Abstract
Objectives
The role of arthroscopic debridement in the painful degenerative knee is controversial. Studies have shown that arthroscopic surgery for knee osteoarthritis provides no additional benefit to optimized physical and medical therapy. There are however, limited studies on the management of the subgroup of significantly symptomatic patients who remain refractory to maximal conservative treatment and are poor candidates for knee replacement surgery.
We propose that with careful patient selection, arthroscopic debridement can provide good symptomatic relief with sustained benefits in the degenerative knee.
Methods
We performed a retrospective, single-surgeon study of 180 consecutive knee arthroscopies performed in 169 patients, aged 40 years and above, who had mechanical symptoms affecting their daily lives and underwent arthroscopic debridement after failure of a minimum 2 months of optimized medical and physical therapy. Severity of the knee osteoarthritis on plain radiographs was assessed using the Kellgren-Lawrence classification.
Functional and satisfaction scores were assessed using Oxford Knee Score, Koos Knee Survey, Short Form-36, Numeric Pain Rating Scale, and questions adapted from the North American Spine Society Questionnaire.
Results
Excellent functional outcomes and patient satisfaction were reported in the majority of patients over the follow-up timeframe of 2–8 years. The mean pre-operative Kellgren-Lawrence score was 2.02 (SD 0.580). Significant improvements compared to pre-operative scores were seen across all scoring systems tested. 90% of patients reported good to excellent results.
Conclusion
Arthroscopic knee debridement can provide good symptomatic relief and sustained benefits in significantly symptomatic patients with early degenerative knees who have failed conservative management. This is most useful in patients with mechanical symptoms secondary to degenerative meniscal tears or chondral flaps, and those with symptomatic patellofemoral osteoarthritis.
Keywords: Arthroscopic debridement, Symptomatic knee osteoarthritis, Mechanical symptoms, Degenerative meniscal tears, Refractory to conservative management
Introduction
The role of arthroscopic debridement in the painful degenerative knee is controversial. In a systematic review and meta-analysis of the benefits and harms of arthroscopic surgery involving partial meniscectomy, debridement or both for middle or older patients with knee pain and degenerative knee disease by Thorlund et al., in 2015, it is suggested that the benefits are limited, absent after two years and associated with harm.1
Supported by landmark articles by Mousley et al. and Kirkley et al. where they found no difference in outcomes in Mousley ‘s single blinded randomized controlled trial in 2002 comparing arthroscopic surgery versus sham surgery and again no difference in outcomes in Kirkley's randomized controlled trial in 2008 comparing arthroscopic surgery versus optimized medical and physical therapy, it may seem that the role of arthroscopic surgery in the degenerative knee is no longer justified.2,3
Interestingly, many specialists still remain convinced of the benefits of the procedure from their experience with several recent reports showing an increase in the incidence of arthroscopic knee surgery with meniscal resection in the past decade.4, 5, 6, 7, 8, 9, 10, 11
In a randomized controlled trial by Katz et al., in 2013 comparing arthroscopic surgery versus physical therapy for symptomatic patients with meniscal tears and knee osteoarthritis, no significant difference in the frequency of adverse events was found between the groups.12 Importantly, 30.2% of patients who were assigned to physical therapy did not have significant improvement in their functional status and underwent surgery within 6 months.12 A further 4.7% of patients did so between 6 and 12 months.12 The mean age of the patients in the physical therapy group was 57.8 years.12
In recent years, there is increasing recognition of the impact of osteoarthritis on younger patients who are still within the workforce with several studies showing significant decrease in productivity in those employed.13, 14, 15 This loss in productivity stems not only from the absence from work, but also from the indirect costs resulting primarily from work impairment due to osteoarthritis pain while at work.16 Unfortunately, there are limited studies on the management of the subgroup of significantly symptomatic patients who remain refractory to maximal conservative treatment and are poor candidates for knee replacement surgery, most of whom belong to the employed population where there is pressure to return to work.
We propose that with careful patient selection, arthroscopic debridement can provide good symptomatic relief with sustained benefits in the degenerative knee in this subgroup of patients.
Materials and methods
We performed a retrospective, single-surgeon study of 180 consecutive knee arthroscopies performed between 2009 and 2013 in 169 patients, aged 40 years and above, who had symptoms affecting their daily lives and underwent arthroscopic debridement after failure of a minimum 2 months of optimized medical and physical therapy.
Patient selection was key in our study. The offer of arthroscopic debridement was made only to those with mechanical symptoms such as locking and pain secondary to degenerative meniscal tears, unstable chondral flaps or loose bodies, and to those with symptomatic patellofemoral osteoarthritis, after they have failed conservative therapy, if their plain knee radiographs do not demonstrate evidence of end-stage osteoarthritic changes. Patients with intra-operative findings of crystal arthropathy were excluded from the study. The minimum follow-up timeframe was 2 years (range 2–8 years). Severity of the knee osteoarthritis on plan radiographs was assessed using the Kellgren-Lawrence classification.
Functional and satisfaction scores were assessed using Oxford Knee Score (OKS), KOOS Knee Survey (KKS), Short Form-36 (SF-36), Numeric Pain Rating Scale (NPRS) and questions adapted from the North American Spine Society (NASS) questionnaire. The two questions adapted from the North American Spine Society (NASS) questionnaire were: 1) Assessment of overall results of your treatment for knee pain, and 2) Has the treatment for your knee condition met your expectation so far?
This study was approved by the hospital’s ethics committee. Informed consent was obtained from all patients involved in the study.
Statistical analysis
The data was compiled and analyzed using SPSS version 21 (SPSS Inc., Chicago, Illinois, USA). Continuous data was expressed as mean values and standard deviations. Analysis of data was made using paired t-test for all subjective outcomes. A significant result was taken as p < 0.05.
Results
Of the 169 patients recruited (95 males, 74 females), 10 patients had bilateral knee arthroscopies and 1 patient had repeat knee arthroscopies on the ipsilateral side within the study time frame between 2009 and 2013.1 had an earlier knee arthroscopy on the ipsilateral knee within the study timeframe when she was 37 years old. There were no prior knee arthroscopies performed on the ipsilateral side in any of the patients before the study timeframe. 3 patients had repeat arthroscopies performed on the ipsilateral side after the study timeframe.
The mean patient age at the time of surgery was 54.1 years (range 40–81 years). The majority of patients were young with 75.6% of patients aged between 40 and 59 and 93.3% of patients aged between 40 and 69.
Fig. 1 shows a breakdown of the patients recruited. Data was collected from 116 patients (125 of the 180 arthroscopies performed). 13 patients underwent subsequent total knee replacement (TKR) at a mean of 36.7 months post arthroscopic debridement (range 5.7–76.6 months).
Fig. 1.
Breakdown of patients recruited.
40 patients were lost to follow-up (42 of the 180 arthroscopies performed). 1 of these patients had bilateral knee arthroscopies and 1 had a repeat knee arthroscopy on the ipsilateral side. There were 3 patients that died (1 died of metastatic colon cancer, 1 died of pneumonia on the background of metastatic lung cancer and 1 died secondary to a road traffic accident). 1 patient was unable to be assessed as he sustained a traumatic cervical spine injury with paraplegia secondary to a road traffic accident. 33 patients were uncontactable, of which 24 were foreign workers on work permits that returned to their home country after completion of their employment contract. 3 patients declined participation in the study.
There were no associated adverse events reported post-operatively. This includes deep and superficial infections, deep vein thrombosis, pulmonary embolism, cardiovascular events and death.
Table 1 shows a comparison of the pre-op versus post-op scores in the general cohort of patients able to be followed up. There were significant improvements across all scoring systems tested (p < 0.001). Oxford Knee Score improved from 29.03 pre-operatively to 43.24 post-operatively. Similar improvements were seen consistently across all parameters for both KOOS Knee Survey and SF-36 subsections. This was again reflected in the improvement of the NPRS score from 7.08 pre-operatively to 1.66 post-operatively.
Table 1.
Outcome scores of general cohort able to be followed up.
| Pre-op (SD) | Post-op (SD) | p-value | |
|---|---|---|---|
| Oxford Knee Score |
29.03 (8.75) |
43.24 (5.01) |
<0.001 |
| KOOS - Pain | 60.07 (18.84) | 90.36 (12.04) | <0.001 |
| KOOS - Other symptoms | 63.43 (18.42) | 89.94 (10.69) | <0.001 |
| KOOS - Function in daily living | 66.56 (16.78) | 92.80 (9.33) | <0.001 |
| KOOS - Function in sports | 35.60 (18.57) | 75.72 (23.38) | <0.001 |
| KOOS - Knee related QOL |
45.25 (18.04) |
79.60 (19.18) |
<0.001 |
| SF36 - Physical functioning | 41.68 (23.04) | 79.12 (21.31) | <0.001 |
| SF36 - Role limitations physical health | 26.80 (36.09) | 81.40 (35.77) | <0.001 |
| SF36 - Role limitations due to emotional problems | 59.20 (44.37) | 85.60 (33.42) | <0.001 |
| SF36 - Energy/Fatigue | 59.12 (13.86) | 71.36 (14.49) | <0.001 |
| SF36 -Emotional well-being | 68.86 (12.28) | 76.06 (12.86) | <0.001 |
| SF36 - Social functioning | 62.90 (21.12) | 87.70 (15.71) | <0.001 |
| SF36 - Pain | 56.20 (21.36) | 86.58 (16.23) | <0.001 |
| SF36 - General health |
59.24 (17.24) |
72.96 (16.02) |
<0.001 |
| NPRS score | 7.08 (1.20) | 1.66 (2.16) | <0.001 |
SD: Standard deviation.
SF36: Short Form-36.
NPRS: Numeric Pain Rating Scale.
Poor pre-operative scores were seen specific for pain, consistent through the KOOS Knee Survey, SF-36 and NPRS score (Table 1). Of note, in addition to these poor pain scores, there was significant compromise seen in the subsections pertaining to function and quality of life seen in both KOOS Knee Survey and SF-36. The ‘Knee related quality of life’ and ‘Function in sports’ subsections scored the two lowest scores in the KOOS Knee Survey while ‘Physical functioning’ and ‘Role limitations in physical health’ subsections scored the lowest scores in the SF-36. These were significantly poorer than the pain scores in their respective scoring systems.
With the adapted questions from the NASS questionnaire, 90% of arthroscopies were rated ‘Good to Excellent’, 10% were rated ‘Fair’ and 0% were rated ‘Poor to Terrible’ in the assessment of the overall results of the knee arthroscopies performed. The arthroscopies met expectations in 96% of the arthroscopies performed.
A subgroup analysis of the patients who were unsatisfied (14 out of 125 arthroscopies) was performed and compared against the general cohort.
Table 2 shows a comparison of the pre-op versus post-op scores in the unsatisfied group of patients. Interestingly, despite being unsatisfied, improvements were seen across all scoring systems tested. Significant improvements were seen in the Oxford Knee Score, KOOS Knee Survey, NPRS and SF-36 subsections for ‘Physical Functioning’, ‘Role limitations physical health’, ‘Social Functioning’ and ‘Pain’. Improvements were also seen in SF-36 subsections for ‘Role limitations due to emotional problems’, ‘Energy/fatigue’, ‘Emotional well-being’ and ‘General Health’ although these did not reach statistical significance.
Table 2.
Outcome scores of unsatisfied group of patients.
| Pre-op (SD) | Post-op (SD) | p-value | |
|---|---|---|---|
| Oxford Knee Score |
24.07 (8.64) |
37.57 (7.59) |
<0.001 |
| KOOS - Pain | 57.74 (19.34) | 84.33 (15.32) | <0.001 |
| KOOS - Other symptoms | 51.28 (18.72) | 84.18 (15.20) | <0.001 |
| KOOS - Function in daily living | 62.50 (16.88) | 87.92 (12.16) | <0.001 |
| KOOS - Function in sports | 30.36 (21.88) | 64.64 (37.18) | <0.001 |
| KOOS - Knee related QOL |
42.86 (21.07) |
66.07 (23.86) |
<0.001 |
| SF36 - Physical functioning | 25.36 (12.63) | 62.14 (30.17) | <0.001 |
| SF36 - Role limitations physical health | 14.29 (21.29) | 64.29 (42.42) | <0.001 |
| SF36 - Role limitations due to emotional problems | 59.52 (45.63) | 76.19 (40.15) | 0.110 |
| SF36 - Energy/Fatigue | 57.14 (11.88) | 61.43 (14.20) | 0.445 |
| SF36 -Emotional well-being | 64.00 (10.29) | 70.86 (12.88) | 0.130 |
| SF36 - Social functioning | 59.82 (19.72) | 81.25 (20.66) | 0.011 |
| SF36 - Pain | 49.29 (13.39) | 74.82 (19.00) | 0.002 |
| SF36 - General health |
55.00 (12.86) |
66.07 (14.17) |
0.059 |
| NPRS score | 7.71 (1.27) | 4.07 (2.76) | <0.001 |
SD: Standard deviation.
SF36: Short Form-36.
NPRS: Numeric Pain Rating Scale.
The pre-op scores were similar in both the general cohort and the unsatisfied group except for KOOS Knee Survey ‘Other symptoms’ subsection which looks at swelling, restricted range of motion and mechanical symptoms, and SF-36 ‘Physical functioning’ subsection where poorer scores were seen in the unsatisfied group (Table 3).
Table 3.
Comparison of general cohort versus the unsatisfied group in terms of (i) preop scores and (ii) change in outcome scores between pre-op and post-op.
| General cohort pre-op (SD) | Unsatisfied group pre-op(SD) | p-value | General cohort change in outcome scores between pre-op and post-op (SD) | Unsatisfied group change in outcome scores between pre-op and post-op (SD) | p-value | |
|---|---|---|---|---|---|---|
| Oxford Knee Score |
29.03 (8.75) |
24.07 (8.64) |
0.059 |
14.21 (9.08) |
13.50(11.55) |
0.827 |
| KOOS - Pain | 60.07 (18.84) | 57.74 (19.34) | 0.674 | 30.29 (19.88) | 26.59 (19.99) | 0.520 |
| KOOS - Other symptoms | 63.43 (18.42) | 51.28 (18.72) | 0.0348 | 26.51 (17.97) | 32.91 (18.96) | 0.247 |
| KOOS - Function in daily living | 66.56 (16.78) | 62.50 (16.88) | 0.405 | 26.24 (16.98) | 25.42 (20.87) | 0.890 |
| KOOS - Function in sports | 35.60 (18.57) | 30.36 (21.88) | 0.402 | 40.12 (26.31) | 34.29 (40.61) | 0.607 |
| KOOS - Knee related QOL |
45.25 (18.04) |
42.86 (21.07) |
0.689 |
34.35 (22.01) |
23.21 (25.05) |
0.131 |
| SF36 - Physical functioning | 41.68 (23.04) | 25.36 (12.63) | <0.001 | 37.44 (26.80) | 36.79 (32.91) | 0.944 |
| SF36 - Role limitations physical health | 26.80 (36.09) | 14.29 (21.29) | 0.069 | 54.60 (45.72) | 50.00 (43.85) | 0.716 |
| SF36 - Role limitations due to emotional problems | 59.20 (44.37) | 59.52 (45.63) | 0.980 | 26.40 (46.24) | 16.67 36.40) | 0.369 |
| SF36 - Energy/Fatigue | 59.12 (13.86) | 57.14 (11.88) | 0.569 | 12.24 (15.52) | 4.29 (20.37) | 0.178 |
| SF36 -Emotional well-being | 68.86 (12.28) | 64.00 (10.29) | 0.118 | 7.20 (12.85) | 6.86 (15.88) | 0.939 |
| SF36 - Social functioning | 62.90 (21.17) | 59.82 (19.72) | 0.590 | 24.80 (21.59) | 21.43 (27.05) | 0.659 |
| SF36 - Pain | 56.20 (21.36) | 49.29 (13.39) | 0.103 | 30.38 (22.88) | 25.54(24.79) | 0.495 |
| SF36 - General health |
59.24 (17.24) |
55.00 (12.86) |
0.275 |
13.72 (16.41) |
11.07 (20.02) |
0.640 |
| NPRS score | 7.08 (1.20) | 7.71 (1.27) | 0.093 | −5.42 (2.38) | −3.64 (3.05) | 0.0521 |
SD: Standard deviation.
SF36: Short Form-36.
NPRS: Numeric Pain Rating Scale.
There was no significant difference in terms of the change in outcome scores between the general cohort versus the unsatisfied group (Table 3).
The pre-op Kellgren-Lawrence scores in the general cohort, unsatisfied group and the TKR group were also assessed. The mean pre-op Kellgren-Lawrence score for the general cohort and unsatisfied group were similar at 2.02 (SD 0.580) and 2.00 respectively (SD 0.500). Higher Kellgren-Lawrence pre-op scores were seen in the TKR group at a mean of 2.4 (SD 0.516).
The general cohort showed progression of mean Kellgren-Lawrence scores from 2.02 (SD 0.580) to 2.67 (SD 0.673) over an average of 56.9 months. The TKR group showed more rapid progression in mean Kellgren Lawrence scores from 2.4 (SD 0.516) to 3.00 (SD 0.707) over an average of 24.6 years. The mean age of our TKR group was slightly older at 59.18 years compared to the mean age of 54.1 years in the general cohort at the time of the arthroscopic debridement.
There were several common procedures that were performed in addition to arthroscopic debridement. These include arthroscopic partial medial meniscectomy (APMM) and/or arthroscopic partial lateral meniscectomy (APLM) for degenerative meniscal tears, chondroplasty for unstable chondral flaps, lateral retinacular release for patellofemoral osteoarthritis in the setting of a tight patella retinaculum with lateral patella tilt, and microfracture for small, well-contained Outerbridge grade 3 to 4 cartilage lesions (<2 cm). Table 4 shows the breakdown of the procedures that were performed.
Table 4.
Arthroscopic procedures performed in addition to arthroscopic debridement.
| Number | Percentage (%) | |
|---|---|---|
| Arthroscopic partial meniscectomy | 131 (total) | 72.8 |
| APMM | 111 | 61.7 |
| APLM | 10 | 5.6 |
| APMM and APLM | 10 | 5.6 |
| Chondroplasty | 104 | 57.8 |
| Lateral retinacular release | 88 | 48.9 |
| Microfracture | 41 | 22.8 |
| Others | ||
| Removal of loose bodies | 8 | 4.4 |
| Synovectomy | 2 | 1.1 |
| Meniscal repair | 2 | 1.1 |
APMM: Arthroscopic Partial Medial Meniscectomy.
APLM: Arthroscopic Partial Lateral Meniscectomy.
Most arthroscopies had multiple procedures performed. Arthroscopic partial menisectomy is the most common procedure, occurring in 72.8% of the 180 arthroscopies performed with the majority being APMM alone. Chondroplasty was performed in 57.8%, lateral retinacular release was performed in 48.9% and microfracture was performed in 22.8% of the cases respectively.
Surgical technique
Herein we describe the surgical techniques used in our study.
Anaesthesia was either a general anaesthesia or spinal anaesthesia. No intravenous or oral prophylactic antibiotics were given pre-operatively or post-operatively for all cases. A tourniquet was used in all cases and routine anteromedial and anterolateral arthroscopic portals were used.
Arthroscopic partial meniscectomy
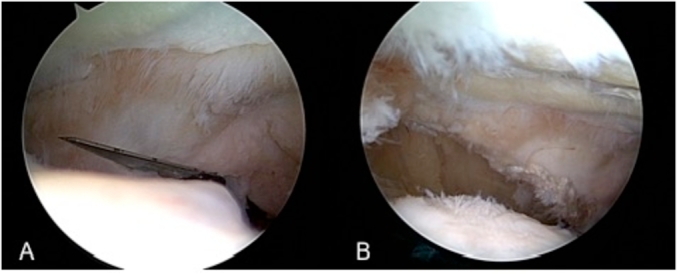
An arthroscopic shaver was used to debride the degenerative meniscal tears to a stable rim during partial meniscectomies (Fig. 2). In cases where the torn meniscus fragments were large and unstable, an arthroscopic punch forceps was used to facilitate the debridement prior to using the arthroscopic shaver.
Fig. 2.

(A) Unstable degenerative meniscal tear (B) Post-debridement of degenerative meniscal tear to stable rim.
Chondroplasty and microfracture
A similar method was employed for chondroplasties. Unstable chondral flaps were debrided to a stable rim and microfracture was performed if the post-debridement defect size was less than 2 cm in size (Fig. 3). This was performed using a 30-degree bone awl to place holes 3–4 mm apart starting with the periphery of the defect and progressing to the center subsequently. To confirm adequate penetration into the subchondral bone, the arthroscopic pump was stopped to confirm marrow elements flowing from the area of microfracture.
Fig. 3.

(A) Unstable chondral flap (B) Chondral defect post-debridement of unstable chondral flap (C) Microfracture performed starting with periphery of defect (D) Microfracture holes placed 3–4 mm apart.
Arthroscopic lateral retinacular releases were only performed in cases that demonstrated clinical findings suggestive of patellofemoral symptoms, radiographic features of lateral patella tilt on Xrays and intraoperative findings of a tight patella retinaculum by assessing the patella tilt with the knee in full extension after the patient has been put under anaesthesia.
Lateral retinacular release was performed using a minimally invasive approach using a size 11 scalpel blade (Fig. 4). The lateral patella retinaculum is visualized from within the knee joint and the blade is introduced into the joint via an arthroscopic portal created superolateral to the patella. A longitudinal cut is then made using the blade through all the retinacular layers in the sulcus between the lateral border of the patella and the lateral edge of the trochlea in a superior to inferior direction under direct visualization using the arthroscope with the blade. Once the procedure is complete, the knee is brought into full extension again and reassessment of the patella tilt is performed. Passive tilt of the patella should increase post-procedure and the patella tilt should range between 30 and 45°.
Fig. 4.
(A) Scalpel blade introduced into joint via superolateral arthroscopic portal (B) Lateral retinacular release performed.
All patients were allowed full weight bearing postoperatively and were assessed by our physiotherapists before they were discharged home. They were then followed up at the outpatient clinic at 1 month, 3 months, 6 months, 1 year, 2 years, and 5 years postoperatively.
Discussion
In a review paper published in The Bone & Joint Journal, Bollen criticized the methodology of Thorlund et al.'s systematic review and questioned the validity of the conclusions derived from the meta-analysis. The choice of papers was scrutinized and deemed not to have sufficient scientific rigor to amount to an unbiased, appropriate selection.17
Our study population is a specific subgroup of patients that are refractory to maximal conservative treatment and unsuitable candidates for knee replacement surgery. This is a group that is generally younger, most of whom belong to the employed population where there is pressure to return to work and to be able to perform.
Patient selection is critical in achieving good outcomes for patients. Patients with end-stage osteoarthritis, severe malalignment and those who do not have mechanical symptoms are unlikely to improve.18 We offered arthroscopic debridement to our group of patients who presented with largely mechanical symptoms suggestive of meniscal tears or chondral flaps and to those with symptomatic patellofemoral osteoarthritis. The majority of our patients had Kellgren-Lawrence Grade 2 knee osteoarthritis on plain radiographs. Our selection of patients suitable for knee arthroscopy was stringent. This is in line with earlier studies suggesting that with proper patient selection, arthroscopic surgery is beneficial in patients with early degenerative arthritis and mechanical symptoms.18,19
Our patients reported that their expectations were met in 96% of the knee arthroscopies performed. 90% of arthroscopies were rated ‘Good to Excellent’ in the assessment of the overall results. This is supported by good functional outcomes with consistent, significant improvements seen across all scoring systems (Oxford Knee Score, KOOS Knee Survey, SF-36, NPRS) used in the evaluation of our intervention. Our findings are consistent with Herrlin et al.'s study where one third of patients receiving physical therapy continued to experience disabling symptoms but improved after arthroscopic intervention.20
The remaining 10% of arthroscopies (13 out of 125 arthroscopies) which were not rated ‘Good to Excellent’ arthroscopies were rated ‘Fair’ in their assessment. Interestingly, despite being rated ‘Fair’, expectations of the surgery were met in 9 of the 13 arthroscopies performed. No arthroscopies were rated ‘Poor to Terrible’.
Arthroscopic debridement did not meet expectations in 4% of arthroscopies (5 out of 125 arthroscopies). One patient reported his results of surgery as ‘Good’ although it did not meet his expectations. The other 4 patients rated the results of surgery as ‘Fair’.
Our results suggest that arthroscopic debridement was able to provide significant symptomatic relief and functional improvement in a setting that is otherwise refractory to non-operative treatment. It is important to highlight that there were no adverse associated events post-operatively in relation to the arthroscopies.
Whilst any surgical procedure may be associated with harm, the incidence of those associated with simple arthroscopy is extremely low.17 Katz et al. reported no significant difference in the frequency of adverse events in patients managed with arthroscopic surgery with post-operative physical therapy compared to physical therapy alone.12
The incidence of symptomatic venous thromboembolism post-arthroscopic knee surgery in the literature is very low. Maletis et al. reported a ninety-day incidence of symptomatic venous thromboembolism post-arthroscopic knee surgery at 0.25% incidence for deep vein thrombosis and 0.17% incidence for pulmonary embolism.21 Mauck et al. reported a similar incidence at 0.4% of venous thromboembolism with DVT and/or pulmonary embolism.22.In a larger study by Hetsroni et al. looking at registry data from 418323 arthroscopies performed between 1997 and 2006, the incidence of pulmonary embolism was even lower at 0.00028% with 117 cases found (2.8 cases for every 10000 arthroscopies).23 There were no cases of symptomatic venous thromboembolism in any of our patients on long-term follow-up.
Surgical site infections post-knee arthroscopy is also rare, with reported rates ranging from 0.01% to 0.48%, and no difference in infection rates with use of antibiotic prophylaxis.24,25 Prophylactic antibiotics is not routinely practised in our practice. Bert et al.'s study comparing the infection rate of patients who received antibiotics versus those who did not in routine arthroscopic meniscectomy of the knee was 0.15% versus 0.16% respectively.25 We report no cases of deep or superficial surgical site infections in the 180 consecutive cases of knee arthroscopies performed in our patients.
The risk of death post-knee arthroscopy is even rarer. In Maletis et al.'s study looking at 20770 patients post elective knee arthroscopy, only one surgically attributable death was reported.21 There were 3 deaths in our study, none of which was related to the surgery. 1 died of metastatic colon cancer, 1 died of pneumonia on the background of metastatic lung cancer and 1 died secondary to a road traffic accident.
Knee arthroscopy is a simple procedure commonly performed on an outpatient basis or with an overnight stay in the hospital. The alternative treatment modality available to the clinician would be to counsel the patients to persist with non-operative interventions, which have proven to be non-efficacious in their case. Although this may possibly take a turn for the better with persisted effort, there is no indication when this turn will happen and patients will still need to face ongoing pressures to return to work during the interim. We believe that in selected patients who are very symptomatic in their daily or work life, refractory to 2 months of maximal conservative treatment and face a strong need to return to good function, arthroscopic debridement may be considered as an effective treatment modality. This is in line with the official European consensus for the management of degenerative meniscus lesions, derived from the ESSKA Meniscus Consensus Project, offering arthroscopic surgery only after failure of non-operative treatment.26
Strengths
Our single surgeon study reduces error from poor standardization in patient selection. As patient selection in our study plays a vital role in the outcomes, having uniformity in patient selection allows direct appreciation of its impact on the results.
Limitations
Although most of our patients were amenable to follow-up, the proportion of patients lost to follow-up was not small (23.7%). 60% of these patients lost to follow-up were foreign workers who were uncontactable after they returned to their home country upon completion of their employment contract.
Conclusion
In conclusion, arthroscopic knee debridement can provide good symptomatic relief and sustained benefits in significantly symptomatic patients with early degenerative knees who have failed conservative management. This is most useful in patients with mechanical symptoms secondary to degenerative meniscal tears, chondral flaps or loose bodies, and those with symptomatic patellofemoral osteoarthritis.
Conflicts of interest statement
The author(s) have no conflicts of interest relevant to this article.
FUNDING/SUPPORT statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Gin Way Law, Email: gin.law26@gmail.com.
Jing Kun Lee, Email: jingkun.lee@mohh.com.sg.
Junwei Soong, Email: junwei.soong@mohh.com.sg.
Jeremy Wei Sern Lim, Email: jeremy.lim@mohh.com.sg.
Karen Ting Zhang, Email: karen.zhang.ting@sgh.com.sg.
Andrew Hwee Chye Tan, Email: andrew.tan.h.c@singhealth.com.sg.
References
- 1.Thorlund J.B., Juhl C.B., Roos E.M., Lohmander L.S. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. BMJ. 2015;350:h2747. doi: 10.1136/bmj.h2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moseley J.B., O'Malley K., Petersen N.J. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81–88. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 3.Kirkley A., Birmingham T.B., Litchfield R.B. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359:1097–1107. doi: 10.1056/NEJMoa0708333. [DOI] [PubMed] [Google Scholar]
- 4.Elattrache N., Lattermann C., Hannon M., Cole B. New England Journal of Medicine article evaluating the usefulness of meniscectomy is flawed. Arthroscopy. 2014;30:542–543. doi: 10.1016/j.arthro.2014.02.010. [DOI] [PubMed] [Google Scholar]
- 5.Krych A.J., Stuart M.J., Levy B.A. Arthroscopic partial meniscectomy for degenerative meniscal tear. N Engl J Med. 2014;370:1259. doi: 10.1056/NEJMc1401128. [DOI] [PubMed] [Google Scholar]
- 6.Rossi M.J., D'Agostino R.B., Jr., Provencher M.T., Lubowitz J.H. Could the New England Journal of Medicine be biased against arthroscopic knee surgery? Arthroscopy. 2014;30:536–537. doi: 10.1016/j.arthro.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 7.Lubowitz J.H., Provencher M.T., Rossi M.J. Could the New England Journal of Medicine be biased against arthroscopic knee surgery? Part 2. Arthroscopy. 2014;30:654–655. doi: 10.1016/j.arthro.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 8.Kim S., Bosque J., Meehan J.P., Jamali A., Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of national surveys of ambulatory surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93:994–1000. doi: 10.2106/JBJS.I.01618. [DOI] [PubMed] [Google Scholar]
- 9.Bohensky M.A., Sundararajan V., Andrianopoulos N. Trends in elective knee arthroscopies in a population-based cohort, 2000-2009. Med J Aust. 2012;197:399–403. doi: 10.5694/mja11.11645. [DOI] [PubMed] [Google Scholar]
- 10.Harris I.A., Madan N.S., Naylor J.M., Chong S., Mittal R., Jalaludin B.B. Trends in knee arthroscopy and subsequent arthroplasty in an Australian population: a retrospective cohort study. BMC Muscoskel Disord. 2013;14:143. doi: 10.1186/1471-2474-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thorlund J.B., Hare K.B., Lohmander L.S. Large increase in arthroscopic meniscus surgery in the middle-aged and older population in Denmark from 2000 to 2011. Acta Orthop. 2014;85:287–292. doi: 10.3109/17453674.2014.919558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz J.N., Losina E. Surgery versus physical therapy for meniscal tear and osteoarthritis. N Engl J Med. 2013 Aug 15;369(7):677–678. doi: 10.1056/NEJMc1307177. [DOI] [PubMed] [Google Scholar]
- 13.Ricci J.A., Stewart W.F., Chee E., Leotta C., Foley K., Hochberg M.C. Pain exacerbation as a major source of lost productive time in US workers with arthritis. Arthritis Rheum. 2005;53(5):673–681. doi: 10.1002/art.21453. [DOI] [PubMed] [Google Scholar]
- 14.Kotlarz H., Gunnarsson C.L., Fang H., Rizzo J.A. Osteoarthritis and absenteeism costs: evidence from US national Survey data. J Occup Environ Med. 2010;52(3):263–268. doi: 10.1097/JOM.0b013e3181cf00aa. [DOI] [PubMed] [Google Scholar]
- 15.Kleinman N., Harnett J., Melkonian A., Lynch W., Kaplan-Machlis B., Silverman S. Burden of fibromyalgia and comparisons with osteoarthritis in the workforce. J Occup Environ Med. 2009;51(12):1384–1393. doi: 10.1097/JOM.0b013e3181bb808b. [DOI] [PubMed] [Google Scholar]
- 16.DiBonaventura M.D., Gupta S., McDonald M., Sadosky A. Evaluating the health and economic impact of osteoarthritis pain in the workforce: results from the National Health and Wellness Survey. BMC Muscoskel Disord. 2011;12:83. doi: 10.1186/1471-2474-12-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bollen S.R. Is arthroscopy of the knee completely useless? Meta-analysis--a reviewer's nightmare. Bone Joint Lett J. 2015 Dec;97-B(12):1591–1592. doi: 10.1302/0301-620X.97B12.37456. [DOI] [PubMed] [Google Scholar]
- 18.Day B. The indications for arthroscopic debridement for osteoarthritis of the knee. Orthop Clin N Am. 2005 Oct;36(4):413–417. doi: 10.1016/j.ocl.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 19.Hunt S.A., Jazrawi L.M., Sherman O.H. Arthroscopic management of osteoarthritis of the knee. J Am Acad Orthop Surg. 2002 Sep-Oct;10(5):356–363. doi: 10.5435/00124635-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Herrlin S.V., Wange P.O., Lapidus G., Hållander M., Werner S., Weidenhielm L. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up. Knee Surg Sports Traumatol Arthrosc. 2013 Feb;21(2):358–364. doi: 10.1007/s00167-012-1960-3. [DOI] [PubMed] [Google Scholar]
- 21.Maletis G.B., Inacio M.C., Reynolds S., Funahashi T.T. Incidence of symptomatic venous thromboembolism after elective knee arthroscopy. J Bone Joint Surg Am. 2012 Apr 18;94(8):714–720. doi: 10.2106/JBJS.J.01759. [DOI] [PubMed] [Google Scholar]
- 22.Mauck K.F., Froehling D.A., Daniels P.R. Incidence of venous thromboembolism after elective knee arthroscopic surgery: a historical cohort study. J Thromb Haemostasis. 2013 Jul;11(7):1279–1286. doi: 10.1111/jth.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hestroni I., Lyman S., Do H., Mann G., Marx R.G. Symptomatic pulmonary embolism after outpatient arthroscopic procedures of the knee: the incidence and risk factors in 418,323 arthroscopies. J Bone Joint Surg [Br] 2011;93-B:47–51. doi: 10.1302/0301-620X.93B1.25498. [DOI] [PubMed] [Google Scholar]
- 24.Babcock H.M., Matava M., Fraser V. Postarthroscopy surgical site infections: review of the literature. Clin Infect Dis. 2002 Jan 1;34(1):65–71. doi: 10.1086/324627. [DOI] [PubMed] [Google Scholar]
- 25.Bert J.M., Giannini D., Nace L. Antibiotic prophylaxis for arthroscopy of the knee: is it necessary? Arthroscopy. 2007 Jan;23(1):4–6. doi: 10.1016/j.arthro.2006.08.014. [DOI] [PubMed] [Google Scholar]
- 26.Beaufils P., Becker R., Kopf S. Surgical management of degenerative meniscus lesions: the 2016 ESSKA meniscus consensus. Knee Surg Sports Traumatol Arthrosc. 2017 Feb;25(2):335–346. doi: 10.1007/s00167-016-4407-4. [DOI] [PMC free article] [PubMed] [Google Scholar]



