Abstract
BACKGROUND:
Mother’s mental state during pregnancy is of substantial importance for the mother, but also for the infant and his/her future growth and development. Depressive maternal disorders during pregnancy have a significant influence on the development of the baby during pregnancy as well as on the future development and mother-baby relation, the breastfeeding process and care for the baby.
AIM:
This study aimed to determine the influence of SSRI antidepressant therapy and psychosocial and therapeutic interventions on depression during pregnancy. It was also our aim to determine the relation between severity of depression and sociodemographic characteristics.
METHODS:
The study included 40 women, with diagnosis F32 and F33 according to ICD 10, that is, with severe depressive disorder within depressive episodes or recurrent depressive disorder. Patients were evaluated at the beginning of the treatment and 3 months after antidepressant treatment. They were followed-up for two years.
RESULTS:
The results obtained have shown that a larger number of mothers treated with antidepressant medications, had normal childbirth with the unremarkable condition of both, the mother and the newborn baby.
CONCLUSION:
A well-combined treatment of maternal depression during pregnancy reduces the risk of postpartum depression, which is by itself a prerequisite for normal emotional and behavioural development of the child.
Keywords: Depression, Pregnancy
Introduction
The mental state of the mother during pregnancy is of substantial importance for the mother, but also for the newborn baby and his/her future development.
Depressive maternal disorders during pregnancy have a significant influence on the development of the baby during pregnancy as well as on the future development and mother-baby relation, the breastfeeding process and care for the baby.
It is estimated that in about 7% of women during pregnancy psychic disorders have been detected, and in ¾ of them, a severe depressive condition has been observed.
Although it is considered that the percentage of women with depression during pregnancy is about 18%, still there is no sufficient information for adequate diagnosing and treatment of depression during pregnancy.
Patients who were screened during pregnancy and diagnosed with depression were significantly more likely to ask for an expert opinion and help earlier during the postpartum period than those who were not recognised [1].
An estimated 1-6% of women suffer from major depression while 15-25% have a milder form of depression. Postnatal or postpartum depression is usually associated with depression during pregnancy, especially if it has not been properly treated.
Antidepressant maternal treatment reduces the risk of relapse or disease exacerbation during pregnancy [2].
Over the last two decades, the use of SSRI antidepressant medications during pregnancy has increased and has been given to 2-8% of pregnant women [3].
Nancy Melville in her study about the risk factors for suicide in women reported that 4% of women who died by suicide in Great Britain during the period 1997-2012 were in their perinatal period (a period that is a few weeks before delivery). The most common diagnoses in these women were depression, bipolar disorders and personality disorders [4] [5]. The most common symptoms included depressed mood, self-harm, suicidal ideas and hopelessness. It has to be emphasised that in one-fifth of these women depression was not recognised, that is, they were not examined during their last month of pregnancy.
Therefore, the question of increased psychiatric and medical care of patients during pregnancy and postpartum is imposed.
This study aimed to determine the influence of SSRI antidepressant therapy and psycho-social therapeutic interventions on depression during pregnancy. It was also our aim to define the relation between severity of depression and sociodemographic characteristics.
Material and Methods
The investigation comprised 40 women with dg. F32 or F33 according to ICD 10, that is depressive condition with expressed characteristics manifested during depressive episodes and recurrent depressive disorder.
Patients were of different age, different environment, working status, education, and marital status. They were also tested for heredity presence.
Patients were examined by using the scales for assessment of depression and anxiety, HAMD rating scale for the severity of depression, and HAMA rating scale for the severity of anxiety. In addition to these two scales, the clinically structured interview was used for obtaining data about pregnancy, heredity, previous treatment or use of antidepressant medications and other characteristics.
Patients were treated with SSRI antidepressant therapy initiated in the 10-12 week with gradual reduction or discontinuation of medications by the end of the pregnancy, i.e., in the last 8 gestational weeks.
They were evaluated at the beginning of the treatment and 3 months after antidepressant treatment.
All patients were informed about the treatment and the risk/benefit ratio regarding their physic condition and pregnancy. All of them paid regular visits to a gynaecologist. The follow-up period was two years.
Results
Table 1 presents the sociodemographic characteristics of patients. The larger number of them was at the age over 30 years, with completed higher education, term delivery and without heredity inheritance.
Table 1.
Sociodemographic characteristics of patients
| Age | Count | Per cent |
|---|---|---|
| < 30 | 10 | 24.4 |
| > = 30 | 29 | 70.7 |
| > = 40 | 2 | 4.9 |
| Pregnancy | ||
| I | 29 | 70.7 |
| II | 8 | 19.6 |
| III | 3 | 7.3 |
| IV | 1 | 2.4 |
| Education | ||
| Faculty | 22 | 53.8 |
| Higher | 16 | 39.0 |
| Basic | 3 | 7.2 |
| Employees | ||
| Yes | 22 | 53.7 |
| No | 19 | 46.3 |
| Delivery | ||
| Time | 34 | 82.9 |
| Caesarean section | 4 | 9.8 |
| Before time | 3 | 7.3 |
| Therapy | ||
| With | 4 | 9.8 |
| Without | 37 | 90.2 |
| Heredity | ||
| - | 32 | 78.0 |
| + | 9 | 22.0 |
They were treated with antidepressant medications and the largest number with sertraline and escitalopram. In a smaller number of patients, antipsychotic medications at small doses were added (up to 1 mg risperidone and up to 5 mg olanzapine) as adjuvant therapy (Table 2).
Table 2.
Therapy administered in patients
| Therapy | Count | Per cent |
|---|---|---|
| Escitalopram | 9 | 21.6 |
| Sertraline | 15 | 36.6 |
| Without therapy | 4 | 9.8 |
| Escitalopram, risperidone | 3 | 7.3 |
| Sertraline, risperidone | 5 | 12.2 |
| Escitalopram, risperidone, alprazolam | 1 | 2.4 |
| Venlafaxine | 1 | 2.4 |
| Citalopram | 2 | 4.9 |
| Olanzapine, sertraline | 1 | 2.4 |
| Total | 41 | 100.0 |
The average HAM anxiety score in patients on 0 days was 36.0 ± 5.2 (severe anxiety), and after 3 months the score reduced to 22.2 ± 3.3 (moderate). The difference was 13.8 units. According to t-test the difference was statistically significant for p < 0.05 (p = 0.00000) (Table 3 and Figure 1).
Table 3.
Average HAMA score, 0 days and after 3 months
| Hama | Mean | Std.dv. | N | Diff. | Std.dv. - diff. | T | Df | P | Confidence - 95.0% | Confidence +95.0% |
|---|---|---|---|---|---|---|---|---|---|---|
| 0 day | 36.0 | 5.236 | ||||||||
| After 3m | 22.2 | 3.285 | 41 | 13.8 | 3.831 | 23.153 | 40 | <0.001 | 12.644 | 15.062 |
Figure 1.
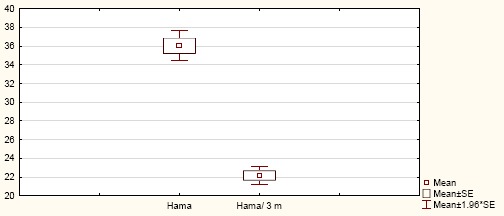
Average HAMA score, 0 days and after 3 months
HAM severe anxiety disorder was registered in 71.0% (22) of patients older than 30 years, and in 30.0% (3) younger than 30 years.
A statistically significant relation was registered between age (over and under 30 y.) and the HAM anxiety score for p < 0.05 (Pearson Chi-square: 6.384, df = 2, p = 0.0410) (Table 3).
HAM severe anxiety disorder was registered in 63.6% (14) of patients with an obtained university degree, in 62.5% (10) with completed high education and 33.3% (1) with primary education. No statistically significant relation was observed between education and HAM anxiety score for p < 0.05 (Pearson Chi-square: 0.893, df = 2, p = 0.639) (Table 3).
HAM severe anxiety disorder was registered in 100% (4) of patients who were delivered with a Cesarean section, in 100% [3] with preterm delivery and 52.9% (18) with term delivery.
No statistically significant relation was registered between mode of delivery and HAM anxiety score for p<0.05 (Pearson Chi-square: 5.402, df=4, p= 0.248) (Table 3).
HAM severe anxiety disorder was registered in 56.3% (18) of patients who were with negative heredity, and in 77.8% (7) in those with positive heredity.
No statistically significant relation was registered between heredity and HAM anxiety score for p < 0.05 (Pearson Chi-square: 1.704, df = 2, p = 0.426) (Table 3).
The average HAM depression score was 33.4 ± 3.5 (severe anxiety) on day 0, and after 3 months it decreased to 20.8 ± 2.1 (moderate). The difference was 12.6 units. According to t-test the difference was statistically significant for p < 0.05 (p = 0.00) (Table 4 and Figure 2).
Table 4.
Average HAMD score, 0 days and after 3 months
| Hamd | Mean | Std.dv. | N | Diff. | Std.dv. - diff. | T | Df | P | Confidence - 95.0% | Confidence +95.0% |
|---|---|---|---|---|---|---|---|---|---|---|
| 0 day | 33.4 | 3.498 | ||||||||
| After 3m | 20.8 | 2.079 | 41 | 12.6 | 2.408 | 33.464 | 40 | 0.00 | 11.825 | 13.345 |
Figure 2.
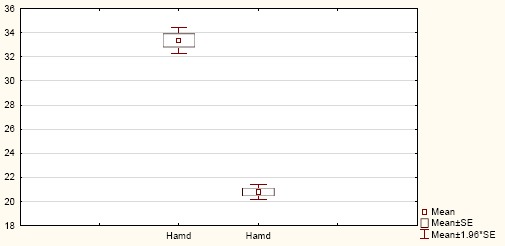
Average HAMD score, 0 days and after 3 months
HAM severe depression disorder was registered in 90.3% (28) of patients older than 30 years and in 60.0% (6) younger than 30 years.
A statistically significant relation was found between age (over and under 30 y.) and HAM depression score for p < 0.05 (Pearson Chi-square: 4.910, df = 1, p = 0.0266) (Table 4).
HAM severe depression disorder was registered in 86.4% (19) of patients with a university degree, in 87.5% (14) of those with completed high education and 33.3% (1) of patients with primary education.
No statistically significant relation was found between level of education and HAM depression score for p < 0.05 (Pearson Chi-square: 5.631, df = 2, p = 0.059) (Table 5).
Table 5.
Relation between HAMA and HAMD versus sociodemographic characteristics
| Characteristics/ Pearson Chi-square | HAMA | HAMD |
|---|---|---|
| Age | P = 0.041080* | P = 0.026698* |
| Pregnancy | P = 0.64087 | P = 0.385549 |
| Education | P = 0.639839 | P = 0.059864 |
| Delivery | P = 0.248447 | P = 0.419394 |
| Heredity | P = 0.426384 | P = 0.590536 |
HAM severe depression disorder was registered in 86.2% (25) of primipara patients and in 75.0% (9) of multipara patients.
No statistically significant relation was found between number of pregnancies and HAM depression score for p < 0.05 (Pearson Chi-square: 0.752, df = 1, p = 0.385) (Table 5).
HAM severe depression disorder was registered in 100% (4) of patients delivered with a Cesarean section, in 100.0% (3) of those who gave preterm childbirth and in 79.4% (27) of patients with normal delivery.
No statistically significant relation was found between mode of delivery and HAM depression score for p < 0.05 (Pearson Chi-square: 1.737, df = 2, p = 0.419) (Table 5).
HAM severe depression disorder was registered in 81.2% (26) of patients with negative heredity and in 88.8% (8) of patients who were found to have positive heredity.
No statistically significant relation was found between heredity and HAM depression score for p < 0.05 (Pearson Chi-square: 0.289, df = 1, p = 0.590) (Table 5).
Discussion
The results obtained have shown a significant improvement in patients about the reduction of depression and anxiety after a 3-month psychopharmacological treatment. A statistically significant relation was found between the severity of depression and anxiety, on the one hand, and age, on the other. Patients older than 30 years presented with more expressed anxiety and depression than the younger pregnant women.
In general, the largest number of primipara patients with depression was at the age over 30 years, which coincides with the trend of getting married after the age of 30/later in life/and raising a family, but it might also be due to the need of secure socioeconomic status.
Although there were more severe depression and anxiety disorders in patients with a university degree in comparison with those with a lower level of education, the difference was not statistically significant. More severe depression manifested in mothers with completed higher education might be a result of their higher awareness and consciousness about their psychological disorders and the need of expert help.
The results have shown that a larger number of pregnant patients treated with antidepressant therapy had a normal delivery with the subsequent normal/unremarkable condition in both, the mother and the newborn infant; only one woman had preterm childbirth, and one had a Cesarean section.
More than 80% of mothers were treated with SSRI antidepressant therapy, and they had normal/uncomplicated pregnancy and delivery, which speaks in favour of the risk/benefit ratio of applying antidepressant therapy.
The task of each therapist/medical expert is to make an individual assessment of the severity of depression during pregnancy, the assessment of the risk for the mother and the newborn infant regarding the eventual damage or benefit from antidepressant medications [1] [2] [6] [7].
Majority of studies point out the differences in psychiatric treatment applied in women with a higher socioeconomic status compared to those with a lower one. Indicators show that women with a higher socioeconomic status were more likely to see a psychiatrist for depression during pregnancy and were treated with SSRI antidepressant medications, whereas those with a lower socioeconomic status were more likely to visit their family/general physicians asking for help about their depression during pregnancy [2].
The results of one research conducted across several European countries with different socioeconomic status indicated that major depression during pregnancy and after delivery was observed in women living in countries with lower socioeconomic status. This leads to the conclusion that these women rarely consult a psychiatrist during pregnancy, which consequently results in a more severe postnatal depression or delayed treatment of postpartum depression. The research has demonstrated that patients who were treated with SSRI medications during pregnancy or patients who had not discontinued their previously started SSRI treatment were at a lower risk of onset or deterioration/ exacerbation of the condition in the postnatal period. It can be concluded that the optimum treatment with SSRI is indispensable in patients with the major depressive disorder [4].
Literature data show that depression during pregnancy is associated with poor care of the mother for her health during pregnancy, including rare visits to a doctor’s office, irregular use of medications, substance abuse, increased risk for preterm birth and low birth weight, and emotional developmental difficulties in the children whose mothers suffered from depression during pregnancy or postpartum [3].
It is considered that depression before and during pregnancy is one of the larger risks for development of postpartum depression, which has a negative effect on the mother/child relation as well as on adequate care for herself and the child [8].
National Institute for Health and Clinical Excellence in the United Kingdom (NICE) guidelines and American Psychiatric Association (APA) recommend CBT (cognitive behavioural therapy) and SSRI antidepressant therapy [9].
Literature suggests that SSRI treatment during pregnancy has no statistically increased risk of giving birth to a child with congenital anomalies than other women [5] [9] [10].
In conclusion, the optimal combined treatment of peripartum depression reduces the risk of postpartum depression, which is a prerequisite for normal emotional and behavioural development of the child.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Venkataesh KK, Nadel H, Blewett D, Freeman MP, Kaimal AJ, Riley LE. Implementation of universal screening for depression during pregnancy: feasibility and impact on obstetric care. Am J Obstet Gynecol. 2016;215(4):517e1–8. doi: 10.1016/j.ajog.2016.05.024. https://doi.org/10.1016/j.ajog.2016.05.024 PMid:27210067. [DOI] [PubMed] [Google Scholar]
- 2.Hanley GE. Socioeconimic status and treatment of depression during pregnancy: a retrospective population –based cohort study in British Columbia, Canada. Arch Womens Ment Health. 2018 doi: 10.1007/s00737-018-0866-6. [DOI] [PubMed] [Google Scholar]
- 3.Anderson P. Untreated Depression in pregnancy Linked to Low Birth Weight. JAMA Psychiatry. 2016. Available from: https://www.medscape.com/viewarticle/864910 .
- 4.Lupattelli A, Twigg MJ, Zagorodnikova K, Moretti ME, Drozd M, Panchaud A, Rieutord A, Juraski RG, Odalovic M, Kennedy D, Rudolf G. Self-reported perinatal depressive symptoms and postnatal symptom severity after treatment with antidepressants in pregnancy: a cross-sectional study across 12 European countries using the Edinburgh Postnatal Depression Scale. Clinical Epidemiology. 2018;10:655. doi: 10.2147/CLEP.S156210. https://doi.org/10.2147/CLEP.S156210 PMid:29922092 PMCid: PMC5997125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Melville NA. Antidepressant Use in pregnancy and Heart Defects: No Links. J Clin Psychiatry. 2016;77:e36–e42. [Google Scholar]
- 6.Brooks M. Antidepressants during pregnancy and psych disorders in kids. 2018. Available from: https://www.medscape.org/viewarticle/887606 .
- 7.Melville NA. Risk factors for suicide in pregnancy identified. 2016. Available from: https://www.medscape.com/viewarticle/857648 .
- 8.Swift D. Pospartum depression affects 1 in 9 new mothers. MMWR. 2017;66(6):153–158. [Google Scholar]
- 9.Koren G, Nordeng H. Antidepressant use during pregnancy and lactation: the benefit-risk ratio. Am J Obstet Gynecol. 2012;207(3):157–163. doi: 10.1016/j.ajog.2012.02.009. https://doi.org/10.1016/j.ajog.2012.02.009 PMid:22425404. [DOI] [PubMed] [Google Scholar]
- 10.Molenaar NM, Brouwer ME, Bockting CL, Bonsel GJ, van der Veere CN, Torij HW, et al. Stop or go?Preventive Cognitive Therapy with Guided Tapering of Antidepressants during Pregnancy. BMC Psychiatry. 2016;16:72. doi: 10.1186/s12888-016-0752-6. https://doi.org/10.1186/s12888-016-0752-6 PMid:26993629 PMCid: PMC4797115. [DOI] [PMC free article] [PubMed] [Google Scholar]


