Abstract
BACKGROUND:
Well-differentiated thyroid carcinoma (DTC) can be locally aggressive, invading aerodigestive tract. The rationale for aggressive surgical resection in this clinical setting is supported by a long-term local control with a positive impact on survival.
CASE REPORT:
A 60-year-old male patient was consulted by a digestive surgeon of unaware thyroid enlargement. Physical and imaging examination showed a suspect of thyroid malignancy. During surgery, we found that a tumour had invaded the anterior side of the trachea. Resection of three tracheal rings was performed, with end-to-end anastomosis. Surgical outcome regarding nervous preservation and parathyroid glands was good as well as cosmetic aspect. During one-year follow-up, no indication of tumour recurrence was found. The management of locally invasive DTC has been controversial yielding the palliative surgery modalities. Advances in surgical technique have given a new perspective of resection in a difficult case. This case report was managed by sleeve resection with end-to-end anastomosis which showed a satisfactory outcome functionally and cosmetically.
CONCLUSION:
Sleeve resection with primary reconstruction of the trachea is a simple one-stage procedure which can adequately address the problem of tracheal invasion by thyroid cancer.
Keywords: Thyroid cancer, Well-differentiated thyroid carcinoma (DTC), Tracheal invasion
Introduction
A well-differentiated thyroid carcinoma can be locally aggressive, invading the aerodigestive tract, such as larynx, trachea, and or oesophagus [1]. In the case where thyroid cancer invaded the trachea, wide resection is needed to achieve minimal residual tumour [2]. In tracheal resection and reconstruction, removal of the invaded airway segment should always be attempted whenever feasible [3].
This case report presented a favourable outcome of a management case of thyroid cancer invading the tracheal with radical resection and end-to-end anastomosis.
Case Report
A 60-year-old male patient was consulted by a digestive surgeon of unware thyroid enlargement. He denied any symptoms of hemoptysis, cough, neck discomfort, nervousness, weight loss, palpitation, or fatigue. He was previously admitted to the digestive department due to cholelithiasis. On neck examination, we palpated a well-defined multinodular painless 5 x 7 cm solid mass. The mass was found to be mobile on swallowing. There was no evidence of cervical lymph nodes enlargement. There was no other remarkable clinical finding.
Cervical x-ray showed inferolateral tracheal deviation to the left side at the level of cervical VII (Figure 1). Ultrasonography showed a large solid mass on the right lobe up to isthmus that caused the tracheal deviation, suspicious of a benign lesion. No metastases lesion was found on chest x-ray examination. Laboratory examination revealed a normal level of thyroid hormone. FNA biopsy showed a follicular neoplasm of the thyroid.
Figure 1.

Cervical x-ray showed inferolateral tracheal deviation
Laparoscopic cholecystectomy was performed, followed by total thyroidectomy. During intubation, the orotracheal tube was inserted easily by the anesthesiologist. During surgery, we found that a tumour had invaded the anterior side of the trachea (Figure 2). Tracheostomy below the tumour level has been decided during the surgery, and a sterile tube was inserted into tracheostomy to replace the orotracheal tube.
Figure 2.
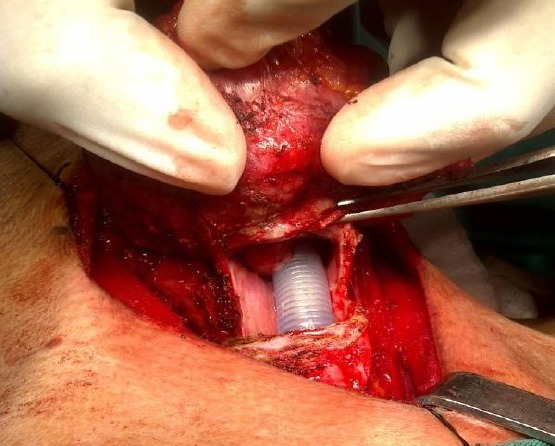
Tumor had invaded the anterior side of the trachea
Intraoperative endoscopy showed invasion of a tumour up to anterior part of the trachea, but the vocal cord was normal. Resection of three tracheal rings (Figure 3) was performed, with end-to-end anastomosis (Figure 4). Bilaterally the recurrent laryngeal nerves were monitored and preserved. Before completing anastomosis, a new orotracheal tube was reinserted to replace the tracheal tube. During neck exploration, we did not find enlarged lymph nodes.
Figure 3.
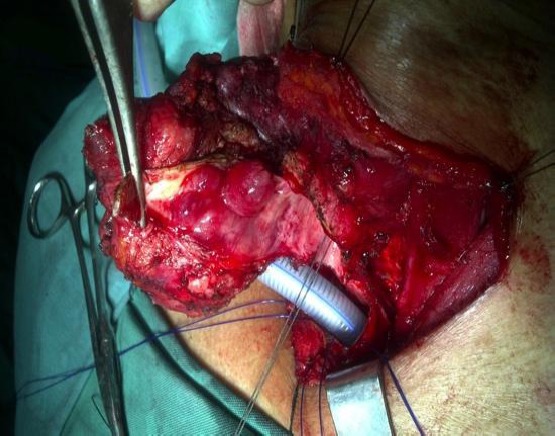
Resection of three tracheal rings
Figure 4.

Sleeve resection with end-to-end anastomosis
Pathology report revealed papillary thyroid carcinoma with tracheal invasion, with a clear margin of the edge of tracheal resection. After resection, the patient was positioned with a fully flexed head (chin to chest position) for about 3 weeks, the orotracheal tube placed for 4 days as the stent, and a nasogastric tube placed for 7 days for feeding. The postoperative condition was uneventful, and the patient recovered satisfactorily.
Surgical outcome regarding preservation of nervous and parathyroid glands as well as the cosmetic aspect was good (Figure 5). During 3-year follow-up, evidence of tumour recurrence and complication was not found (Figure 6).
Figure 5.

Surgical outcome cosmetically was good
Figure 6.

Cervical X-Ray in 3-year follow up
Discussion
Papillary thyroid carcinoma represented the most common type of thyroid cancer (83%) [4]. Mutations occurred in papillary thyroid carcinoma were BRAF/RAS, RET/PTC, PIK3CA, TP53, TSHR, PTEN, GNAS, and CTNNB1 [5]. The most aggressive behaviours were gene mutation of BRAF V600E, a part of MAP kinase cascade, which promotes proto-oncogenes [6]. Besides that, it also caused dysfunction of iodine absorption of follicular cells, blunted the radioiodine therapy [7].
Around 1-8% patients will overcome the aerodigestive tract invasion [8]. From McCaffrey et al., [9] study, it was shown that the most commonly involved aerodigestive were the strap neck muscles, recurrent laryngeal nerve, rings of trachea, oesophagus, lateral neck structures, and larynx. The frequency of thyroid cancer involving tracheal was not well documented in Sanglah General Hospital was not well recorded. Not surprising, patients with thyroid cancer extending to trachea often had bad results due to airway obstruction [10]. This condition dropped 45% of ten years survival in thyroid cancer [1].
Thyroid malignancy was shown to invade directly to the thyroid cartilage. In this case report, the invasion was found to the anterior side. This can occur through invasion from isthmus or paratracheal lymph nodes, until extracapsular extension [11]. The invasion of trachea occurred gradually from outer layer to inner layer [12].
This case report was categorized in stage IV according to Shin et al., [13] classification for thyroid cancer involving aerodigestive tract and recommended a complete resection. Pappalardo et al., [14] reported that the survival for stage IV thyroid cancer with aerodigestive tract involvement ranged from 18 to 108 months. However, by MACIS score calculation, this case has = (0.08 x age) + (0.3 x tumor size in cm) + 1 (if incomplete excision) + 1 (if locally invasive) + 3 (if distant metastases) = (0.08 x 60) + (0.3 x 7) = 4.8 + 2.1 = 6.9, thus the survival was 89% [15].
Generally, the resection surgery for thyroid cancer aims to reach the complete excision and control the invasion [16]. The best goal is to preserve all the thyroid health structures [17]. However, the survival rate was only 15-39% with 1.2% mortality, worse that incomplete resection [14], [15]. The most common surgical complications were airway obstruction, infection, bleeding, and anastomotic dehiscence [18]. This made the surgery for locally-invasive DTC has been controversial. Thus, palliative surgery had been the most common surgical procedure or treatment for many years. Nowadays, advances in surgical techniques have improved the radicality of surgery, which excellent preservation of vocal cord function and survival satisfactory [19].
Various methods have been carried out by surgeons for reaching the best outcome for the patient. The there most common procedure was two stages surgery for thyroid carcinoma invading the trachea [20]. First was resection of a tumour and second was reconstruction closure of the tracheal defect using cartilage graft and musculocutaneous or latissimus dorsi flap [21]. However, reconstruction of the tracheal wall is challenging due to unstable tracheal lumen [22]. Another method for simpler cases was segmental resection of the tracheal and end to end anastomosis. If the case were too advanced, total laryngectomy and permanent tracheotomy would likely to be done [23].
Pappalardo et al., [14] reported a successful radical resection of extrathyroidal thyroid cancer which invaded the tracheal lumens until the blood vessels with 9 years of satisfactory survival and functionality. Shigemitsu et al., [22] reported a successful case also with a partial tracheal resection with latissimus dorsi musculocutaneous flap reconstruction. Endo et al., [23] reported that a single staged thyroidectomy with auricular cartilage and sternohyoid reconstruction successfully cured the patient [24]. In Tsai et al., [24] study, thyroid and en bloc tracheal resection with end to end anastomosis is the treatment of choice of a thyroid tumour invading the trachea. This method showed the highest survival rate, reported to be 78%.
Patients with inoperable thyroid cancers are usually treated by RAI (radioactive iodine) therapy and external beam radiation therapy [25]. The surgery method needs to be tailored to each in an individual with three main principles, such as to accomplish the possible complete resection, prevent airway obstruction, and prolonged the survival. An incomplete tumour resection has a bad outcome and increases the risk of recurrent. Tangential tumour resection (shaving) is indicated if no invasion in transmural of the trachea.
Due to the anterior invasion of the tumor, we decided to carry out resection of three tracheal rings. End to end anastomosis was performed to ensure the intact vascularity around. Bilaterally the recurrent laryngeal nerves were carefully monitored and preserved. Surgical outcome regarding preservation of nervous and parathyroid glands as well as cosmetic aspect was good. This case report will add information of another resection with end-to-end anastomosis with a favourable outcome.
The successful management of well-differentiated thyroid cancer requires meticulous preparation, because of the vitality of the surrounding structures. The goal of resection was to achieve the larger extension as possible with restoration of functionality for the patient.
In conclusion, sleeve resection with primary reconstruction of the trachea is a simple one-stage procedure which could adequately address the problem of tracheal invasion by thyroid cancer.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Price DL, Wong RJ, Randolph GW. Invasive thyroid cancer: management of the trachea and esophagus. Otolaryngol Clin North Am. 2008:1155–8. doi: 10.1016/j.otc.2008.08.002. https://doi.org/10.1016/j.otc.2008.08.002 PMid:19040976 PMCid: PMC2750808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grillo HC, Zannini P. Resectional management of airway invasion by thyroid carcinoma. Ann Thorac Surg. 1986;42:287–98. doi: 10.1016/s0003-4975(10)62737-3. https://doi.org/10.1016/S0003-4975(10)62737-3. [DOI] [PubMed] [Google Scholar]
- 3.Yang CC, Lee CH, Wang LS. Resectional treatment for thyroid cancer with tracheal invasion: A long-term follow-up study. JAMA Surgery. 2000;135:704–7. doi: 10.1001/archsurg.135.6.704. [DOI] [PubMed] [Google Scholar]
- 4.Tuttle RM, Ball DW, Byrd D. Thyroid carcinoma. J Natl Compr Canc Netw. 2010;8:1228–74. doi: 10.6004/jnccn.2010.0093. https://doi.org/10.6004/jnccn.2010.0093 PMid:21081783. [DOI] [PubMed] [Google Scholar]
- 5.Nikiforova MN, Wald AI, Roy S, Durso MB, Nikiforov YE. Targeted next-generation sequencing panel (ThyroSeq) for detection of mutations in thyroid cancer. J Clin Endocrinol Metab. 2013;98:1852–60. doi: 10.1210/jc.2013-2292. https://doi.org/10.1210/jc.2013-2292 PMid:23979959 PMCid: PMC3816258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xing M, Westra WH, Tufano RP. BRAF mutation predicts a poorer clinical prognosis for papillary thyroid cancer. J Clin Endocrinol Metabol. 2005;90:6373–9. doi: 10.1210/jc.2005-0987. https://doi.org/10.1210/jc.2005-0987 PMid:16174717. [DOI] [PubMed] [Google Scholar]
- 7.Ito Y, Yoshida H, Kihara M, Kobayashi K, Miya A, Miyauchi A. BRAF mutation analysis in papillary thyroid carcinoma: is it useful for all patients? World J Surg. 2013;38:679–87. doi: 10.1007/s00268-013-2223-2. https://doi.org/10.1007/s00268-013-2223-2 PMid:24052184. [DOI] [PubMed] [Google Scholar]
- 8.Brauckhoff M, Dralle H. Extrathyroidal thyroid cancer: results of tracheal shaving and tracheal resection. Chirurg. 2011;82:134–40. doi: 10.1007/s00104-010-1975-6. https://doi.org/10.1007/s00104-010-1975-6 PMid:21153528. [DOI] [PubMed] [Google Scholar]
- 9.McCaffrey TV, Bergstralh EJ, Hay ID. Locally invasive papillary thyroid carcinoma 1940-1990. Head Neck. 1994;16:165–72. doi: 10.1002/hed.2880160211. https://doi.org/10.1002/hed.2880160211 PMid:8021137. [DOI] [PubMed] [Google Scholar]
- 10.Pearson FG, Cooper JD, Nelems JM, Van Nostr, and AWP. Primary tracheal anastomosis after resection of the cricoid cartilage with preservation of recurrent laryngeal nerves. J Thorac Cardiovasc Surg. 1975;70:806–16. PMid:118627;2. [PubMed] [Google Scholar]
- 11.Urken ML. Prognosis and management of invasive well-differentiated thyroid cancer. Otolaryngol Clin N Am. 2010;43:301–28. doi: 10.1016/j.otc.2010.02.002. https://doi.org/10.1016/j.otc.2010.02.002 PMid:20510716. [DOI] [PubMed] [Google Scholar]
- 12.Kim H, Jung HJ, Lee SY, Kwon TK, Kim KH, Sung MW, et al. Prognostic factors of locally invasive well-differentiated thyroid carcinoma involving the trachea. Eur Arch Otorhinolaryngol. 2016;273:1919–26. doi: 10.1007/s00405-015-3724-4. https://doi.org/10.1007/s00405-015-3724-4 PMid:26198285. [DOI] [PubMed] [Google Scholar]
- 13.Shin DH, Mark EJ, Suen CSH, Grillo HC. Pathologic staging of papillary carcinoma of the thyroid with airway invasion based on the anatomic manner of extension to the trachea: a clinicopathologic study based on 22 patients who underwent thyroidectomy and airway resection. Human Pathology. 1993;24:866–70. doi: 10.1016/0046-8177(93)90136-5. https://doi.org/10.1016/0046-8177(93)90136-5. [DOI] [PubMed] [Google Scholar]
- 14.Pappalardo V, La Rosa S, Imperatori A, Rotolo N, Tanda ML, Sessa A, et al. Thyroid cancer with tracheal invasion: a pathological estimation. Gland Surg. 2016;5:541–5. doi: 10.21037/gs.2016.10.02. https://doi.org/10.21037/gs.2016.10.02 PMid:27867870 PMCid: PMC5106376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCaffrey JC. Aerodigestive tract invasion by well-differentiated thyroid carcinoma: diagnosis, management, prognosis, and biology. Laryngoscope. 2006;116:1–11. doi: 10.1097/01.MLG.0000200428.26975.86. https://doi.org/10.1097/01.MLG.0000200428.26975.86 PMid:16481800. [DOI] [PubMed] [Google Scholar]
- 16.Rotoko N, Cattoni M, Imperatori A. Complications from tracheal resection for thyroid carcinoma. Gland Surg. 2017;6:574–8. doi: 10.21037/gs.2017.08.05. https://doi.org/10.21037/gs.2017.08.05 PMid:29142850 PMCid: PMC5676159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shenoy AM, Burrah R, Rao V, Chavan P. Tracheal resection for thyroid cancer. J Laryngol Otol. 2012;126:594–7. doi: 10.1017/S002221511200059X. https://doi.org/10.1017/S002221511200059X PMid:22494608. [DOI] [PubMed] [Google Scholar]
- 18.Piazza C, Del Bon F, Barbieri D, Grazioli P, Paderno A, Perotti P, et al. Tracheal and Crico-Tracheal Resection and Anastomosis for Malignancies Involving the Thyroid Gland and the Airway. Ann Otol Rhinol Laryngol. 2016;125:97104–6. doi: 10.1177/0003489415599000. https://doi.org/10.1177/0003489415599000 PMid:26296930. [DOI] [PubMed] [Google Scholar]
- 19.Chernichenko N, Shaha AR. Role of tracheal resection in thyroid cancer. Curr Opin Oncol. 2012;24:29–34. doi: 10.1097/CCO.0b013e32834d6dd7. https://doi.org/10.1097/CCO.0b013e32834d6dd7 PMid:22048058. [DOI] [PubMed] [Google Scholar]
- 20.Ebihara M, Kishimoto S, Hayashi R, Miyazaki M, Shinozaki T, Daiko H, et al. Window Resection of the Trachea and Secondary Reconstruction for Invasion by Differentiated Thyroid Carcinoma. Auris Nasus Larynx. 2011;38:271–5. doi: 10.1016/j.anl.2010.09.003. https://doi.org/10.1016/j.anl.2010.09.003 PMid:21093183. [DOI] [PubMed] [Google Scholar]
- 21.Nakahira M, Nakatani H, Takeuchi S, Higashiyama K, Fukushima K. Safe Reconstruction of a Large Cervico-Mediastinal Tracheal Defect with a Pectoralis Major Myocutaneous Flap and Free Costal Cartilage Grafts. Auris Nasus Larynx. 2006;33:203–6. doi: 10.1016/j.anl.2005.09.009. https://doi.org/10.1016/j.anl.2005.09.009 PMid:16289423. [DOI] [PubMed] [Google Scholar]
- 22.Shigemitsu K. Naomoto Y, Haisa M, Yamatsuji T, Noguchi H, Kataoka M, et al. Case of Thyroid Cancer Involving the Trachea: Treatment by Partial Tracheal Resection and Repair with a Latissimus Dorsi Musculocutaneous Flap. Jpn J Clin Oncol. 2000;30:235–8. doi: 10.1093/jjco/hyd053. https://doi.org/10.1093/jjco/hyd053 PMid:10857502. [DOI] [PubMed] [Google Scholar]
- 23.Endo K, Ueno T, Kondo S, Wakisaka N, Murono S, Yoshizaki T. Successful Treatment of Thyroid Carcinoma Invading the Trachea as a Single-Stage Procedure: A Case Report. Case Reports in Clinical Medicine. 2015;4:50–4. https://doi.org/10.4236/crcm.2015.42012. [Google Scholar]
- 24.Tsai YF, Tseng YL, Wu MH. Aggressive resection of the airway invaded by thyroid carcinoma. Br J Surg. 2005;92:13827–9. doi: 10.1002/bjs.5124. https://doi.org/10.1002/bjs.5124 PMid:16044411. [DOI] [PubMed] [Google Scholar]
- 25.Honings J, Stephen AE, Marres HA, Gaissert HA. The role of oral RAI in airway invasion has not been investigated separately. The management of thyroid carcinoma invading the larynx or trachea. Laryngoscope. 2010;120:682–9. doi: 10.1002/lary.20800. https://doi.org/10.1002/lary.20800 PMid:20213659. [DOI] [PubMed] [Google Scholar]


