Abstract
BACKGROUND:
The impact of resiliency on professional burnout in nurses has been evaluated in several studies.
AIM:
This meta-analysis was conducted to examine the effect of resiliency on different aspects of nurses’ professional burnout.
MATERIAL AND METHODS:
Publications were identified through targeted literature review in national and international databases between 1980-2017, in Persian and English. Two independent coders assessed and extracted articles. Data analysis was done by a random effects model. Study heterogeneity was measured by the I2 test. The data were analysed by STATA software v. 14.
RESULTS:
Initially, 227 articles were extracted. After titles and abstract screening, 108 articles were selected for full-text review. Only five of them had the necessary inclusion criteria for analysis. The meta-analysis performed on these observational studies showed that the correlation between resiliency and burnout was -0.57 with a 95% confidence interval of -0.354 to -0.726.
CONCLUSION:
Regarding the inverse relationship between resiliency and burnout, it is recommended to plan for the interventions that can improve the resilience of nurses against burnout. Conducting interventional and resilient training courses for nurses in nursing education can be considered.
Keywords: Resiliency, Burnout, Nursing, Meta-analysis, Iran
Introduction
Occupation is one of the most important sources of stress. If stress persists more than usual, it can endanger the person’s health by causing physical, psychological, and behavioural harms [1] [2]. Among all types of jobs, health care providers, especially nurses, are commonly known as high-risk groups for stress and burnout [3], and they experience various forms of stress and physical and mental harms [4] [5].
Depression, anxiety, and fatigue are common problems in this occupational group. In various studies, the level of stress among nurses have been reported to be 90% [6]. The Institute for Occupational Health and Safety, which studies the relationship between mental illnesses and occupational stress, reports that among the 136 studied professions, nurses ranked 22 regarding acceptance of occupational, psychological problems. The US National Occupational Safety Administration has also introduced nursing among the top 40 high-stress professions [7].
Nurses are one of the important pillars of health care organisations, and any shortcomings in this group will have irreparable consequences due to their important role in patient treatment. Therefore, paying attention to the factors affecting the performance of nurses in this area is of paramount significance. Nurses are exposed to the highest levels of occupational harms, including burnout, due to exposure to physical, psychological, and emotional stressors [8] [9] [10]. In some studies, the rate of burnout in nurses has been reported four times higher than other service occupations [11].
Burnout in nurses jeopardises patient recovery more than any other factor [12]. This problem is one of the main factors in reducing efficiency, loss of human resources, and physical and mental health problems [13] [14]. Experts believe that instead of focusing solely on the sources of stress, it is better to equip nurses with personal, psychological, and personal capacities.
One of the most important human abilities that facilitates effective adaptation to risk factors and is a good strategy for promoting mental health in individuals is the resiliency attribute [15] [16]. Personality characteristics such as resiliency act as a barrier against stressful events and work-related mental health problems, such as burnout [13]. Resiliency helps individuals to face and adapt to difficult living conditions and protect them from mental disorders and life problems. Resilient individuals have a high degree of adaptation to environmental stressors in their lives [17]. Nurses will also be able to withstand many psychological pressures using the resiliency element [18].
One of the most important goals of meta-analyses is to provide a precise and valid result due to an increase in the sample size through the combination of various studies, thus, reducing confidence interval and solving problems arising from the controversial results of former studies. According to numerous studies with different findings, in this study, we systematically reviewed the findings of previous studies and combined their data to obtain an accurate estimate of the relationship between resiliency and burnout in nurses. For any kind of planning and policy-making to prevent conditions such as burnout and promote resilience in nurses, a precise estimation of the target group is necessary. Given the fact that so far there have been a plethora of studies on the relationship between resiliency and burnout, it seems that accumulating their results in the form of a meta-analysis can help generalise their findings. For this reason, the present study aimed to investigate the relationship between resiliency and burnout in nurses in the form of meta-analysis.
Material and Methods
This meta-analysis was undertaken to investigate the association between resiliency and burnout in nurses in 2017.
We systematically searched SID, Magiran, Irandoc, Medlib, and IranMedex databases, as well as Science Direct, ProQuest, Embase, MEDLINE, SCOPUS, CINAHL, and The Web of Science for studies on nurses’ resiliency and burnout that were completed by October 2017. The following keywords were used to select the studies on the relationship between resiliency and burnout in nurses: (Resiliency OR resilience) AND (burnout OR “occupational burnout” OR “occupational burnout syndrome” OR OBS) AND (nurse) AND (Iran). For example PubMed database was searched using the following script:
((((((Resiliency[All Fields] OR resilience[All Fields]) AND burnout[All Fields]) OR (“burnout, professional “[MeSH Terms] OR (“burnout” [All Fields] AND “professional” [All Fields]) OR “professional burnout” [All Fields] OR (“occupational” [All Fields] AND “burnout” [All Fields]) OR “occupational burnout” [All Fields])) OR ((“burnout, professional” [MeSH Terms] OR (“burnout” [All Fields] AND “professional” [All Fields]) OR “professional burnout” [All Fields] OR (“occupational” [All Fields] AND “burnout” [All Fields]) OR “occupational burnout” [All Fields]) AND (“syndrome” [MeSH Terms] OR “syndrome”[All Fields]))) OR OBS [All Fields]) AND (“nurses” [MeSH Terms] OR “nurses” [All Fields] OR “nurse” [All Fields])) AND (“iran” [MeSH Terms] OR “iran” [All Fields]).
The Persian equivalents of these keywords were also used in Persian databases. At this stage of the study, all the studies in which the mentioned keywords were used in the title or abstract were included in the list for review. Also, the references list of the included articles was also examined for further articles.
Quality of the selected articles was also evaluated using the STROBE checklist. This checklist contains 22 items that examine all parts of a study. To reduce bias and error in data collection, two researchers independently screened the articles. After the initial review and deleting the duplicate and unrelated articles, finally, five studies were entered in the final analysis.
In cases where the researchers disagreed in choosing an article, the reasons for the disagreement were discussed and, if the issue was not resolved, the article was referred to a third researcher expert in the field of meta-analysis. Finally, we investigated the studies that were on the relationship between resiliency and burnout in nurses.
The inclusion criteria consisted of Persian or English-language studies, observational studies, available full-text articles, and studies on nurses working in medical centres. Considering that the subject of this study was to investigate the relationship between resiliency and burnout among nurses, studies on nursing students due to lack of employment, studies that examined burnout among other health care providers, interventional studies, and studies that did not use Conner-Davidson or Mason’s tools for measuring resiliency were excluded.
We considered articles that addressed the correlation coefficient between the two variables of resiliency and burnout or Z-test between the two. Based on the inclusion and exclusion criteria, articles collected by the two authors (independent of each other) were examined once based on the title and abstract, and the second round the full text of the articles was considered for eligibility. To record the information, a form was used including the variables of the first author of the article, the year of publication, study setting, type of study, sample size, data collection tool, the correlation between resiliency and burnout, and the correlation between resiliency and dimensions of burnout.
Concerning the Connor-Davidson questionnaire, it can be said that this resiliency scale has 25 items rated using a 5-point Likert scale (i.e., never, rarely, theoretically, sometimes, and always) with the minimum and maximum possible scores of 25 and 125, respectively. This scale was customised for use in Iran by Mohammadi. He distributed the questionnaire among 248 individuals, and its reliability was confirmed by measuring the internal consistency of Cronbach’s alpha (89%) (19). The other questionnaire was the Maslach Burnout Questionnaire, which is used to measure occupational burnout. This questionnaire consists of 22 separate items and includes three dimensions that include emotional exhaustion, depersonalization, and feeling of personal incompetence [20].
In this meta-analysis, data analysis was performed using the random effects model (Mantel-Haenszel). The standard error of the mean for each study was estimated using the normal distribution. The effect size in each study was estimated using the formula  , where r is the correlation coefficient in each study. To convert Z to r, the formula
, where r is the correlation coefficient in each study. To convert Z to r, the formula  was employed. After conversion of Z scores, the size of the joint effect was estimated using a random effects model. In order to investigate any heterogeneity in selected studies, Q-Cochran test and I2 index (I2 index in three classes 0.025 [low heterogeneity], 0.025-0.075 [medium heterogeneity], and more than 0.075 [high heterogeneity]) were used. P < 0.01 and I2 > 75% were considered as significant heterogeneity of studies. Sensitivity analysis was used to investigate the effect of each study on the final result. All the statistical analyses were performed using STATA software, version 14.
was employed. After conversion of Z scores, the size of the joint effect was estimated using a random effects model. In order to investigate any heterogeneity in selected studies, Q-Cochran test and I2 index (I2 index in three classes 0.025 [low heterogeneity], 0.025-0.075 [medium heterogeneity], and more than 0.075 [high heterogeneity]) were used. P < 0.01 and I2 > 75% were considered as significant heterogeneity of studies. Sensitivity analysis was used to investigate the effect of each study on the final result. All the statistical analyses were performed using STATA software, version 14.
In this study, all investigations in the area of the relationship between burnout and resiliency were based on the four steps of PRISMA. In the first stage of the search, 227 articles were retrieved. After screening the titles and abstracts of the articles, 119 articles were excluded from the study due to irrelevance to the research topic and being reviews. Finally, the full text of 108 articles was studied and, if the article met the inclusion criteria, the necessary information was extracted. In this phase, 103 studies were excluded due to irrelevance to the research question, being replications of other studies, lack of homogeneity of resiliency tools, and unreliable data analysis. In the end, only five articles met the required criteria to enter the analysis (Figure 1).
Figure 1.
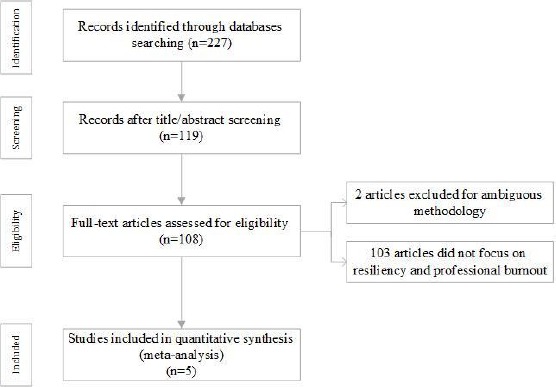
PRISMA flowchart for article identification and exclusion
In this meta-analysis, five studies published between 2009 and 2016 with a total sample size of 1169 people, investigated the relationship between resiliency and burnout in nurses. Specifications of the above studies are listed in Table 1.
Table 1.
Summary of studies characteristics
| No | First author | Year | Sample size | Location | Correlation | Z score | P-value |
|---|---|---|---|---|---|---|---|
| 1 | Khodabakhshi | 2016 | 140 | Semnan | -0/685 | -0/838 | <0/0001 |
| 2 | Momeni | 2010 | 426 | Kermanshah | -0/602 | -0/708 | <0/0001 |
| 3 | Amini | 2013 | 304 | Tehran | -0/355 | -0/371 | <0/001 |
| 4 | Arbabshastan | 2014 | 175 | Shiraz | -0/208 | -0/211 | <0/0001 |
| 5 | Shakerinia | 2010 | 124 | Rasht | -0/806 | -1/112 | <0/0001 |
In this study, considering that the heterogeneity index of studies was I2=95.4%, the random effects model was used to estimate the joint correlation coefficient between resiliency and burnout.
The highest and lowest sample sizes were related to the study by Momeni (2010) with 426 subjects [21] and Shakerinia (2010) with 124 cases [22], respectively. The general correlation between resiliency and burnout was calculated using the random effects model and after converting the z-scores (-0.57) with confidence interval (95% CI: -0.726 to -0.354; Figure 2).
Figure 2.
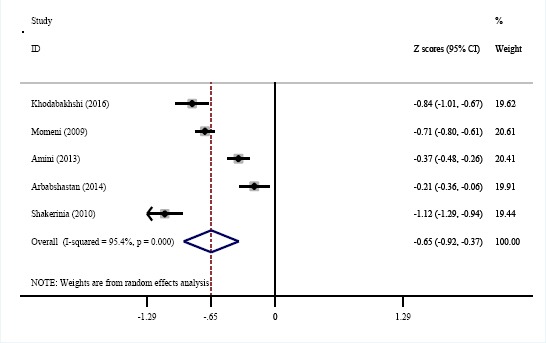
Association between resiliency and professional burnout
According to the results of correlation analysis between resiliency and burnout dimensions, the general correlation between resiliency and emotional exhaustion was -0.55 (95% CI: -0797 to -0.149; Figure 3), correlation with the depersonalization dimension was -0.388 (95% CI: -0.537 to -0.216; Figure 4), and correlation with the incompetence dimension was -0.254 (95% CI: -0.422 to -0.039; Figure 5).
Figure 3.
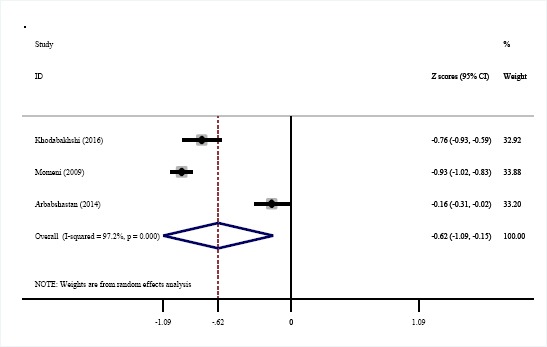
Association between resiliency and emotional exhaustion
Figure 4.

Association between resiliency and depersonalization
Figure 5.
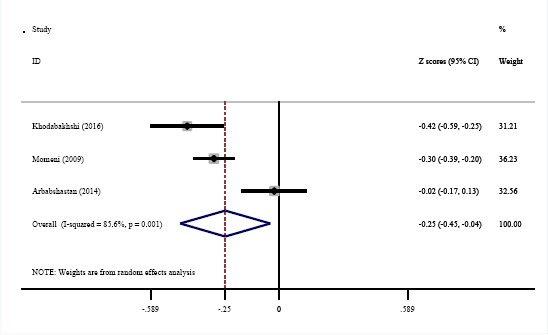
Association between resiliency and personal incompetence
In this study, the result of the sensitivity analysis showed that none of the studies alone had a significant impact on the outcome.
Discussion
The findings of this study that aimed to investigate the relationship between resiliency and burnout in the nursing community in Iran showed that the correlation between resiliency and burnout in Iranian nurses was -0.57. The results of the study by Rushton et al., (2015), which aimed to investigate the relationship between and burnout in nurses, showed that resiliency has a high correlation with the dimensions of emotional exhaustion, depersonalization, and personal incompetence, which is consistent with the findings of this research [23].
Nurses use resilient behaviours in dealing with work problems to maintain their mental health and to go through negative experiences more easily and turn them into positive ones to feel burnout less [24]. The results of a study by Guo et al., in China indicated a weak correlation between resiliency and burnout in nurses [25]. The findings of various studies have also supported the relationship between resiliency and occupational burnout among nurses [26] [27]. Warelow et al., (2007) proposed that nurses who use resilient behaviours are less likely to develop burnout [24]. Jackson et al., (2008) studied resilience as a strategy for survival and growth in threatening work environments. They concluded that resilience is a kind of ability to adapt positively to problems and hardships, and it is positively associated with creating positive professional relationships, maintaining positivity, developing emotional insight, achieving balance in life, and promoting spirituality in nursing [18].
The results of Olson et al., (2015) showed that resiliency only has a significant negative correlation with emotional exhaustion and does not correlate with the other two dimensions [28]. In a cross-sectional study, Guo et al. investigated the correlation between resiliency and burnout in nurses in China. They noted a correlation between resiliency with all the three aspects of burnout in nurses [25)]. The results of the study by McCain et al., on physicians revealed a negative correlation between resiliency and burnout [29]. Accordingly, it can be stated that resiliency (successful coping capacity) in each occupational group can lead to a reduction in burnout.
Regarding the relationship between resiliency variable and burnout dimensions, the findings showed a significant negative correlation between the dimensions of burnout (emotional exhaustion, depersonalization and personal incompetence) and resiliency variable. Considering the significant relationship between resilience and emotional exhaustion (-0.55), it can be noted that resiliency can help nurses to cope with stressful conditions and prevent emotional exhaustion, which can reduce psychological, motivational and emotional symptoms at work. Emotional exhaustion with symptoms such as chronic fatigue, sleep disturbance, and various physical symptoms and feeling of being pressured is associated with loss of emotional resources in an individual.
In the study of Talaee et al., about a quarter of nurses reported moderate emotional exhaustion [9]. The results of the study of Silvia et al. showed that burnout among nurses in emergency departments was high in the dimensions of emotional exhaustion and depersonalization, and it was low in the aspect of personal incompetence [30]. The findings of Spooner (2004) indicated that younger nurses experience higher levels of emotional exhaustion and depersonalization [31]. One of the important factors associated with emotional exhaustion is work experience. Emotional exhaustion is reported more often in less experienced nurses [32]. In the study by Momeni et al., (2010), which was aimed at comparing burnout among nurses working in treatment and education sectors, a significant direct relationship was noted between emotional exhaustion and employees’ experience in the treatment sector, and in subjects with higher work experience, burnout rates in this dimension were greater [21].
Increased occupational burnout reduces the individual’s ability to adapt to stressors and, as a result, causes behavioural and physical symptoms. Also, stresses induced from occupational conditions have a significant effect on the physical and mental health of individuals. Burnout due to persistent stresses reduces the ability of individuals to adapt to stressors [33]. The negative correlation between resiliency and burnout is indicative of the strength of prediction of resilience as a strong predictor of occupational burnout, that is, with higher resiliency, the degree of burnout is reduced. From the relationship between occupational burnout and resiliency, it can be noted that resiliency increases the individual’s adaptability to stressors, which reduces the psychological, motivational and emotional symptoms at work, thus, reducing resiliency with increasing emotional exhaustion.
On the other hand, reduced resiliency in the subscale of depersonalization leads to the development of a negative attitude and the emergence of negative emotional responses about individuals and the environment. The low level of resilience in the subscale of personal incompetence reduces self-esteem and leads to the negative evaluation of the person’s job and their ineffective relationship with colleagues and clients [21]. The negative correlation between resiliency and occupational burnout dimensions indicates that resiliency is a strong predictor of occupational burnout, such that with increasing resiliency, occupational burnout can be predicted in nurses. Nowadays, nurses’ physical and mental health is emphasised to provide desirable health care and treatment services, and occupational burnout is one of the most important debilitating factors for nurses’ health [34].
Measures and interventions that have been taken to reduce burnout and stress in nurses have often focused on organisational and managerial factors. If necessary, nurses should focus on improving individual factors to face workplace problems and difficulties. In this regard, Scholes (2008) has proposed 10 steps to promote resilient behaviours in nurses, which can cope with the professional identity crisis [35]. The literature on burnout and resilience shows that having a positive social network, good relationships with friends and colleagues, and having a supportive environment greatly affects these two variables [36]. Recently, the concept of resilience has been widely associated with the nursing profession [37]. Nurses must skillfully elaborate their resilience to cope with professional problems and maintain their mental health [24]. Resiliency has an effective effect on adaptation to risk factors and can play an effective role in reducing burnout [38].
Overall, the findings of this study showed a significant negative correlation between resiliency and burnout, thus, by improving the level of resiliency in nurses using strategies such as educating the importance of resiliency, monitoring and practising in the area of resiliency, and controlling occupational stresses the risk of burnout can be reduced. Also, promoting resiliency has other benefits, including maintaining peace of mind and increasing mental capacity and professional performance. In this regard, nursing and hospital authorities should, while paying attention to resiliency in their staff, create an effective management system to promote this characteristic. Also, since resiliency is learned over time, nursing education managers should pay attention to this issue in nursing students’ curriculum.
There were several limitations to this meta-analysis. Few studies were found that had all of our inclusion criteria, for example, some articles did not address the correlation coefficient between the two variables of resiliency and their data sources did not report complete data for the meta-analysis.
Acknowledgements
This research was derived from a research project approved by Mashhad University of Medical Sciences with the code 961458 and the Code of Ethics Committee IR.MUMS.REC.1397.013. We wish to thank the Deputy of Research of Mashhad University of Medical Sciences for their cooperation in this project.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Rahmani F, Behshid M, Zamanzadeh V, Rahmani F. Relationship between general health, occupational stress and burnout in critical care nurses of Tabriz teaching hospitals. Iran Journal of Nursing. 2010;23(66):54–63. [Google Scholar]
- 2.Saberi HR, Moravveji SAR, Ghoraishi F, Heidari Z. Post-traumatic stress disorder in Kashan and Arak emergency medicine departments'staffs during 2009. KAUMS Journal (FEYZ) 2009;12(5):1–6. [Google Scholar]
- 3.Tummers GE, Janssen PP, Landeweerd A, Houkes I. A comparative study of work characteristics and reactions between general and mental health nurses: A multi-sample analysis. Journal of advanced nursing. 2001;36(1):151–62. doi: 10.1046/j.1365-2648.2001.01952.x. https://doi.org/10.1046/j.1365-2648.2001.01952.x PMid:11555059. [DOI] [PubMed] [Google Scholar]
- 4.Cho SH, Lee JY, Mark BA, Yun SC. Turnover of new graduate nurses in their first job using survival analysis. Journal of Nursing Scholarship. 2012;44(1):63–70. doi: 10.1111/j.1547-5069.2011.01428.x. https://doi.org/10.1111/j.1547-5069.2011.01428.x PMid:22233430. [DOI] [PubMed] [Google Scholar]
- 5.Niday P, Smithgall L, Hilton S, Grindstaff S, McInturff D. Redesigning nurse staffing plans for acute care hospitals: at Johnson City Medical Center in Tennessee, a team approach to better managing nurse staffing not only saved $7 million annually in contract labor costs, but also led to increased nursing satisfaction. Healthcare Financial Management. 2012;66(6):112–7. PMid:22734326. [PubMed] [Google Scholar]
- 6.Rahimi A, Ahmadi F, Akhond M. An investigation of amount and factors affecting nurses'job stress in some hospitals in Tehran. Hayat. 2004;10(3):13–22. [Google Scholar]
- 7.Zandi A, Sayari R, Ebadi A, Sanainasab H. Abundance of depression, anxiety and stress in militant Nurses. Journal Mil Med. 2011;13(2):103–8. [Google Scholar]
- 8.Abdi H, Shahbazi L. Correlation between occupation stress in nurses at intensive care unit with job burnout. Journal of Shahid Sadoughi University of Medical Sciences and Health Services. 2001;9(3):58–63. [Google Scholar]
- 9.Talaee A, Mokhber N, Mohammad nejad M, Samari A. Burnout and its associated factors in Mashhad hospital employees. Journal of Semnan Medical Sciences University. 2008;9(3):237–47. [Google Scholar]
- 10.Toubaei S, Sahraeian A. Burnout and job satisfaction of nurses working in internal, surgery, psychiatry burn and burn wards. The Horizon of Medical Sciences. 2007;12(4):40–5. [Google Scholar]
- 11.Bakker AB, Van Der Zee KI, Lewig KA, Dollard MF. The relationship between the big five personality factors and burnout: A study among volunteer counselors. The Journal of social psychology. 2006;146(1):31–50. doi: 10.3200/SOCP.146.1.31-50. https://doi.org/10.3200/SOCP.146.1.31-50 PMid:16480120. [DOI] [PubMed] [Google Scholar]
- 12.Vahey DC, Aiken LH, Sloane DM, Clarke SP, Vargas D. Nurse burnout and patient satisfaction. Medical care. 2004;42(2 Suppl):II57. doi: 10.1097/01.mlr.0000109126.50398.5a. https://doi.org/10.1097/01.mlr.0000109126.50398.5a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amini F. The Relationship between Resiliency and Burnout in Nurses. JGBFNM. 2013;10(2):94–102. [Google Scholar]
- 14.McAllister M, McKinnon J. The importance of teaching and learning resilience in the health disciplines: a critical review of the literature. Nurse education today. 2009;29(4):371–9. doi: 10.1016/j.nedt.2008.10.011. https://doi.org/10.1016/j.nedt.2008.10.011 PMid:19056153. [DOI] [PubMed] [Google Scholar]
- 15.Gobaribanab B. Spiritual intelligence. Andishe Novine Dini. 2008;3(10):100–10. [Google Scholar]
- 16.Hosseini Ghomi T, Salimi Bajestani H. Effectiveness of resilience training on stress of mothers whose children, suffer from cancer in Imam Khomeini hospital of Tehran. Health Psychology. 2013;1(4):97–109. [Google Scholar]
- 17.Hamid N, Keikhosravani M, Babamiri M, Dehghani M. The relationship between mental health, spiritual intelligence with resiliency in student of Kermanshah University of Medical Sciences. Jentashapir Journal of Health Research (Jentashapir) 2012;3(2):331–8. [Google Scholar]
- 18.Jackson D, Firtko A, Edenborough M. Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: a literature review. Journal of advanced nursing. 2007;60(1):1–9. doi: 10.1111/j.1365-2648.2007.04412.x. https://doi.org/10.1111/j.1365-2648.2007.04412.x PMid:17824934. [DOI] [PubMed] [Google Scholar]
- 19.Mohammadi M. The study of key factors influences on resiliency of substance abuse at risk. Tehran: University of Social Welfare and Rehabilitation Sciences; 2005. [Google Scholar]
- 20.Maslach C, Jackson SE. The measurement of experienced burnout. Journal of organizational behavior. 1981;2(2):99–113. https://doi.org/10.1002/job.4030020205. [Google Scholar]
- 21.Momeni H, Salehi A, Seraji A. The comparison of burnout in nurses working in clinical and educational sections of Arak University of Medical Sciences in 2008. AMUJ. 2010;12(4):113–23. [Google Scholar]
- 22.Shakerinia I, Mohammadpour M. Relationship between job stress and resiliency with occupational burnout among nurses. J Kermanshah Univ Med Sci. 2010;14(2):e79518. Epub 2010-09-01. [Google Scholar]
- 23.Rushton CH, Batcheller J, Schroeder K, Donohue P. Burnout and resilience among nurses practicing in high-intensity settings. American Journal of Critical Care. 2015;24(5):412–20. doi: 10.4037/ajcc2015291. https://doi.org/10.4037/ajcc2015291 PMid:26330434. [DOI] [PubMed] [Google Scholar]
- 24.Warelow P, Edward Kl. Caring as a resilient practice in mental health nursing. International Journal of Mental Health Nursing. 2007;16(2):132–5. doi: 10.1111/j.1447-0349.2007.00456.x. https://doi.org/10.1111/j.1447-0349.2007.00456.x PMid:17348964. [DOI] [PubMed] [Google Scholar]
- 25.Guo Yf, Luo Yh, Lam L, Cross W, Plummer V, Zhang Jp. Burnout and its association with resilience in nurses: a cross-sectional study Nurse burnout and resilience. Journal of clinical nursing. 2018;27(1-2):441–9. doi: 10.1111/jocn.13952. https://doi.org/10.1111/jocn.13952 PMid:28677270. [DOI] [PubMed] [Google Scholar]
- 26.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93. doi: 10.1001/jama.288.16.1987. https://doi.org/10.1001/jama.288.16.1987 PMid:1238765;0. [DOI] [PubMed] [Google Scholar]
- 27.Iglesias MEL, de Bengoa Vallejo RB. Prevalence and relationship between burnout, job satisfaction, stress, and clinical manifestations in Spanish critical care nurses. Dimensions of Critical Care Nursing. 2013;32(3):130–7. doi: 10.1097/DCC.0b013e31828647fc. https://doi.org/10.1097/DCC.0b013e31828647fc PMid:23571196. [DOI] [PubMed] [Google Scholar]
- 28.Olson K, Kemper KJ, Mahan JD. What factors promote resilience and protect against burnout in first-year pediatric and medicine-pediatric residents? Journal of evidence-based complementary & alternative medicine. 2015;20(3):192–8. doi: 10.1177/2156587214568894. https://doi.org/10.1177/2156587214568894 PMid:25694128. [DOI] [PubMed] [Google Scholar]
- 29.McCain RS, McKinley N, Dempster M, Campbell WJ, Kirk SJ. A study of the relationship between resilience, burnout and coping strategies in doctors. Postgraduate medical journal. 2017 doi: 10.1136/postgradmedj-2016-134683. postgradmedj-2016-134683. [DOI] [PubMed] [Google Scholar]
- 30.Silvia L, Gutiérrez C, Rojas PL, Tovar SS, Guadalupe J, Tirado O, et al. Burnout syndrome among Mexican hospital nursery staff. Rev Med IMSS. 2005;43(1):11–5. [PubMed] [Google Scholar]
- 31.Spooner-Lane R. The influence of work stress and work support on burnout in public hospital nurses: Queensland University of Technology. 2004 [Google Scholar]
- 32.Kutluturkan S, Sozeri E, Uysal N, Bay F. Resilience and burnout status among nurses working in oncology. Annals of general psychiatry. 2016;15(1):33. doi: 10.1186/s12991-016-0121-3. https://doi.org/10.1186/s12991-016-0121-3 PMid:27895699 PMCid: PMC5109709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khodabakhshi M, Abdollahi M, Gholamrezaei S, Habibi E. Work place burnout prediction based on resiliency in nurses in relation to gender. Koomesh. 2016;17(4):845–55. [Google Scholar]
- 34.Rafiee F, Oskouie F, Nikravesh M. Key factors in nurses'reaction to Burnout: A qualitative study. Razi Journal of Medical Sciences. 2007;13(53):83–94. [Google Scholar]
- 35.Scholes J. Coping with the professional identity crisis: is building resilience the answer? International Journal of Nursing Studies. 2008;45(7):975–8. doi: 10.1016/j.ijnurstu.2007.12.002. https://doi.org/10.1016/j.ijnurstu.2007.12.002 PMid:18255070. [DOI] [PubMed] [Google Scholar]
- 36.Treglown L, Palaiou K, Zarola A, Furnham A. The dark side of resilience and burnout: a moderation-mediation model. PloS one. 2016;11(6):e0156279. doi: 10.1371/journal.pone.0156279. https://doi.org/10.1371/journal.pone.0156279 PMid:27336304 PMCid: PMC4918953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tusaie K, Dyer J. Resilience: A historical review of the construct. Holistic nursing practice. 2004;18(1):3–10. doi: 10.1097/00004650-200401000-00002. https://doi.org/10.1097/00004650-200401000-00002 PMid:14765686. [DOI] [PubMed] [Google Scholar]
- 38.Garmezy N, Masten AS. The protective role of competence indicators in children at risk. 1991 [Google Scholar]


