Abstract
Background
Depression is a major cause of disability among children and adolescents and is associated with elevated risks for substance abuse, HIV transmission risk behavior, and suicide. Among adolescents living with HIV (ALWH), depression undermines adherence to antiretroviral treatment, leading to poorer health outcomes. However, there are few instruments available for depression screening among ALWH in sub-Saharan Africa.
Methods
Using mixed methods we developed and validated a 20-item depression screening scale to be used among ALWH in rural Uganda. First, we conducted focus group discussions and in-depth interviews with adolescents and adult caregivers (n = 80) to elicit participant perspectives about mental health challenges facing HIV-affected children and adolescents. We generated an initial pool of 40 items, pilot tested it with ALWH and adolescents of unknown serostatus (n = 40), and then administered the items to a validation sample of ALWH (n = 224). Exploratory factor analysis was used to examine the factor structure of the scale. We evaluated the scale for its reliability, and validity.
Results
The mean age of the participants in the validation sample was 14.9 years (standard deviation [SD] 1.4), 131 (58%) were girls and 48 (21%) were orphans. Exploratory factor analysis revealed two factors related to affective and cognitive symptoms of depression. The 20-item depression scale was internally consistent (Cronbach’s alpha = 0.91) with moderate test-retest and inter-rater reliability. Construct validity was excellent, as demonstrated through correlation with related constructs like stigma (P< 0.001) and bullying (P< 0.001). At the optimized cutoff score, 64 (29%) participants screened positive for probable depression. Using the Mini-International Neuropsychiatric Interview for Children and Adolescents, we found that 37 participants (17%) were diagnosed with major depressive disorder. In reference to the criterion standard, the depression scale showed excellent discrimination (c-statistic = 0.84).
Conclusion
This new 20-item depression scale was reliable and valid for detecting major depressive disorder among ALWH in rural Uganda.
Keywords: HIV, Adolescent, Depression, Screening, Uganda
Highlights
-
•
There are few culturally- and age-appropriate screening scales for use among adolescents with HIV in sub-Saharan Africa.
-
•
We used qualitative methods to generate new scale items, and adapted items from previously published depression screening scales.
-
•
The items in the newly developed scale consist of well-known affective and cognitive symptoms of depression.
-
•
The scale has adequate internal consistency, test-retest, and inter-rater reliability, and adequate evidence of construct and criterion-related validity.
1. Background
Depression is a leading cause of disability among children and adolescents worldwide (World Health Organization, 2008). In these key populations, depression has been associated with substance abuse, early sexual debut, HIV transmission risk behavior and elevated suicide risk (Dick and Ferguson, 2015, Mutumba and Harper, 2015, Rubin et al., 2009, Saluja et al., 2004, Tinasti, 2018). In sub-Saharan Africa, the burden of depression is thought to be higher among HIV-affected children and adolescents compared with those in the general population (Lester et al., 2002, Mutumba et al., 2015a, Rotheram-Borus et al., 2005), with an estimated prevalence of 17–25 percent (Betancourt et al., 2014, Kamau et al., 2012, Kim et al., 2014a). Among adults with HIV, depression has been additionally linked to poor adherence to antiretroviral treatment and poorer health outcomes (Dow et al., 2016, Lowenthal et al., 2015, Mutumba et al., 2016, Tsai, 2014, Tsai et al., 2010).
Despite the impact of depression on health outcomes, there remain limited data regarding its prevalence among adolescents living with HIV (ALWH) in sub-Saharan Africa. There are few culturally sensitive, standardized, and validated depression screening scales for use in this population (Mutumba, Tomlinson, & Tsai, 2014). The few depression scales available were developed for adults and imported from high income countries (Binagwaho et al., 2016, Kim et al., 2014a, Stockings et al., 2015). A notable departure is the Hopkins Symptom Check List (HSCL), which has been used extensively to screen for depression among adults living with HIV in rural Uganda (Ashaba et al., 2018b, Kaida et al., 2014, Martinez et al., 2008), and which was adapted for use in Uganda based on an ethnographic and psychometric study by Bolton and Ndogoni (2001). However, the HSCL has not been validated for use among adolescents.
Of most relevance to our work is the 25-item symptom checklist developed by Mutumba et al. (2015b) for use among ALWH in urban Uganda. Our scale differs from theirs in several ways. First, their scale was not validated against a criterion standard (e.g., diagnosis of major depressive disorder). Second, their scale is intended as a general screen for psychosocial distress and includes a range of symptoms like social isolation, somatization, and anxiety that are not specific to depression. Third, their scale was developed and validated among ALWH in Kampala, which is an urban setting that is dominated by the Baganda ethnic group. Our scale was developed and validated in southwestern Uganda, which is a rural setting that is dominated by the Banyankore ethnic group. ALWH in this region have different social networks, economic challenges, and different experiences and expressions of depression. Since the presentation of depression varies across cultures and age groups (Bass, Bolton, & Murray, 2007), we sought to develop, adapt, and validate a depression screening scale for use among ALWH in rural Uganda.
2. Materials and methods
2.1. Study site and participants
We conducted the study from February 2016 to March 2017 in Mbarara District of southwestern Uganda. Mbarara Town is the area’s commercial hub, with a population of 195,013 (Uganda Bureau of statistics, 2014). Most district residents live in rural areas outside of Mbarara Town. Subsistence agriculture, animal husbandry, and local trading are the predominant sources of income, and both food and water insecurity are common (Tsai et al., 2011, Tsai et al., 2016).
We recruited both adult women caregivers/parents and adolescent boys and girls, purposively sampling from several different sites to obtain diverse perspectives on mental health problems faced by HIV-positive and HIV-affected adolescents:
-
a.
Adult women were recruited from the Mbarara Regional Referral Hospital (MRRH) HIV Clinic and the MRRH psychiatric ward where their children were receiving care, and a rural community site (Nyakabare Parish). Although Ugandan men do participate in the rearing of children, most day-to-day care is handled by women (Kipp et al., 2007, Russell and Seeley, 2010, Taylor et al., 1996), therefore only women caregivers were recruited to participate.
-
b.
Adolescent participants were only recruited from the MRRH HIV clinic and the rural community site (Ashaba et al., 2018b, Cooper-Vince et al., 2017). Adolescent participants were not recruited from the MRRH psychiatry ward as most would not have been able to participate fully in the focus group discussions and/or one-on-one in-depth interviews due to current/active mental health issues. All ALWH were fully aware of their seropositivity and were receiving care at the MRRH HIV clinic.
Further details about these adult women caregivers/parents, and adolescent boys and girls, are provided below.
2.2. Focus group discussions and one-on-one interviews
We conducted 5 focus group discussions. In order to elicit diverse perspectives about HIV, mental health, and adolescents, we recruited both caregivers and adolescents, people with various degrees of personal experience with HIV (HIV-positive, HIV-affected, or HIV-negative/HIV-unaffected), and people with various degrees of personal experience with mental health problems.
-
a.
There were three adult women-only focus groups (n = 25). One adult group consisted of women recruited from the MRRH HIV clinic (n = 8) who were primary caregivers of HIV-positive children receiving care in the MRRH HIV clinic. The second adult group involved women (n = 9, serostatus unknown) who were recruited from the MRRH psychiatric ward where their children were receiving mental health care. The third adult group involved women recruited from the community site (n = 8, serostatus unknown) who were caregivers to adolescents aged 13–17 years of age.
-
b.
There were two mixed-gender, adolescent-only focus groups (n = 15) consisting of boys and girls aged 13 to 17 years. One adolescent focus group consisted of participants purposively recruited from the community (2 boys and 5 girls, serostatus unknown). The other adolescent focus group consisted of participants purposively recruited from the MRRH HIV clinic (2 boys and 6 girls, all ALWH).
We conducted 40 one-on-one, in-depth interviews with adolescent boys and girls (n = 10) and with adult women (n = 30). The 10 adolescents included 2 boys (1 from the community whose serostatus was unknown and 1 living with HIV from the MRRH HIV clinic) and 8 girls (4 from the community whose serostatus was unknown and 4 living with HIV from the MRRH HIV clinic). The 30 adult women included 5 recruited from the MRRH HIV clinic and 15 recruited from the MRRH psychiatry ward, where their children were receiving care; and 10 recruited from the community. All women were primary caregivers for children aged 13 to 17 years of age.
Focus group discussions and in-depth interviews were guided by open-ended questions eliciting participants’ perspectives about major stressors facing HIV-positive and HIV-affected adolescents in the community. Open-ended questions were followed by probes to explore the social contexts and consequences of these stressors in the lives of adolescents. Focus group discussions and one-on-one, in-depth interviews were undertaken in the local language (Runyankore), audio recorded, and transcribed directly into English. Two members of the research team read the transcripts concurrently to identify themes relevant to depression.
2.3. Item selection
In developing the scale, we followed the principles described by Krause (2002), starting with focus group discussions and one-on-one, in-depth interviews to identify constructs for potential inclusion in the intended depression scale. We identified constructs from the qualitative interviews to include in the initial item pool using the process described by Kostick, Schensul, Singh, Pelto, and Saggurti (2011). For example, if a participant mentioned thinking too much or having too many thoughts while describing a narrative about depression or life stress, we added “having too many thoughts” as a potential scale item. Constructs identified from the qualitative data included: being desperate, loss of hope, self-hatred, weight loss, loneliness, anger, uselessness, lack of confidence, forgetfulness, having too many thoughts, lack of peace, frustration with life, feeling stressed, and suicidal thoughts. We incorporated additional items from the BDI-II (Beck, Steer, & Brown, 1996) and the HSCL (Bolton et al., 2004; Derogatis & Fitzpatrick, 2004b) based on their similarity to constructs identified in the qualitative data. From the HSCL we included the following items, fearful, fidgety, worthlessness, hopelessness, loneliness, self-blame, loss of interest in things, low energy and not caring about one’s own health. From the BDI-II we included sadness, feeling like a failure, loss of pleasure, guilt, self-dislike, self-blame, crying easily, pessimism, feelings of being punished, being self-critical, agitation, change in sleeping patterns, changes in weight, and loss of interest in sex.
We then reviewed and compared items from the BDI-II and the HSCL with the new constructs (identified in the focus group discussions and one-on-one in-depth interviews) to check for conceptual overlap. Eight items generated from the qualitative data had no overlap with any of the BDI-II or HSCL items: anger, being desperate, lack of confidence, self-hatred, having too many thoughts, lack of peace, frustration with life, and feeling stressed. In case of overlap, the items that could easily be translated to the local language (Runyankore) were retained, while items that were not culturally appropriate were either dropped or adapted. For example, “loss of interest in sex” was replaced with “loss of interest in girls/boys of your age,” a more age-appropriate item in this cultural context (Biddlecom, Awusabo-Asare, & Bankole, 2009). Similarly, “feelings of being punished” was replaced with “feelings of being punished by God,” given prevailing norms about religiosity and spirituality in the local context (Mugisha, Hjelmeland, Kinyanda, & Knizek, 2013). Altogether, the initial item pool included 40 items that covered a wide range of cognitive, affective, and somatic symptoms of depression.
2.4. Translation
The 40 items were translated into the local language (Runyankore) and reviewed by a Runyankore-speaking psychiatrist. The translation process ensured that the original meaning of the items was maintained and checked for consistency to ensure that local expressions of depressive symptoms were appropriately conveyed. Items were then back-translated to English to verify that they were conceptually equivalent to the source (Flaherty et al., 1988).
2.5. Expert review
The 40 items were reviewed by a team of mental health professionals, including a licensed Ugandan psychiatrist, a Ugandan counselling psychologist, and a Ugandan diploma-level psychiatric clinical officer, along with input from key Ugandan informants, all fluent in Runyankore and English. These were assisted by two international mental health experts. The review team discussed translations to ensure validity in the cultural context and reviewed items for consistency, overlap, ambiguity in relation to the local dialect, and overall meaning. When items were found to have similar meanings, the most appropriate item was retained. For example, the terms “pessimistic” and “hopeless” have a similar conceptual meaning when translated to Runyankore (okuhurira nk’oteine matsiko omu by’omumeisho), so “pessimistic” was dropped, and “hopeless” was retained. Similarly, “fidgety” and “fearful” could not be differentiated in Runyakore (okuhurira otinire), so the item “fidgety” was dropped, and “fearful” was retained. These modifications narrowed the initial item pool to 36 items.
2.6. Pilot testing
The pool of 36 items was pilot tested in a purposive sample of 35 ALWH (9 boys, 26 girls) recruited from the MRRH HIV clinic and 15 adolescents (3 boys, 12 girls) of unknown serostatus recruited from the community. Each scale item was scored on a 4-point Likert-type scale (0–3): not at all, much of the time, most of the time, all the time. The study participants’ comments were recorded, and the items were re-reviewed. After the pilot survey, the item about feeling stressed was dropped: the respondents found it ambiguous because it could mean either “being overwhelmed with challenges” or “thinking too much”. The remaining 35 items were retained for administration to the validation sample.
2.7. Reliability and validity testing procedures
The psychometric properties of the depression scale were evaluated using a consecutive sample of 224 ALWH aged 13–17 years recruited from the MRRH HIV clinic. We excluded adolescents who were not fully aware of their HIV status, even if they were in HIV care and/or were being administered antiretroviral medications; those who were not physically strong enough to remain present for the duration of the interview; and those who had difficulty fully understanding the interview questions due to cognitive impairments, as assessed clinically in consultation with a licensed Ugandan psychiatrist.
To evaluate inter-rater reliability of the depression scale, the first 30 participants were re-interviewed by a different research assistant within 2 h of the first administration of the survey. To determine test-retest reliability, 60 participants who lived within 5 km of the HIV clinic were requested to return within a period of 2 weeks to be re-interviewed by the same research assistant. A shorter test-retest period would have been preferable, but most clinic patients lived in rural areas and would have had difficulty returning to the clinic within a short period of time even if given a transportation reimbursement; therefore, we permitted retest participants to return to the clinic within a longer time window of 2 weeks.
To determine criterion-related validity, the criterion standard was a diagnosis of major depressive disorder consistent with the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition. Depression diagnoses were based on the Mini-International Neuropsychiatric Interview for Children and Adolescents (MINI-KID) (Hergueta et al., 1998, Sheehan et al., 2010). The MINI-KID has previously been adapted to obtain valid diagnoses of mental disorders in the Ugandan context (Idro et al., 2016, Kinyanda et al., 2013, Nalugya-Sserunjogi et al., 2016, Okello et al., 2007) and was translated into Runyankore for the purposes of our study. The MINI-KID was administered in a separate room by a diploma-level Ugandan psychiatric clinical officer who was blinded to the study participant’s responses to the rest of the survey.
2.8. Data analysis
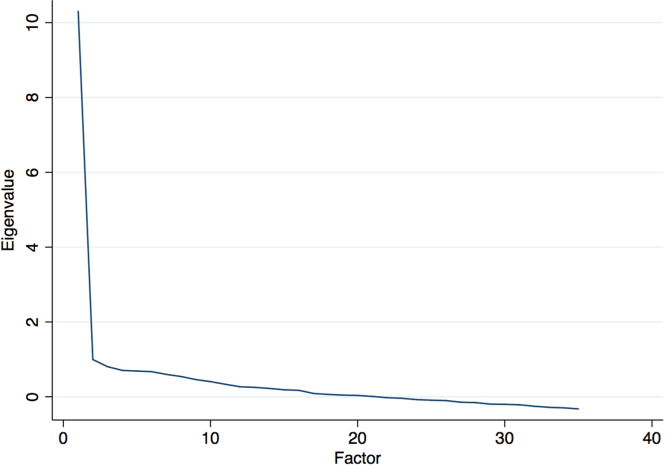
We conducted exploratory factor analysis using principal components with promax rotation to assess the factor structure of the depression scale and to potentially reduce the 35-item pool to a smaller number of items (Costello & Osborne, 2005). Any identified factors were retained based on three criteria. First, we scrutinized factors with eigenvalues ≥ 1.0. Second, the eigenvalues were plotted in descending order to identify the scree, i.e., the portion of the graph where the slope of decreasing eigenvalues approaches zero. Third, the factor loadings were examined, and an item was assigned to a factor if its factor loading was ≥ 0.40 (Floyd & Widaman, 1995). We measured the internal consistency of any retained factors using Cronbach’s alpha.
To estimate inter-rater and test–retest reliability, we calculated the correlation between the two values using the Spearman rank correlation coefficient. To estimate construct validity, we used Spearman’s rank correlation coefficient to calculate the correlation between the depression scores and two variables that have been linked with depression in numerous studies of persons with HIV: stigma and bullying (Ashaba et al., 2018a, Kim et al., 2015, Vreeman et al., 2017). We measured HIV stigma using the Internalized AIDS-Related Stigma Scale (IARSS), a six-item scale designed to measure internalized stigma. The IARSS was developed for use among a sample of people living with HIV from the United States, South Africa and Swaziland (Kalichman et al., 2009) and has been validated for use in the Ugandan context (Tsai et al., 2013b). In the present study, the internalized stigma scale also showed good reliability (Cronbach’s alpha = 0.75). We measured bullying using the nine-item Social and Health Assessment Peer Victimization Scale, which elicits experiences of bullying in the past year (Ruchkin, Schwab-Stone, & Vermeiren, 2004). The scale was adapted from the Multidimensional Peer Victimization Scale and showed excellent reliability (Cronbach’s alpha = 0.82) among adolescents in the United Kingdom (Mynard & Joseph, 2000) and in studies conducted among black South African children and adolescents (Cronbach’s alpha = 0.81) (Cluver et al., 2010). In the present study, the bullying scale also showed good reliability (Cronbach’s alpha = 0.81).
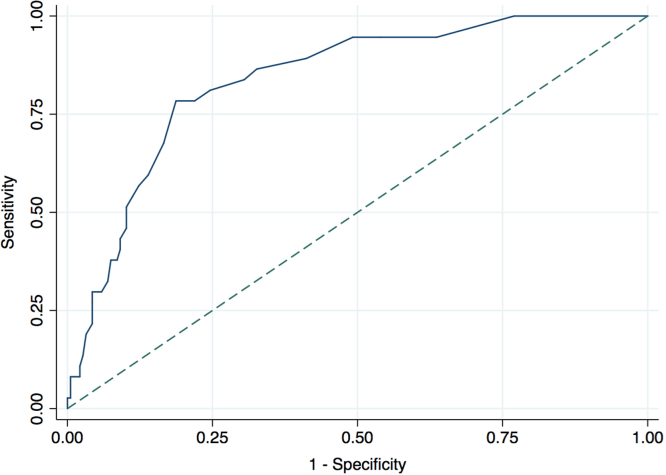
To estimate criterion-related validity, we compared the depression scale measurements with diagnoses of major depressive disorder per the MINI-KID. We analyzed the receiver-operator characteristic (ROC) curve to estimate sensitivity and specificity at different depression scores. We identified the optimal cut-off score as the point in the ROC curve that maximized Youden’s Index, or the point on the curve farthest from chance (and which has been defined as the accuracy of a test in clinical epidemiology) (Kraemer, 1992). All analyses were conducted in Stata version 13 (StataCorp LP, College Station, Texas).
2.9. Ethics
We interviewed participants after obtaining consent and/or assent. For adolescents who were under the care of their parents/guardians, written informed consent was obtained from the parents and assent was obtained from the adolescents. Emancipated minors, and adolescents who were responsible for managing their own HIV care per report of the HIV care provider, were permitted to provide written informed consent without involvement of their parents/guardians. Research assistants read the consent forms to the participants in Runyankore, and participants were given a chance to ask questions for clarification before consenting. Participants received 10,000 Ugandan shillings (approximately 3 U.S. dollars at the time of the study) to cover transportation costs. Research assistants received training in interviewing techniques, mental health literacy, and how to elicit sensitive information. Adolescents found to be in acute psychological distress were referred to the MRRH department of psychiatry for appropriate care. We received ethical approval for our study from the Research Ethics Committee, Mbarara University of Science and Technology; and the Partners Human Research Committee, Massachusetts General Hospital. Consistent with national guidelines, we also received clearance for the study from the Uganda National Council for Science and Technology and from the Research Secretariat in the Office of the President.
3. Results
The validation sample consisted of 131 (58%) girls, and the mean age was 14.9 years (standard deviation [SD], 1.4). There were 48 (21%) orphans. The mean duration on antiretroviral treatment was 8.4 years (SD, 4.4). The sociodemographic characteristics of the validation sample are summarized in Table 1.
Table 1.
Summary statistics (N = 224).
| Characteristics | Mean (SD) or N (%) |
|---|---|
| Age | 14.9 (1.4) |
| Duration on ART (years) | 8.4 (4.4) |
| Distance from the clinic (km) | 29.8 (30) |
| Sex | |
| Female | 131 (58%) |
| Male | 93 (42%) |
| Education | |
| Some primary | 38 (17%) |
| Completed primary | 117 (52%) |
| More than primary | 69 (31%) |
| Orphan | |
| Yes | 48 (21%) |
| No | 176 (79%) |
| Type of school | |
| Day | 149 (67%) |
| Boarding | 75 (33%) |
| Type of caregiver | |
| Both parents | 60 (27%) |
| Mother alone | 79 (35%) |
| Father alone | 22 (10%) |
| Other | 63 (28%) |
| Serostatus of the caregiver | |
| Positive | 145 (65%) |
| Negative | 28 (13%) |
| Unknown | 51 (23%) |
| Bullying | |
| Yes | 97 (43%) |
| No | 127 (57%) |
| Internalized stigma | |
| Yes | 91 (41%) |
| No | 133 (59%) |
| Suicidality risk | |
| None | 193 (86%) |
| Low | 9 (4%) |
| Medium | 13 (6%) |
| High | 9 (4%) |
| Major depressive disorder | |
| Yes | 37 (17%) |
| No | 187 (83%) |
Exploratory factor analysis revealed one factor with an eigenvalue of 10.3 that explained 67 percent of the variance. Eleven items loaded heavily on this factor, with factor loadings ranging from 0.40 to 0.68. These items correspond to well-known affective symptoms of depression. The affective symptoms subscale was internally consistent, with a Cronbach’s alpha of 0.85. The second factor had an eigenvalue of 1.0 and explained 6.5 percent of the variance. Nine items loaded heavily on this factor, with factor loadings ranging from 0.41 to 0.82. These items correspond to well-known cognitive symptoms of depression. The cognitive symptoms subscale was also internally consistent, with a Cronbach’s alpha of 0.85 (Table 2). Visual examination of the scree plot confirmed the two-factor structure (Fig. 1). The remaining 15 scale items did not load substantively on either of the two retained factors.
Table 2.
Two-factor structure of the depression scale.
| Factor 1 (affective) | Factor 2 (cognitive) |
|---|---|
| Felt sad | Disliked my self |
| Kuhurira enaku | Kuhurira otarikwekunda |
| Felt a failure | Had no interest in people/activities |
| Kuremererwa omuri burikimwe | Kuhurira otarikufa aha bantu/emirimo |
| Felt guilty | Felt worthless |
| Kuhurira nohemuka ahamutima | Kuhurira nk’oribusha |
| Had suicidal thoughts | Had difficulty in concentration |
| Kugira ebiteekateeko by’okweyita | Okugumirwa kuta omutima ahaby’orikukora |
| Had difficulty making decisions | Hopeless about the future |
| Kikugumirwa okusharamu eby’okukora | Kuhurira oteine matsiko omu by’omumeisho |
| Felt low in energy | Felt desperate |
| Kwehurira oine amaani makye | Kuhurira nk’oyehwiireho |
| Felt fearful | Felt useless |
| Kuhurira oine okutiina | Kuhurira nk’oteine mugasho |
| Felt lonely | Felt frustrated |
| Kuhurira nk’ori wenka | Kuhurira oteganisiibwe |
| Had no peace | Had no confidence in myself |
| Kubura obusingye | Kubura kweyikiririzamu nk’omuntu |
| Had many thoughts | |
| Kugira ebiteekateeko byingi | |
| Felt tired | |
| Kuhurira oruhire |
Fig. 1.
Scree. The graph shows the eigenvalues of the identified factors, in declining order of magnitude. As is shown in the figure, the eigenvalue was largest for factor 1, followed by a steep decline for factor 2.
The 20-item depression scale consisting of these two factors showed excellent internal consistency, with a Cronbach’s alpha of 0.91. With each item scored on a 4-point Likert-type scale (0–3), the lowest possible total score was 0 and the maximum possible total score was 60. In our sample, the range of values was 0–43. The average depression score in the validation sample was 7.8 (SD, 9.4). The level of depression symptom severity was 7.5 among boys and 8.1 among girls (t = 0.40; P = 0.69).
Among the first 30 participants who were re-interviewed by a different research assistant within 2 h of the initial survey, we estimated a statistically significant correlation between the two values (Spearman’s rho = 0.85; P< 0.001). Among the 60 participants who were re-interviewed within 2 weeks, we estimated a statistically significant correlation between the two values (Spearman’s rho = 0.44; P< 0.001). Depression scores were closely correlated with variables hypothesized to be correlated with depression, including stigma (Spearman’s rho = 0.30; P< 0.001) and bullying (Spearman’s rho = 0.40; P< 0.001), providing strong evidence of construct validity.
On the criterion standard, 37 (17%) study participants were diagnosed with major depressive disorder using the MINI-KID. Comparing the depression scale values to the MINI-KID diagnoses, the area under ROC curve was 0.84 (95% confidence interval [CI], 0.77–0.90), indicating a strong ability to discriminate between cases and non-cases (Fig. 2). The depression score threshold that maximized Youden’s Index was ≥ 10. At this cutoff point, the depression scale had a specificity of 0.81 (95% CI, 0.76–0.87) and sensitivity of 0.78 (95% CI, 0.65–0.92) for detecting major depressive disorder, with a positive likelihood ratio of 4.2, a negative likelihood ratio of 0.27, a positive predictive value of 0.45, and a negative predictive value of 0.94. Also at this cutoff point, 64 (29%) participants screened positive for probable depression.
Fig. 2.
Receiver operating characteristic curve. The graph shows the diagnostic ability of the depression scale as the discrimination threshold is varied. The point on the graph that maximizes the sum of sensitivity and specificity (Youden's Index) corresponds to a total depression score threshold of ≥ 10.
4. Discussion
We developed and validated a 20-item depression scale for ALWH in rural Uganda using a mixed methods study. A two-factor structure emerged, capturing well-known affective and cognitive symptoms of depression, consistent with previous research (Grothe et al., 2005). The study procedures provided adequate evidence of internal consistency, test-retest and inter-rater reliability, and construct and criterion-related validity. Given the paucity of research in this area, this new depression scale is one of the few validated depression scales for use among ALWH in sub Saharan Africa (Betancourt et al., 2012, Binagwaho et al., 2016, Kim et al., 2014b). Strengths of this study in relation to previously published work include our use of qualitative methods to generate potential scale items, as well as our use of structured diagnostic interviews to generate standardized diagnoses of major depressive disorder to serve as the criterion standard. Of the existing scale development studies in the literature on African youth, few have assessed criterion-related validity (Betancourt et al., 2012, Binagwaho et al., 2016, Mutumba et al., 2015b).
The psychological distress scale by Mutumba et al. (2015b), although validated among ALWH in Uganda, is a multidimensional scale capturing depressive, anxiety, and somatic symptoms that are not all specific to depression (Derogatis & Fitzpatrick, 2004a; Mutumba et al., 2015b). Their scale was developed and validated among ALWH in Kampala, which is more urban and is dominated by the Baganda ethnic group – in contrast to southwestern Uganda, the site of our study, which is dominated by the Banyankore ethnic group. The predominantly rural-dwelling ALWH in our study experience different challenges shaped by the environment, such as those related to subsistence agriculture and food/water insecurity, and have different social network structures that may shape their experience and expression of depression (Hove et al., 2013, Raymond and Zolnikov, 2018). Consistent with these arguments, an increased risk of psychological disorders has been reported among HIV-affected children and adolescents in rural settings compared to urban settings (Nabunya and Ssewamala, 2014, Nyamukapa et al., 2010).
A significant strength of our study is the use of qualitative methods to generate items relevant to the local context instead of validating a scale developed elsewhere. This design aspect enabled us to identify expressions of depression from the local context. One of the new items, “having many thoughts” is similar to other findings from studies in central Uganda (Nakimuli-Mpungu et al., 2012, Okello and Ekblad, 2006) in which adult participants have described depression as an illness of many thoughts. Notably, “thinking too much” is an idiom of distress that has been described in many settings worldwide (Kaiser et al., 2015). Out of the final 20 items on the new scale, six items were derived from the qualitative interviews with no overlap from existing scales. The remaining 14 items were adapted from the BDI-II and the HSCL. However, other items (e.g. changes in sleeping patterns, appetite, and/or sexual interest) were dropped from the scale, a notable departure from studies showing that the presentation of depression among adults with HIV has a strong somatic component (Ashaba et al., 2017, Ashaba et al., 2018b, Psaros et al., 2015). These findings contribute to existing literature showing that the presentation of depression varies across age groups and cultures (Bass et al., 2007) and underscores previous emphasis on the need to validate mental health screening scales to fit the local context before use (Betancourt et al., 2012).
Our new 20-item scale showed adequate reliability and validity. Internal consistency was excellent, as indicated by the Cronbach’s alpha of 0.91 (see Supplementary appendix). Evidence of test-retest and inter-rater reliability was obtained by strong correlations of scale values obtained by different raters and by the same raters at different time points. Scale values correlated strongly with other constructs hypothesized to be related to depression among ALWH, including stigma (Cluver et al., 2008; Mutumba et al., 2015a; Tsai et al., 2013a; Tsai et al., 2012) and bullying (Boyes et al., 2014, Boyes and Cluver, 2015; Cluver et al., 2010; Pantelic, Boyes, Cluver, & Meinck, 2017), thereby providing evidence of construct validity. We did not assess discriminant validity, as was done by Mutumba et al. (2015b), who correlated their psychological distress scale with several measures of happiness and general wellbeing. Finally, in an advance on most studies in this literature, we were able to estimate criterion-related validity by comparing the scale values to a criterion standard. Consistent with the meta-analysis of Tsai (2014), the prevalence of probable depression screens exceeded the prevalence of major depressive disorder by a factor of two.
Several limitations should be taken into consideration when interpreting our results. First, the scale was validated using a consecutive sample of ALWH attending a single HIV clinic in rural Uganda. Our findings may not necessarily generalize to ALWH in other HIV clinics throughout Uganda. However, the MRRH HIV clinic has a wide catchment area that spans southwestern Uganda and includes parts of Rwanda and the Democratic Republic of the Congo. We do not claim that our findings generalize to ALWH in these other countries, but the wide catchment area of the MRRH HIV clinic does speak to the fact that our findings likely generalize beyond the narrow geographic scope of Mbarara. Secondly, although we did elicit perspectives from adolescents and caregivers of unknown serostatus, the validation sample consisted only of ALWH. Thus, the scale may not be suitable for use among adolescents in the general population.
5. Conclusion
We have developed and validated a 20-item depression scale for ALWH in Uganda with good psychometric properties. The items in the scale represent well known affective and cognitive symptoms of depression. As such, it may provide opportunities for accurately screening for depressive symptoms among ALWH, potentially improving mental health, HIV treatment adherence, and health outcomes.
Acknowledgement
We acknowledge Ben Jimmy Forry, Badru Kayongo, Patricia Tushemereirwe and Rose Kyarisiima for their assistance with data collection, study administration, and infrastructure development; and Novatus Nyemara, Allen Kiconco, Patrick Gumisiriza and Elizabeth Namara for conducting the qualitative interviews and for their assistance with translation and survey review.
Acknowledgments
Competing interests
The authors have no competing interests to declare.
Funding
The authors acknowledge the funders; the U.S. National Institutes of Health (Fogarty International Center, National Institute of Mental Health, National Institute of Neurological Disorders and Stroke) under award D43TW010128 and Africa Development Bank (ADB). Dr. Tsai acknowledges salary and infrastructure support through NIH R01MH113494 and Dr. Cooper-Vince also acknowledges salary support through T32MH093310.
Ethics statement
The study received ethical approval from the Research Ethics Committee of Mbarara University of Science and Technology; and the Partners Human Research Committee, Massachusetts General Hospital. Written informed consent was obtained from the parents and assent was obtained from the adolescents.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2018.100332.
Appendix A. Supplementary material
Supplementary materials
References
- Ashaba S., Cooper-Vince C., Maling S., Rukundo G., Akena D., Tsai A. Internalized HIV stigma, bullying, major depressive disorder, and high-risk suicidality among HIV-positive adolescents in rural Uganda. Global Mental Health. 2018;5:e22. doi: 10.1017/gmh.2018.15. (page 1 -10) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashaba S., Kaida A., Burns B.F., ONeil K., Dunkley E., Psaros C. Understanding coping strategies during pregnancy and the postpartum period: A qualitative study of women living with HIV in rural Uganda. BMC Pregnancy and Childbirth. 2017;17:138. doi: 10.1186/s12884-017-1321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashaba S., Kakuhikire B., Vořechovská D., Perkins J.M., Cooper-Vince C.E., Maling S. Reliability, validity, and factor structure of the Hopkins symptom checklist-25: Population-based study of persons living with HIV in rural Uganda. AIDS and Behavior. 2018;22:1467–1474. doi: 10.1007/s10461-017-1843-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bass J.K., Bolton P.A., Murray L.K. Do not forget culture when studying mental health. The Lancet. 2007;370:918–919. doi: 10.1016/S0140-6736(07)61426-3. [DOI] [PubMed] [Google Scholar]
- Beck A.T., Steer R.A., Brown G.K. Psychological Corporation; San Antonio, TX: 1996. Beck Depression Inventory-II (BDI-II) [Google Scholar]
- Betancourt T., Scorza P., Kanyanganzi F., Fawzi M.C., Sezibera V., Cyamatare F. HIV and child mental health: A case-control study in Rwanda. Pediatrics. 2014;134:e464–e472. doi: 10.1542/peds.2013-2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt T., Scorza P., Meyers-Ohki S., Mushashi C., Kayiteshonga Y., Binagwaho A. Validating the center for epidemiological studies depression scale for children in Rwanda. Journal of the American Academy of Child Adolescent Psychiatry. 2012;51:1284–1292. doi: 10.1016/j.jaac.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biddlecom A., Awusabo-Asare K., Bankole A. Role of parents in adolescent sexual activity and contraceptive use in four African countries. International Perspectives on Sexual and Reproductive health. 2009;35:72–81. doi: 10.1363/ipsrh.35.072.09. [DOI] [PubMed] [Google Scholar]
- Binagwaho A., Fawzi M.C.S., Agbonyitor M., Nsanzimana S., Karema C., Remera E. Validating the Children’s Depression Inventory in the context of Rwanda. BMC Pediatrics. 2016;16:29. doi: 10.1186/s12887-016-0565-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton, & Ndogoni (2001). Cross-cultural assessment of trauma-related mental illness (Phase II): a report of research conducted by World Vision Uganda and The Johns Hopkins University.
- Bolton Wilk, Ndogoni Assessment of depression prevalence in rural Uganda using symptom and function criteria. Social Psychiatry and Psychiatric Epidemiology. 2004;39:442–447. doi: 10.1007/s00127-004-0763-3. [DOI] [PubMed] [Google Scholar]
- Boyes M.E., Bowes L., Cluver L.D., Ward C.L., Badcock N.A. Bullying victimisation, internalising symptoms, and conduct problems in South African children and adolescents: A longitudinal investigation. Journal of Abnormal Child Psychology. 2014;42:1313–1324. doi: 10.1007/s10802-014-9888-3. [DOI] [PubMed] [Google Scholar]
- Boyes M.E., Cluver L.D. Relationships between familial HIV/AIDS and symptoms of anxiety and depression: The mediating effect of bullying victimization in a prospective sample of South African children and adolescents. Journal of Youth and Adolescence. 2015;44:847–859. doi: 10.1007/s10964-014-0146-3. [DOI] [PubMed] [Google Scholar]
- Cluver Bowes, Gardner Risk and protective factors for bullying victimization among AIDS-affected and vulnerable children in South Africa. Child Abuse Neglect. 2010;34:793. doi: 10.1016/j.chiabu.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Cluver Gardner, Operario Effects of stigma on the mental health of adolescents orphaned by AIDS. Journal of Adolescent Health. 2008;42:410–417. doi: 10.1016/j.jadohealth.2007.09.022. [DOI] [PubMed] [Google Scholar]
- Cooper-Vince C., Kakuhikire B., Vořechovská D., McDonough A., Perkins J., Venkataramani A. Household water insecurity, missed schooling, and the mediating role of caregiver depression in rural Uganda. Global Mental Health. 2017;4 doi: 10.1017/gmh.2017.14. (e15-e15) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello A.B., Osborne J.W. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment, Research Evaluation. 2005;10:1–9. [Google Scholar]
- Derogatis, & Fitzpatrick (2004a). The SCL-90-R, the Brief Symptom Inventory (BSI), and the BSI-18.
- Derogatis, & Fitzpatrick . The SCL-90-R, the Brief Symptom Inventory (BSI), and the BSI-18. In: Maruish M.E., editor. The use of psychological testing for treatment planning and outcomes assessment: Instruments for adults. Lawrence Erlbaum Associates Publishers; Mahwah, NJ, US: 2004. pp. 1–41. [Google Scholar]
- Dick B., Ferguson B.J. Health for the world’s adolescents: A second chance in the second decade. Journal of Adolescent Health. 2015;56:3–6. doi: 10.1016/j.jadohealth.2014.10.260. [DOI] [PubMed] [Google Scholar]
- Dow D.E., Turner E.L., Shayo A.M., Mmbaga B., Cunningham C.K., O’Donnell K. Evaluating mental health difficulties and associated outcomes among HIV-positive adolescents in Tanzania. AIDS Care. 2016;28:825–833. doi: 10.1080/09540121.2016.1139043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flaherty J.A., Gaviria F.M., Pathak D., Mitchell T., Wintrob R., Richman J.A. Developing instruments for cross-cultural psychiatric research. The Journal of Nervous and Mental Disease. 1988;176:260–263. [PubMed] [Google Scholar]
- Floyd F.J., Widaman K.F. Factor analysis in the development and refinement of clinical assessment instruments. Psychological Assessment. 1995;7:286. [Google Scholar]
- Grothe K.B., Dutton G.R., Jones G.N., Bodenlos J., Ancona M., Brantley P.J. Validation of the Beck Depression Inventory-II in a low-income African American sample of medical outpatients. Psychological Assessment. 2005;17:110. doi: 10.1037/1040-3590.17.1.110. [DOI] [PubMed] [Google Scholar]
- Hergueta T., Baker R., Dunbar G.C. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IVand ICD-10. Journal of Clinical Psychiatry. 1998;59:2233. [PubMed] [Google Scholar]
- Hove M., Ngwerume E., Muchemwa C. The urban crisis in Sub-Saharan Africa: A threat to human security and sustainable development. Stability: International Journal of Security and Development. 2013;2(1):1–14. (7) [Google Scholar]
- Idro R., Kakooza-Mwesige A., Asea B., Ssebyala K., Bangirana P., Opoka R.O. Cerebral malaria is associated with long-term mental health disorders: A cross sectional survey of a long-term cohort. Malaria Journal. 2016;15:184. doi: 10.1186/s12936-016-1233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaida A., Matthews L.T., Ashaba S., Tsai A.C., Kanters S., Robak M. Depression during pregnancy and the postpartum among HIV-infected women on antiretroviral therapy in Uganda. Journal of Acquired Ammune Deficiency Syndromes (1999) 2014;67:S179. doi: 10.1097/QAI.0000000000000370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser B.N., Haroz E.E., Kohrt B.A., Bolton P.A., Bass J.K., Hinton D.E. “Thinking too much”: A systematic review of a common idiom of distress. Social Science Medicine. 2015;147:170–183. doi: 10.1016/j.socscimed.2015.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman S.C., Simbayi L.C., Cloete A., Mthembu P.P., Mkhonta R.N., Ginindza T. Measuring AIDS stigmas in people living with HIV/AIDS: The Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21:87–93. doi: 10.1080/09540120802032627. [DOI] [PubMed] [Google Scholar]
- Kamau J.W., Kuria W., Mathai M., Atwoli L., Kangethe R. Psychiatric morbidity among HIV-infected children and adolescents in a resource-poor Kenyan urban community. AIDS Care. 2012;24:836–842. doi: 10.1080/09540121.2011.644234. [DOI] [PubMed] [Google Scholar]
- Kim, Mazenga A.C., Devandra A., Ahmed S., Kazembe P., Yu X. Prevalence of depression and validation of the Beck Depression Inventory-II and the Children’s Depression Inventory-Short amongst HIV-positive adolescents in Malawi. Journal of the International AIDS Society. 2014;17 doi: 10.7448/IAS.17.1.18965. (18965-18965) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, Mazenga A.C., Devandra A., Ahmed S., Yu X., Kazembe P.N. Prevalence of depression and validation of the Beck Depression Inventory-II and the Children’s Depression Inventory-Short amongst HIV-positive adolescents in Malawi. Journal of the International AIDS Society. 2014;17 doi: 10.7448/IAS.17.1.18965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M., Mazenga A., Yu X., Devandra A., Nguyen C., Ahmed S. Factors associated with depression among adolescents living with HIV in Malawi. BMC Psychiatry. 2015;15 doi: 10.1186/s12888-015-0649-9. (264-264) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinyanda E., Kizza R., Abbo C., Ndyanabangi S., Levin J. Prevalence and risk factors of depression in childhood and adolescence as seen in 4 districts of north-eastern Uganda. BMC International Health and Human Rights. 2013;13:19. doi: 10.1186/1472-698X-13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kipp W., Tindyebwa D., Rubaale T., Karamagi E., Bajenja E. Family caregivers in rural Uganda: The hidden reality. Health Care for Women International. 2007;28:856–871. doi: 10.1080/07399330701615275. [DOI] [PubMed] [Google Scholar]
- Kostick K.M., Schensul S.L., Singh R., Pelto P., Saggurti N. A methodology for building culture and gender norms into intervention: An example from Mumbai, India. Social Science Medicine. 2011;72:1630–1638. doi: 10.1016/j.socscimed.2011.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer H.C. Sage publications Newbury Park; CA: 1992. Evaluating medical tests: Objective and quantitative guidelines. [Google Scholar]
- Krause N. A comprehensive strategy for developing closed-ended survey items for use in studies of older adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2002;57:S263–S274. doi: 10.1093/geronb/57.5.s263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester, Chesney M., Cooke M., Weiss R., Whalley P., Perez B. When the time comes to talk about HIV: Factors associated with diagnostic disclosure and emotional distress in HIV-infected children. Journal of Acquired Immune Deficiency Syndromes (1999) 2002;31:309–317. doi: 10.1097/00126334-200211010-00006. [DOI] [PubMed] [Google Scholar]
- Lowenthal E.D., Marukutira T., Tshume O., Chapman J., Anabwani G.M., Gross R. Prediction of HIV virologic failure among adolescents using the Pediatric Symptom Checklist. AIDS and Behavior. 2015;19:2044–2048. doi: 10.1007/s10461-015-1061-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez P., Andia I., Emenyonu N., Hahn J.A., Hauff E., Pepper L. Alcohol use, depressive symptoms and the receipt of antiretroviral therapy in southwest Uganda. AIDS and Behavior. 2008;12:605–612. doi: 10.1007/s10461-007-9312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugisha J., Hjelmeland H., Kinyanda E., Knizek B.L. Religious views on suicide among the Baganda. Uganda: A qualitative study Death Studies. 2013;37:343–361. doi: 10.1080/07481187.2011.641136. [DOI] [PubMed] [Google Scholar]
- Mutumba M., Bauermeister J.A., Musiime V., Byaruhanga J., Francis K., Snow R.C. Psychosocial challenges and strategies for coping with HIV among adolescents in Uganda: A qualitative study. AIDS Patient Care and STDs. 2015;29:86–94. doi: 10.1089/apc.2014.0222. [DOI] [PubMed] [Google Scholar]
- Mutumba M., Harper G. Mental health and support among young key populations: An ecological approach to understanding and intervention. Journal of the International AIDS Society. 2015;18 doi: 10.7448/IAS.18.2.19429. (19429-19429) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutumba M., Musiime V., Lepkwoski J.M., Harper G.W., Snow R.C., Resnicow K. Examining the relationship between psychological distress and adherence to anti-retroviral therapy among Ugandan adolescents living with HIV. AIDS Care. 2016;28:807–815. doi: 10.1080/09540121.2015.1131966. [DOI] [PubMed] [Google Scholar]
- Mutumba M., Resnicow K., Bauermeister J.A., Harper G.W., Musiime V., Snow R.C. Development of a psychosocial distress measure for Ugandan adolescents living with HIV. AIDS and Behavior. 2015;19:380–392. doi: 10.1007/s10461-014-0973-y. [DOI] [PubMed] [Google Scholar]
- Mutumba M., Tomlinson M., Tsai A.C. Psychometric properties of instruments for assessing depression among African youth: A systematic review. Journal of Child Adolescent Mental Health. 2014;26:139–156. doi: 10.2989/17280583.2014.907169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mynard H., Joseph S. Development of the multidimensional peer-victimization scale. Aggressive Behavior. 2000;26:169–178. [Google Scholar]
- Nabunya P., Ssewamala F.M. The Effects of parental loss on the psychosocial wellbeing of AIDS-orphaned children living in AIDS-impacted communities: Does gender matter? Children and Youth Services Review. 2014;43:131–137. doi: 10.1016/j.childyouth.2014.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakimuli-Mpungu E., Mojtabai R., Alexandre P.K., Katabira E., Musisi S., Nachega J.B. Cross-cultural adaptation and validation of the self-reporting questionnaire among HIV+ individuals in a rural ART program in southern Uganda. HIV AIDS. 2012;4:51–60. doi: 10.2147/HIV.S29818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalugya-Sserunjogi J., Rukundo G.Z., Ovuga E., Kiwuwa S.M., Musisi S., Nakimuli-Mpungu E. Prevalence and factors associated with depression symptoms among school-going adolescents in Central Uganda. Child and Adolescent Psychiatry and Mental Health. 2016;10:39. doi: 10.1186/s13034-016-0133-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamukapa C., Gregson S., Wambe M., Mushore P., Lopman B., Mupambireyi Z. Causes and consequences of psychological distress among orphans in eastern Zimbabwe. AIDS Care. 2010;22:988–996. doi: 10.1080/09540121003615061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okello E.S., Ekblad S. Lay concepts of depression among the Baganda of Uganda: A pilot study. Transcultural Psychiatry. 2006;43:287–313. doi: 10.1177/1363461506064871. [DOI] [PubMed] [Google Scholar]
- Okello J., Onen T., Musisi S. Psychiatric disorders among war-abducted and non-abducted adolescents in Gulu district, Uganda: a comparative study. African Journal of Psychiatry. 2007:225–231. doi: 10.4314/ajpsy.v10i4.30260. [DOI] [PubMed] [Google Scholar]
- Pantelic M., Boyes M., Cluver L., Meinck F. HIV, violence, blame and shame: Pathways of risk to internalized HIV stigma among South African adolescents living with HIV. Journal of the International AIDS Society. 2017;20 doi: 10.7448/IAS.20.1.21771. (21771-21771) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Psaros C., Haberer J.E., Boum Y., II, Tsai A.C., Martin J.N., Hunt P.W. The factor structure and presentation of depression among HIV-positive adults in Uganda. AIDS and Behavior. 2015;19:27–33. doi: 10.1007/s10461-014-0796-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond J.M., Zolnikov T.R. AIDS-affected orphans in sub-Saharan Africa: A scoping review on outcome differences in rural and urban environments. AIDS and Behavior. 2018:1–13. doi: 10.1007/s10461-018-2134-1. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus M.J., Weiss R., Alber S., Lester P. Adolescent adjustment before and after HIV-related parental death. Journal of Consulting and Clinical Psychology. 2005;73:221. doi: 10.1037/0022-006X.73.2.221. [DOI] [PubMed] [Google Scholar]
- Rubin A., Gold M., Primack B.A. Associations between depressive symptoms and sexual risk behavior in a diverse sample of female adolescents. Journal of Pediatric and Adolescent Gynecology. 2009;22:306–312. doi: 10.1016/j.jpag.2008.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruchkin V., Schwab-Stone M., Vermeiren R. Yale University; New Haven: 2004. Social and Health Assessment (SAHA): Psychometric development summary. [Google Scholar]
- Russell S., Seeley J. The transition to living with HIV as a chronic condition in rural Uganda: Working to create order and control when on antiretroviral therapy. Social Science Medicine. 2010;70:375–382. doi: 10.1016/j.socscimed.2009.10.039. [DOI] [PubMed] [Google Scholar]
- Saluja G., Iachan R., Scheidt P.C., Overpeck M.D., Sun W., Giedd J.N. Prevalence of and risk factors for depressive symptoms among young adolescents. Archives of Pediatrics Adolescent Medicine. 2004;158:760–765. doi: 10.1001/archpedi.158.8.760. [DOI] [PubMed] [Google Scholar]
- Sheehan D.V., Sheehan K.H., Shytle R.D., Janavs J., Bannon Y., Rogers J.E. Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID) The Journal of Clinical Psychiatry. 2010;71:313–326. doi: 10.4088/JCP.09m05305whi. [DOI] [PubMed] [Google Scholar]
- Stockings E., Degenhardt L., Lee Y.Y., Mihalopoulos C., Liu A., Hobbs M. Symptom screening scales for detecting major depressive disorder in children and adolescents: A systematic review and meta-analysis of reliability, validity and diagnostic utility. Journal of Affective Disorders. 2015;174:447–463. doi: 10.1016/j.jad.2014.11.061. [DOI] [PubMed] [Google Scholar]
- Taylor L., Seeley J., Kajura E. Informal care for illness in rural southwest Uganda: The central role that women play. Health Transition Review. 1996:49–56. [PubMed] [Google Scholar]
- Tinasti K. HIV and AIDS among adolescents who use drugs: Opportunities for drug policy reform within the sustainable development agenda. Journal of the International AIDS Society. 2018;21:e25045. doi: 10.1002/jia2.25045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C. Reliability and validity of depression assessment among persons with HIV in sub-Saharan Africa: Systematic review and meta-analysis. Journal of Acquired Immune Deficiency Syndromes (1999) 2014;66:503. doi: 10.1097/QAI.0000000000000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Bangsberg D.R., Bwana M., Haberer J.E., Frongillo E.A., Muzoora C. How does antiretroviral treatment attenuate the stigma of HIV? Evidence from a cohort study in rural Uganda. AIDS and Behavior. 2013;17:2725–2731. doi: 10.1007/s10461-013-0503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Bangsberg D.R., Emenyonu N., Senkungu J.K., Martin J.N., Weiser S.D. The social context of food insecurity among persons living with HIV/AIDS in rural Uganda. Social Science Medicine. 2011;73:1717–1724. doi: 10.1016/j.socscimed.2011.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Bangsberg D.R., Frongillo E.A., Hunt P.W., Muzoora C., Martin J.N. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Social Science Medicine (1982) 2012;74(12):2012–2019. doi: 10.1016/j.socscimed.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Kakuhikire B., Mushavi R., Vořechovská D., Perkins J.M., McDonough A.Q. Population-based study of intra-household gender differences in water insecurity: Reliability and validity of a survey instrument for use in rural Uganda. Journal of Water and Health. 2016;14:280–292. doi: 10.2166/wh.2015.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Weiser S.D., Petersen M.L., Ragland K., Kushel M.B., Bangsberg D.R. A marginal structural model to estimate the causal effect of antidepressant medication treatment on viral suppression among homeless and marginally housed persons with HIV. Archives of General Psychiatry. 2010;67:1282–1290. doi: 10.1001/archgenpsychiatry.2010.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Weiser S.D., Steward W.T., Mukiibi N.F., Kawuma A., Kembabazi A. Evidence for the reliability and validity of the internalized AIDS-related stigma scale in rural Uganda. AIDS and Behavior. 2013;17:427–433. doi: 10.1007/s10461-012-0281-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uganda Bureau of statistics . Citypopulation; Kamapala: 2014. The population of the regions of the Republic of Uganda and allcities and towns of more than 15,000 inhabitants. [Google Scholar]
- Vreeman R.C., McCoy B.M., Lee S. Mental health challenges among adolescents living with HIV. Journal of the International AIDS Society. 2017;20:21497. doi: 10.7448/IAS.20.4.21497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2008). The global burden of disease: 2004 update. Geneva.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary materials