CAPSULE SUMMARY
Exclusive breastfeeding during the first month of life and vaginal delivery may mitigate the transmission of atopy from mother to child. These results could have implications for potential targeted prevention strategies in high-risk offspring of atopic mothers.
Keywords: Breastfeeding, Mode of delivery, Maternal atopy, Childhood atopy, Specific immunoglobulin E, Food sensitization, Food allergy, Inhalant sensitization, Atopic dermatitis, Cesarean section
To the Editor:
A family history of allergy, especially maternal allergy, is associated with an increased likelihood of allergic sensitization and allergic diseases during childhood. 1, 2 Furthermore, infancy and early childhood may be a critical period for environmental exposures to modulate allergic disease risk. While breastfeeding and delivery mode appear to modify risk of childhood allergic outcomes,3–5 it is unclear if they have the potential to attenuate or intensify the risk associated with vertical transmission of maternal atopy. In the Detroit area WHEALS (Wayne County Health, Environment, Allergy, and Asthma Longitudinal Study) birth cohort, we investigated whether the association between maternal atopy and childhood eczema and atopy depends upon mode of delivery or breastfeeding.
Analyses were performed on data collected from protocols approved by the Henry Ford Health System Institutional Review Board. The WHEALS cohort included 1258 babies; 255 were dropped for reasons such as refusals and noncompliance. Of the remaining 1003 eligible, 673 were included in the analytic sample, as maternal atopy status was ascertained as described below and the child completed the 2-year clinic visit. Participants included in the analysis were more likely to be married, white, and breastfeed their children, among others (see Table E1 in the Online Repository). The women were interviewed during their pregnancy to obtain demographic and environmental information. Postpartum questionnaires and home visits were targeted for ages 1 and 6 months. At the 1-month interview, women were asked about breastfeeding practices to determine whether they were exclusively breastfeeding (report of current breastfeeding and no formula). Delivery records were abstracted to obtain delivery type (vaginal or C-section), as well as antimicrobial or antifungal use during pregnancy. Maternal atopy during pregnancy was defined as a serum IgE level of 0.35 IU/mL or greater for at least 1 of 8 common allergens, including dust mite, ragweed, Alternaria alternata, dog, cat, grass, cockroach, and egg. In cases where a prenatal maternal serum sample was missing, a 1-month postnatal sample was substituted, as we have previously shown that sensitization status is relatively stable from the prenatal to the early postnatal period.6 A clinic visit and interview was performed at 2-4 years of age (mean age 2.2) by Henry Ford Medical Group physicians and staff who were instructed in the study protocol. Physicians determined past or present eczema considering combined patient history and physical examination. Children’s serum total and specific IgE was determined by ImmunoCAP and atopy was defined as a serum IgE level of 0.35 IU/mL or greater for at least 1 of 10 common allergens (dust mite, ragweed, Alternaria alternata, dog, cat, grass, cockroach, egg, milk and peanut). The association between maternal atopy and childhood outcomes was assessed using logistic regression (p<0.05 considered significant), with effect modification by mode of delivery and breastfeeding evaluated (p<0.10 considered significant).
Among the 673 children, 384 (57%) had atopic mothers (Table 1). Atopic mothers were more likely to be African American (p < 0.001) and have used antifungals during pregnancy (p = 0.008). Atopic mothers also received more antibiotics during pregnancy, but this trend did not reach statistical significance (p = 0.056).
Table 1:
Description of maternal, birth, and early life characteristics and associations with maternal atopy
| Covariate | Response | Overall (N=673) N (%) | By Maternal Atopy Status N (%) | p-value* | |
|---|---|---|---|---|---|
| Non-atopic (N=289) | Atopic (N=384) | ||||
| Maternal marital status | Not married | 218 (32.4) | 88 (30.4) | 130 (33.9) | 0.35 |
| Married | 455 (67.6) | 201 (69.6) | 254 (66.1) | ||
| Household income | <$20K | 76 (11.3) | 36 (12.5) | 40 (10.4) | 0.075 |
| 20K-<$40K | 140 (20.8) | 67 (23.2) | 73 (19) | ||
| 40K-<$80K | 179 (26.6) | 83 (28.7) | 96 (25) | ||
| $80K-<$100K | 92 (13.7) | 41 (14.2) | 51 (13.3) | ||
| ≥$100K | 97 (14.4) | 33 (11.4) | 64 (16.7) | ||
| Refused to answer | 89 (13.2) | 29 (10) | 60 (15.6) | ||
| Maternal education | <HS diploma | 28 (4.2) | 10 (3.5) | 18 (4.7) | 0.84 |
| HS diploma/equivalent | 100 (14.9) | 45 (15.6) | 55 (14.3) | ||
| Some college | 304 (45.2) | 132 (45.7) | 172 (44.8) | ||
| ≥Bachelor’s degree | 241 (35.8) | 102 (35.3) | 139 (36.2) | ||
| Maternal race | White | 176 (26.2) | 87 (30.1) | 89 (23.2) | <0.001 |
| African American | 386 (57.4) | 142 (49.1) | 244 (63.5) | ||
| Mixed/Other | 111 (16.5) | 60 (20.8) | 51 (13.3) | ||
| Prenatal antibiotic use† | No | 293 (45.4) | 139 (49.6) | 154 (42.1) | 0.056 |
| Yes | 353 (54.6) | 141 (50.4) | 212 (57.9) | ||
| Prenatal antifungal use† | No | 526 (81.4) | 241 (86.1) | 285 (77.9) | 0.008 |
| Yes | 120 (18.6) | 39 (13.9) | 81 (22.1) | ||
| Indoor pets at pre-delivery | No | 417 (62.0) | 185 (64) | 232 (60.4) | 0.34 |
| Yes | 256 (38.0) | 104 (36) | 152 (39.6) | ||
| Mode of delivery of offspring† | Vaginal | 425 (63.2) | 176 (61.1) | 249 (64.8) | 0.32 |
| C-Section | 247 (36.8) | 112 (38.9) | 135 (35.2) | ||
| Current breastfeeding at 1 month† | No | 278 (42.8) | 125 (45.3) | 153 (40.9) | 0.26 |
| Yes | 372 (57.2) | 151 (54.7) | 221 (59.1) | ||
| Exclusive breastfeeding at 1 month† | No | 542 (83.4) | 229 (83) | 313 (83.7) | 0.81 |
| Yes | 108 (16.6) | 47 (17) | 61 (16.3) | ||
C-section, Cesarean section
HS, high school
Calculated by the chi-square test.
Some missing values in covariate: all rates of missingness < 5%.
After covariate adjustment, the odds of eczema by age 2 did not significantly differ between children of atopic and non-atopic mothers (odds ratio [OR] comparing children of atopic versus non-atopic mothers = 1.15, 95% confidence interval [CI]=[0.75, 1.77], p = 0.51, see Table E2 in the Online Repository). However, children of atopic mothers had approximately double the odds of being atopic (OR = 2.35 [1.56, 3.53], p < 0.001), sensitized to foods (OR = 2.2 [1.46, 3.31], p < 0.001), and sensitized to inhalants (OR = 2.04 [1.29, 3.24], p = 0.002). Because women who delivered via C-section were less likely to exclusively breastfeed their child at 1 -month of age (11.3% vs. 19.7%, p=0.006), we assessed the effect of maternal atopy on child outcomes within each of four subgroups: vaginal/non-exclusively breastfed (VN), vaginal/exclusively breastfed (VB), C-section/non-exclusively breastfed (CN), and C-section/exclusively breastfed (CB) (Fig 1). The association between maternal atopy and childhood eczema was not significantly modified by mode of delivery nor exclusive breastfeeding (both interaction p≥0.10; Fig 1, A). However, exclusive breastfeeding significantly modified the association between maternal atopy and child atopy (interaction p=0.013; Fig 1, B). Specifically, regardless of mode of delivery, maternal atopy was only associated with higher odds of child atopy if they were not exclusively breastfed at 1-month of age (OR [95% CI]VN=2.34 [1.33, 4.12]; ORVB=0.60 [0.23, 1.59]; ORCN=4.61 [2.20, 9.67]; ORCB=1.18 [0.36, 3.87]). Similar results were observed for the association between maternal atopy and child inhalant sensitivity (breastfeeding interaction p=0.012; C-section interaction p=0.49; Fig 1, D). Further, both exclusive breastfeeding and mode of delivery jointly modified the association between maternal atopy and child food sensitivity (interaction p=0.053, 0.042, respectively; Fig 1, C), where both exclusive breastfeeding and vaginal delivery appeared to mitigate the association between maternal atopy and child food sensitivity. Specifically, maternal atopy was highly associated with child food sensitivity among children who were born via C-section and were non-exclusively breastfed (ORCN=4.64 [2.22, 9.72]), whereas, there was no association among children who were vaginally delivered and were exclusively breastfed (ORVB=0.65 [0.25, 1.70]).
Fig 1.
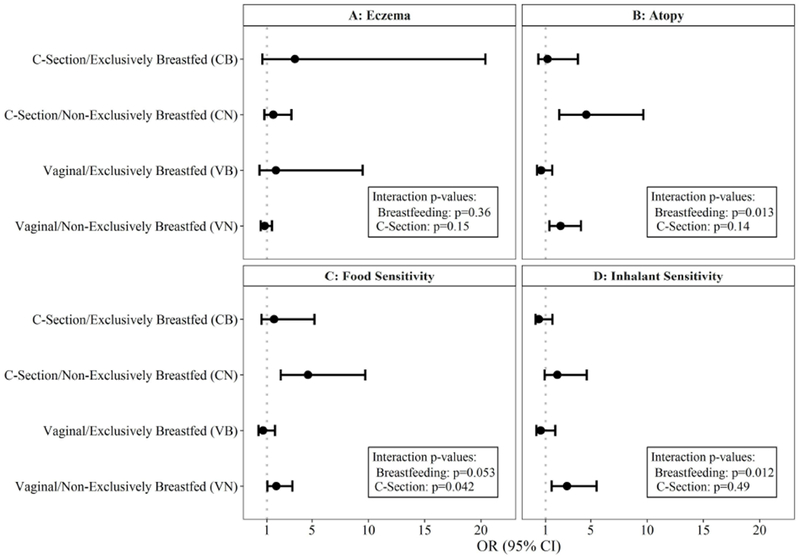
Association between maternal atopy and childhood allergic outcomes, by mode of delivery and exclusive breastfeeding at 1-month. Presented odds ratios (ORs) and 95% confidence intervals (CIs) compare the odds of each outcome in children of atopic versus non-atopic mothers, within each of the four subgroups. Outcomes examined include eczema (adjusted for maternal race, A), atopy (adjusted for maternal race, B), food sensitivity (adjusted for maternal race, C), and inhalant sensitivity (adjusted for prenatal antibiotic use, D).
While interpreting our results, we acknowledge certain limitations. We were able to obtain adequate information on maternal but not paternal atopy. Data were only available on a subset of the full cohort: this not only limits power to examine effect modification, but also generalizability, as there was evidence of selection bias.
Our analyses suggest vaginal delivery and exclusive breastfeeding in combination significantly modify the association between maternal atopy and atopic outcomes and suggest that the excess risk of allergy in offspring due to maternal atopy depends upon these exposures. We found that maternal atopy is primarily a risk factor among children born via C-section and in non-exclusively breastfed children, with early breastfeeding and vaginal delivery mitigating the transmission of atopy from mother to child. The biological mechanism explaining the effects of breastfeeding and delivery mode on allergy development is unknown. As we have previously shown in this cohort that these factors associate with an altered early life gut microbiota,7 we speculate that this pathway may play a role in early-life immune development. Studies have also directly linked C-section delivery to altered stress response, immune function, and epigenetic changes in offspring.8 Additionally, human milk contains a variety of immunoactive components (e.g., oligosaccharides, metabolites, microbes) as well as vitamins and nutrients that may provide protection.9 These results may be informative in regard to potential targeted prevention strategies in high-risk offspring of atopic mothers, though further studies will be necessary to determine the biological mechanisms behind these protective effects.
Supplementary Material
Acknowledgments
Funding:
Supported by the National Institutes of Health (P01 AI089473; R01AI051598) and the Fund for Henry Ford Hospital
ABBREVIATIONS
- WHEALS
Wayne County Health, Environment, Allergy, and Asthma Longitudinal Study
- C-section
Cesarean section
- HS
high school
- IgE
immunoglobulin E
- IU
international unit
- mL
milliliter
- VN
vaginally born/non-exclusively breastfed
- VB
vaginally born/exclusively breastfed
- CN
C-section born/non-exclusively breastfed
- CB
C-section born/exclusively breastfed
- OR
odds ratio
- CI
confidence interval
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest:
None
REFERENCES
- 1.Bertelsen R, Rava M, Carsin A, Accordini S, Benediktsdottir B, Dratva J, et al. Clinical markers of asthma and IgE assessed in parents before conception predict asthma and hayfever in the offspring. Clinical & Experimental Allergy 2017; 47:627–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xu R, DeMauro SB, Feng R. The impact of parental history on children’s risk of asthma: a study based on the National Health and Nutrition Examination Survey-III. Journal of asthma and allergy 2015; 8:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nwaru B, Craig L, Allan K, Prabhu N, Turner S, McNeill G, et al. Breastfeeding and introduction of complementary foods during infancy in relation to the risk of asthma and atopic diseases up to 10 years. Clinical & Experimental Allergy 2013; 43:1263–73. [DOI] [PubMed] [Google Scholar]
- 4.Bager P, Wohlfahrt J, Westergaard T. Caesarean delivery and risk of atopy and allergic disesase: meta-analyses. Clinical & Experimental Allergy 2008; 38:634–42. [DOI] [PubMed] [Google Scholar]
- 5.van Nimwegen FA, Penders J, Stobberingh EE, Postma DS, Koppelman GH, Kerkhof M, et al. Mode and place of delivery, gastrointestinal microbiota, and their influence on asthma and atopy. Journal of Allergy and Clinical Immunology 2011; 128:948–55. e3. [DOI] [PubMed] [Google Scholar]
- 6.Perry LM, Ownby DR, Wegienka GR, Peterson EL, Woodcroft KJ, Joseph CL, et al. Differences in total and allergen specific IgE during pregnancy compared with 1 month and 1 year post partum. Annals of Allergy, Asthma & Immunology 2009; 103:342–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levin AM, Sitarik AR, Havstad SL, Fujimura KE, Wegienka G, Cassidy-Bushrow AE, et al. Joint effects of pregnancy, sociocultural, and environmental factors on early life gut microbiome structure and diversity. Scientific Reports 2016; 6:31775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Magne F, Puchi Silva A, Carvajal B, Gotteland M. The elevated rate of Cesarean section and its contribution to non-communicable chronic diseases in Latin America: the growing involvement of the microbiota. Frontiers in pediatrics 2017; 5:192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Munblit D, Peroni DG, Boix-Amorós A, Hsu PS, Land BVt, Gay MC, et al. Human milk and allergic diseases: an unsolved puzzle. Nutrients 2017; 9:894. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


