Abstract
Substantial research has examined birth outcomes by race/ethnicity, noting not only disparities by race/ethnicity, but different maternal age patterns in low birth weight (LBW) prevalence. Few studies have examined these disparities among American Indian/Alaska Native (AI/AN) mothers, whose LBW prevalence is below the national average, despite substantial socioeconomic disadvantage among the population. Prior work has hypothesized that AI/AN mothers should exhibit LBW age patterns similar to those seen in NH black mothers as a result of exposure to cumulative stress, trauma, and socioeconomic disadvantage, but this has not been empirically tested. This paper uses data from the 2014–2016 U.S. Birth File, which contains records of all U.S. births for those years to examine maternal age patterns in birth weight among AI/AN mothers. Importantly, this study also considers high birth weight (HBW) births, given higher prevalence of diabetes in the AI/AN population, and proposes that if “weathering” is occurring in this population, HBW prevalence likely will influence the observed maternal age patterns in birth weight, such that prevalence of births in normal range may resemble NH blacks, even if LBW prevalence does not. Findings suggest modest evidence of weathering in AI/AN populations for LBW. Examination of normal birth weight births suggests that inclusion of HBW to the risk profile of AI/AN births better defines birth outcome risk in this population relative to white mothers. Smoking during pregnancy and gestational diabetes were particularly prevalent among AI/AN mothers and present reason for concern in spite of relatively favorable birth outcomes.
Keywords: American Indian/Alaska Native, Birth outcomes, Weathering hypothesis
Highlights
-
•
American Indian/Alaska Native (AI/AN) birth outcomes resemble white mothers, despite substantially higher rates of gestational diabetes.
-
•
Age patterns of low birth weight in AI/AN mothers modestly suggest patterns in line with the weathering hypothesis.
-
•
AI/AN birth outcomes and risks have been ignored in research literature because of relatively small population size.
-
•
AI/AN mothers have higher rates of gestational diabetes than other groups, and higher smoking rates at older ages.
1. Introduction
Disparities in birth outcomes are an important marker of population health, with implications for both maternal and child health. Racial and ethnic disparities in low birth weight (LBW) in the United States are well established. NH black mothers exhibit LBW prevalence about 1.8 times higher than white mothers, and substantially higher than most other racial/ethnic groups (Martin, Hamilton, Osterman, Curtin, & Mathews, 2015). Beyond these disparities, a body of research has explored a pattern termed the “weathering hypothesis,” which is represented by findings of disproportionately increasing rates of LBW and infant mortality by maternal age among NH black relative to white mothers (Cohen, 2016, Dennis and Mollborn, 2013, Geronimus, 1992, Geronimus, 1996, Reichman and Pagnini, 1997, Rich-Edwards et al., 2003). Explanations suggest that exposure to cumulative stress associated with higher rates of socioeconomic disadvantage over the life course produce an accelerated aging, or weathering, in this population. This age pattern has also been explored in Mexican American mothers, with evidence suggesting weathering in infant mortality, but less so for LBW (Collins et al., 2012, Powers, 2013, Wildsmith, 2002). This paper extends exploration of potential weathering patterns to another population with high levels of socioeconomic disadvantage, American Indian and Alaska Native (AI/AN) mothers. AI/AN birth outcomes are often excluded from studies on the weathering hypothesis, likely because of their much smaller relative population size, making up only about 2% of the U.S. population (Annual Estimates, 2016).
About 7.5% of AI/AN births in 2013 were LBW, only slightly higher than the 7% of non-Hispanic (NH) white births (Martin et al., 2015). Despite this reasonably small disparity, maternal age patterns in LBW prevalence have not been explored. If long-term exposure to disadvantage is in fact the primary driver of the age patterns of unfavorable birth outcomes that exemplify the weathering hypothesis, AI/AN mothers should exhibit similar patterns to NH blacks, even if overall levels of LBW are much lower.
Palacios and Portillo (2009) provide a long list of unfavorable health outcomes with high prevalence in the AI/AN population, similarly noting socioeconomic disparities in the population. Further, they suggest that historical trauma and cumulative stressors relating to a population with high rates of suicide, alcohol, and disease morbidity have the potential to produce accelerated deterioration of health in AI/AN women of childbearing age relative to other racial/ethnic groups. Nearly one-third of AI/AN families with young children are in poverty, with rates even higher among some specific tribal populations (Sarche & Spicer, 2008).
The understanding of maternal age patterns in LBW prevalence for AI/AN women is complicated by two factors with counterbalancing effects on birth weight. First, 26% of AI/AN women report smoking during pregnancy, relative to NH white (14.3%), NH black (8.9%), and Hispanic (3.4%) mothers (Tong et al. 2013). Smoking during pregnancy is associated with increased likelihood of LBW (Ventura, Hamilton, Mathews, & Chandra, 2003). The second factor, diabetes, may potentially influence birth weights upward. American Indian populations have among the highest rates of Type II diabetes nationally (33%), including higher prevalence at younger ages, whereas Alaska Natives have among the lowest overall prevalence (5.3%) (Spanakis & Golden, 2013). Despite elevated rates of Type II diabetes, multi-state estimates place AI/AN gestational diabetes prevalence at 8.9%, lower than Hispanic (12.1%) and NH black (10.5), but higher than NH white (6.8%) mothers (DeSisto, Kim, & Sharma, 2014). Gestational diabetes is known to be associated with macrosomia, or high birth weight, (HBW, >4000 g) births (IADPSG, 2010).
National prevalence of HBW in AI/AN mothers is 9.8%, the highest among all reported racial/ethnic groups compared to a national average of 8.2%, although only slightly higher than the 9.6% among NH white mothers (Martin et al., 2015). Risks of HBW to mother and infant are relatively lower than those for LBW births, although HBW is associated with unfavorable early life health outcomes as well as some later life outcomes such as diabetes and asthma (Harder, Rodekamp, Schellong, Dudenhausen, & Plagemann, 2007; Lindberg, Adams, & Prince, 2012; Orskou, Henrisksen, Kesmodel, & Secher, 2003; Remes, Patel, Hartikainen, Jarvelin, & Pekkanen, 2008; Stene et al., 2001).
Consideration of the effects of smoking and gestational diabetes, taken as independent effects, would suggest that perhaps birth weight would be balanced between the countervailing effects such that LBW and HBW prevalence may not signal the AI/AN population to be a particularly high birth risk group. The standard outcomes of LBW or HBW may perhaps be too simplistic a measure to pick up birth outcomes risk in this population.
2. Data and methods
Data for this study come from the 2014–2016 U.S. Birth File, which contains records of all births in the U.S. for those years. The data is collected and compiled by the National Center for Health Statistics and downloaded from the National Bureau of Economic Research (NBER.org, 2018; NCHS, 2014–2016). Three years of data are combined to obtain an adequate sample size of AI/AN births. Data for this study are deidentified and freely available, and as such, the institutional review board declined to review the study as human subjects research based on these criteria.
The focal dependent variables are defined by standard cutoffs for LBW (less than 2500 g, about 5.5 lbs) and HBW (over 4000 g, about 8.8 lbs.) (Harder et al., 2007, Kramer, 1987). A category of “normal birth weight” (NBW) is also created to designate births that fall between the low and high birth weight births (2500–4000 g).
Analyses are limited to singleton births recorded in the vital statistics file as the mother’s first birth, as parity is known to be positively associated with birth weight (Swamy, Edwards, Gelfand, James, & Miranda, 2012). A number of past studies on the weathering hypothesis have limited analyses to this subpopulation (Geronimus, 1996, Nabukera et al., 2009). Table 1 shows frequencies by maternal age and race/ethnicity, resulting in a population size of 23,956 births for the focal group of AI/AN mothers. Foreign-born mothers are excluded due to potential bias from immigrant health advantage effects (Acevedo-Garcia, Soobader, & Berkman, 2005). Birth files from years 2011–2013 do not contain data on maternal nativity and were not aggregated with this data set. Maternal ages are grouped into 5 year categories, with a few exceptions, including “under 15” and “35 plus”. The number of first births at age 40 plus is not large enough for comparisons of this category.
Table 1.
Singleton first births (N), smoking (%,N), and gestational diabetes (%,N) among U.S. born mothers, by race/ethnicity and maternal age.
| Maternal age | NH white | NH black | AI/AN | Hispanic |
|---|---|---|---|---|
| Under 14 | 1587 | 2246 | 118 | 2173 |
| 15–19 | 196,573 | 97,916 | 7443 | 127,448 |
| 20–24 | 494,728 | 169,461 | 9619 | 180,517 |
| 25–29 | 581,637 | 73,231 | 4273 | 90,017 |
| 30–34 | 426,672 | 34,999 | 1811 | 46,399 |
| 35 plus | 146,641 | 16,692 | 662 | 17,283 |
| Total | 1,847,838 | 394,545 | 23,926 | 463,837 |
| Smoking during pregnancy | ||||
| Under 15 | 7.80 (122) | 0.76 (17) | 2.54 (<10) | 0.98 (21) |
| 15–19 | 17.43 (33,894) | 2.74 (2647) | 11.91 (872) | 2.02 (2560) |
| 20–24 | 15.12 (73,963) | 4.23 (7069) | 14.18 (1344) | 2.54 (4552) |
| 25–29 | 5.95 (34,248) | 4.41 (3182) | 10.70 (453) | 1.87 (1673) |
| 30–34 | 3.54 (14,927) | 3.80 (1310) | 8.58 (154) | 1.36 (625) |
| 35 plus | 3.79 (5485) | 3.32 (546) | 8.66 (57) | 1.35 (232) |
| Total | 8.90 (162,639) | 3.80 (14,771) | 12.21 (2883) | 2.10 (9663) |
| Gestational diabetes | ||||
| Under 15 | 1.58 (25) | 0.72 (16) | 2.54 (<10) | 1.06 (23) |
| 15–19 | 2.21 (4343) | 1.46 (1429) | 3.51 (261) | 1.83 (2322) |
| 20–24 | 3.31 (16,341) | 2.65 (4482) | 5.84 (560) | 3.18 (5723) |
| 25–29 | 4.36 (25,285) | 4.50 (3288) | 9.42 (402) | 5.16 (4638) |
| 30–34 | 5.29 (22,514) | 6.45 (2252) | 12.02 (217) | 6.72 (3115) |
| 35 plus | 7.44 (10,885) | 7.99 (1331) | 18.15 (120) | 9.06 (1563) |
| Total | 4.31 (79,393) | 3.25 (12,798) | 6.55 (1563) | 3.75 (17,384) |
Source: NCHS 2014–2016
Although vital statistics data provides minimal individual characteristics or behaviors, smoking during pregnancy (defined as any reported smoking while pregnant) and gestational diabetes are available for a majority of cases. Some cases are lost with the inclusion of these variables due to incomplete birth records or differences in state reporting standards. Given that education is highly correlated with maternal age for the study population, this study uses payment status, categorized as Medicaid, private insurance, self-pay, or other/unknown as a rough approximation for socioeconomic status (Geronimus, 1996).
The analysis for this study is performed on the population of births for a 3-year period in the U.S., rather than a sample. Statistical testing is designed to test how well sample characteristics represent the full population. As such, sample statistics are not appropriate for the findings here, as the differences in the population here do not have to be inferred, because the full population is already presented. Logistic regression odds ratios predicting NBW present 95% confidence intervals for reference, although again, the data set is not a representative sample and inferential statistics are not particularly meaningful. Vital statistics data of this nature lacks the detail of most in-depth survey datasets. However, this study aims to fill an important gap by understanding where AI/AN mothers fit in regard to birth outcome risks relative to other racial/ethnic groups.
3. Hypothesis
H1
: AI/AN mothers will have disproportionately increasing prevalence of LBW births with increasing age, relative to white mothers.
H2
: AI/AN mothers will have disproportionately lower prevalence of NBW births with increasing age, relative to white mothers.
4. Results
The use of large vital statistics birth files provides a large comparison population of race/ethnicity and maternal age for comparison of population birth weights. Table 1 highlights that smoking during pregnancy is highest in NH white mothers under age 25 and highest in AI/AN mothers from age 25 on. Gestational diabetes is highest in AI/AN mothers at all ages, although particularly at older ages. Combined, these health factors stand to have a substantial impact on AI/AN birth outcomes at later childbearing ages.
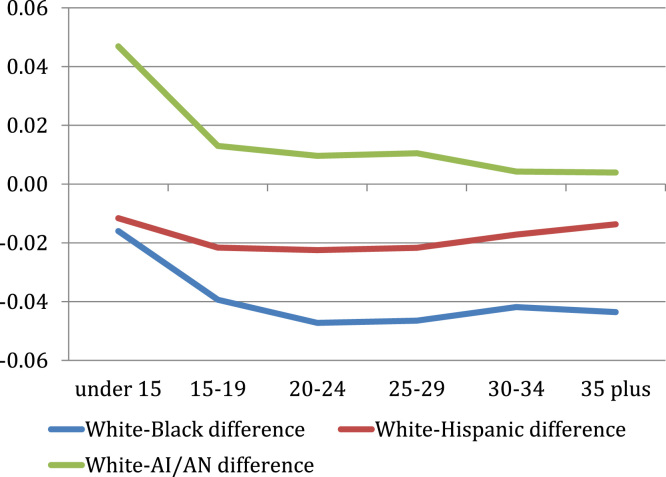
Table 2 shows LBW prevalence in the 3-year period for first births, among the four racial/ethnic groups of interest. AI/AN birth weights in this table do not differ greatly in magnitude from white mothers at any age in this table. However, the weathering hypothesis posits that prevalence of unfavorable birth outcomes accelerates with age. As such, the two columns on the right hand side of Table 2, followed by Fig. 1, demonstrate that AI/AN LBW prevalence worsens with age, relative to white mothers. The gradient of this difference is similar to that of NH black mothers, despite the magnitude of the difference being much larger for NH black mothers.
Table 2.
Prevalence of LBW,* by Race/Ethnicity, among U.S.-born first births, 2014–2016.
| Maternal age | White | Black | Hispanic | AI/AN |
| Under 15 | 0.10 | 0.14 | 0.10 | 0.08 |
| 15–19 | 0.07 | 0.13 | 0.07 | 0.06 |
| 20–24 | 0.06 | 0.12 | 0.07 | 0.06 |
| 25–29 | 0.05 | 0.13 | 0.07 | 0.07 |
| 30–34 | 0.06 | 0.14 | 0.07 | 0.07 |
| 35 plus | 0.08 | 0.18 | 0.09 | 0.11 |
| White-Black difference | White-Hispanic difference | White-AI/AN difference | ||
| Under 15 | – | 0.04 | 0.01 | -0.02 |
| 15–19 | – | 0.05 | 0.00 | -0.01 |
| 20–24 | – | 0.06 | 0.01 | 0.00 |
| 25–29 | – | 0.08 | 0.02 | 0.02 |
| 30–34 | – | 0.09 | 0.02 | 0.02 |
| 35 plus | – | 0.10 | 0.02 | 0.03 |
LBW - <2500 g.
Source: NCHS 2014–2016
Fig. 1.
Difference in low birth weight prevalence relative to NH white mothers among NH black, Hispanic, and AI/AN mothers.
Although the absolute differences are small, the differences in LBW between 15–19 year old teenage mothers and their 30–34 year old counterparts provide interesting racial/ethnic differences. The white age 30–34 group exhibits lower 1% LBW prevalence than the 15–19 year-old group, whereas NH black and AI/AN 30–34 year old mothers each have 1% higher prevalence of LBW, respectively, than their 15–19 year old counterparts. White mothers’ LBW prevalence, as has been well established, begins very high in teenage years and drops to its lowest point at ages 25–29. For NH black and AI/AN mothers, this drop happens earlier, at 20–24, or is practically non-existent, in the case of AI/AN mothers, who see no improvement in LBW prevalence from ages 15–19 to 20–24.
The descriptive findings above provide modest support for hypothesis 1, which posits that AI/AN birth outcomes will become increasingly unfavorable with age, relative to those of whites. However, despite some evidence of patterns supportive of the weathering hypothesis, AI/AN LBW prevalence is low relative to NH black mothers. This finding leads to the second hypothesis, which suggests that consideration of HBW may provide better insight into the risk profile of AI/AN birth outcomes.
Table 3 shows that, as expected based on national rates, HBW prevalence is higher for AI/AN mothers compared to the other three groups across all ages, although the difference between AI/AN and white mothers after age 30 is negligible. Fig. 2 illustrates how HBW prevalence is very similar for white and AI/AN mothers, much lower for NH black mothers, and slightly higher for Hispanic mothers.
Table 3.
Prevalence of HBW,* by Race/Ethnicity, among U.S.-born first births, 2014–2016.
| Maternal age | White | Black | Hispanic | AI/AN |
| Under 15 | 0.04 | 0.02 | 0.03 | 0.08 |
| 15–19 | 0.06 | 0.02 | 0.04 | 0.07 |
| 20–24 | 0.08 | 0.03 | 0.05 | 0.09 |
| 25–29 | 0.09 | 0.04 | 0.07 | 0.10 |
| 30–34 | 0.09 | 0.05 | 0.07 | 0.09 |
| 35 plus | 0.08 | 0.04 | 0.07 | 0.09 |
| White-Black difference | White-Hispanic difference | White-AI/AN difference | ||
| Under 15 | – | -0.02 | -0.01 | 0.05 |
| 15–19 | – | -0.04 | -0.02 | 0.01 |
| 20–24 | – | -0.05 | -0.02 | 0.01 |
| 25–29 | – | -0.05 | -0.02 | 0.01 |
| 30–34 | – | -0.04 | -0.02 | 0.00 |
| 35 plus | – | -0.04 | -0.01 | 0.00 |
HBW - >4000 g.
Source: NCHS 2014–2016
Fig. 2.
Difference in high birth weight prevalence relative to NH white mothers among NH black, Hispanic, and AI/AN mothers.
Table 4 produces prevalence for NBW births by race/ethnicity and maternal age. Findings suggest that AI/AN and NH black mothers have disproportionately lower prevalence of NBW births relative to NH white mothers with increasing age, with the exception of ages 15–19, where NH white and AI/AN mothers are largely equal. Fig. 3 demonstrates a trend of decreasing NBW prevalence in NH black mothers, by age, relative to whites, supporting the weathering hypothesis. Hispanic mothers exhibit consistently higher NBW prevalence (i.e., more favorable birth outcomes), supporting prior research on the Hispanic (or Epidemiologic) Paradox (Acevedo-Garcia et al., 2005).
Table 4.
Prevalence of NBW,* by Race/Ethnicity, among U.S.-born first births, 2014–2016.
| Maternal age | White | Black | Hispanic | AI/AN |
| Under 15 | 0.87 | 0.84 | 0.87 | 0.84 |
| 15–19 | 0.87 | 0.85 | 0.89 | 0.86 |
| 20–24 | 0.86 | 0.85 | 0.88 | 0.85 |
| 25–29 | 0.86 | 0.83 | 0.86 | 0.83 |
| 30–34 | 0.86 | 0.81 | 0.86 | 0.84 |
| 35 plus | 0.84 | 0.78 | 0.84 | 0.81 |
| White-Black difference | White-Hispanic difference | White-AI/AN difference | ||
| Under 15 | – | -0.03 | 0.01 | -0.03 |
| 15–19 | – | -0.01 | 0.02 | 0.00 |
| 20–24 | – | -0.01 | 0.02 | -0.01 |
| 25–29 | – | -0.03 | 0.00 | -0.03 |
| 30–34 | – | -0.05 | 0.00 | -0.02 |
| 35 plus | – | -0.06 | 0.00 | -0.03 |
NBW - ≥ 2500 g & ≤ 4000 g.
Source: NCHS 2014–2016.
Fig. 3.
Difference in normal birth weight prevalence relative to NH white mothers among NH black, Hispanic, and AI/AN mothers.
Table 5 shows logistic regression odds ratios predicting NBW by maternal age and race/ethnicity, with controls for smoking during pregnancy, gestational diabetes, and payment source. Fig. 4 provides predicted probabilities based on logistic regression coefficients from the full model. After age 25, AI/AN mothers show modest evidence of the weathering hypothesis, with rates of NBW less than white mothers at comparable ages. Overall, the weathering hypothesis is more apparent among NH black mothers, whereas NBW prevalence for Hispanic mothers largely tracks with NH whites, with more favorable outcomes for Hispanic births at younger ages.
Table 5.
Logistic regression odds ratios predicting NBW among U.S.-born single births.
| OR | 95% CI | OR | 95% CI | |
|---|---|---|---|---|
| Race/ethnicity (NH white = ref) | ||||
| NH black | 0.83 | 0.82, 0.84 | 0.80 | 0.78, 0.82 |
| AI/AN | 0.91 | 0.88, 0.94 | 0.84 | 0.77, 0.91 |
| Hispanic | 1.10 | 1.08, 1.11 | 1.05 | 1.03, 1.07 |
| Maternal age (25–29 = ref) | ||||
| Under 15 | 1.07 | 1.00, 1.16 | 1.09 | 0.94, 1.26 |
| 15–19 | 1.15 | 1.14, 1.17 | 1.10 | 1.08, 1.12 |
| 20–24 | 1.10 | 1.09, 1.11 | 1.06 | 1.05, 1.07 |
| 30–34 | 0.95 | 0.94, 0.96 | 0.96 | 0.95, 0.97 |
| 35 plus | 0.84 | 0.83, 0.85 | 0.86 | 0.84, 0.87 |
| Smoked during pregnancy | 0.85 | 0.84, 0.86 | 0.86 | 0.85, 0.88 |
| Gestational diabetes | 0.83 | 0.82, 0.84 | 0.83 | 0.82, 0.84 |
| Payment status (private insurance =r ef) | ||||
| Medicaid | 0.94 | 0.93, 0.95 | 0.94 | 0.93, 0.95 |
| Self pay | 0.89 | 0.86, 0.91 | 0.89 | 0.87, 0.91 |
| Other/Unknown | 0.97 | 0.96, 0.99 | 0.98 | 0.96, 0.99 |
| Race*Age interactions | ||||
| NH black*under 15 | 1.00 | 0.83, 1.20 | ||
| NH black*15–19 | 1.10 | 1.07, 1.14 | ||
| NH black*20–24 | 1.11 | 1.08, 1.14 | ||
| NH black*30–34 | 0.92 | 0.89, 0.95 | ||
| NH black*35 plus | 0.86 | 0.82, 0.90 | ||
| AI/AN*under 15 | 0.96 | 0.57, 1.61 | ||
| AI/AN*15–19 | 1.18 | 1.06, 1.31 | ||
| AI/AN*20–24 | 1.11 | 1.01, 1.23 | ||
| AI/AN*30–34 | 1.06 | 0.91, 1.23 | ||
| AI/AN*35 plus | 1.01 | 0.82, 1.25 | ||
| Hispanic*under 15 | 1.02 | 0.84, 1.24 | ||
| Hispanic*15–19 | 1.13 | 1.10, 1.16 | ||
| Hispanic*20–24 | 1.09 | 1.07, 1.12 | ||
| Hispanic*30–34 | 0.97 | 0.93, 1.00 | ||
| Hispanic*35 plus | 0.95 | 0.91, 1.00 | ||
| Constant | 6.26 | 6.22, 6.30 | 6.31 | 6.27, 6.36 |
N = 2,685,180.
Source: NCHS 2014–2016
Fig. 4.
Predicted probabilities of NBW by maternal age and race/ethnicity, controlling for smoking status during pregnancy, insurance status, and gestational diabetes.
5. Discussion
This paper sought to explore LBW prevalence among AI/AN populations via the framework of the weathering hypothesis, as theorized by Palacios and Portillo (2009). Findings indicate that although AI/AN birth outcomes are reasonably similar to white mothers in aggregate, divisions by maternal age suggest modestly increasingly unfavorable birth outcomes with advancing age. This population level evidence provides indications that weathering is present in this population, and as such, AI/AN mothers of advancing age have increased risk of unfavorable birth outcomes relative to white mothers. AI/AN, NH black, and Hispanic mothers, do not see the reduction in LBW prevalence between the ages 15–19 and 30–34 that is seen in white mothers. That is, whereas white mothers’ birth weights benefit from delay of childbearing past the teenage years, other minority groups do not.
Bivariate findings in Table 1 highlight primary concerns for the AI/AN population, with particularly prevalent health insults due to smoking during pregnancy and gestational diabetes. AI/AN prevalence of gestational diabetes is 1.5–2 times as high as that of NH white mothers in every age group, and consistently higher than that found in NH black and Hispanic mothers as well. Smoking during pregnancy is problematic for both NH white and AI/AN mothers, although most prevalent for NH whites before age 25 and for AI/AN mothers after age 25. The contributions of these factors may cancel out impacts on birth weight in cases where both are present, and as such, birth weight may be a poor population-level indicator of birth outcomes in the AI/AN population.
Although Flores, Simonsen, Manuck, Dyer, and Turok (2012) find that foreign-born Hispanic mothers exhibit the most favorable birth outcomes, these findings suggest a birth weight advantage among U.S.-born Hispanics relative to NH whites as well. Fig. 3, Fig. 4 particularly highlight the overall favorable birth outcomes of U.S.-born Hispanic mothers relative to the other three groups. Among AI/AN mothers, increasing age generally produces lower prevalence of NBW, although the magnitude of difference is reasonably small and the trend does not follow a smooth age curve. Again, absolute differences are reasonably small, but provide modest support of hypothesis 2 in the context of NBW outcomes. As such, the weathering hypothesis among AI/AN mothers is defined primarily by differences in age patterns, with minor acceleration of unfavorable birth outcomes by age, in spite of overall similarities in LBW prevalence. Despite elevated risk factors for birth outcomes, AI/AN birth outcomes remain relatively similar to those of NH whites, particularly at younger ages. Although modest, Fig. 3, Fig. 4 demonstrate that AI/AN mothers do exhibit NBW prevalence indicative of the weathering hypothesis after age 25 relative to NH white mothers.
5.1. Limitations
Public use birth files do not allow for the identification of mothers residing on AI/AN reservations. Birth file data prior to 2005 provides some context on geographical location, but not with a level of specificity to identify individuals residing on a reservation. As such, this study uses the most recent years of data available (2014–2016) with information on maternal nativity.
Future analyses should examine second and later births, as weathering as a mechanism of accelerated aging should not be limited to women who are having their first child at later ages. This line of inquiry also relates to integrating an understanding of how normative age at first birth factors into the birth outcome risk of a population. AI/AN, NH black, and Hispanic mothers have lower average age at first birth than whites, and similarly have less favorable birth outcomes at earlier ages. This relationship should be explored more fully.
6. Conclusions
Support for weathering in the AI/AN population is modest, and although overall LBW prevalence for this population resembles that of white mothers, the age pattern of LBW relative to whites follows a trajectory of the weathering hypothesis. Age patterns in birth weight are similar in NH black and AI/AN mothers, although the former has much higher levels of LBW, whereas the latter has higher levels of HBW. Rates of NBW may better represent the birth risk in the AI/AN population, and HBW births should be considered for their potential risk factors as well. The potentially countervailing effects of smoking during pregnancy and gestational diabetes on birth weight are also a relevant point of discussion, suggesting that birth weight may be an overall poor measure of birth outcomes in this population. Future work should explore infant mortality, fetal distress, or other available birth outcomes to ascertain if this is the case. This study aims to take a first step toward understanding the basic age profile of AI/AN mothers relative to other racial/ethnic groups.
Ethical statements
I have no financial disclosures relating to this manuscript.
I have no other ethical declarations of interest for this manuscript.
References
- Acevedo-Garcia D., Soobader M.J., Berkman L.F. The differential effect of foreign-born status on low birth weight by race/ethnicity and education. Pediatrics. 2005;115(1):e20–e30. doi: 10.1542/peds.2004-1306. [DOI] [PubMed] [Google Scholar]
- Annual Estimates of the Resident Population by Sex (2016). Age, race alone or in combination, and hispanic origin for the United States and States: April 1, 2010 to July 1, 2015. Source: U.S. Census Bureau, Population Division. Release Date: June 2016. 〈https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?Pid=PEP_2015_PEPASR6H&prodType=table〉 (Accessed 24 April 2018).
- Cohen P.N. Maternal age and infant mortality for white, black, and mexican mothers in the United States. Sociological Science. 2016;3(2):32–38. [Google Scholar]
- Collins J.W., Rankin K.M., Hedstrom A.B. Exploring weathering: The relation of age to low birth weight among first generation and established United States-born Mexican-American women. Maternal and Child Health Journal. 2012;16:967–972. doi: 10.1007/s10995-011-0827-4. [DOI] [PubMed] [Google Scholar]
- Dennis J.A., Mollborn S. Young maternal age and low birth weight risk: An exploration of racial/ethnic disparities in the birth outcomes of mothers in the United States. Social Science Journal. 2013;50:625–634. doi: 10.1016/j.soscij.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSisto C.L., Kim S.Y., Sharma A.J. Prevalence estimates of gestational diabetes mellitus in the United States, pregnancy risk assessment monitoring system (PRAMS), 2007–2010. Preventing Chronic Disease. 2014;11:E104. doi: 10.5888/pcd11.130415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flores M.E., Simonsen S.E., Manuck T.A., Dyer J.M., Turok D.K. The ‘Latina Epidemiologic Paradox’: Contrasting patterns of adverse birth outcomes in U.S.-born and foreign-born Latinas. Women’States Health Issues. 2012;22:e501–e507. doi: 10.1016/j.whi.2012.07.005. [DOI] [PubMed] [Google Scholar]
- Geronimus A.T. The weathering hypothesis and the health of African-American women and infants: Evidence and speculations. Ethnicity Disease. 1992;2(3):207–221. [PubMed] [Google Scholar]
- Geronimus A.T. Black/white differences in the relationship of maternal age to birthweight: A population-based test of the weathering hypothesis. Social Science and Medicine. 1996;42:589–597. doi: 10.1016/0277-9536(95)00159-x. [DOI] [PubMed] [Google Scholar]
- Harder T., Rodekamp E., Schellong K., Dudenhausen J.W., Plagemann A. Birth weight and subsequent risk of Type 2 Diabetes: A meta-analysis. American Journal of Epidemiology. 2007;165:849–857. doi: 10.1093/aje/kwk071. [DOI] [PubMed] [Google Scholar]
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel (IADPSG) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–682. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer M.S. Determinants of low birth weight: Methodological assessment and meta-analysis. Bulletin of the World Health Organization. 1987;65:663–737. [PMC free article] [PubMed] [Google Scholar]
- Lindberg S.M., Adams A.K., Prince R.J. Early predictors of obesity and cardiovascular risk among American Indian children. Maternal and Child Health Journal. 2012;16:1879–1886. doi: 10.1007/s10995-012-1024-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- J.A. Martin, B.E. Hamilton, M.J.K. Osterman, S.C. Curtin, T.J. Mathews Final data for 2013. National vital statistics reports 2015 National Center for Health Statistics Hyattsville, MD 1 68.
- Nabukera S.K., Wingate M.S., Owen J., Salihu H.M., Swaminathan S., Alexander G.R., Kirby R.S. Racial disparities in perinatal outcomes and pregnancy spacing among women delaying initiation of childbearing. Maternal and Child Health Journal. 2009;13:81–89. doi: 10.1007/s10995-008-0330-8. [DOI] [PubMed] [Google Scholar]
- National Bureau of Economic Research (2018). 〈http://www.nber.org/data/natality.html〉 (Accessed 9 March 2018).
- National Center for Health Statistics (2014–2016). Data File Documentations, Natality, 2014–2016, National Center for Health Statistics, Hyattsville, Maryland.
- Orskou J., Henrisksen T.B., Kesmodel U., Secher N.J. Maternal characteristics and lifestyle factors and the risk of delivering high birth weight infants. Obstetrics Gynecology. 2003;102:115–120. doi: 10.1016/s0029-7844(03)00402-2. [DOI] [PubMed] [Google Scholar]
- Palacios J.F., Portillo C.J. Understanding native women’s health. Journal of Transcultural Nursing. 2009;20:15–27. doi: 10.1177/1043659608325844. [DOI] [PubMed] [Google Scholar]
- Powers D.A. Paradox revisited: A further investigation of race/ethnic differences in infant mortality by maternal age. Demography. 2013;50:495–520. doi: 10.1007/s13524-012-0152-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichman N.E., Pagnini D.L. Maternal age and birth outcomes: Data from New Jersey. Family Planning Perspectives. 1997;29 (268–72+295) [PubMed] [Google Scholar]
- Remes S.T., Patel S.P., Hartikainen A.L., Jarvelin M.R., Pekkanen J.H. High birth weight, asthma and atopy at the age of 16 yr. Pediatric Allergy and Immunology. 2008;19:541–543. doi: 10.1111/j.1399-3038.2007.00707.x. [DOI] [PubMed] [Google Scholar]
- Rich-Edwards J.W., Buka S.L., Brennan R.T., Earls F. Diverging associations of maternal age with low birthweight for black and white mothers. International Journal of Epidemiology. 2003;32:83–90. doi: 10.1093/ije/dyg008. [DOI] [PubMed] [Google Scholar]
- Sarche M., Spicer P. Poverty and health disparities for American Indian and Alaska Native children: Current knowledge and future prospects. Annals of the New York Academy of Sciences. 2008;1136:126–136. doi: 10.1196/annals.1425.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanakis E.K., Golden S.H. Race/Ethnic difference in diabetes and diabetic complications. Current Diabetes Reports. 2013;13(6) doi: 10.1007/s11892-013-0421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stene L.C., Magnus P., Lie R., Sovik T., Joner O., G. & The Norwegian Childhood Diabetes Study Group Birth weight and childhood onset Type 1 Diabetes: Population based cohort study. British Medical Journal. 2001;322:889–892. doi: 10.1136/bmj.322.7291.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swamy G.K., Edwards S., Gelfand A., James S.A., Miranda M.L. Maternal age, birth order, and race: Differential effects on birthweight. Journal Epidemiology Community Health. 2012;66:136–142. doi: 10.1136/jech.2009.088567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong V.T., Dietz P.M., Morrow B., D'Angelo D.V., Farr S.L., Rockhill K.M. Trends in smoking before, during, and after pregnancy—Pregnancy Risk Assessment Monitoring System, United States, 40 sites, 2000–2010. MMWR Surveill Summ. 2013;62:1–19. [PubMed] [Google Scholar]
- Ventura S.J., Hamilton B.E., Mathews T.J., Chandra A. Trends and variations in smoking during pregnancy and low birth weight: Evidence from the birth certificate, 1990–2000. Pediatrics. 2003;111(5):1176–1180. [PubMed] [Google Scholar]
- Wildsmith E.M. Testing the weathering hypothesis among Mexican-origin women. Ethnicity Disease. 2002;12:470–479. [PubMed] [Google Scholar]