI] [PubMed] [Google Scholar]
- 8.Breneman D, Savin R, VandePol C et al. Double-blind, randomized, vehicle- controlled clinical trial of once-daily benzoyl peroxide/clindamycin topical gel in the treatment of patients with moderate to severe rosacea. INT J DERMATOL 2004; 43: 381–7. [DOI] [PubMed] [Google Scholar]
- 9.Czernielewski J, Liu Y. Comparison of 15% azelaic acid gel and 0.75% metronidazole gel for the topical treatment of papulopustular rosacea. Arch Dermatol 2004; 140: 1282–3, 1283. [DOI] [PubMed] [Google Scholar]
- 10.Hongcharu W, Taylor CR, Chang Y et al. Topical ALA-photodynamic therapy for the treatment of acne vulgaris. J INVEST DERMATOL 2000; 115: 183–92. [DOI] [PubMed] [Google Scholar]
- 11.Nybaek H, Jemec GBE. Photodynamic Therapy in the Treatment of Rosacea. DERMATOLOGY 2005; 211: 135–8. [DOI] [PubMed] [Google Scholar]
- 12.Katz B, Patel V. Photodynamic therapy for the treatment of erythema, papules, pustules, and severe flushing consistent with rosacea. J DRUGS DERMATOL 2006; 5: 6–8. [PubMed] [Google Scholar]
- 13.Bryld LE, Jemec GB. Photodynamic therapy in a series of rosacea patients. J Eur Acad Dermatol Venereol 2007; 21: 1199–202. [DOI] [PubMed] [Google Scholar]
- 14.Ma Y, Chen Q, Liu Y et al. Effects of 5-aminolevulinic acid photodynamic therapy on TLRs in acne lesions and keratinocytes co-cultured with P. acnes.hotodiagnosis Photodyn Ther 2016; 15: 172–81. [DOI] [PubMed] [Google Scholar]
- 15.Karrer S, Bosserhoff AK, Weiderer P, et al. Keratinocyte-derived cytokines after photodynamic therapy and their paracrine induction of matrix metalloproteinases in fibroblasts. Br J Dermatol 2004; 151: 776–83. [DOI] [PubMed] [Google Scholar]
- 16.Woo YR, Lim JH, Cho DH et al. Rosacea: Molecular Mechanisms and Management of a Chronic Cutaneous Inflammatory Condition. INT J MOL SCI 2016; 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilaberte Y, Frias MP, Rezusta A et al. Photodynamic therapy with methyl aminolevulinate for resistant scalp folliculitis secondary to Demodex infestation. J Eur Acad Dermatol Venereol 2009;23:718–719. [DOI] [PubMed] [Google Scholar]
- 18.Kim M, Jung HY, Park HJ. Topical PDT in the treatment of benign skin diseases: principles and new applications. INT J MOL SCI 2015; 16: 23259–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Friedmann DP, Goldman MP, Fabi SG et al. Multiple sequential light and laser sources to activate aminolevulinic acid for rosacea. J Cosmet Dermatol 2016; 15: 407–12. [DOI] [PubMed] [Google Scholar]