Abstract
Background:
Breast carcinoma is the most important cause of death in women’s oncologic pathology worldwide. Due to its high frequency, important advances in diagnostic and management of this entity were made. Because of its rarity (only 0.5-1% in all breast cancers), little is known about male breast cancer, and no specific male standardised protocol was made, treatment and follow-up being adopted from women breast cancer guidelines. We consider that this entity, with its hormone specific profile, is worth being considered for further studies, taking into account that male breast cancer has a far worse prognostic than female breast cancer.
Methods:
We present our four-year experience with male breast lesions in a retrospective review study, including gynecomastia and breast carcinoma cases.
Results:
We identified 17 male breast lesions, 11 of them with a diagnosis of gynaecomastia, the rest being breast carcinomas. Four malignant lesions were encountered in the 5th, 6th and 7th decade, with two of them in young adults (35 and 40 years old). In a single case, two different histotypes of breast carcinoma were found. All of them were G2, with tumoral stages varying between IB to IV. Androgen receptors were expressed in each case, in different percentages.
Conclusion:
Male breast carcinoma is a rare entity with a poor prognosis, a diffuse and profound invasion of adjacent structures, and a high expression of hormone receptors, and with no histologic relation to gynaecomastia, considering that no associated benign lesions were found.
Keywords:gynaecomastia, male breast carcinoma, androgen receptors, hormonal profile.
INTRODUCTION
Male breast lesions are not uncommon, but comparing with female counterpart, there are some important histologic and physiologic differences. Morphologically, the male breast gland is not fully developed, and only in rare cases real terminal duct lobular unit (TDLU) (the main site of origin for female breast lesions) can be found. This is the reason why lobular lesions and fibroadenomas (their stromal component originates in the interlobular stroma) are exceedingly rare.
Gynaecomastia is far more common. According to the fourth edition of the World Health Organisation (WHO) classification of breast lesions, its histologic definition consists in a non-neoplastic, often reversible enlargement of the male breast associated with proliferation of ductal elements and mesenchymal components. It is seen in up to 90% of all new-borns (1); its prevalence in adult population ranges between 30% and 70% in different statistics. In most of the cases, it represents the expression of an imbalanced androgen to oestrogen ratio; besides, a physiologic manifestation of development (in new-borns or peripubertal boys) may appear in relation to certain pathologic conditions such as Klinefelter syndrome, cirrhosis, hypogonadism, HCG producing tumours or hyperthyroidism. More commonly, it is associated with a variety of drugs including spironolactone (2), cyclic antidepressants (3), or finasteride, which are used for prostatic hyperplasia (4). Relevant substances linked to gynaecomastia include alcohol, heroin and marijuana (5). Histologically, there are two recog - nised patterns: florid and fibrous. Both are the expression of different steps of development; in the majority of cases they coexist, one being more prevalent than the other. The florid pattern is characterised by proliferated branched ducts with epithelial hyperplasia, and the fibrous pattern by a more hyalinized stroma with a flat bilayer of epithelial cells inside the scant ducts. Male breast carcinoma is a rare condition, accounting for less than 1% of all breast carcinomas (6). Only 0.1% (7) of mortality among male oncologic conditions is attributed to this pathologic entity. Considering these data, it is obvious that comparing to females, among whom breast cancer is the first cause of oncologic death in most European and American countries, the disease is less studied, treated and followed in males.
The most important risk factors are represented by hormonal imbalance (caused by the metabolic syndrome even in young patients (8), hyperthyroidism, testicular disorders of development, traumatic or infectious origin or antiandrogenic medication used for prostatic carcinoma) and environmental conditions (therapeutic or professional exposure to radiation). Most studies did not find any correlation between breast cancer and gynaecomastia in men. Clinically, in most of the cases it manifests as a painless mass, usually unilateral, with a marked tendency of infiltration in the adjacent structures. When extended to the nipple or skin, nipple retraction or ulceration is observed. In almost all cases, imagistic investigation is performed in advanced stages, and it seems that mammography provides the most accurate size measurement (5); for BIRADS system of scoring, the protocol is identical to that used in women, with similar results (10).
From a histologic point of view, NST (no special type) is the most common histotype, but papillary carcinoma or Paget disease was also described. Invasive lobular carcinoma is an exceptional entity, a fact explained by the usual absence of TDLU in normal male breast. Immunohistochemically, the panel of markers is the same as that used for female breast carcinoma, and most of male breast carcinomas are strongly positive for ER and PR.
For appreciating the prognostic factors, the Nottingham grading system and classification of molecular subtypes are used. Comparing to females, breast male carcinoma tends to be discovered in more severe stages of disease and, at least for this reason, the overall prognostic is worst.
The aim of this paper is to show the last four-year experience of the department of Pathology of the Emergency University Hospital of Bucharest concerning breast male lesion, benign and malignant, with their histological and immunohistochemically particularities.
METHODS
A four-year period (1st of January 2014 – 31st of December 2017) retrospective study of male breast lesions was done using the pathological report database from the Department of Pathology of the Emergency University Hospital of Bucharest. The authors found 17 cases of male breast lesions (11 benign and six malignant) who underwent surgery. All of them were reviewed in classic stain, HE, and the immunohistochemical expression of certain markers was analysed. Data were collected and processed using Microsoft Excel 2016. We evaluated our cases from a clinical, demographic, histopathological and immunohistochemical point of view.
RESULTS
We identified 17 patients with breast lesions that were surgically cured. Eleven of them were gynaecomastia lesions and six invasive breast carcinoma. All patients were males, with ages ranging from 21 to 83 years old. Most of them were surgically treated in the general surgery department and only a minority were addressed to plastic surgery.
From the medical report, the clinical background of patients with gynaecomastia and breast carcinoma ranged from no medical history to patients with severe diseases such as multiple secretory myeloma or prostatic adenoma that needed long time medical treatment. Despite these facts, all patients had dyslipidemia and an excess of body weight, with or without systemic complications (arterial atheromatous disease, cardiovascular events or imbalanced venous vascular status). All subjects presented with palpable mass that caused aesthetic discomfort (60%) or associated pain (40%); none of them had ulcerated lesions. Most of them were young (8 out of 11 were under 40) and had unilateral disease (we recorded a single bilateral case).
In comparison, male breast carcinomas were found in patients with a history of dyslipidemia and obesity, whose age ranged between 35 and 77, a third of them being under 40. All cases were unilateral and four out of six cases had ulcerated or microscopically invaded skin by tumour cells. A single case was multicentric and had more than a single histotype. Axillary adenopathy was clinically absent in all examined cases and it was microscopically detected in half of the cases analysed by us.
All cases of breast lesions were reviewed, and in those with breast carcinoma, an extended panel of immunohistochemical markers was tested.
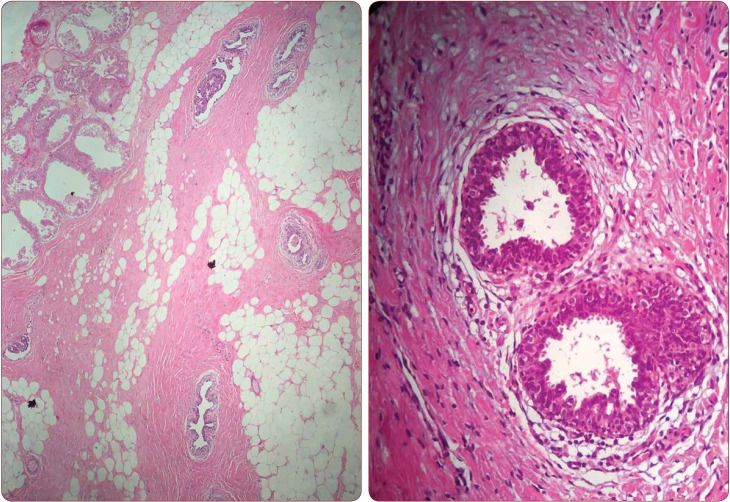
All gynaecomastia lesions were typical, in their florid, fibrotic or mixed stage of evolution; Apocrine metaplasia was a usual finding in our cases (Figure 1).
All breast carcinomas had NST histotype and were found in an advanced stage of the disease (ranging from IIA to IV according to WHO classification), most of them centrally (retro areolar) located, with ulcerated adjacent skin. Tumoral dimensions varied between 2 cm to 3.3 cm. According to Nottingham scale system, almost all male breast carcinomas (five out of six) were moderately differentiated (G2) and a single case, the one with multicentric tumours, was poorly differentiated (G3) (Table 1).
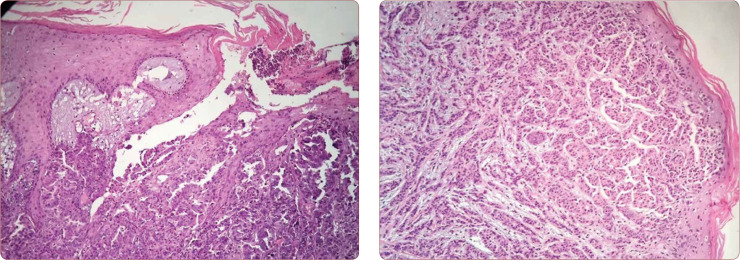
Histologic examination revealed some particularities with unknown significance: an intraductal papilloma close (2 mm) to an NST, PASH and a multicentric multifocal carcinoma with micropapillary differentiation in one tumoral compartment. The last one was the case of a 40-year-old patient with multiple bone and liver metastasis. An important prevalent feature in our series of cases is represented by tumoral invasion of the skin. We found microscopic involvement of the dermis in three out of six cases (Figure 2).
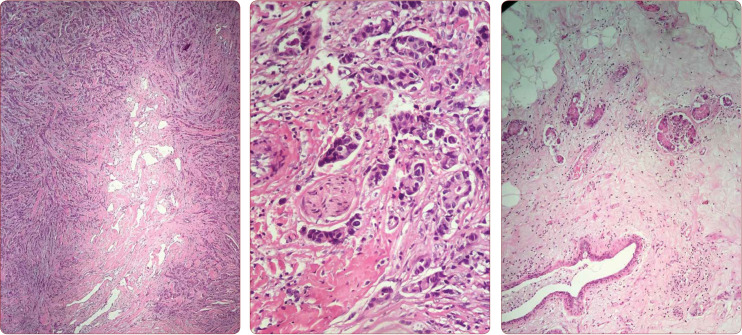
Other histologic features were similar to those noticed in any aggressive invasive carcinoma: perineural invasions, tumoral emboli, infiltrating pattern of growth and desmoplastic reaction (Figure 3).
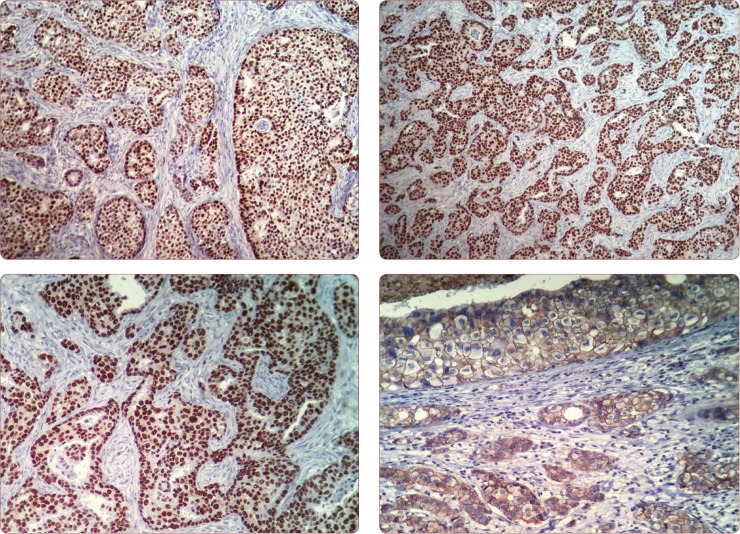
The immunohistochemical examination revealed some interesting findings: all male breast carcinomas were strongly positive for hormonal receptors. We also tested AR and, with a single exception, all cases were expressing it in at least 80% of tumour cells. Because several papers reported about differential diagnosis with metastatic prostatic adenocarcinoma, all our selected cases were tested for PSA. None of them was positive (Figures 4 and 5).
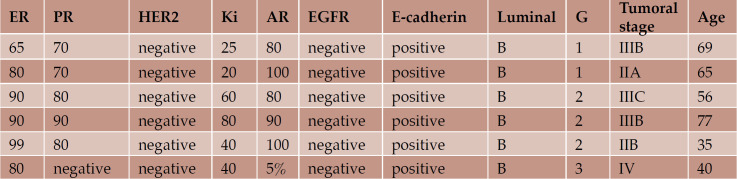
TABLE 1.
Histologic and immunohistochemical assessment of prognostic and predictive breast male carcinoma
FIGURE 1.
Gynaecomastia with apocrine metaplasia (a) and intraductal hyperplasia of usual type (b)
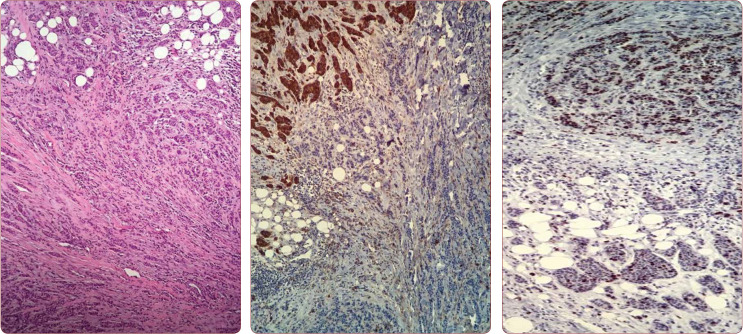
FIGURE 2.
Microscopic invasion of papillary dermis (a) and ulceration of the skin (b) in NST carcinoma
FIGURE 3.
PASH (a); perineural invasion (b); and tumoral emboli (c)
FIGURE 4.
(a) HE of micropapillary differention; (b) Different EMA expression in the two components of the tumour; (c) Ki67 has a higher expression in the micropapillary component
FIGURE 5.
Hormonal expression of no special type (ductal) male breast carcinoma. (a) 10X AR diffuse positive; (b) 20X ER >90% positive; (c) 40X PR >90% positive; (d) 40X E-cadherin positivity in areas with in situ carcinoma and in invasive component
DISCUSSION
Breast disorders in males can be worrisome for both patients (who feel embarrassed and anxious) and doctors (5), who might feel uncertain about differentiating a gynaecomastia from a male breast carcinoma. The last entity is rare, representing less than 1% of all breast carcinomas, usually it is discovered later in its evolution comparing to females, and it tends to have a worse prognostics, mostly because of the delayed initial diagnostic.
Given the similarities with breast carcinoma in women, the same neoadjuvant treatment is used for treatment of the disease: surgery, radiotherapy and hormonal medication when indicated (for ER positive modulators of oestrogen or aromatase inhibitors, for HER2 positive monoclonal antibodies like Herceptin, etc) (5).
This review, based on a four-year experience in a university hospital, aims to highlight the histologic and immunohistochemical particularities in breast male lesions. We noticed a uniformity in terms of histotype and molecular subtype: all our cases were NST and evaluated as luminal B by immunohistochemical studies. However, we could easily see that those similarities were contrasted by important differences such as grade of differentiation (G1 to G3), expression of certain receptors (EMA and AR in the case with micropapillary differentiation), tumoral infiltration or ulceration of adjacent dermis, perineural infiltration or tumoral intravascular emboli and, probably the most important parameter, oncologic stage.
CONCLUSION
For a better prognostic in this exceptionally type of carcinoma, we believe that further studies are necessary, and a better medical education of patients is needed. Although gynaecomastia is the most frequent breast disorder in men, every clinician should perform at least an imagistic investigation whenever a malignant disease is suspected.
Conflicts of interest: none declared.
Financial support: none declared
Acknowledgments: The authors would like towards thank “RESEARCH 62 – Doctorat în context european, contract POSDRU/187/1.5/S/156069” for general suport.
Contributor Information
Oana Cristina VOINEA, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; University Emergency Hospital, Bucharest, Romania.
Monica Mihaela CÎRSTOIU, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; University Emergency Hospital, Bucharest, Romania.
Daniel ION, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; University Emergency Hospital, Bucharest, Romania.
Maria SAJIN, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; University Emergency Hospital, Bucharest, Romania.
Adrian Vasile DUMITRU, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; University Emergency Hospital, Bucharest, Romania.
Oana Mari PATRASCU, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; University Emergency Hospital, Bucharest, Romania.
Dan-Corneliu JINGA, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; University Emergency Hospital, Bucharest, Romania.
Adriana Elena NICA, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania; University Emergency Hospital, Bucharest, Romania.
REFERENCES
- Kauf E. Gynäkomastie im Kindesalter. Fortschr Med. 1998;116:23–26. [PubMed] [Google Scholar]
- Mann NM. Gynecomastia during therapy with spironolactone. . JAMA. 1963;184:778–780. [Google Scholar]
- Andersen JA, Gram JB. Ginecomasty: histological aspects in a surgical material. Acta Pathol Microbiol Immunol Scand. 1982;90:185–190. [PubMed] [Google Scholar]
- Niewoehner CB, Nuttall FQ. Gynecomastia in a hospitalised male population. J Clin Endocrinol Metab. 1979;48:338. doi: 10.1210/jcem-48-2-338. [DOI] [PubMed] [Google Scholar]
- Schanz S, Schreiber G, Zitzmann M, et al. S1 guidelines: Gynecomastia in adults. JDDG. 2017;4:465–472. doi: 10.1111/ddg.13080. [DOI] [PubMed] [Google Scholar]
- Niewoehner CB, Schorer AE. Gynaecomastia and breast cancer in men. . BMJ. 2008;7646:709–713. doi: 10.1136/bmj.39511.493391.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White J, Kearins O, Dodwell D, Horgan K, Hanby AM, Speirs V. Male breast carcinoma: increased awareness needed. . Breast Cancer Res. 2011;5:219. doi: 10.1186/bcr2930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obata A, Okauchi S, et al. Advanced breast cancer in a relatively young man with severe obesity and type 2 diabetes mellitus. J Diabetes Investig. 2017;3:395–396. doi: 10.1111/jdi.12570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streng M, Ignatov A, Reinisch M, Costa S-D, Eggermann H. A comparison of tumor size measurement with palpation, ultrasound and mammography in male breast cancer: first results of the prospective register study. . J Cancer Res Clin Oncol. 2018;2:381–387. doi: 10.1007/s00432-017-2554-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalkhali I, Cho J. Male breast cancer imaging. The Breast Journal. 2015;3:217–218. doi: 10.1111/tbj.12399. [DOI] [PubMed] [Google Scholar]