Abstract
Rationale
Improved birth weight outcomes have been reported for infants of mothers imprisoned during pregnancy relative to similarly disadvantaged mothers, however, findings are equivocal and evidence is lacking from jurisdictions outside the United States.
Objective
To investigate whether maternal imprisonment during pregnancy is a determinant of low birth weight (<2500 g) for Indigenous and non-Indigenous infants in Western Australia.
Methods
A longitudinal sample of 41,910 singleton infants born in Western Australia (October 1985-December 2013), was identified with linked administrative data and examined by five mutually exclusive categories of maternal corrections history; (i) imprisonment in pregnancy, (ii) imprisonment before pregnancy, (iii) first imprisonment after birth, (iv) community-based corrections record without imprisonment at any time, and (v) no corrections record at any time. Univariate and multivariate Poisson regression was performed to determine key risk factors for low birth weight. Prevalence of risk factors were calculated by maternal corrections history.
Results
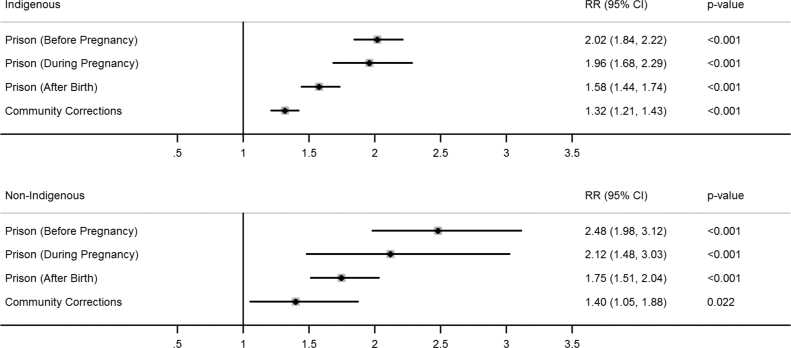
After adjusting for other significant pregnancy risks, maternal imprisonment before (Indigenous RR 2.02, 95%CI 1.84–2.22, p<.001; non-Indigenous RR 2.48, 95%CI 1.98–3.12, p<.001) or during (Indigenous RR 1.96, 95%CI 1.68–2.29, p<.001; non-Indigenous RR 2.12, 95%CI 1.48–3.03, p<.001) pregnancy remained strong determinants of low birth weight, and carried greater risk than imprisonment after birth (Indigenous RR 1.58, 95%CI 1.44–1.74, p<.001; non-Indigenous RR 1.75, 95%CI 1.51–2.04, p<.001) or community-based corrections orders (Indigenous RR 1.32, 95%CI 1.21–1.43, p<.001; non-Indigenous RR 1.40, 95%CI 1.05–1.88, p<.001), relative to no corrections record. Pregnancy risk factors more prevalent amongst infants whose mothers were imprisoned before or during pregnancy included substance-use related service contacts, hospitalisation for injury, mental health service contacts, and having a sibling in contact with the child protection system.
Conclusion
Western Australian infants with mothers imprisoned before or during pregnancy experience elevated risk of low birth weight and exposure to maternal substance use, injury and mental distress in pregnancy.
Keywords: Australia, Low birth weight, Women prisoners, Linked data, Indigenous
1. Introduction
The high level of disadvantage within the women prisoner population is well documented. Women prisoners experience elevated levels of adversity including intimate partner violence, mental health disorders, alcohol and other substance misuse, unemployment, and insecure housing (Knight & Plugge, 2005a). There are, however, comparatively few studies on the perinatal outcomes of women prisoners (Bard, Knight, & Plugge, 2016; Shaw, Downe, & Kingdon, 2014; Knight & Plugge, 2005b).
Birth weight is an important perinatal outcome, with low birth weight potentially representing the product of a suboptimal intrauterine environment (Knight & Plugge, 2005b). A birth weight of less than 2500 g is associated with an increased risk of infant mortality, and of developing health problems in later life including cardiovascular problems and diabetes (McMillen and Robinson, 2005, Xiao et al., 2010, Zhang et al., 2013, Arnold et al., 2015, Hoy and Nicol, 2010, Luyckx et al., 2013, White et al., 2010).
Three systematic reviews (Bard et al., 2016, Shaw et al., 2015, Knight and Plugge, 2005b) have identified five studies (Martin et al., 1997a, Kyei-Aboagye et al., 2000, Terk et al., 1993, Mertens, 2001, Bell et al., 2004), all conducted within the United States, that have compared low birth weight outcomes for infants of mothers imprisoned during pregnancy to disadvantaged and/or general population controls. Together these studies have generally found a reduction in low birth weight for infants whose mothers were imprisoned during pregnancy, compared to similarly disadvantaged controls, suggesting imprisonment may have a beneficial, rather than detrimental effect on perinatal outcomes (Knight & Plugge, 2005b). It has been postulated that maternal imprisonment may improve infant birth weight outcomes through increased access to antenatal care, better nutrition, and reduced exposure to alcohol, drugs and intimate partner violence (Martin et al., 1997a, Kyei-Aboagye et al., 2000). In contrast, the only Australian study to investigate the impact of maternal imprisonment on birth weight did not find a beneficial association between maternal imprisonment and birth weight (Walker, Hilder, Levy, & Sullivan, 2014). It is not clear whether maternal imprisonment has a direct impact on perinatal outcomes, or whether such outcomes are predominantly a consequence of the high level of socioeconomic disadvantage and other adversity experienced by the prisoner population.
In Australia, there is a wide disparity in health and social outcomes for Aboriginal and Torres Strait Islander people, hereafter Indigenous people, resulting from the impacts of colonisation, including land dispossession, forced removal of children from families, and continuing discriminatory policies, practices, and societal attitudes (Council of Australian Governments (COAG), 2009). Despite some improvement, Indigenous infants remain more likely to be born of low birth weight and experience higher rates of chronic disease and shorter life expectancy than non-Indigenous children. Indigenous women are also overrepresented in the prison population. In Western Australia, for example, Indigenous people represent 4% of the general population and 46% of the female prison population (Australian Bureau of Statistics (ABS), 2016, Australian Bureau of Statistics (ABS), 2011). It is therefore important to understand whether maternal imprisonment is a risk factor for poor perinatal outcomes for Indigenous infants.
1.1. Objectives
The primary objective of this study was to determine whether maternal imprisonment during pregnancy is a risk factor for low birth weight for Indigenous and non-Indigenous children.
The specific aims of the study were to determine: (i) the prevalence of low birth weight for Indigenous and non-Indigenous infants of mothers with different corrections histories; (ii) key social, demographic and pregnancy-related risk factors (identifiable from health-related administrative datasets), which may contribute to low birth weight in Indigenous and non-Indigenous populations; (iii) the importance of maternal corrections history as a determinant of low birth weight after accounting for significant social, demographic and pregnancy-related risk factors; and (iv) the prevalence of significant risk factors for low birth weight between infants with different maternal corrections histories.
2. Methods
2.1. Study design and sampling
In the present study we have used data from a large data linkage project to explore determinants of low birth weight within Indigenous and non-Indigenous children of mothers who had been exposed to the corrections system at different times in relation to their pregnancy. We compared the outcomes for infants whose mothers were imprisoned during pregnancy, to groups of infants whose mothers had a history of imprisonment at a time other than during pregnancy, were just exposed to community-based correctional orders, or with no history of contact with corrective services.
The study population was derived from a longitudinal cohort study of all Western Australian children born from 1985 to 2011 whose biological mother was imprisoned within 18-years of their birth, with a randomly sampled comparison group of children whose mothers had no imprisonment record within 18-years after their birth. Three comparison children were sampled for each cohort children and matched on Indigenous status, age and sex. All cohort and comparison group children were liveborn. Data were also obtained on the second-generation children born from 1998 to 2014 to the female members of the cohort and comparison group.
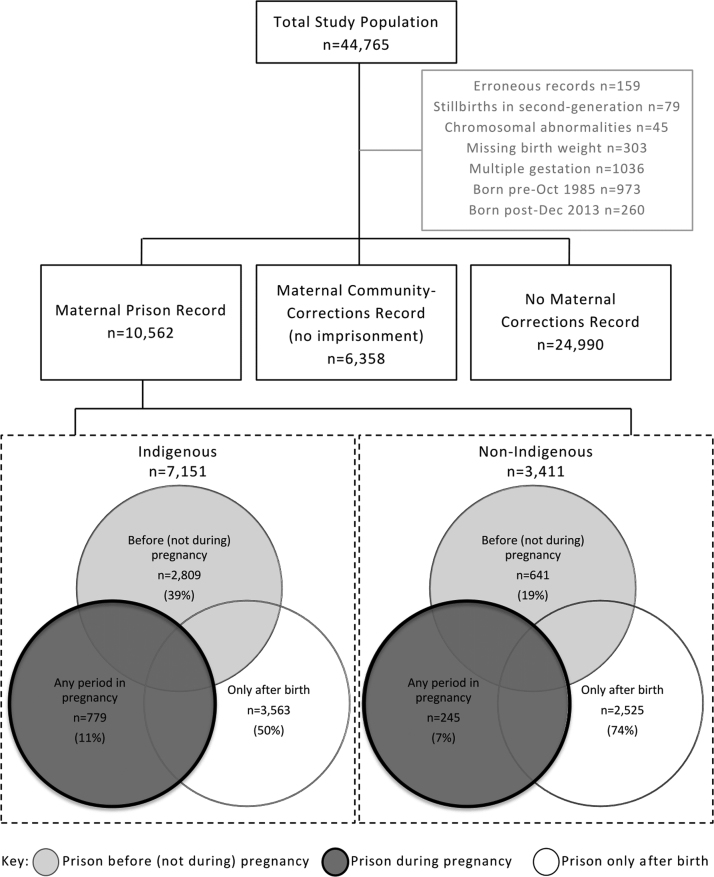
All children with available data, including second-generation children, were included in the total study population (Fig. 1). Children were excluded from the study population if they were stillborn (second-generation only), a multiple gestation pregnancy (twins, triplets, etc.), or diagnosed with a chromosomal abnormality. The study population was limited to children born between October 1985 and December 2013 to ensure nine months of pregnancy data was available for all individuals. In total, there were 41,910 infants in the final study population including 36,557 from the first-generation and 5353 from the second-generation.
Fig. 1.
Selection of the study population and classification by maternal corrections history.
The proportion of infants in the various maternal corrections history sub-groups (shown in Fig. 1), relate only to the study population and do not reflect the prevalence of these groups across the whole Western Australian population.
2.2. Data sources
The Western Australian Data Linkage Branch (WADLB) identified the study population, conducted the data linkage and provided de-identified data extracts to the project researchers through the Western Australian Data Linkage System (WADLS). The WADLS uses highly accurate computerised, probabilistic matching with clerical review to create linkages between administrative data collections across a range of Western Australian government departments and services (Holman, Bass, Rouse, & Hobbs, 1999).
Table 1 outlines the data collections utilised for the present study. These are all statutory State-wide data collections with good coverage of the Western Australian population. Data on birth registrations, midwives records, and child protection system contacts were obtained for all first- and second-generation children. Hospital data was only obtained for first-generation children. Corrections, hospital, and mental health data was obtained for all mothers.
Table 1.
Brief description of data sources.
| Data Collection | Data Coverage |
|---|---|
| Midwives Notifications System (MNS) | Notifications for all births attended by a midwife where the gestational age is at least 20 weeks or infant weight 400 g+ if gestation unknown |
| Birth Registrations | All births registered in Western Australia |
| Department of Corrective Services | All records of adult and juvenile offenders detained in Western Australian prisons, and under departmental supervision on community-based orders |
| Hospital Morbidity Data Collection (HMDC) | All inpatient records for Western Australian public and private acute and psychiatric hospitals |
| Mental Health Information System (MHIS) | All presentations to public community mental health services |
| Department of Communities: Child Protection and Family Support | All reports of concern for child welfare, investigations, protection applications and orders, and placements in out-of-home care |
The Hospital Morbidity Data Collection (HMDC) and Mental Health Information (MHIS) data collections use the International Statistical Classification of Diseases (ICD) (ICD-9-CM to June 1999, ICD-10-AM from July 1999), to classify diagnosis, or reason for health service contact. For hospital records, the principal diagnosis code and up to four codes for external causes of injury, were obtained.
Indigenous status for children and mothers was provided through the Derived Indigenous Status Flag variable generated by the WADLS using best-practice algorithms, which assess individuals’ Indigenous status across numerous data collections to increase accuracy (Christensen et al., 2014).
2.3. Definition of maternal corrections history
The total study population was subdivided based on maternal corrections records (Fig. 1), including infants whose mothers had: a prison record at any time (n=7,151 Indigenous; n=3,411 non-Indigenous); community-based correctional orders but no prison record (n=5,716 Indigenous; n=642 non-Indigenous); and no corrections record (n=12,677 Indigenous; n=12,313 non-Indigenous).
Women with community-based correctional orders are sentenced offenders, but may differ to women given custodial prison sentences based on the severity or frequency of their offending and other individual factors. Community-based sentences may involve treatment or vocational programs, community service, and place restrictions on offenders.
Imprisonment records were for prison stays of any length of time, and included unsentenced remandees detained before trial as well as sentenced prisoners. Infants of mothers who had a prison record at any time over the study period were further subdivided so as to explore the effect of timing of maternal imprisonment on infant birth weight. The first group included infants whose mothers had any record of imprisonment during pregnancy. The second group included infants whose mothers had imprisonment records any time before, but not during, pregnancy. The third group included infants whose mothers first record of imprisonment only occurred after their birth. These main groupings are summarised in Fig. 1 and were based on mother’s prison reception date and the infant’s birth date.
2.4. Definition of low birth weight
Following the World Health Organization (WHO) definition, children in the study population with a birth weight less than 2500 g were classified as being ‘low birth weight’ (WHO, 1992).
2.5. Pregnancy and birth dates
Child month and year of birth was provided by the Midwives Notification System (MNS), or if missing from the Birth Registration data. As gestational age was not obtained, pregnancy start date was calculated as being nine months before the first day of the child’s birth-month.
2.6. Conceptual framework
The Mosley and Chen (1984) framework for the study of child survival was used to identify other important pregnancy risk factors from the available study data. The basis of the framework is that broader determinants necessarily operate through biological pathways or mechanisms, to impact on the healthy development of the fetus. Our adaptation includes four key groups: demographic factors; baseline pregnancy risk factors, which are largely unmodifiable from the commencement of pregnancy; pregnancy complications, that are precursors to poor perinatal outcomes; and other maternal factors and exposures which may indicate maternal vulnerability or household dysfunction.
2.6.1. Demographic characteristics
The Birth Registration and MNS data provides social and demographic characteristics of mothers and children at time of birth, including sex, socioeconomic status (Socio-economic Indexes for Areas Index of Relative Socio-economic Disadvantage), and geographical remoteness (Accessibility/Remoteness Index of Australia). For remoteness, major cities and inner regional areas were combined given both have greater accessibility of relevant services.
2.6.2. Baseline pregnancy risk factors
Maternal birth date was determined using all available data sources and maternal age was calculated as the age of mother at time of birth. Parity and duration of birth spacing were derived using sibling birth dates (Kozuki et al., 2013). Maternal history of abortion was identified from maternal hospital records.
2.6.3. Pregnancy complications
The separate and combined effects of key pregnancy complications (Salihu et al., 2013), identified from maternal hospital records were tested. These complications included hospitalisation during pregnancy for infections, anaemia, diabetes, hypertension, preeclampsia, eclampsia, abruptio placentae, placenta previa, other placental disorders, premature rupture of membranes and renal disorders (see Supplementary Table 1 for relevant ICD-codes). Admissions for hypertension, preeclampsia or eclampsia were combined in a single category, as were admissions for abruptio placentae, placenta previa or other placental disorders. Non-significant factors, including anaemia and diabetes, were not reported.
2.6.4. Other maternal risk factors and exposures
Other risk factors identified included maternal hospital admissions for any injuries from external causes, and mental health related service presentations (identified from HMDC and MHIS), both excluded substance use and poisoning related service contacts. Maternal substance use (including alcohol and poisoning) related service contacts during pregnancy were identified from HMDC and MHIS.
Sibling contact with child protection services during pregnancy was also identified as an indicator of household dysfunction and maternal risk.
2.7. Statistical analysis
All analyses were stratified by infants’ Indigenous status. Statistical analyses were conducted using Stata Version 14.0.
First, prevalence of low birth weight by maternal corrections history, key demographic and pregnancy-related factors (described above) were calculated. Second, univariate analysis was conducted using Poisson regression with robust error variance to estimate the corresponding Relative Risk for individual factors with low birth weight (McNutt et al., 2003, Zou, 2004, Greenland, 2004). Birth year was the only continuous variable, its relationship with low birth weight was assessed using independent-samples t-tests for Indigenous and non-Indigenous infants separately.
Third, the strength of correlation between pairs of all variables of interest was assessed using Chi-square tests with Cramer’s V statistic. For variable pairs with an effect size >0.3 (Cohen, 1988), one variable was excluded from the multivariate analysis as determined on the basis of the univariate Relative Risk and statistical significance (p>0.05) of each variable with low birth weight. Multivariate Poisson regression, with a robust error variance, was performed for each grouping of variables (demographic factors, baseline pregnancy risk factors, pregnancy complications, and other maternal factors/exposures in pregnancy) with low birth weight. Variables that were not associated with low birth weight (as determined by Relative Risk close to 1) and were not statistically significant (p>0.05) were excluded from further analysis. Remaining variables were entered in separate models for Indigenous and non-Indigenous infants using Poisson regression, with robust error variance. A manual backwards elimination approach was used to remove individual variables based on their association with low birth weight as determined by Relative Risk (close to null) and statistical significance (p>0.05), and Goodness-of-Fit as determined by Akaike Information Criterion (AIC) values.
Finally, the prevalence of key demographic and pregnancy-related risk factors, as ascertained from the univariate analyses and multivariate models, were calculated for maternal corrections history subgroups. The Relative Risk of experiencing each factor were calculated using Poisson regression with robust error variance for each sub-population with maternal corrections history, relative to infants whose mothers had no corrections record.
3. Results
There was a 2.1-fold greater risk of low birth weight for Indigenous infants compared to non-Indigenous infants (95% CI: 2.0–2.3, p<.001). The proportions of low birth weight by key pregnancy risk factors, and associated Relative Risks, are shown in Table 2. Despite overlapping confidence intervals among non-Indigenous children, the point estimates suggest that infants whose mothers were imprisoned before or during pregnancy had a higher prevalence of low birth weight than infants of mothers imprisoned after birth, with community corrections orders, or no corrections records.
Table 2.
Univariate analysis of potential determinants of low birth weight by Indigenous status.
| Indigenous Infants, n=25544 |
Non-Indigenous Infants, n=16366 |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2500 g+ | <2500 g |
2500 g+ | <2500 g |
|||||||||
| n | n | % | RR | (95% CI) | p | n | n | % | RR | (95% CI) | p | |
| Infants | 22363 | 3181 | 12.5 | 15414 | 952 | 5.8 | ||||||
| Maternal Corrections History | ||||||||||||
| Prison (before pregnancy)b | 2235 | 574 | 20.4 | 2.20 | (2.01–2.41) | <.001 | 549 | 92 | 14.4 | 3.23 | (2.63–3.97) | <.001 |
| Prison (during pregnancy) | 622 | 157 | 20.2 | 2.17 | (1.87–2.52) | <.001 | 216 | 29 | 11.8 | 2.66 | (1.87–3.79) | <.001 |
| Prison (after birth) | 3024 | 539 | 15.1 | 1.63 | (1.48–1.79) | <.001 | 2287 | 238 | 9.4 | 2.12 | (1.83–2.46) | <.001 |
| Community corrections | 4984 | 732 | 12.8 | 1.38 | (1.26–1.50) | <.001 | 596 | 46 | 7.2 | 1.61 | (1.21–2.16) | .001 |
| No corrections record* | 11498 | 1179 | 9.3 | 11766 | 547 | 4.4 | ||||||
| Demographic Factors | ||||||||||||
| Sexc | ||||||||||||
| Female | 10708 | 1682 | 13.6 | 1.19 | (1.12–1.27) | <.001 | 7376 | 488 | 6.2 | 1.14 | (1.01–1.29) | .040 |
| Male* | 11578 | 1488 | 11.4 | 7994 | 461 | 5.5 | ||||||
| Maternal Indigenous status | ||||||||||||
| Indigenous | 21259 | 3090 | 12.7 | 1.67 | (1.36–2.04) | <.001 | ||||||
| Non-Indigenous* | 1104 | 91 | 7.6 | 15414 | 952 | 5.8 | ||||||
| Socioeconomic statusd | ||||||||||||
| Very low (0–5%) | 5934 | 971 | 14.1 | 1.58 | (1.37–1.81) | <.001 | 899 | 100 | 10.0 | 2.25 | (1.81–2.80) | <.001 |
| Low (6–25%) | 9667 | 1400 | 12.7 | 1.42 | (1.24–1.62) | <.001 | 4086 | 314 | 7.1 | 1.61 | (1.38–1.88) | <.001 |
| Medium (26–50%) | 4447 | 582 | 11.6 | 1.30 | (1.12–1.50) | <.001 | 4187 | 248 | 5.6 | 1.26 | (1.07–1.49) | .006 |
| High (51–100%)* | 2296 | 225 | 8.9 | 6197 | 288 | 4.4 | ||||||
| Geographical remotenesse | ||||||||||||
| Cities/Inner regional* | 8948 | 1354 | 13.1 | 12557 | 795 | 6.0 | ||||||
| Outer regional | 3792 | 518 | 12.0 | 0.91 | (0.83–1.01) | .064 | 1689 | 111 | 6.2 | 1.04 | (0.85–1.26) | .721 |
| Remote | 4237 | 487 | 10.3 | 0.78 | (0.71–0.86) | <.001 | 797 | 30 | 3.6 | 0.61 | (0.43–0.87) | .007 |
| Very remote | 5366 | 819 | 13.2 | 1.01 | (0.93–1.09) | .856 | 314 | 13 | 4.0 | 0.67 | (0.39–1.14) | .140 |
| Baseline Pregnancy Risk Factors | ||||||||||||
| Birth spacing | ||||||||||||
| <18months | 2581 | 444 | 14.7 | 1.21 | (1.10–1.33) | <.001 | 992 | 97 | 8.9 | 1.59 | (1.30–1.95) | <.001 |
| Firstborn/18months+* | 19782 | 2737 | 12.2 | 14422 | 855 | 5.6 | ||||||
| Maternal age | ||||||||||||
| 12–19 years | 6694 | 942 | 12.3 | 0.98 | (0.90–1.07) | .634 | 1623 | 124 | 7.1 | 1.35 | (1.11–1.63) | .002 |
| 20–24 years | 8335 | 1144 | 12.1 | 0.96 | (0.88–1.04) | .303 | 3687 | 250 | 6.4 | 1.21 | (1.04–1.40) | .013 |
| 25–34 years* | 6546 | 943 | 12.6 | 8390 | 466 | 5.3 | ||||||
| 35+years | 788 | 152 | 16.2 | 1.28 | (1.10–1.50) | .002 | 1714 | 112 | 6.1 | 1.17 | (0.95–1.42) | .133 |
| Parity | ||||||||||||
| Nulliparous | 7888 | 1181 | 13.0 | 1.10 | (1.02–1.19) | .010 | 7382 | 477 | 6.1 | 1.14 | (1.00–1.29) | .054 |
| Parity 1–2* | 9574 | 1283 | 11.8 | 7032 | 397 | 5.3 | ||||||
| Parity 3+ | 4901 | 717 | 12.8 | 1.08 | (0.99–1.18) | .078 | 1000 | 78 | 7.2 | 1.35 | (1.07–1.71) | .011 |
| Previous abortion | ||||||||||||
| Yes | 4428 | 675 | 13.2 | 1.08 | (1.00–1.17) | .060 | 3049 | 234 | 7.1 | 1.30 | (1.13–1.50) | <.001 |
| No* | 17935 | 2506 | 12.3 | 12365 | 718 | 5.5 | ||||||
| Pregnancy Complications | ||||||||||||
| Hypertension, preeclampsia or eclampsia | ||||||||||||
| Yes | 972 | 299 | 23.5 | 1.98 | (1.78–2.20) | <.001 | 732 | 96 | 11.6 | 2.10 | (1.72–2.57) | <.001 |
| No* | 21391 | 2882 | 11.9 | 14682 | 856 | 5.5 | ||||||
| Any placental disorder | ||||||||||||
| Yes | 126 | 72 | 36.4 | 2.96 | (2.46–3.57) | <.001 | 144 | 40 | 21.7 | 3.86 | (2.91–5.11) | <.001 |
| No* | 22237 | 3109 | 12.3 | 15270 | 912 | 5.6 | ||||||
| Premature rupture of membranes | ||||||||||||
| Yes | 805 | 390 | 32.6 | 2.85 | (2.61–3.11) | <.001 | 345 | 82 | 19.2 | 3.52 | (2.87–4.32) | <.001 |
| No* | 21558 | 2791 | 11.5 | 15069 | 870 | 5.5 | ||||||
| Renal disorders in pregnancy | ||||||||||||
| Yes | 28 | 12 | 30.0 | 2.41 | (1.50–3.88) | <.001 | 13 | <5 | 13.3 | 2.29 | (0.63–8.35) | .280 |
| No* | 22335 | 3169 | 12.4 | 15401 | 950 | 5.8 | ||||||
| Infection related hospitalization | ||||||||||||
| Yes | 1,759 | 285 | 13.9 | 1.13 | (1.01–1.27) | .032 | 351 | 31 | 8.1 | 1.41 | (1.00–1.99) | .051 |
| No* | 20604 | 2896 | 12.3 | 15063 | 921 | 5.8 | ||||||
| Other Maternal Factors/Exposures in Pregnancy | ||||||||||||
| Substance use related service contactf | ||||||||||||
| Yes | 309 | 94 | 23.3 | 1.90 | (1.59–2.27) | <.001 | 238 | 52 | 17.9 | 3.20 | (2.48–4.13) | <.001 |
| No* | 22054 | 3087 | 12.3 | 15176 | 900 | 5.6 | ||||||
| Hospitalisation for external causes of injuryg | ||||||||||||
| Yes | 1,143 | 338 | 22.8 | 1.93 | (1.75–2.13) | <.001 | 250 | 29 | 10.4 | 1.81 | (1.28–2.57) | .001 |
| No* | 21220 | 2843 | 11.8 | 15164 | 923 | 5.7 | ||||||
| Mental health related service contacth | ||||||||||||
| Yes | 626 | 141 | 18.4 | 1.50 | (1.29–1.75) | <.001 | 371 | 52 | 12.3 | 2.18 | (1.68–2.83) | <.001 |
| No* | 21737 | 3040 | 12.3 | 15043 | 900 | 5.6 | ||||||
| Sibling in contact with Child Protection | ||||||||||||
| Yes | 689 | 166 | 19.4 | 1.59 | (1.38–1.83) | <.001 | 202 | 34 | 14.4 | 2.53 | (1.84–3.48) | <.001 |
| Firstborn/No* | 21674 | 3015 | 12.2 | 15212 | 918 | 5.7 | ||||||
Reference category
Prison before, not during, pregnancy
88 Indigenous and 47 non-Indigenous infants missing sex.
22 Indigenous and 47 non-Indigenous infants missing socioeconomic status.
23 Indigenous and 60 non-Indigenous infants missing remoteness.
Includes substance use and other (MHIS or HMDC).
Includes assault, excludes poisoning (HMDC).
Excludes substance use related contacts (MHIS or HMDC).
There was a statistically significant difference in year of birth for Indigenous infants with low birth weight (M=1999.33, SD=7.93) and normal/high birth weight (M=1998.55, SD=8.00); t(25542)=-5.17, p<.0001. There was no significant difference in birth years for non-Indigenous infants with low birth weight (M=1997.82, SD=6.75) and normal/high birth weight (M=1997.75, SD=6.89); t(16364)=-0.32, p=.7476.
Demographic factors associated with low birth weight for Indigenous and non-Indigenous infants were female sex, maternal Indigenous status, and being born in the lowest 50% of areas by socio-economic status. Birth spacing of less than 18-months was a significant risk factor for all infants. All maternal age groups outside of 25–34 years were associated with low birth weight for non-Indigenous infants, whereas only maternal ages of 35 years and above were significant for Indigenous infants. All pregnancy complications and other maternal factors were associated with low birth weight, except for renal disorders in pregnancy for non-Indigenous infants.
3.1. Multivariate regression of low birth weight by Indigenous status
For Indigenous infants, geographical remoteness was excluded from the multivariate analysis due to its correlation with socioeconomic status. For non-Indigenous infants, renal disorders in pregnancy was excluded as it was not statistically significant following univariate analysis with low birth weight (Table 2). Birth year was excluded from the full regression model for non-Indigenous infants as it was not statistically significant after multivariate analysis with other demographic factors (RR 1.00, 95%CI 0.99–1.01, p=.868).
Table 3, Table 4 present the full and final regression models of low birth weight for Indigenous (Table 3) and non-Indigenous (Table 4) infants. Relative to other factors included in the model maternal corrections history, particularly imprisonment before and during pregnancy, remained a strong determinant of low birth weight after adjusting for other key risk factors for both Indigenous and non-Indigenous infants.
Table 3.
Regression model of low birth weight for Indigenous infants.
| Full Model |
Final Model |
||||||
|---|---|---|---|---|---|---|---|
| RR | (95% CI) | p | RR | (95% CI) | p | ||
| Maternal corrections history | Prison (before pregnancy) | 2.01 | (1.82–2.21) | <.001 | 2.02 | (1.84–2.22) | <.001 |
| Prison (during pregnancy) | 1.95 | (1.67–2.27) | <.001 | 1.96 | (1.68–2.29) | <.001 | |
| Prison (after birth) | 1.57 | (1.43–1.74) | <.001 | 1.58 | (1.44–1.74) | <.001 | |
| Community corrections | 1.31 | (1.20–1.43) | <.001 | 1.32 | (1.21–1.43) | <.001 | |
| No corrections record | ref. | ||||||
| Any placental disorder* | Yes | 2.99 | (2.47–3.63) | <.001 | 3.01 | (2.48–3.65) | <.001 |
| No | ref. | ||||||
| PROM | Yes | 2.72 | (2.49–2.97) | <.001 | 2.73 | (2.49–2.98) | <.001 |
| No | ref. | ||||||
| Renal disorder | Yes | 2.40 | (1.49–3.86) | <.001 | 2.40 | (1.50–3.87) | <.001 |
| No | ref. | ||||||
| Hypertension, preeclampsia | Yes | 2.17 | (1.95–2.41) | <.001 | 2.17 | (1.95–2.41) | <.001 |
| No | ref. | ||||||
| External injury hospitalisation | Yes | 1.57 | (1.41–1.74) | <.001 | 1.58 | (1.43–1.75) | <.001 |
| No | ref. | ||||||
| Socioeconomic status | Very low (0–5%) | 1.53 | (1.34–1.75) | <.001 | 1.53 | (1.33–1.75) | <.001 |
| Low (6–25%) | 1.40 | (1.22–1.59) | <.001 | 1.39 | (1.22–1.59) | <.001 | |
| Medium (26–50%) | 1.28 | (1.11–1.48) | .001 | 1.28 | (1.11–1.47) | .001 | |
| High (51–100%) | ref. | ||||||
| Maternal Indigenous status | Indigenous | 1.40 | (1.15–1.71) | .001 | 1.39 | (1.14–1.70) | .001 |
| Non-Indigenous | ref. | ||||||
| Substance use related contact** | Yes | 1.33 | (1.11–1.61) | .002 | 1.36 | (1.13–1.63) | .001 |
| No | ref. | ||||||
| Maternal age at time of birth | 35+-years | 1.32 | (1.13–1.54) | <.001 | 1.32 | (1.13–1.54) | <.001 |
| <35-years | ref. | ||||||
| Birth spacing | <18months | 1.23 | (1.12–1.35) | <.001 | 1.23 | (1.11–1.35) | <.001 |
| Firstborn/18months+ | ref. | ||||||
| Sex | Female | 1.19 | (1.11–1.27) | <.001 | 1.19 | (1.11–1.27) | <.001 |
| Male | ref. | ||||||
| Parity | Nulliparous | 1.18 | (1.09–1.28) | <.001 | 1.17 | (1.09–1.26) | <.001 |
| Parity 1–2 | ref. | ||||||
| Parity 3+ | 0.95 | (0.87–1.04) | .287 | 0.96 | (0.87–1.05) | .405 | |
| Birth year | 1.01 | (1.00–1.01) | .001 | 1.01 | (1.00–1.01) | .001 | |
| Sibling contact Child Protection | Yes | 1.06 | (0.91–1.22) | .479 | |||
| Firstborn/No | ref. | ||||||
| Previous abortion | Yes | 1.05 | (0.97–1.14) | .229 | |||
| No | ref. | ||||||
| Mental health related contact | Yes | 1.05 | (0.90–1.23) | .520 | |||
| No | ref. | ||||||
| Infection related hospitalisation | Yes | 1.01 | (0.91–1.14) | .801 | |||
| No | ref. | ||||||
| Observations | 24,951 | 24,951 | |||||
| AIC | 0.7291 | 0.7289 | |||||
| Log pseudolikelihood | -9071.42 | -9072.33 | |||||
Includes abruptio placentae, placenta previa, and other placental disorders.
Includes hospital admissions and mental health service contacts related to substance use, including alcohol and poisoning.
Table 4.
Regression model of low birth weight for non-Indigenous infants.
| Full Model |
Final Model p |
||||||
|---|---|---|---|---|---|---|---|
| RR | (95% | p | RR | (95% CI) | p | ||
| Maternal corrections history | Prison (before pregnancy) | 2.36 | (1.85–3.00) | <.001 | 2.48 | (1.98–3.12) | <.001 |
| Prison (during pregnancy) | 1.99 | (1.38–2.88) | <.001 | 2.12 | (1.48–3.03) | <.001 | |
| Prison (after birth) | 1.72 | (1.47–2.02) | <.001 | 1.75 | (1.51–2.04) | <.001 | |
| Community corrections | 1.41 | (1.05–1.88) | .022 | 1.40 | (1.05–1.88) | .022 | |
| No corrections record | ref. | ||||||
| Any placental disorder* | Yes | 4.03 | (3.04–5.33) | <.001 | 4.04 | (3.05–5.36) | <.001 |
| No | ref. | ||||||
| PROM | Yes | 3.11 | (2.50–3.85) | <.001 | 3.16 | (2.56–3.91) | <.001 |
| No | ref. | ||||||
| Hypertension, preeclampsia | Yes | 2.32 | (1.89–2.84) | <.001 | 2.32 | (1.90–2.84) | <.001 |
| No | ref. | ||||||
| Substance use related contact** | Yes | 1.84 | (1.37–2.47) | <.001 | 1.97 | (1.49–2.59) | <.001 |
| No | ref. | ||||||
| Socioeconomic status | Very low (0–5%) | 1.61 | (1.29–2.02) | <.001 | 1.62 | (1.30–2.03) | <.001 |
| Low (6–25%) | 1.34 | (1.14–1.56) | <.001 | 1.33 | (1.14–1.56) | <.001 | |
| Medium (26–50%) | 1.14 | (0.96–1.34) | .125 | 1.13 | (0.96–1.34) | .136 | |
| High (51–100%) | ref. | ||||||
| Birth spacing | <18months | 1.57 | (1.27–1.96) | <.001 | 1.55 | (1.25–1.93) | <.001 |
| Firstborn/18months+ | ref. | ||||||
| Parity | Nulliparous | 1.24 | (1.08–1.43) | .003 | 1.21 | (1.06–1.39) | .005 |
| Parity 1–2 | ref. | ||||||
| Parity 3+ | 1.05 | (0.83–1.33) | .682 | 1.07 | (0.84–1.35) | .584 | |
| Previous abortion | Yes | 1.16 | (1.01–1.34) | .042 | 1.17 | (1.02–1.36) | .029 |
| No | ref. | ||||||
| Sex | Female | 1.13 | (1.00–1.28) | .046 | 1.14 | (1.01–1.28) | .041 |
| Male | ref. | ||||||
| Mental health related contact | Yes | 1.23 | (0.92–1.64) | .154 | |||
| No | ref. | ||||||
| Sibling contact Child Protection | Yes | 1.16 | (0.81–1.67) | .411 | |||
| Firstborn/No | ref. | ||||||
| Infection related hospitalisation | Yes | 1.12 | (0.79–1.57) | .525 | |||
| No | ref. | ||||||
| External injury hospitalisation | Yes | 1.09 | (0.75–1.60) | .641 | |||
| No | ref. | ||||||
| Maternal age at time of birth | <20-years | 0.92 | (0.75–1.12) | .410 | |||
| 20+-years | ref. | ||||||
| Geographical remoteness | Outer regional | 1.05 | (0.87–1.27) | .601 | |||
| Remote | 0.68 | (0.48–0.97) | .034 | ||||
| Very remote | 0.87 | (0.51–1.48) | .600 | ||||
| Major cities/Inner regional | ref. | ||||||
| Observations | 16,285 | 16,298 | |||||
| AIC | 0.4255 | 0.4250 | |||||
| Log pseudolikelihood | −3439.79 | −3446.47 | |||||
**Includes hospital admissions and mental health service contacts related to substance use, including alcohol and poisoning.
Includes abruptio placentae, placenta previa, and other placental disorders.
Fig. 2 displays the relationships between maternal corrections history (relative to no corrections record) and low birth weight that were found in the final regression models for Indigenous and non-Indigenous infants. Maternal imprisonment before pregnancy had the strongest effect on low birth weight for both Indigenous and non-Indigenous infants. The effect of maternal imprisonment before pregnancy also appeared separate from the effect of imprisonment after birth for both Indigenous and non-Indigenous infants, despite a small overlap in confidence intervals for non-Indigenous infants. For Indigenous infants, the confidence intervals for maternal imprisonment during pregnancy overlapped with those for maternal imprisonment before pregnancy, and to a small but non-significant extent with maternal imprisonment after birth. For non-Indigenous infants, the effect of maternal imprisonment during pregnancy overlapped with the effects of imprisonment before and after birth.
Fig. 2.
The Relative Risk of low birth weight by maternal corrections history relative to no corrections record, in the final regression models for Indigenous and non-Indigenous infants.
3.2. Prevalence of key risk factors by maternal corrections history
The prevalence of key risk factors by maternal corrections history is shown in Table 5. The proportion of infants born in areas of very low socioeconomic status was relatively high for all Indigenous children and did not differ greatly by maternal corrections history. For non-Indigenous children, infants with any maternal corrections history had higher proportions of very low socioeconomic status than those with no maternal corrections history.
Table 5.
Prevalence of selected determinants of low birth weight, by maternal corrections history and Indigenous status.
| Indigenous infants |
Non-Indigenous infants |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Prison (before preg.) | Prison (during preg.) | Prison (after birth) | Comm- unity | No Correct-ions | Prison (before preg.) | Prison (during preg.) | Prison (after birth) | Comm- unity | No Correct-ions | |
| n=2898 | n=807 | n=3658 | n=5919 | n=13068 | n=669 | n=249 | n=2588 | n=662 | n=12639 | |
| Very low SESa | ||||||||||
| % | 23.4 | 22.3 | 29.2 | 29.8 | 26.3 | 13.7 | 12.8 | 13.0 | 12.3 | 3.9 |
| RR | 0.89 | 0.85 | 1.11 | 1.13 | ref. | 3.56 | 3.31 | 3.37 | 3.20 | ref. |
| p-value | .001 | .015 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | ||
| Birth spacing <18mth | ||||||||||
| % | 17.9 | 10.5 | 14.0 | 12.8 | 9.5 | 12.2 | 8.2 | 9.9 | 10.4 | 5.5 |
| RR | 1.88 | 1.10 | 1.47 | 1.34 | ref. | 2.22 | 1.49 | 1.81 | 1.91 | ref. |
| p-value | <.001 | .361 | <.001 | <.001 | <.001 | .066 | <.001 | <.001 | ||
| Nulliparous | ||||||||||
| % | 21.5 | 34.8 | 38.8 | 32.5 | 39.1 | 33.2 | 39.2 | 53.5 | 43.3 | 48.1 |
| RR | 0.55 | 0.89 | 0.99 | 0.83 | ref. | 0.69 | 0.81 | 1.11 | 0.90 | ref. |
| p-value | <.001 | .021 | .773 | <.001 | <.001 | .011 | <.001 | .023 | ||
| Previous abortion | ||||||||||
| % | 26.9 | 22.2 | 17.4 | 20.7 | 18.7 | 36.3 | 33.5 | 24.6 | 28.2 | 17.6 |
| RR | 1.44 | 1.19 | 0.93 | 1.10 | ref. | 2.07 | 1.90 | 1.40 | 1.60 | ref. |
| p-value | <.001 | .014 | .067 | .002 | <.001 | <.001 | <.001 | <.001 | ||
| Hypertension, etc.b | ||||||||||
| % | 3.1 | 4.2 | 3.8 | 4.4 | 6.0 | 4.4 | 4.9 | 4.7 | 4.8 | 5.2 |
| RR | 0.52 | 0.71 | 0.64 | 0.74 | ref. | 0.84 | 0.95 | 0.91 | 0.93 | ref. |
| p-value | <.001 | .046 | <.001 | <.001 | .366 | .843 | .331 | .694 | ||
| Placental disorders | ||||||||||
| % | 0.8 | 0.9 | 0.8 | 0.8 | 0.7 | 0.3 | 1.6 | 1.6 | 0.8 | 1.1 |
| RR | 1.14 | 1.25 | 1.17 | 1.15 | ref. | 0.29 | 1.52 | 1.51 | 0.73 | ref. |
| p-value | .571 | .565 | .447 | .448 | .083 | .403 | .019 | .481 | ||
| PROMc | ||||||||||
| % | 6.7 | 5.4 | 5.0 | 5.2 | 3.9 | 5.5 | 3.3 | 3.5 | 3.3 | 2.2 |
| RR | 1.73 | 1.40 | 1.30 | 1.35 | ref. | 2.45 | 1.47 | 1.58 | 1.47 | ref. |
| p-value | <.001 | .032 | .002 | <.001 | <.001 | .277 | <.001 | .084 | ||
| Substance used | ||||||||||
| % | 3.3 | 7.1 | 2.1 | 1.6 | 0.7 | 12.5 | 10.2 | 4.6 | 3.1 | 0.4 |
| RR | 4.61 | 9.84 | 2.89 | 2.19 | ref. | 32.02 | 26.18 | 11.89 | 7.99 | ref. |
| p-value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | ||
| External injury | ||||||||||
| % | 10.9 | 15.0 | 9.3 | 6.4 | 2.9 | 7.2 | 6.5 | 3.5 | 2.2 | 0.9 |
| RR | 3.83 | 5.26 | 3.24 | 2.24 | ref. | 7.75 | 7.05 | 3.81 | 2.36 | ref. |
| p-value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | .002 | ||
| Mental health | ||||||||||
| % | 6.9 | 8.7 | 3.5 | 3.1 | 1.6 | 13.1 | 11.0 | 5.1 | 5.1 | 1.2 |
| RR | 4.36 | 5.53 | 2.24 | 2.00 | ref. | 10.69 | 8.98 | 4.13 | 4.19 | ref. |
| p-value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | ||
| Sibling in contact CPe | ||||||||||
| % | 11.3 | 14.2 | 5.1 | 2.6 | 0.7 | 13.1 | 11.4 | 4.3 | 1.6 | 0.04 |
| RR | 15.22 | 19.22 | 6.92 | 3.54 | ref. | 322.71 | 281.44 | 106.31 | 38.36 | ref. |
| p-value | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | ||
Very low socioeconomic status defined as 0–5%, 22 Indigenous and 47 non-Indigenous infants missing socioeconomic status.
Hypertension, preeclampsia, and eclampsia.
Premature rupture of membranes.
Substance use, alcohol and poisoning related hospital admissions and mental health service contacts.
Older sibling in contact with the child protection system during infant’s pregnancy.
There was a higher prevalence of birth spacing less than 18-months for all infants with any maternal corrections history compared to no maternal corrections history, which was significant for all corrections subgroups except for infants whose mothers were imprisoned during pregnancy. There was a higher prevalence of previous abortion for all infants with any maternal corrections history relative to infants with no maternal corrections history, except for Indigenous infants whose mothers were first imprisoned after birth.
The prevalence of hospitalisation for hypertension during pregnancy, preeclampsia or eclampsia was lower for all infants with a maternal corrections history relative to no corrections history, however, this difference was only significant for Indigenous infants. Hospitalisation for placental disorders did not differ by maternal corrections history for Indigenous children, and was only higher for non-Indigenous infants whose mothers were first imprisoned after their birth. Prevalence of hospitalisation for premature rupture of membranes was higher for Indigenous infants with any maternal corrections history, and likewise for non-Indigenous infants but the difference was not significant for non-Indigenous infants whose mothers were imprisoned during pregnancy. Prevalence of renal disorders in pregnancy was low and did not differ by maternal corrections history.
Generally, infants of mothers with any corrections history had higher prevalence of service contact in pregnancy for substance use (including alcohol and poisoning), external causes of injury, and mental health, and sibling contact with the child protection system, compared to infants whose mothers had no corrections history. Prevalence of these service contacts in pregnancy was highest for infants whose mothers were imprisoned before or during pregnancy, compared to infants whose mothers were imprisoned after birth or had community orders alone. For Indigenous infants, the highest prevalence was experienced by infants whose mothers were imprisoned during pregnancy, while for non-Indigenous infants it was highest amongst infants whose mothers were imprisoned before pregnancy.
4. Discussion
To our knowledge this is the largest study comparing low birth weight outcomes for 1,024 infants born to mothers imprisoned during pregnancy, to infants of mothers with differing maternal corrections histories and infants of mothers with no corrections records. Previous studies have included samples ranging from three to a maximum of 496 infants of mothers imprisoned in pregnancy (Knight and Plugge, 2005b, Walker et al., 2014). Importantly, this is the first study to comprehensively investigate low birth weight outcomes for Indigenous infants of pregnant prisoners, who are a high-priority population with unique circumstances that warrant their separate consideration from non-Indigenous infants.
For Indigenous and non-Indigenous infants, low birth weight was highest for infants whose mothers were imprisoned before or during pregnancy. There was a lower prevalence of low birth weight for infants whose mothers were first imprisoned after birth compared to those whose mothers were imprisoned before birth. In addition, infants of mothers who had a history of community correctional orders with no imprisonment, had a lower prevalence of low birth weight compared to infants of mothers with any history of imprisonment, and higher prevalence than those infants whose mothers had no corrections history.
The strongest determinants of low birth weight were pregnancy complications (excluding infection related hospitalisations during pregnancy). These complications are also adverse pregnancy outcomes independent of their relationship to low birth weight, and are likely contributed to by other risk factors such as those demographic factors, baseline pregnancy risk factors, and other maternal exposures in pregnancy included in the full regression models. A history of maternal imprisonment, particularly before and during pregnancy, remained a strong determinant of low birth weight after adjusting for these pregnancy complications and other key risk factors.
Our findings are in line with the only other Australian study to date conducted by Walker and colleagues (2014) in New South Wales. They too found that women imprisoned during pregnancy experienced similarly poor perinatal outcomes, including low birth weight, as women imprisoned at times other than pregnancy. They did not look separately at outcomes for women imprisoned ‘before’ and ‘after’ pregnancy. We found infants born to mothers imprisoned before or during pregnancy had a higher prevalence of low birth weight than women first imprisoned after birth.
A review of prior studies mainly conducted in the United States found that mothers imprisoned during pregnancy have better birth weight outcomes than similarly disadvantaged women (Knight & Plugge, 2005b). Together the findings in the present study and Walker et al. (2014), suggest a general difference with respect to pregnancy outcomes for Australian women prisoners than those reported in the international literature.
A key question of the literature has been whether maternal imprisonment itself has an effect on birth weight or if it predominantly acts as a proxy for socioeconomic disadvantage and other risk behaviours associated with the prisoner population. We found that prevalence of adverse maternal exposures in pregnancy such as alcohol and other substance use and injury, were highest for those infants whose mothers were also imprisoned during pregnancy (Indigenous) or before pregnancy (non-Indigenous). This suggests a possible co-occurrence of these risk factors with timing of imprisonment.
An alternative explanation, that aligns with the findings of the present study, is that the high level of pre-existing disadvantage experienced by women in contact with the prison system places women in a position of vulnerability whereby the experience of imprisonment may have a separate and additive effect that contributes to existing disadvantage. Numerous studies have reported that as adversities accumulate, health and social outcomes deteriorate (Kalmakis & Chandler, 2015). This may explain the differences in this study between Indigenous and non-Indigenous populations, as Indigenous women are generally of lower socioeconomic status (stemming from a history of discrimination and disadvantage) which may place them at a “lower baseline” whereby imprisonment may have a more substantial effect. If maternal imprisonment was acting solely as a proxy for socioeconomic disadvantage and other risk behaviours associated with the prisoner population, we would have expected more overlap between the effects of imprisonment before and after pregnancy, given the models were adjusted for key pregnancy risks including alcohol and substance use and socioeconomic disadvantage.
Walker and colleagues (2014) proposed that a key reason for the difference between the findings of Australian and other studies may be the length of prison stay experienced by women prisoners in different jurisdictions. It has been shown that longer prison stays in pregnancy have been associated with higher birth weight (Martin et al., 1997b, Howard et al., 2011). In our study of young Western Australian children whose mothers were imprisoned after birth and before their second birthday, we found nearly half of prison stays were for less than a fortnight and only one-fifth were for periods of six-months or more (Dowell, Mejia, Preen, & Segal, 2018). In Western Australia, prisoners sentenced for periods less than six-months, in general, are not provided with a management plan or access to treatment programs (Ferguson, 2015).
It is likely that maternal imprisonment during pregnancy has varied effects on infant birth weight depending on the characteristics of the mother, infant, and characteristics of imprisonment in pregnancy, particularly duration, frequency and timing in relation to gestational age. Prison may have a beneficial effect for some infants in certain circumstances, and a detrimental effect for others. To identify which infants are at greater risk, further analyses examining individual predicted probabilities should be conducted.
Regardless, the results of the present study in Western Australia clearly demonstrate the impact of imprisonment of women before and during pregnancy resulting in a greater risk of low birth weight for their infants. These results highlight the importance of criminal justice policies that address both the underlying vulnerabilities of women prisoners generally and the needs of pregnant prisoners specifically. Western Australia has made significant steps towards providing women-centred prison services. This includes, notably, the establishment of the Boronia Pre-release Centre for Women in 2004, which has been described as a model for good practice in the management of women prisoners (Bartels & Gaffney, 2011). This study highlights the importance of the continuation and expansion of women-centred approaches throughout the criminal justice system, and the need for these approaches to extend to addressing the potential impacts on women’s infants and children as a priority issue.
4.1. Limitations
For infants whose mother had a prison record at any time, the sampling method included comparatively fewer non-Indigenous infants whose mothers had a prison record before or during pregnancy. Smaller numbers of observations of non-Indigenous infants with low birth weight were reported within the group imprisoned before or during pregnancy. This will have affected power to detect relationships, but should not have introduced any bias.
As gestational age was not obtained and birth date was provided to month of birth only, pregnancy was taken to begin nine-months prior to month of birth for all infants. Accordingly, some records of exposure (including imprisonment) that were attributed to having occurred during pregnancy may have occurred prior to pregnancy if gestation was shorter than nine-months. There is evidence, however, that the adverse events within the preconception period (6-0 months before pregnancy) can increase infant mortality risk (Class et al., 2013, Class et al., 2015).
In using administrative data and only having primary diagnosis codes for key service contacts (not co-diagnoses), the study has not fully captured heavy drinking or substance use in pregnancy, mental illness, or injuries indicative of domestic violence in pregnancy within the study population. O’Leary et al. (2013) examined alcohol-use disorders in pregnant women and the extent of under-reporting using Western Australian linked data. They used hospital, mental health service, drugs and alcohol service, and the register for developmental anomalies, and found 70% of mothers of children diagnosed with foetal alcohol syndrome did not have an alcohol diagnosis recorded in pregnancy. This suggests the relative risks associated with drinking or substance use in pregnancy, or mental illness, or injuries may be understated, due to misclassification of some affected by these risks as not.
Maternal smoking in pregnancy is an important risk factor for low birth weight that was not fully captured in the study. It is likely that smoking in pregnancy will have been partly captured by maternal corrections history and socioeconomic status. For example, for infants born from 1998 onwards, maternal smoking in pregnancy was high for all Indigenous and non-Indigenous infants whose mothers had any corrections history (range 58–78%), compared to infants whose mothers had no corrections record (41% Indigenous, 19% non-Indigenous).
Hospital data were not available for second-generation children. While explanatory variables based on hospital data were primarily taken from maternal hospital records (available for all mothers), there may have been some missed some cases of chromosomal abnormalities, and alcohol and other substance use related service contacts in pregnancy, for the second-generation children.
5. Conclusions
This study adds to the literature that suggests Australian infants born to mothers imprisoned during pregnancy do not generally experience the improved birth weight outcomes reported in the international literature. This study demonstrates that infants of women imprisoned in Western Australia, particularly before and during pregnancy, experience an increased risk of low birth weight. Infants with mothers imprisoned before or during pregnancy experience a higher prevalence of maternal risk exposures in pregnancy related to alcohol and other substance use, injury and mental distress. However, the strength of relationship between a history of maternal imprisonment before or during pregnancy is maintained after adjusting for these additional maternal risk exposures, suggesting that maternal imprisonment may have a separate impact on risk of low birth weight. Identifying whether particular groups of infants of women prisoners experience the worse outcomes is an important next step.
Acknowledgements
We thank the Developmental Pathways in Western Australian Children Project, the Western Australian Data Linkage Branch, the Western Australian Aboriginal Health Research Ethics Committee, the Western Australian Aboriginal and Torres Strait Islander community, the Western Australian Department of Justice, the Department of Communities: Child Protection and Family Support, the Western Australian Department of Health and the custodians of the Western Australian Birth and Death Registrations, Hospital and Morbidity Data Collection, Mental Health Information System, and Midwives Notification System for the linkages, provision of data and ongoing ethical review of project outputs.
Material presented cannot be considered as either endorsed by the Western Australian Department of Justice or an expression of the policies or view of the Department, and any errors or omission or commission are the responsibility of the Researchers.
Responsibility for interpretation of the data supplied through the Government of Western Australia, the Developmental Pathways in Western Australian Children Project, and by any other data custodian, is the Researchers’ alone.
Acknowledgments
Data statement
This study used linked routinely-collected administrative data from the Western Australian Departments of Health, Justice, and Communities: Child Protection and Family Support. While these data are accessible to approved researchers through the standard ethical and data application processes, they are not publicly available and are maintained by the relevant government data custodians. As a result, while future researchers are able to apply directly for these data we are restricted under Statutory requirement from releasing any of our project data to a third party. This includes making the study data available in a publicly available repository.
Ethics approval
Ethical approval for the project was received from the Department of Health Human Research Ethics Committee, the Western Australian Aboriginal Health Ethics Committee, and the University of South Australia Human Research Ethics Committee.
The study uses data that is routinely collected by the Department of Justice and other Western Australian Government departments and services and linked for research purposes by the Western Australian Data Linkage Branch. In cases such as this the National Health and Medical Research Council outlines in the National Statement on Conduct in Human Research the requirements for waiver of consent. Under the National Statement, a Human Research Ethics Council can grant a waiver of consent if it is satisfied certain conditions have been met. The criteria for allowing a waiver listed under the National Statement apply to the project. Specifically as the project carries no more than a low risk; it is not feasible to obtain consent due to the age and quantity of the data required; and measures are being taken to ensure the continued protection of the confidentiality of the data.
Conflict of interest
The authors have no conflict of interest.
Financial disclosure statement
CD was funded by an Australian Government Research Training Program (RTP) Scholarship.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2018.11.008.
Appendix A. Supplementary material
Supplementary material.
.
References
- Arnold L., Hoy W., Wang Z. Low birthweight increases risk for cardiovascular disease hospitalisations in a remote Indigenous Australian community – a prospective cohort study. Australian and New Zealand Journal of Public Health. 2015;40(S1):S102–S106. doi: 10.1111/1753-6405.12426. [DOI] [PubMed] [Google Scholar]
- Australian Bureau of Statistics (ABS) (2011). Estimated resident Aboriginal and Torres Strait Islander and Non-Indigenous population, States and Territories, 30 June 2011, Tables 1 & 3, viewed 20 December 2017, 〈http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3238.0.55.001June%202011?OpenDocument〉.
- Australian Bureau of Statistics (ABS) (2016). Prisoners in Australia, 2016, Table 20, viewed 20 December 2017, 〈http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/4517.02016?OpenDocument〉.
- Bard E., Knight M., Plugge E. Perinatal health care services for imprisoned pregnant women and associated outcomes: A systematic review. BMC Pregnancy and Childbirth. 2016;16(285) doi: 10.1186/s12884-016-1080-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartels L., Gaffney A. Australian Institute of Criminology; Canberra: 2011. Good practice in women’s prisons: A literature review. (AIC Reports: Technical and Background Paper 41) [Google Scholar]
- Bell J.F., Zimmerman F.J., Cawthon M.L., Huebner C.E., Ward D.H., Schroeder C.A. Jail incarceration and birth outcomes. Journal of Urban Health. 2004;81:630–644. doi: 10.1093/jurban/jth146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen D., Davis G., Draper G., Mitrou F., McKeown S., Lawrence D. Evidence for the use of an algorithm in resolving inconsistent and missing Indigenous status in administrative data collections. Australian Journal of Social Issues. 2014;49(4):423–443. [Google Scholar]
- Class Q.A., Khashan A.S., Lichtenstein P., Långström N., D’Onofrio B.M. Maternal stress and infant mortality: The importance of the preconception period. Psychological Science. 2013;24(7):1309–1316. doi: 10.1177/0956797612468010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Class Q.A., Mortensen P.B., Henriksen T.B., Dalman C., D’Onofrio B.M., Khashan A.S. Preconception maternal bereavement and infant and childhood mortality: A Danish population-based study. Psychosomatic Medicine. 2015;77(8):863–869. doi: 10.1097/PSY.0000000000000229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Elsevier Science; 1988. Statistical power analysis for the behavioral sciences, revised edition; p. 222. (Ebook ISBN 9781483276489) [Google Scholar]
- Council of Australian Governments (COAG) (2009). Closing the Gap on Indigenous Disadvantage: The Challenge for Australia, February 2009, viewed 20 December 2017, 〈https://www.dss.gov.au/sites/default/files/documents/05_2012/closing_the_gap.pdf〉.
- Dowell C.M., Mejia G.C., Preen D.B., Segal L. Maternal incarceration, child protection, and infant mortality: A descriptive study of infant children of women prisoners in Western Australia. Health and Justice. 2018;6(2) doi: 10.1186/s40352-018-0060-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson C. Australian Institute of Criminology; Canberra: 2015. Parole in Western Australia: An analysis of parole cancellations of female offenders, Trends & issues in crime and criminal justice, No. 501. [Google Scholar]
- Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. American Journal of Epidemiology. 2004;160(4):301–305. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- Holman C.D., Bass A.J., Rouse I.L., Hobbs M.S. Population based linkage of health records in Western Australia: Development of a health services research linked database. Australian and New Zealand Journal of Public Health. 1999;23(5):453–459. doi: 10.1111/j.1467-842x.1999.tb01297.x. [DOI] [PubMed] [Google Scholar]
- Howard D.L., Strobino D., Sherman S.G., Crum R.M. Maternal incarceration during pregnancy and infant birthweight. Maternal and Child Health Journal. 2011;15:478–486. doi: 10.1007/s10995-010-0602-y. [DOI] [PubMed] [Google Scholar]
- Hoy W., Nicol J. Birthweight and natural deaths in a remote Australian Aboriginal community. Medical Journal of Australia. 2010;192(1):14–19. doi: 10.5694/j.1326-5377.2010.tb03394.x. [DOI] [PubMed] [Google Scholar]
- Kalmakis K.A., Chandler G.E. Health consequences of adverse childhood experiences: A systematic review. Journal of the American Association of Nurse Practitioners. 2015;27:457–465. doi: 10.1002/2327-6924.12215. [DOI] [PubMed] [Google Scholar]
- Kyei-Aboagye K., Vragovic O., Chong D. Birth outcome in incarcerated, high-risk pregnant women. Journal of Reproductive Medicine. 2000;45:190–194. [PubMed] [Google Scholar]
- Knight M., Plugge E. Risk factors for adverse perinatal outcomes in imprisoned pregnant women: A systematic review. BMC Public Health. 2005;5(111) doi: 10.1186/1471-2458-5-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight M., Plugge E. The outcomes of pregnancy among imprisoned women: A systematic review. BJOG: An International Journal of Obstetrics and Gynaecology. 2005;112:1467–1474. doi: 10.1111/j.1471-0528.2005.00749.x. [DOI] [PubMed] [Google Scholar]
- Kozuki N., Lee A.C.C., Silveira M.F., Sania A., Vogel J., Adair L., Barros F., Caulfield L.E., Christian P., Fawzi W., Humphrey J., Huybregts L. The associations of parity and maternal age with small-for-gestational-age, preterm, and neonatal and infant mortality: A meta-analysis. BMC Public Health. 2013;13(Suppl 3):S2. doi: 10.1186/1471-2458-13-S3-S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luyckx V.A. Effect of fetal and child health on kidney development and long-term risk of hypertension and kidney disease. The Lancet. 2013;382(9888):273–283. doi: 10.1016/S0140-6736(13)60311-6. [DOI] [PubMed] [Google Scholar]
- Martin S.L., Kim H., Kupper L.L., Meyer R.E., Hays M. Is incarceration during pregnancy associated with infant birthweight. American Journal of Public Health. 1997;87:1526–1531. doi: 10.2105/ajph.87.9.1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin S.L., Rieger R.H., Kupper L.L., Meyer R.E., Qaqish B.F. The effect of incarceration during pregnancy on birth outcomes. Public Health Reports. 1997;112(4):340–346. [PMC free article] [PubMed] [Google Scholar]
- McMillen I.C., Robinson J. Developmental Origins of the Metabolic Syndrome: Prediction, Plasticity, and Programming. Physiological Reviews. 2005;85:571–663. doi: 10.1152/physrev.00053.2003. [DOI] [PubMed] [Google Scholar]
- McNutt L.A., Wu C., Xue X., Hafner J.P. Estimating the relative risk in cohort studies and clinical trials of common outcomes. American Journal of Epidemiology. 2003;157(10):940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- Mertens D.J. Pregnancy outcomes of inmates in a large county jail setting. Public Health Nursing. 2001;18:45–53. doi: 10.1046/j.1525-1446.2001.00045.x. [DOI] [PubMed] [Google Scholar]
- Mosely H.W., Chen L.C. An analytical framework for the study of child survival in developing countries. Population and Development Review. 1984;10:25–45. [Google Scholar]
- O’Leary C.M., Halliday J., Bartu A., D’Antoine H., Bower C. Alcohol-use disorders during and within one year of pregnancy: a population-based cohort study 1985-2006. BJOG: Int. J. Obstet. Gynaecol. 2013;120(6):744–753. doi: 10.1111/1471-0528.12167. [DOI] [PubMed] [Google Scholar]
- Salihu H.M., August E.M., de la Cruz C., Mogos M.F., Weldeselasse H., Alio A.P. Infant mortality and the risk of small for gestational age in the subsequent pregnancy: A retrospective cohort study. Maternal and Child Health Journal. 2013;17(6):1044–1051. doi: 10.1007/s10995-012-1085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw J., Downe S., Kingdon C. Systematic mixed-methods review of interventions, outcomes and experiences for imprisoned pregnant women. Journal of Advanced Nursing. 2015;71(7):1451–1463. doi: 10.1111/jan.12605. [DOI] [PubMed] [Google Scholar]
- Terk J.V., Martens M.G., Williamson M.A. Pregnancy outcomes of incarcerated Women. Journal of Maternal-Fetal Medicine. 1993;2:246–250. [Google Scholar]
- Walker J.R., Hilder L., Levy M.H., Sullivan E.A. Vol. 14. 2014. Pregnancy, prison and perinatal outcomes in New South Wales, Australia: A retrospective cohort study using linked health data; p. 214. (BMC Pregnancy & Childbirth). [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A., Wong W., Sureshkumur P., Singh G. The burden of kidney disease in indigenous children of Australia and New Zealand, epidemiology, antecedent factors and progression to chronic kidney disease. Journal of Paediatrics and Child Health. 2010;46(9):504–509. doi: 10.1111/j.1440-1754.2010.01851.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) WHO; Geneva: 1992. International Classification of Diseases and Related Health Problems, 10th Revision. [Google Scholar]
- Xiao X., Zhang Z., Li W., Feng K., Sun Q., Cohen H., Xu T., Wang H., Liu A., Gong X., Shen Y., Yi Z. Low birth weight is associated with components of the metabolic syndrome. Metabolism. 2010;59:1282–1286. doi: 10.1016/j.metabol.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z., Kris-Etherton P.M., Hartman T.J. Birth weight and risk factors for cardiovascular disease and type 2 diabetes in US children and adolescents: 10 year results from NHANES. Maternal and Child Health Journal. 2013;18(6):1423–1432. doi: 10.1007/s10995-013-1382-y. [DOI] [PubMed] [Google Scholar]
- Zou G. A modified Poisson regression approach to prospective studies with binary data. American Journal of Epidemiology. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.