Abstract
Objective:
Success in diabetes research and self-management is often defined as a significant decrease in glycated hemoglobin (A1C). The aim of this article is to explore different types of successes experienced by adults with type-2 diabetes participating in a health technology and nurse coaching clinical trial.
Methods:
A qualitative analysis was conducted using surveys and documentation from motivational interview-based coaching sessions between study nurses and intervention participants.
Results:
Of the 132 cases reviewed, types of success predominantly fell into five categories: 1) change in health behaviors; 2) change in mindset or awareness; 3) change in engagement with healthcare resources; 4) change in physical or emotional health; and 5) change in health indicators.
Conclusion:
Experiences of success in diabetes are more varied than traditional A1C-based outcome models. Our findings suggest coaching and technology can assist patients to achieve a range of successes in diabetes management through goal setting, health tracking, resolving barriers, and aligning goals with factors that impact change.
Practice Implications:
While A1C reduction is a critical factor in decreasing risk of diabetes-related complications, when healthcare professionals focus on A1C as the main indicator of diabetes management success, important changes in individuals’ health and well-being may be overlooked or undervalued.
Keywords: diabetes mellitus, type-2, patient-centered care, qualitative research, motivational interviewing, patient outcome assessment, patient generated data
1. INTRODUCTION
Diabetes mellitus is among the most common and complex chronic conditions in the United States, affecting 12–14% of adults [1]. Improvement in diabetes care has traditionally been viewed through a disease-centered approach, with the degree of change in bio-physiological measures being used as the primary indicator of positive change and adherence with treatment [2, 3]. Specifically, glycated hemoglobin (A1C), which reflects an individual’s average glycemic control over several months [4], is the gold standard for measuring diabetes management in clinical practice and research. Lowering A1C is worthy of focus because improved A1C is associated with fewer serious diabetes-related health outcomes such as amputation, blindness and death [5–7].
Achieving the recommended A1C goal of 7.0% is difficult for many individuals with diabetes. From 2007–2010, only 52.5% of diabetic patients met this target, and less than 20% achieved recommended guidelines for A1C, blood pressure, and cholesterol combined [8, 9]. Unlike acute illnesses with time-limited and transparent treatment guidelines, complicated chronic conditions such as diabetes require daily self-management for a person to achieve control. Factors such as diet, activity, stress, medication adherence, and comorbid conditions can result in fluctuating A1C [10]. Social and environmental barriers such as job demands, financial stressors and caregiving responsibilities may also make it difficult for an individual to focus on the self-management required for optimal A1C control [11]. In the face of these challenges, significant A1C improvement may be out of reach for many people with diabetes until social, environmental and health-related barriers are addressed. Thus, A1C and other biophysiological measures alone may provide an incomplete view of an individual’s level of effort and success with diabetes management.
The focus on A1C as the predominant measure of success in diabetes can be contrasted with a more person-centered approach that encourages benchmarks of success connected to individual goals and circumstances [12]. Most factors important for achieving success in diabetes management are modifiable and require active participation in self-management behaviors, including healthy eating, regular physical activity, blood glucose monitoring, taking medications routinely, healthy coping strategies and problem-solving abilities [13]. Persons living with diabetes have cited improving diet, weight loss and achieving stable blood glucose levels as goals that are important and extend beyond clinical outcomes often prioritized by healthcare providers [14]. The person-centered approach for understanding success in diabetes self-management recognizes that developing skill in these behaviors can positively impact A1C [15–17]. However, there is limited research studying the range and variety of positive change individuals with diabetes may achieve, or how they perceive and talk about their success with diabetes self-management. In this paper, we use a person-centered approach for understanding and defining success in diabetes. Specifically, we examine types of successes experienced by adults with type-2 diabetes who participated in a randomized control trial involving a technology-enabled nurse coaching intervention.
2. METHODS
2.1. Overview of Project P2E2T2 Clinical Trial
This study focuses on participants who completed the Patient and Provider Engagement and Empowerment Through Technology (P2E2T2) Trial to Improve Health in Diabetes, funded by the Patient Centered Outcomes Research Institute (ClinicalTrials.org #NCT02672176) and approved by our University Institutional Review Board in 2015 [18]. The P2E2T2 trial enrolled English-speaking adults with type-2 diabetes from primary care clinics at a health system in Northern California between February-December 2016. Participants were randomized to one of two study arms: 1) usual care at the health system; or 2) the treatment arm, consisting of six nurse coaching sessions and use of personal health tracking technologies that included an online nutrition application (MyFitnessPal, Under Armor) and a fitness tracking watch (VivosmartHR, Garmin) with integration of their data into their electronic health record patient portal (MyChart, EPIC Hyperspaces). Total study participation time was nine months for both arms. Study outcomes, including self-efficacy, HgbA1C, and quality of life measures were measured at baseline, after the final coaching session, and at nine months.
2.2. Nurse Coaching and Health Technology Intervention
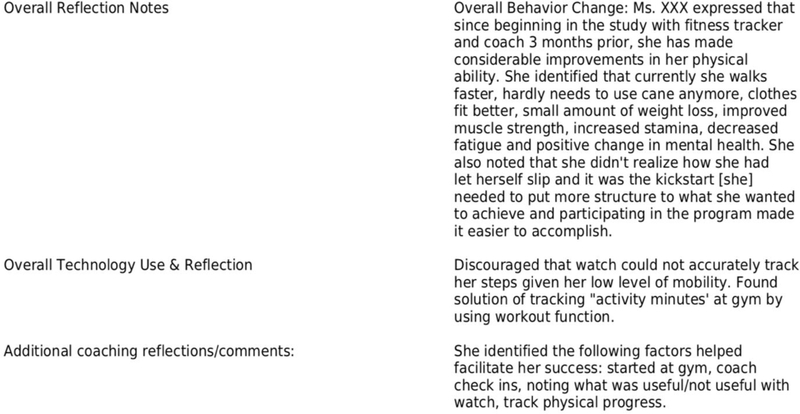
The nurse health coaching portion of the intervention used Motivational Interviewing —an approach that empowers individuals to identify personally salient areas for health change [19]. The coaches were all registered nurses who were certified in motivational interviewing prior to the start of the intervention. Participants in the intervention arm took part in six, one-on-one, biweekly telephone calls with study nurses, focused on eliciting participant motivations for health behavior change and encouraging participants to self-identify priority areas for health improvements. These areas for improvement often were centered on participant-generated activity, nutrition and sleep data, but nurse coaches also aided participants in self-identifying and prioritizing goals and barriers to overall self-care from any aspect of their life. After each session, the nurses documented their encounters in progress notes located in the research database [20]. Progress notes information regarding both the participant and nurse’s evaluation of the individual’s goal success and any barriers they reported encountering (see Figure 1). Participants also completed an online survey at the conclusion of the coaching intervention that asked about their progress and experience with the nurse coaching and technology intervention elements.
Figure 1.
Nurse Coaching Documentation Sample
2.3. Data Analysis
P2E2T2 trial participants randomized to the intervention arm who completed all six coaching sessions with the nurse health coach were eligible for this qualitative document review study. Two sets of data were examined. First, nurse progress notes were reviewed, with a focus on participant success and interventional factors that may have influenced success. The following fields of the nursing note were extracted for document analysis: motivations for behavior change; participant-identified goals and achievements; barriers and facilitators to change; and participant reflections from the final coaching session. Second, end-of-intervention survey responses were examined for participant-reported success at completion of the nurse coaching intervention. From the surveys, open-ended responses relating to program experiences and feedback regarding the coaching sessions were extracted. These documentation and survey items were selected for analysis because they captured goal progress and reflections through both nurse and participant reports. Extracted nursing notes and participant surveys were compiled and uploaded to Dedoose, a software program used to facilitate analysis [21].
Thematic analysis was conducted using an iterative process of deductive and emergent coding to examine the nursing notes and survey responses from each participant. Initially, two reviewers independently read and coded the extracted documentation and survey responses. Each participant case included approximately 3–4 pages of data to review. After 10 cases were coded, members of the research team met to discuss early codes and case memos. This process led to a refinement and clarification of codes and was followed by the review of another 25 participant charts and surveys using the new coding scheme. Data saturation was determined to have been reached by the coders after the review of 35 cases. The team then met again for initial theme development. To confirm and validate the themes, notes from the final participant-nurse coaching session and survey responses of the remaining 97 participants were analyzed. Descriptive statistics were used to characterize participant demographics.
3. RESULTS
3.1. Participant Characteristics
In total, 132 participants completed the nurse coaching portion of the intervention and were included in the document analysis. Participants had a mean age of 59.6 years and 60% percent selfidentified as White, 15% as African American, 16% as Hispanic, and 9% as Asian. Slightly more than half of the participants were male (52%). The group was well educated with 52% reporting attending at least some college and 42% indicating they attained a bachelors or graduate degree. Participants had been living with diabetes for a range of 0 to 35 years, with a median of 9 years. Only 28% of participants reported “good diabetes control” in the previous 6 months and the ability to walk for 15-minutes (63%). Table 1 provides additional details on participant characteristics.
Table 1.
Participant demographics and characteristics
| Characteristics | |
|---|---|
| Age, mean (SD) | 59.6 (11.2) |
| Gender, n (%) | |
| Male | 68 (52.3) |
| Female | 62 (47.7) |
| Ethnicity, n (%) | |
| Hispanic or Latino | 19 (16.2) |
| Non-Hispanic | 98 (83.8) |
| Race, n (%) | |
| White or Caucasian | 76 (59.4) |
| Black or African American | 19 14.8) |
| Asian | 11 (8.6) |
| Other | 22 (17.2) |
| Education, n (%) | |
| 8th Grade or High School | 9 (6.8) |
| Some College or Associates | 68 (51.5) |
| Bachelor or Graduate degree | 55 (41.7) |
| # of years living with diabetes, Median (IQR) | 9 (3,15.5) |
| Self- Reported Health Status, n (%) | |
| Excellent or very good | 26 (19.7) |
| Good | 59 (44.7) |
| Fair or poor | 47 (35.6) |
| Diabetes has been in ‘good control’ for more than 6 months, n (%) | 36 (27.5) |
| Able to go for at least a 15 min walk, n (%) | 84 (63.3) |
3.2. Types of Successes Experienced by Participants
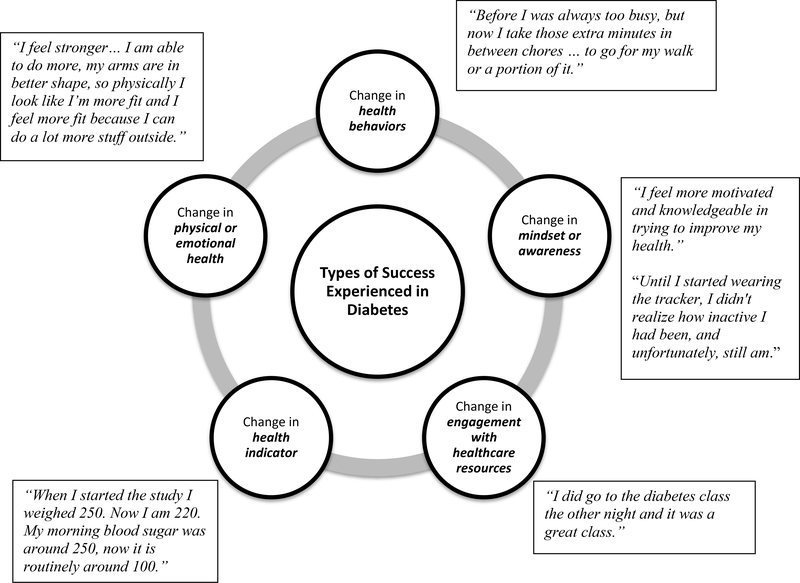
Of the 132 participants who completed the nurse health coaching intervention and used the personal health tracking technology, 96% reported some level of positive change in their health or ability to manage their diabetes. In only four cases, both the participants and the nurse coach noted minimal to no positive changes. Most participant goals focused on making improvements to their activity levels, diet, medications, and mental health, coinciding with the success types experienced. The types of success participants experienced fell predominantly into five interdependent categories: 1) change in health behaviors; 2) change in mindset or awareness; 3) change in engagement with healthcare resources; 4) change in physical or emotional health; and 5) change in health indicators (see Figure 2). Frequently, participants and nurse coaches reported participant success in more than one category.
Figure 2.
Types of Success Experienced in Diabetes
3.2.1. Change in Health Behaviors
One of the positive changes most frequently noted was change in health behaviors. Health behavior change manifested primarily in modifications participants made to their daily habits such as increasing activity or exercise, making dietary changes, improving medication adherence and sleep quality. Positive changes in nutrition commonly included reducing high carbohydrate or “problem” foods such as sugary drinks, or sticking to a daily calorie consumption goal. Examples of activity change included incorporating walks during work, or partnering with a family member or friend to go to the gym. As described by a female participant who altered her activity, “I used to sit at my desk for hours without getting up because I was busy. Now I understand the importance of moving and take 2 walks a day during work (usually about 1 mile each).” Making smaller behavior changes sometimes led to more significant change. For instance, another participant noted, “In addition to walking, I joined a gym and am working out 3 days a week!”
The health technology supported changes in behavior by streamlining ease of tracking and providing objective measures for counting activity, nutritional intake and sleep. As one participant told his nurse coach, the watch “kept him honest” and helped him stay on track. Participants also reported specific functionalities of the watch that were motivating, such as alerts that encouraged movement and those that reward participants reaching their goal. One participant noted “I was surprised at how it helped me get up and move when it told me to move.”
The nurse coaches used their clinical knowledge to assist participants in selecting goals and changing habits according to evidence-based guidelines. While the technology provided nutrition and activity recommendations based on participant height, weight, and age, the nurses helped participants adjust population-based targets to individual needs, disease specific recommendations, and functional status. This personalization maximized the applicability of the goal setting functions already built into the technology.
3.2.2. Change in Mindset or Awareness
Change in mindset or awareness was defined as an improved focus or prioritization on health. This category included participants who experienced a change in the way they perceived themselves, their habits, or interest in the importance of managing their health. Participants often reported that being in the study was the “push” they needed to refocus on their health. A female participant, who exemplified this type of change, reported in their survey, “I think the program was good and put me in a different mindset on trying to get exercise into my lifestyle at 65. It is a lifetime change for me, but I think I am moving in the right direction, but I am not there yet.” Changes in awareness helped many participants come to terms with adjustments in expectations and goals to fit age-related changes and fluctuations in health. The nurse coaches helped participants connect their motivations to goals that led to lifestyle changes they perceived as important. In some cases, this manifested through reflection and brainstorming about new strategies to achieve goals, when previously successful methods were no longer possible.
The health technology contributed to change in awareness by providing participants with quantified metrics for activity, calorie consumption, and sleep quality. Individuals were often unaware of how little activity they engaged in; the technology allowed them to reflect on changes they needed to make to improve their health based on these new insights. Being able to discuss self-management changes with the nurse coach helped participants see the value in the changes they were making and place their progress in context within their larger goals. In another example of a change in mindset or awareness, a male participant reflected upon the intervention in his survey, “It helped me to see what a change in diet could do for blood sugar levels. That a 30-minute walk was important to controlling both weight and blood sugar.” By experiencing a change in mindset, participants were able to understand how all their health habits were connected and important to managing their diabetes.
3.2.3. Change in Engagement with Healthcare Resources
A third category in which participants experienced success was a deepening engagement with healthcare resources, including providers and health education opportunities. Given the complexity of diabetes management and the need for multiple factors to come together for effective change, many participants identified issues unrelated to their diabetes as barriers to focusing on diabetes management such as alcohol abuse, mental health, finances, mobility, and stressful environments or relationships. In these situations, coaching sessions often focused on solving problems, identifying resources or making changes to their environment. As a result, many of the changes participants experienced involved (re)connecting with their healthcare team or obtaining counseling, case management, or targeted education.
In some cases, the increased engagement led to improved communication and connection between participants and providers. An example of this is described in a nursing note for a female participant:
In the past, she would cancel appointments or not take her medicine as prescribed. She notes that now she is taking her medicine regularly and has been checking in with her PCP regularly and the MSW through Care Coordination.
While connecting with health resources was not always directly related to diabetes management, the challenges participants faced took significant time and energy that often interfered with their ability to effectively manage diabetes. By addressing these challenges, participants were better positioned to focus on their diabetes management and make health changes.
3.2.4. Change in Physical or Emotional Health
Another category of change described was generally “feeling better,” either physically or emotionally. Participants reported feelings of accomplishment, self-control with dietary changes, and more energy after implementing their health goals. Participants also reported a sense of pride in their success and felt encouraged to continue focusing on their health. Participants highlighted improvements in mobility, stamina, clothing fit and physical strength that were often unrelated to diabetic markers such a blood glucose. A nursing progress note illustrates these physical and emotional changes participants described:
She has made considerable improvements in her physical ability. She identified that currently she walks faster, hardly needs to use her cane anymore, clothes fit better … improved muscle strength, increased stamina, decreased fatigue and positive change in mental health.
Another participant described a similar experience in the end-of-intervention survey:
[I feel] stronger. I went from a size 12 to a size 10 pants again and my core muscles are stronger, I’m able to do more, my arms are in better shape so physically I look like I’m more fit and I feel more fit because I can do a lot more stuff outside.
In both examples, participants achieved changes in their physical or emotional health. Participants also expressed the value they found in having someone listen to them as important to their emotional health. One participant described, “[The coach] helped me get out of a depression I was in for a long time…she listened and encouraged and gave me hope…she gave me tools for achieving goals.” The coaching sessions gave participants a chance to talk about the challenges and stressors they were facing, and helped keep them on track with their goals despite those challenges. The feedback from the technology and reflection time with the nurse coaches further reinforced feelings of accomplishment.
3.2.5. Change in Health Indicators
Lastly, participants looked to changes in traditional health indicators to measure success. A change in health indicators was defined as a positive, numeric shift in a clinical indicator related to diabetes self-management. Participants described improvements related to A1C lab results, weight loss, reduced insulin requirements, or an observed decrease in blood glucose values from self-monitoring. Those that experienced changes in health indicators often also reported success in one or more of the other categories and were motivated to continue with their goals. A male participant described, “After the coaching and encouragement and along with the tracking device, I’ve been able to lower my A1C, which has given me a lot of motivation to continue doing exercise.”
While achieving health indicator goals were viewed as a sign of success, mixed results were not uncommon. A female participant describes this experience, “My lab work, A1C, improved during the course of the study and I was more active, but I didn’t see much reduction in weight.” Results where one indicator improved but another stayed stagnant, could be related to physical factors such as stress, secondary illnesses or infections, or insufficient time passing for the effects of incremental changes to result in clinically meaningful numeric shifts. This discordance has the potential to cause confusion and lead to discouragement. As another participant noted, “If all of this [weight loss, improved fitness] is good, why did my A1C go up? It just baffles me. I guess that’s what’s frustrating.” In these situations, nurses were able to offer perspective on the complexity of diabetes management and help participants reconnect with the value of the many types of successes they had achieved.
4. DISCUSSION & CONCLUSION
4.1. Discussion
In this qualitative document analysis of nurse coaching encounter notes and participant openended survey responses, we found that the types of successes identified by adults with type-2 diabetes participating in a nurse coaching and health technology randomized controlled trial extended beyond bio-physical indicators traditionally used by researchers. Success was experienced in five categories related to changes in health behaviors, mindset or awareness, engagement with resources, physical or emotional health, and health indicators. Nearly all participants in the study experienced success in at least one of the five categories and many experienced successes in more than one category.
Incorporating a broader definition of success recognizes individuals’ experiences in making positive change in their ability to manage their diabetes. However, most clinical trials continue to use A1C as the primary measure of success in diabetes management [3, 22]. In a systematic review of 25 technology trials among adult diabetics, 88% of studies included A1C as an outcome, however, fewer than 16% of the trials reported outcomes such as self-efficacy or quality of life measures [22]. The primary outcome of the overall P2E2T2 study was self-efficacy, measured at baseline, after the final coaching session and at nine-months [18]. While full P2E2T2 trial outcome results will be disseminated in an upcoming manuscript, preliminary outcomes show that the intervention group had significantly improved self-efficacy scores at three months relative to the usual care group. The results of the primary outcome of the overall trial supports the qualitative findings presented in this paper; that participants experienced improvements in their diabetes management. However, self-efficacy scores were not significantly different between the two groups at nine months. We expect that some of the decline in self-efficacy gains made by the intervention group may be due to the cessation of coaching and that if long-term health changes are to be sustained, individuals may benefit from ongoing opportunity to connect with a coach.
The circumstances that impact success in diabetes are complicated, and often inter-related. The P2E2T2 intervention was incorporated into individuals’ lives over a 3–4-month period. During that time participants encountered numerous life stressors which impacted their ability to focus on diabetes selfmanagement. These barriers to self-management have also been reported in the literature. A review by Murray (2013) found barriers such as education, lack of family support, limited finances, and depression were factors that acted as deterrents for uptake and sustainability of behavior change [23]. Social functioning, capacity to access and use resources, health literacy, and self-efficacy also can influence an individual’s ability to meet their healthcare demands [24–26]. More expansive self-management successes should be acknowledged and encouraged, recognizing that some of these underlying issues may need to be resolved before a controlled A1C level can be obtained.
A major role of the nurse coach during the intervention was partnering with participants to identify their priorities, their goals for health improvement, and barriers to achieve their goals. While reduction in A1C is traditionally the primary goal set by healthcare providers for patients with diabetes, this intervention encouraged participants to self-identify health related goals that were most important to them and that they could track over time. The importance of supporting individuals in developing individualized self-management skills is well recognized [27, 28], along with the value of incremental goal setting to improve outcomes in diabetes [29, 30] and cardiovascular disease self-management [31]. Individuals are more likely to make changes if they create right-sized, manageable goals, and perceive challenges as possible to overcome. Nurses are well suited to fill a coaching role and support chronic disease management, as they merge clinical knowledge with a person-centered approach to health.
The health tracking technologies used in the study provided a wide range of opportunities for generating awareness, motivation, learning, and improved decision-making related to health. Many individuals are open to remote monitoring; in a recent weight loss trial, over 80% of participants identified the ability to track their data online and review data from a health coach as the most helpful intervention components [32]. In our study, the nurse coach had access to participant-generated data which could be used to provide objective feedback to the participant. Pairing patient-generated data with feedback from a healthcare professional has been identified as essential for interventions that incorporate technology to support diabetes health [22, 33]. As remote and personal health tracking technologies are increasingly ubiquitous and validated, the ability to integrate technology and patientgenerated data more fully into the existing healthcare workflow brings multiple opportunities to support individuals in achieving better health.
The strength of this study is the comprehensive review of nurse coaching notes and participant reflections for study participants with diabetes who received a technology-enabled person-centered intervention aimed at health improvement. The participant-nurse coaching data allowed us to analyze how individuals approached behavior change, worked through barriers, and provided insight into how participants viewed the results of their efforts. This study also has several limitations worth consideration. First, success was analyzed based on self-report and we have not correlated individual perceived success to success as defined within the larger trial results. Second, because the study is descriptive, we are unable to determine gradations of success. Third, a portion of the analysis was based on nursing documentation, which may introduce some bias, as the notes provide a summary of the coaching encounter and are somewhat subjective. Finally, as all participants received the combined technology-coaching intervention, it was not possible to determine which component had a greater impact on supporting health changes. However, the coaching notes and surveys suggest the impact of the components varied for different participants and may have changed over time.
4.2. Conclusion
Our results suggest participant experiences of success in diabetes are more robust than the traditional A1C-based model. This study highlights how health technology paired with nurse coaching, can assist patients to achieve a range of successes in diabetes management through goal setting, health tracking, and resolving barriers impacting change. It is important to note that of the five different types of success experienced by participants, four were not direct clinical outcomes. This finding demonstrates that individuals are experiencing important gains outside of conventional outcome measures.
4.3. Practice Implications
While A1C is an important indicator of risk for diabetes-related complications, when healthcare providers focus on A1C as the sole indicator of diabetes management success, important changes and incremental steps toward health improvement may be overlooked or undervalued. Patient successes should be recognized to support outcomes that matter to the individual. Nurse coaches can be a valuable addition to the care team to support individuals living with diabetes to actively engage in their self-management and make health improvements.
HIGHLIGHTS.
A person-centered approach measures success in diabetes control in relation to individual goals.
Broader definition of success includes making positive personal changes to manage diabetes.
Nurse coaching and technology support goal setting, health tracking and resolving barriers.
Success types: change in behavior, mindset, engagement, physical/emotional health, indicators
ACKNOWLEDGEMENTS
We would like to acknowledge Yajarayma Tang-Feldman, Daicy Luo, Bridget Levich, Deborah Greenwood, Nazifa Hamdard, Michael Dang and Sarah Haynes for their contributions to the nurse health coaching program and the overall clinical trial.
FUNDING
This work was supported by the Patient Centered Outcomes Research Institute [HIS-1310–07894] and by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
CONFLICT OF INTEREST
None.
“I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.”
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Menke A, Casagrande S, Geiss L, Cowie CC, Prevalence of and Trends in Diabetes Among Adults in the United States, 1988–2012, JAMA 314(10) (2015) 1021–9. [DOI] [PubMed] [Google Scholar]
- [2].Davies K, What is effective intervention?--using theories of health promotion, Br J Nurs 15(5) (2006) 252–6. [PubMed] [Google Scholar]
- [3].Gandhi GY, Murad MH, Fujiyoshi A, Mullan RJ, Flynn DN, Elamin MB, Swiglo BA, Isley WL, Guyatt GH, Montori VM, Patient-important outcomes in registered diabetes trials, Jama 299(21) (2008) 2543–9. [DOI] [PubMed] [Google Scholar]
- [4].American Diabetes Association, Standards of Medical Care in Diabetes-2015. Abridged for Primary Care Providers., Diabetes Care 38(Supplement 1) (2015) 97–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Pscherer S, Dippel FW, Lauterbach S, Kostev K, Amputation rate and risk factors in type 2 patients with diabetic foot syndrome under real-life conditions in Germany, Primary care diabetes 6(3) (2012) 241–6. [DOI] [PubMed] [Google Scholar]
- [6].Ray KK, Seshasai SR, Wijesuriya S, Sivakumaran R, Nethercott S, Preiss D, Erqou S, Sattar N, Effect of intensive control of glucose on cardiovascular outcomes and death in patients with diabetes mellitus: a meta-analysis of randomised controlled trials, Lancet 373(9677) (2009) 1765–72. [DOI] [PubMed] [Google Scholar]
- [7].Zhao W, Katzmarzyk PT, Horswell R, Wang Y, Johnson J, Heymsfield SB, Cefalu WT, Ryan DH, Hu G, HbA1c and lower-extremity amputation risk in low-income patients with diabetes, Diabetes care 36(11) (2013) 3591–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ali MK, Bullard KM, Gregg EW, Achievement of goals in U.S. Diabetes Care, 1999–2010, N Engl J Med 369(3) (2013) 287–8. [DOI] [PubMed] [Google Scholar]
- [9].Casagrande SS, Cowie CC, Fradkin JE, Utility of the US Preventive Services Task Force criteria for diabetes screening, Am J Prev Med 45(2) (2013) 167–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Walker RJ, Smalls BL, Egede LE, Social determinants of health in adults with type 2 diabetes--Contribution of mutable and immutable factors, Diabetes Res Clin Pract 110(2) (2015) 193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Nam S, Chesla C, Stotts NA, Kroon L, Janson SL, Barriers to diabetes management: patient and provider factors, Diabetes Res Clin Pract 93(1) (2011) 1–9. [DOI] [PubMed] [Google Scholar]
- [12].Spenceley SM, Williams BA, Self-care from the perspective of people living with diabetes, Can J Nurs Res 38(3) (2006) 124–45. [PubMed] [Google Scholar]
- [13].A.A.o.D. Educators, AADE guidelines for the practice of diabetes self-management education and training (DSME/T), The Diabetes Educator 35(3 suppl) (2009) 85S–107S. [Google Scholar]
- [14].Lopez JM, Katic BJ, Fitz-Randolph M, Jackson RA, Chow W, Mullins CD, Understanding preferences for type 2 diabetes mellitus self-management support through a patient-centered approach: a 2-phase mixed-methods study, BMC Endocrine Disorders 16(1) (2016) 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Greenwood D, Young H, Quinn C, Telehealth remote monitoring systematic review: structured self-monitoring of blood glucose and impact on A1C, Journal of diabetes science and technology 8(2) (2014) 378–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Thorpe CT, Fahey LE, Johnson H, Deshpande M, Thorpe JM, Fisher EB, Facilitating healthy coping in patients with diabetes: a systematic review, Diabetes Educ 39(1) (2013) 33–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Thomas DE, Elliott EJ, Naughton GA, Exercise for type 2 diabetes mellitus, Cochrane Database Syst Rev (3) (2006) Cd002968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Miyamoto S, Dharmar M, Fazio S, Tang-Feldman Y, Young HM, mHealth Technology and Nurse Health Coaching to Improve Health in Diabetes: Protocol for a Randomized Controlled Trial, JMIR research protocols 7(2) (2018) e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Miller WR, Rose GS, Toward a theory of motivational interviewing, American Psychologist 64(6) (2009) 527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support, Journal of biomedical informatics 42(2) (2009) 377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Dedoose, Web application for managing, analyzing, and presenting qualitative and mixed method research data Los Angeles, CA: SocioCultural Research Consultants, LLC; Version 7.0.23 (2016). [Google Scholar]
- [22].Greenwood D, Gee P, Fatkin K, Peeples M, A Systematic Review of Reviews Evaluating Technology-Enabled Diabetes Self-Management Education and Support, Journal of Diabetes Science and Technology 0(0) (2017) 1932296817713506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Murray J, Fenton G, Honey S, Bara AC, Hill KM, House A, A qualitative synthesis of factors influencing maintenance of lifestyle behaviour change in individuals with high cardiovascular risk, BMC Cardiovascular Disorders 13(1) (2013) 48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Boehmer KR, Barakat S, Ahn S, Prokop LJ, Erwin PJ, Murad MH, Health coaching interventions for persons with chronic conditions: a systematic review and meta-analysis protocol, Systematic Reviews 5(1) (2016) 146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Stead M, Craigie AM, Macleod M, McKell J, Caswell S, Steele RJ, Anderson AS, Why are some people more successful at lifestyle change than others? Factors associated with successful weight loss in the BeWEL randomised controlled trial of adults at risk of colorectal cancer, International journal of behavioral nutrition and physical activity 12(1) (2015) 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Wilkinson A, Whitehead L, Ritchie L, Factors influencing the ability to self-manage diabetes for adults living with type 1 or 2 diabetes, Int J Nurs Stud 51(1) (2014) 111–22. [DOI] [PubMed] [Google Scholar]
- [27].Moser A, van der Bruggen H, Spreeuwenberg C, Widdershoven G, Autonomy through identification: a qualitative study of the process of identification used by people with type 2 diabetes, J Clin Nurs 17(7B) (2008) 209–16. [DOI] [PubMed] [Google Scholar]
- [28].Mulder BC, Lokhorst AM, Rutten GE, van Woerkum CM, Effective Nurse Communication With Type 2 Diabetes Patients: A Review, West J Nurs Res 37(8) (2015) 1100–31. [DOI] [PubMed] [Google Scholar]
- [29].Young H, Miyamoto S, Ward D, Dharmar M, Tang-Feldman Y, Berglund L, Sustained effects of a nurse coaching intervention via telehealth to improve health behavior change in diabetes, Telemedicine and e-Health 20(9) (2014) 828–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].DeWalt DA, Davis TC, Wallace AS, Seligman HK, Bryant-Shilliday B, Arnold CL, Freburger J, Schillinger D, Goal setting in diabetes self-management: taking the baby steps to success, Patient Educ Couns 77(2) (2009) 218–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Handley M, MacGregor K, Schillinger D, Sharifi C, Wong S, Bodenheimer T, Using action plans to help primary care patients adopt healthy behaviors: a descriptive study, J Am Board Fam Med 19(3) (2006) 224–31. [DOI] [PubMed] [Google Scholar]
- [32].Dalcin AT, Jerome GJ, Fitzpatrick SL, Louis TA, Wang NY, Bennett WL, Durkin N, Clark JM, Daumit GL, Appel LJ, Coughlin JW, Perceived helpfulness of the individual components of a behavioural weight loss program: results from the Hopkins POWER Trial, Obes Sci Pract 1(1) (2015) 23–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Miyamoto SW, Henderson S, Young HM, Pande A, Han JJ, Tracking Health Data Is Not Enough: A Qualitative Exploration of the Role of Healthcare Partnerships and mHealth Technology to Promote Physical Activity and to Sustain Behavior Change, JMIR mHealth and uHealth 4(1) (2016) e5. [DOI] [PMC free article] [PubMed] [Google Scholar]