Abstract
BACKGROUND:
Repetitive traumatic brain injury (RTBI) has gained much attention in this decade, especially in contact sports athletes and military personals. This injury is correlated with early neurodegenerative changes that are marked with the increased of tau protein. Turmeric extract (TE) is a well-known anti-inflammation and antioxidant that decreases tau protein expression in neurodegenerative disease.
AIM:
This study aimed to prove the effect of TE on tau protein level after RTBI.
METHODS:
Forty Sprague Dawley mice were divided into four groups, i.e. negative sham control group, the control group, and two treatment groups. A weight drop model was used by applying a 40-gram mass that was dropped from a 1-meter height onto the vertex of the head, with a total frequency of 12 times, divided into 4 days (day 0, 1, 3, and 7; 3 traumas on each day). TE was given to all treatment groups with 500 mg/kg BW doses once daily. The first treatment group had TE for seven days along the trauma. The second treatment group had pretreatment TE extract, given from seven days before first trauma and continued along the trauma protocol days. Tau protein level was measured on brain and serum using ELISA method.
RESULTS:
There was a significant reduction of tau protein level in both treatment groups compared to trauma group, either in serum or brain, but we also found significant differences regarding brain tau level between the treatment and pretreatment group.
CONCLUSION:
This study might provide evidence of with the role of pretreatment TE in RTBI.
Keywords: Repetitive traumatic brain injury, Turmeric extract, Tau protein
Introduction
Repetitive traumatic brain injury (RTBI), particularly concussion, is frequently happened in some populations, like contact sports athletes and military personals. In a survey involving 222 professional football players, the incident of head impact is very diverse, from four times to 125 times in two weeks. Another report said that around 30% of football players do heading for more than 1000 times annually [1]. In the military, it is estimated that up to 35% of American service personnel in Iraq and Afghanistan have sustained a concussion [2]. Almost all sports-related traumatic brain injury is minor, with spontaneous recovery within days to weeks, even a small number of individuals develop long-lasting and progressive symptoms.
Following traumatic brain injury, even in mildest form, ionic flux, hyper glycolysis, and metabolic uncoupling will result in an energy crisis that can be lasted until 7 to 10 days [3]. The time needed for recover may render the brain vulnerable to the second event. RTBI has been shown they exacerbate the impairment of the brain’s cellular oxidative metabolism similar to severe traumatic brain injury [4]. RTBI itself will result in progressive white matter injury and behavioural dysfunction [5]. Around 17% of individuals with RTBI will develop a constellation of several dysfunctions in behaviour, mood, cognitive, and motoric [6]. Over the last several decades, it is known that these symptoms are correlated with progressive neurodegeneration process that happens in this population. This early neurodegenerative process is named chronic traumatic encephalopathy (CTE). The epidemiology of CTE is unknown since microscopic examination after an autopsy is the only widely accepted way to diagnose this condition [7].
As in another neurodegenerative process, there are several proteinopathies that can be found in CTE. Protein tau is the main proteinopathy. Hyperphosphorylation will dissociate tau from tubulin and expose new phosphorylation site. In this state, protein tau will be insoluble, accumulated into oligomers and neurofibrillary tangles [8]. This condition resembles Alzheimer’s disease (AD), with different in tau distribution. In CTE, tau is most commonly found in the superficial layer, compared to layers III and V in AD [9] [10]. Factors that initiate the development of tau pathology are still unknown but associated with chronic neuroinflammation. Neuroinflammation is a common finding after TBI, especially in moderate and severe TBI. In mild TBI, neuroinflammation is usually short-lived, but RTBI may lead to chronic neuroinflammation due to self-perpetuating inflammatory cycle, including the sustained release of inflammatory mediators. It is shown that microglial neuroinflammation contributes to tau accumulation in CTE [11].
To this date, there is no approved therapy for CTE. Rest and symptomatic therapy are the main treatment approaches. The answer may lie in understanding the principle of tau proteins, where tau proteins aggregate through nucleation, templating, growth, multiplication, and spread. Each of these mechanisms represents a potential target for therapeutic intervention. Therapies that target tau phosphorylation, tau aggregation, and microtubule stabilisation are already in clinical trials [12].
For a long time, practitioners of Ayurvedic, traditional Chinese medicine, and Southeast Asian medicine have used turmeric root extract (TE) for the culinary, religious, and medical condition. Curcumin, the major active compound of TE, is a strong anti-inflammatory and antioxidant properties [13]. The use of curcumin in the AD has been studied extensively. Curcumin reduces accumulation of soluble tau aggregates via inhibition the kinase [14]. Even so, all human clinical trials fail to prove the role of curcumin in the AD, regarding cognitive function [15]. The main problem is curcumin’s low bioavailability [16].
The present study was undertaken to evaluate the effects of turmeric extract in RTBI concerning protein tau level, both in brain and plasma.
Materials and Methods
The subjects of this experiment were 6-8 weeks old Sprague Dawley rats weighing 300-350 g (n = 40). This experimental protocol was approved by an Institutional Ethics Committee in Universitas Sumatera Utara, Medan, Indonesia. The animals were housed with 12 h light/12 h cycle and given access to food and water ad libitum.
The animals were exposed to the weight-drop model of TBI that had been described before [17]. A 40 g mass was dropped from 1 m high unto the vertex. A 2.5 cm metal plate was placed on the vertex to prevent skull fracture. The total cumulative traumas were 12 times, divided 3 times each day on day 0, 1, 3, and 7. We did not use anaesthesia in this protocol.
The rats were randomly allocated into four groups (n = 10) as follow: a control (sham-operated) group, a trauma group, and two group treatments, i.e., treatment 1 (after trauma), and treatment 2 (pretreatment) groups. The control group underwent neither trauma nor TE. The trauma group underwent trauma only, but no TE. The first treatment group received TE for seven days along the trauma and the second treatment group received TE started from seven days before the trauma and along the trauma.
Turmeric extract (Sido Muncul, Indonesia, 18% curcumin) was suspended in distilled water and administered to animals via oral gavage in 2 cc solution. Turmeric extract was given per oral with dose 500 mg/kgBW once daily. The animals were weighed after the acclimatisation. Turmeric extract was administered in the morning, 1 hour before the first trauma.
As a marker of neurodegenerative process, we investigated AT-8 expression. The expression of all markers was investigated on paraffin-embedded sections using the avidin-biotin-peroxidase complex method. Four-millimetre-thick paraffin sections were dewaxed, rehydrated, and microwave for 10 minutes. The endogenous peroxidase activity of the investigated specimens was blocked with 3 per cent H2O2 for 10 minutes, followed by 25 minutes washing with phosphate-buffered saline (PBS). The tissue sections were incubated with normal rabbit serum for 10 minutes, and then the slides were incubated at room temperature with monoclonal mouse AT-8 (Santa Cruz). Sections were washed with PBS and incubated with a secondary antibody for 30 minutes. Sections were washed twice with PBS, developed with 0.05% 3, 3 diamino-benzinetetrahydrochloride for five minutes, and slightly counterstained.
All samples were evaluated by the first author (not blinded to specimen). A positive signal for AT-8 in brain tissue was quantitatively estimated by the distribution of positively stained cells in the cortical brain. Cell counts were carried out using a light binocular microscope with 1000 times magnification in 20 high power fields.
Protein tau level was measured in plasma and brain. Animals were sacrificed one day after the last protocol day. After anaesthesia, rats were decapitated, and brains were dissected. Brain tissues were homogenised in ice-cold homogenization buffer (50 mM Trizma base/HCl buffer, pH 7.4 containing protease inhibitors and 2 ÌM of the phosphatase inhibitor okadaic acid), these brain homogenates were placed in -20°C.
Blood was taken from the left ventricle. After collection of the whole blood, blood was left undisturbed at room temperature for 15-30 minutes. The clot was removed by centrifuging at 1,000-2,000 x g for 10 minutes. The plasma then was maintained at -20°C. Blood and plasma levels of total tau were determined using a commercially available sandwich ELISA system (Cusabio).
Values were expressed as means ± SD. The results were computed statistically using one-way analysis of variance for each group. The Tuckey post hoc testing was performed for intergroup comparisons. A difference was considered significant at the p < 0.05 level.
Results
There was no mortality rate in this protocol. We also did not find a decrease in body weight (Table 1). There was no significant difference regarding body weight on all three groups (Table 1), either in negative sham control group (377.22 ± 29.72 gr vs. 378.44 ± 29.66 gr), trauma group (351.78 ± 29.89 gr vs. 349.33 ± 38.90 gr), or in treatment group (367.89 ± 36.70 gr vs. 357.89 ± 39.89 gr).
Table 1.
Weight changes in subjects (Mean ± SD)
| Group | Day 0 (gr) | Day 7 (gr) | p |
|---|---|---|---|
| Negative sham | 377.22 ± 29.72 | 378.44 ± 29.66 | 0.910 |
| Trauma | 351.78 ± 29.89 | 349.33 ± 38.90 | 0.482 |
| Treatment | 367.89 ± 36.70 | 357.89 ± 39.89 | 0.950 |
Paired t-test. Significant if p < 0.05
There was significantly difference between tau level between the negative sham group and trauma group, either in the brain (Figure 1A) or plasma (Figure 1B). In the negative sham control group, brain protein tau level was 4.21 ± 0.22 pg/ml while plasma tau protein level was 4.36 ± 0.13 pg/ml). There was significant increase of tau protein level following RTBI, either in brain (17.76 ± 2.06 ng/ml, p < 0.05) or plasma (6.16 ± 1.11 ng/ml, p < 0.05).
Figure 1.
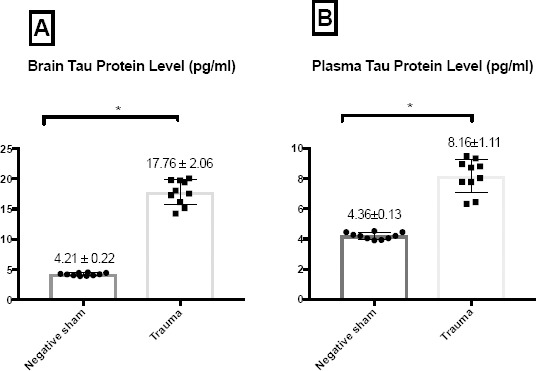
Change in protein tau level following RTBI in the brain (A) and plasma (B). There was significant protein tau level difference between trauma and negative sham group both in the brain and in plasma. Data was shown as Mean ± SD. T-test; significant if p < 0.05
There was a significant decrease of tau protein level in both treatment groups compared to the trauma group, either in the brain (Figure 2A) or in plasma (Figure 2B). In treatment 1 group, the brain tau protein level was 13.31 ± 1.45 pg/ml and the plasma tau protein level was 5.25 ± 0.77 pg/ml.
Figure 2.
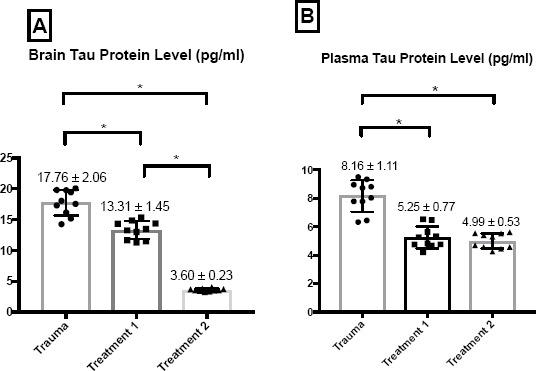
Change in protein tau level after TE supplementation on the brain (A) and plasma (B). There was significant protein tau level difference among either treatment 1 or treatment 2 group with trauma group in brain and plasma. There was also a significant difference regarding protein tau level between treatment 1 and treatment 2 group in bran. The significant difference was not found in plasma. Data was shown as Mean ± SD. T-test; significant if p < 0.05
These were significantly different compared to in trauma group (p < 0.05). In treatment 2 group, either brain tau protein level (3.60 ± 0.23 pg/ml) or plasma tau protein level (4.99 ± 0.53 pg/ml) was also significantly different compared to trauma group (p < 0.05). There was significant brain tau protein level between treatment 1 group and treatment 2 group, which was not seen at the plasma.
Discussion
We reported no mortality rate in this protocol. Xu et al., (2006) report the same finding. The mortality rate is increased along the increased weight and height. With the 50 g-1 m impact, mortality is 18.2%, and with the 60 g-1 m impact, mortality is increased up to 40% [17].
We also did not find a decrease in body weight (Table 1). In this RTBI model, the animals underwent injury schedule at days 0, 1, 3, and 7, with three hits daily. It made a total of 12 TBI events. The use of this model was meant to replicate the pattern of multiple concussion in contact sports athlete. This model did not show evidence of weight loss, compared to the more “severe” model. Samini et al., (2013) find significant weight decrease following a weight-drop model of TBI. The body weight decrease was probably due to injury affecting feeding behaviour and injury to the anterior hypothalamus, even though multi-factorial mechanisms are involved in TBI [18].
Tau is a soluble intracellular protein with little secondary structure. One of protein tau’s functions is to modulate the stability of microtubules. Tau is localised in neuronal cells, but it is not released. Therefore, CSF and blood tau levels in healthy subjects are expected to be low or non-existent.
In pathologic conditions, associated with tauopathy, the soluble protein tau becomes hyperphosphorylated at specific site forming an insoluble form. The brains of some individuals who experience RTBI and develop CTE display tauopathy, predominantly perivascular and in the cortex [19]. Several pathogenic mechanisms have been suggested to contribute to this tau-specific pathology profile, include an imbalance in the activity levels of the tau-specific kinase, dysfunction in protein clearance mechanism, prolonged neuroinflammation, and increased genetic susceptibility (ApoE4 allele) [20]. Increased of protein tau’s level in the brain is reported in neurodegenerative diseases, such as AD (21). High protein tau level is also found in the brain’s interstitial fluid [22], CSF [23], and blood [24].
Neselius et al., (2013) reported that tau plasma levels were significantly increased in Olympic boxers, even without a symptom of concussion [25]. In mild TBI, tau is a poor predictor of CT lesions and post-concussion syndrome [26]. There are inconsistencies regarding the evaluation of protein tau across the literature, i.e. in the form of cleaved-tau, total-tau, and phosphorylated tau. This inconsistency may also be a result of many factors, including the sensitivity and specificity of the tau assays used and the timing of the sample [27].
Penetration of protein tau into the blood suggested that this protein might enter the circulation through the blood-brain barrier (BBB) disruption. Although the integrity of BBB was not assessed, the disruption of BBB in the previous report with the same trauma protocol was minimal [17]. Kane et al., (2012) also reported minimal BBB disruption when using 95-g mass dropped from a 1.5-m height [28]. Other hypotheses that could be proposed are release via glymphatic system or a more complex intracellular transport via macrophages of phagocytic microglia (24). However, these hypotheses require further studies.
However, the mechanism behind tau pathology in repetitive concussive head injury is unknown. Although protein tau is widely used as a biomarker for the diagnosis of CTE, it is not yet clear that tau is the principal mediator of pathogenesis. Protein tau deposition could be just a result of cumulative biochemical changes that happen after RTBI [29].
In this study, treatment groups were divided into two groups. The first treatment group received TE along the trauma for seven days. The second group was pretreatment group that received TE seven days before the trauma was started and continued along the trauma. Protein tau level was significantly lower in either first or second treatment group compared to the trauma group. Nevertheless, protein tau level on the brain was significantly lower on the second treatment group compared to the first. The same difference was not found in plasma (Figure 2A and 2B).
The potential role of TE in degenerative disease is supported by epidemiological evidence. It is reported that people age 70-79 years old in India has a 4.4-fold less prevalence of AD compared to the same population age in the US. The regular intake of turmeric in common Indian diet has been thought as the primary reason for this finding [30]. In Singapore, it was also found that people who regularly ate curry have better cognitive performance than people who rarely or never ate curry [31].
Curcumin was shown to affect protein kinase modulation, such as Akt [32], JNK [33], and GSK-3β [34]. Since protein kinase has a crucial role in protein tau phosphorylation, it may explain why tau protein level was significantly decreased in both treatment group. In neurodegenerative disease, there is also dysfunction in molecular chaperone. Molecular chaperones, such as heat shock proteins (HSPs), play a significant role in the removal of misfolded or mutant proteins. Curcumin affects augmenting expression or function of HSPs in the cell [35]. The anti-inflammatory properties of curcumin also play a significant role in this effect. Curcumin also induces M2 macrophage polarisation in experimental autoimmune myocarditis [36]. M2 macrophages are associated with the production of anti-inflammatory cytokines, increased phagocytic activity, as well as regulation of tissue repair and remodelling [37].
In this research, we found significant protein tau level difference between the first and second treatment group. The second treatment group was a pre-treatment group that received TE for one week before TBI. Curcumin retreatment will induce Nrf2 that is a regulator of cellular resistance to oxidants [38]. In a model of traumatic brain injury, curcumin pre-treatment also decreases malondialdehyde expression, decreases the lesion size, and improves neurological function [18]. This finding might also support the role of curcumin as a neuroprotective agent, not as a treatment agent. It also could explain the reason behind the failure of curcumin in a human study regarding Alzheimer’s disease [15].
There was no significant difference regarding total plasma tau protein level between the two treatment groups. The expression of tau is predominantly in brain, but tau can also be found at both mRNA and protein level in salivary glands and kidney. This is a potential confounder that may help explain the difference of total tau protein level between brain and plasma. In plasma, the half-life of tau appears to be shorter (hours) than in cerebrospinal fluid (weeks) [39].
In conclusion, turmeric extract supplementation reduces tau protein level in brain and plasma following repetitive traumatic brain injury. The most significant effect was found in the pre-treatment group. Further studies to demonstrate the effect of turmeric extract on the clinical outcome will be needed.
Acknowledgements
This project was supported by Basic Research Award from the TALENTA Universitas Sumatera Utara, Indonesia. The authors also acknowledge Wibi Riawan from Biochemistry and Biomolecular Laboratory, Universitas Brawijaya, Malang, Indonesia, for the help in performing animal experimentation and ELISA examination.
Footnotes
Funding: This project was supported by Basic Research Award from the TALENTA Universitas Sumatera Utara, Indonesia
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Hawkes N. Professional football may be linked to brain injuries usually seen in boxing. 2017:811. doi: 10.1136/bmj.j811. [DOI] [PubMed] [Google Scholar]
- 2.Peskind ER, Brody D, Cernak I, McKee A, Ruff RL. Military- and sports-related mild traumatic brain injury: clinical presentation, management, and long-term consequences. J Clin Psychiatry. 2013;74(2):180–8. doi: 10.4088/JCP.12011co1c. quiz188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giza CC, Hovda DA. The New Neurometabolic Cascade of Concussion. Neurosurgery. 2014;75:S24–S33. doi: 10.1227/NEU.0000000000000505. https://doi.org/10.1227/NEU.0000000000000505 PMid:25232881 PMCid: PMC4479139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vagnozzi R, Signoretti S, Cristofori L, Alessandrini F, Floris R, Isgro E, et al. Assessment of metabolic brain damage and recovery following mild traumatic brain injury: a multicentre, proton magnetic resonance spectroscopic study in concussed patients. Brain. 2010;133(11):3232–42. doi: 10.1093/brain/awq200. https://doi.org/10.1093/brain/awq200 PMid:20736189. [DOI] [PubMed] [Google Scholar]
- 5.Longhi L, Saatman KE, Fujimoto S, Raghupathi R, Meaney DF, Davis J, et al. Temporal Window of Vulnerability to Repetitive Experimental Concussive Brain Injury. Neurosurgery. 2005;56(2):364–74. doi: 10.1227/01.neu.0000149008.73513.44. https://doi.org/10.1227/01.NEU.0000149008.73513.44 PMid:15670384. [DOI] [PubMed] [Google Scholar]
- 6.Montenigro PH, Baugh CM, Daneshvar DH, Mez J, Budson AE, Au R, et al. Clinical subtypes of chronic traumatic encephalopathy: literature review and proposed research diagnostic criteria for traumatic encephalopathy syndrome. Alz Res Therapy. 2014;6(5-8):709–17. doi: 10.1186/s13195-014-0068-z. https://doi.org/10.1186/s13195-014-0068-z PMid:25580160 PMCid: PMC4288217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKee AC, Cairns NJ, Dickson DW, Folkerth RD, Keene CD, Litvan I, et al. The first NINDS/NIBIB consensus meeting to define neuropathological criteria for the diagnosis of chronic traumatic encephalopathy. Acta Neuropathol. 2017;131(1):75–86. doi: 10.1007/s00401-015-1515-z. https://doi.org/10.1007/s00401-015-1515-z PMid:26667418 PMCid: PMC4698281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cowan CM, Mudher A. Are tau aggregates toxic or protective in tauopathies? Front Neurol. 2013;4:114. doi: 10.3389/fneur.2013.00114. https://doi.org/10.3389/fneur.2013.00114 PMid:23964266 PMCid: PMC3741634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmidt ML, Zhukareva V, Newell KL, Lee VM, Trojanowski JQ. Tau isoform profile and phosphorylation state in dementia pugilistica recapitulate Alzheimer's disease. Acta Neuropathol. 2001;101(5):518–24. doi: 10.1007/s004010000330. PMid:11484824. [DOI] [PubMed] [Google Scholar]
- 10.McKee AC, Cantu RC, Nowinski CJ, Hedley-Whyte ET, Gavett BE, Budson AE, et al. Chronic Traumatic Encephalopathy in Athletes: Progressive Tauopathy After Repetitive Head Injury. Journal of Neuropathology & Experimental Neurology. 2009;68(7):709–35. doi: 10.1097/NEN.0b013e3181a9d503. https://doi.org/10.1097/NEN.0b013e3181a9d503 PMid:19535999 PMCid: PMC2945234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cherry JD, Tripodis Y, Alvarez VE, Huber B, Kiernan PT, Daneshvar DH, Mez J, Montenigro PH, Solomon TM, Alosco ML, Stern RA. Microglial neuroinflammation contributes to tau accumulation in chronic traumatic encephalopathy. Acta neuropathologica communications. 2016;4(1):112. doi: 10.1186/s40478-016-0382-8. https://doi.org/10.1186/s40478-016-0382-8 PMid:27793189 PMCid: PMC5084333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van den Bedem H, Kuhl E. Molecular mechanisms of chronic traumatic encephalopathy. Current Opinion in Biomedical Engineering. 2017;1:23–30. https://doi.org/10.1016/j.cobme.2017.02.003. [Google Scholar]
- 13.Curcumin: an orally bioavailable blocker of TNF and other pro-inflammatory biomarkers. British Journal of Pharmacology. 2013;169(8):1–21. doi: 10.1111/bph.12131. PMid:23072488 PMCid: PMC3632233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Darvesh AS, Carroll RT, Bishayee A, Novotny NA, Geldenhuys WJ, Van der Schyf CJ. Curcumin and neurodegenerative diseases: a perspective. Expert Opinion on Investigational Drugs. 2012;21(8):1123–40. doi: 10.1517/13543784.2012.693479. https://doi.org/10.1517/13543784.2012.693479 PMid:22668065. [DOI] [PubMed] [Google Scholar]
- 15.Hamaguchi T, Ono K, Yamada M. REVIEW: Curcumin and Alzheimer's Disease. CNS Neuroscience & Therapeutics. 2010;16(5):285–97. doi: 10.1111/j.1755-5949.2010.00147.x. https://doi.org/10.1111/j.1755-5949.2010.00147.x PMid:20406252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anand P, Kunnumakkara AB, Newman RA, Aggarwal BB. Bioavailability of Curcumin: Problems and Promises. Mol Pharmaceutics. 2007;4(6):807–18. doi: 10.1021/mp700113r. https://doi.org/10.1021/mp700113r PMid:17999464. [DOI] [PubMed] [Google Scholar]
- 17.Xu L, Nguyen JV, Lehar M, Menon A, Rha E, Arena J, et al. Repetitive mild traumatic brain injury with impact acceleration in the mouse: Multifocal axonopathy, neuroinflammation, and neurodegeneration in the visual system. Experimental Neurology. 2016;275(Part 3):436–49. doi: 10.1016/j.expneurol.2014.11.004. https://doi.org/10.1016/j.expneurol.2014.11.004 PMid:25450468. [DOI] [PubMed] [Google Scholar]
- 18.Samini F, Samarghandian S, Borji A, Mohammadi G, bakaian M. Curcumin pretreatment attenuates brain lesion size and improves neurological function following traumatic brain injury in the rat. Pharmacology, Biochemistry and Behavior. 2013;110(C):238–44. doi: 10.1016/j.pbb.2013.07.019. https://doi.org/10.1016/j.pbb.2013.07.019 PMid:23932920. [DOI] [PubMed] [Google Scholar]
- 19.McKee AC, Alosco ML, Huber BR. Repetitive Head Impacts and Chronic Traumatic Encephalopathy. Neurosurg Clin N Am. 2016;27(4):529–35. doi: 10.1016/j.nec.2016.05.009. https://doi.org/10.1016/j.nec.2016.05.009 PMid:27637402 PMCid: PMC5028120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ojo J-O, Mouzon B, Greenberg MB, Bachmeier C, Mullan M, Crawford F. Repetitive mild traumatic brain injury augments tau pathology and glial activation in aged hTau mice. Journal of Neuropathology & Experimental Neurology. 2013;72(2):137–51. doi: 10.1097/NEN.0b013e3182814cdf. https://doi.org/10.1097/NEN.0b013e3182814cdf PMid:23334597. [DOI] [PubMed] [Google Scholar]
- 21.Scheltens P, Blennow K, Breteler MMB, de Strooper B, Frisoni GB, Salloway S, et al. Alzheimer's disease. Lancet. 2016;388(10043):505–17. doi: 10.1016/S0140-6736(15)01124-1. https://doi.org/10.1016/S0140-6736(15)01124-1. [DOI] [PubMed] [Google Scholar]
- 22.Marklund N, Blennow K, Zetterberg H, Ronne-Engström E, Enblad P, Hillered L. Monitoring of brain interstitial total tau and beta amyloid proteins by microdialysis in patients with traumatic brain injury. Journal of Neurosurgery. 2009;110(6):1227–37. doi: 10.3171/2008.9.JNS08584. https://doi.org/10.3171/2008.9.JNS08584 PMid:19216653. [DOI] [PubMed] [Google Scholar]
- 23.Franz G, Beer R, Kampfl A, Engelhardt K, Schmutzhard E, Ulmer H, et al. Amyloid beta 1-42 and tau in cerebrospinal fluid after severe traumatic brain injury. Neurology. 2003;60(9):1457–61. doi: 10.1212/01.wnl.0000063313.57292.00. https://doi.org/10.1212/01.WNL.0000063313.57292.00 PMid:12743231. [DOI] [PubMed] [Google Scholar]
- 24.Olczak M, Niderla-Bielińska J, Kwiatkowska M, Samojłowicz D, Tarka S, Wierzba-Bobrowicz T. Tau protein (MAPT) as a possible biochemical marker of traumatic brain injury in postmortem examination. Forensic science international. 2017;280:1–7. doi: 10.1016/j.forsciint.2017.09.008. https://doi.org/10.1016/j.forsciint.2017.09.008 PMid:28942078. [DOI] [PubMed] [Google Scholar]
- 25.Neselius S, Zetterberg H, Blennow K, Randall J, Wilson D, Marcusson J, et al. Olympic boxing is associated with elevated levels of the neuronal protein tau in plasma. Brain Injury. 2013;27(4):425–33. doi: 10.3109/02699052.2012.750752. https://doi.org/10.3109/02699052.2012.750752 PMid:23473386. [DOI] [PubMed] [Google Scholar]
- 26.Ma M, Lindsell CJ, Rosenberry CM, Shaw GJ, Zemlan FP. Serum cleaved tau does not predict postconcussion syndrome after mild traumatic brain injury. The American Journal of Emergency Medicine. 2008;26(7):763–8. doi: 10.1016/j.ajem.2007.10.029. https://doi.org/10.1016/j.ajem.2007.10.029 PMid:18774039 PMCid: PMC2576476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Papa L, Ramia MM, Edwards D, Johnson BD, Slobounov SM. Systematic Review of Clinical Studies Examining Biomarkers of Brain Injury in Athletes after Sports-Related Concussion. J Neurotrauma. 2015;32(10):661–73. doi: 10.1089/neu.2014.3655. https://doi.org/10.1089/neu.2014.3655 PMid:25254425 PMCid: PMC4426313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kane MJ, Angoa-Pérez M, Briggs DI, Viano DC, Kreipke CW, Kuhn DM. A mouse model of human repetitive mild traumatic brain injury. Journal of Neuroscience Methods. 2012;203(1):41–9. doi: 10.1016/j.jneumeth.2011.09.003. https://doi.org/10.1016/j.jneumeth.2011.09.003 PMid:21930157 PMCid: PMC3221913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ojo JO, Mouzon BC, Crawford F. Repetitive head trauma, chronic traumatic encephalopathy and tau: Challenges in translating from mice to men. Experimental Neurology. 2016;275(Part 3):389–404. doi: 10.1016/j.expneurol.2015.06.003. https://doi.org/10.1016/j.expneurol.2015.06.003 PMid:26054886. [DOI] [PubMed] [Google Scholar]
- 30.Chandra V, Pandav R, Dodge HH, Johnston JM, Belle SH, DeKosky ST, et al. Incidence of Alzheimer's disease in a rural community in India The Indo–US Study. Neurology. Lippincott Williams & Wilkins; 2001;57(6):985–9. doi: 10.1212/wnl.57.6.985. https://doi.org/10.1212/WNL.57.6.985. [DOI] [PubMed] [Google Scholar]
- 31.Ng TP, Chiam PC, Lee T, Chua HC, Lim L, Kua EH. Curry Consumption and Cognitive Function in the Elderly. American Journal of Epidemiology. 2006;164(9):898–906. doi: 10.1093/aje/kwj267. https://doi.org/10.1093/aje/kwj267 PMid:168706;99. [DOI] [PubMed] [Google Scholar]
- 32.Gao Y, Li J, Wu L, Zhou C, Wang Q, Li X, Zhou M, Wang H. Tetrahydrocurcumin provides neuroprotection in rats after traumatic brain injury: autophagy and the PI3K/AKT pathways as a potential mechanism. Journal of surgical research. 2016;206(1):67–76. doi: 10.1016/j.jss.2016.07.014. https://doi.org/10.1016/j.jss.2016.07.014 PMid:27916377. [DOI] [PubMed] [Google Scholar]
- 33.Wang YL, Li JF, Wang YT, Xu CY, Hua LL, Yang XP, Geng S, Wang SS, Wang Z, Yin HL. Curcumin reduces hippocampal neuron apoptosis and JNK-3 phosphorylation in rats with Aβ-induced Alzheimer's disease: protecting spatial learning and memory. Journal of Neurorestoratology. 2017;5:117–23. https://doi.org/10.2147/JN.S125567. [Google Scholar]
- 34.Sun J, Zhang X, Wang C, Teng Z, Li Y. Curcumin Decreases Hyperphosphorylation of Tau by Down-Regulating Caveolin-1/GSK-3βin N2a/APP695swe Cells and APP/PS1 Double Transgenic Alzheimer's Disease Mice. Am J Chin Med. 2017;45(08):1667–82. doi: 10.1142/S0192415X17500902. https://doi.org/10.1142/S0192415X17500902 PMid:29132216. [DOI] [PubMed] [Google Scholar]
- 35.Maiti P, Manna J, Veleri S, Frautschy S. Molecular chaperone dysfunction in neurodegenerative diseases and effects of curcumin. BioMed Research International. 2014;2014(1):495091–14. doi: 10.1155/2014/495091. https://doi.org/10.1155/2014/495091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gao S, Zhou J, Liu N, Wang L, Gao Q, Wu Y, Zhao Q, Liu P, Wang S, Liu Y, Guo N. Curcumin induces M2 macrophage polarization by secretion IL-4 and/or IL-13. Journal of molecular and cellular cardiology. 2015;85:131–9. doi: 10.1016/j.yjmcc.2015.04.025. https://doi.org/10.1016/j.yjmcc.2015.04.025 PMid:25944087. [DOI] [PubMed] [Google Scholar]
- 37.Simon DW, McGeachy MJ, Bayır H, Clark RSB, Loane DJ, Kochanek PM. The far-reaching scope of neuroinflammation after traumatic brain injury. Nature Reviews Neurology. 2017;13(3):171–91. doi: 10.1038/nrneurol.2017.13. https://doi.org/10.1038/nrneurol.2017.13 PMid:2818617;7 PMCid: PMC5675525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.González-Reyes S, Guzmán-Beltrán S, Medina-Campos ON, Pedraza-Chaverri J. Curcumin pretreatment induces Nrf2 and an antioxidant response and prevents hemin-induced toxicity in primary cultures of cerebellar granule neurons of rats. Oxidative Medicine and Cellular Longevity. Hindawi. 2013;2013(22):801418–14. doi: 10.1155/2013/801418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zetterberg H. Review: Tau in biofluids - relation to pathology, imaging and clinical features. Neuropathol Appl Neurobiol. 2017;43(3):194–9. doi: 10.1111/nan.12378. https://doi.org/10.1111/nan.12378 PMid:28054371. [DOI] [PubMed] [Google Scholar]


