Abstract
AIM:
The objective of this study was to evaluate the frequency of risk factors for bacteremia in children less than 15 years of age was determined in Bahrami Hospital during 2013-2016.
METHODS:
This study conducted on 84 children aged 3 months’ to15 years old, who hospitalised in the pediatrics ward and the PICU in Bahrami Hospital from 2012 to 2016. Our study consisted of 46 boys (54.2%) and 38 girls. Moreover, 24.1% of subjects (20 patients) were entered in the study as young as three months old, followed by three months to three years (49.4 %; 41 subjects), and 3 to 15 years of age (26.5%; 22 individuals).
RESULTS:
The average hospitalization duration was determined to be 15.30 ± 8.75 days. Moreover, our results revealed that a history of blood transfusion in 11.2% of patients. On the other hand, 35.7% of cases were determined to be positive for blood cultures. The microorganisms reported from positive blood cultures include Enterobacter (81.48%), Escherichia coli (11.11%) and Klebsiella (3.70%). Also, 50% of patients were hospitalised in the internal ward, 12% received immunosuppressive drugs, and 96.4% of the patients had a history of vaccination.
CONCLUSION:
Pediatric severe sepsis remains a burdensome public health problem, with prevalence, morbidity, and mortality rates similar to those reported in critically ill adult populations. International clinical trials targeting children with severe sepsis are warranted.
Keywords: Children, Risk factor, Septicemia, Septic shock, Systemic inflammatory response Syndrome
Introduction
Systemic Inflammatory Response Syndrome (SIRS) is an inflammatory state initiated by the host in response to infectious or noninfectious insult. Sepsis is known to be a life-threatening complication, which can be referred to SIRS due to a suspected or confirmed infection [1]. Bacteremia diseases one of the most serious infectious diseases in children, which can be potentially life-threatening. Bacteremia can be caused by a wide range of gram-negative and gram-positive microorganisms and can be manifested with or without a specific site of infection, such as pneumonia or meningitis. Some bacteremia is a transient self-limiting [2] [3]. An epidemiological study of sepsis has shown that in the period from 1979 to 2000, Gram-positive infections have dominated [4], although recent studies of 14,000 patients in 75 countries have suggested that the cases composed predominantly of gram-negative bacteria (62%), followed by gram-positive (47%) and fungi (19%) [5].
The incidence of bacteremia in children in the hospital and outpatient department has been investigated. The most common microorganisms in healthy children over a month of age are pneumococcal bacteremia, Haemophilus influenzae type B, and Neisseria meningitidis, which is characterised by moderate to severe pathogenesis. Staphylococcus aureus, Salmonella and Streptococcus A have been reported in children and also in children who suffer from pyelonephritis or diarrhoea due to Gram-negative bacteria [5].
The underlying disease in children reduces the host’s response to the infection and may cause bacteremia to spread by the same microorganisms. In this group of children, especially when hospitalised, Enterobacteriaceae, Staphylococcus aureus, Staphylococcus coagulase negative and fungi are the most important organisms that are commonly isolated from the blood cultures [7] [8]. The use of intravascular and urethral catheters, endotracheal tubes, and other extraneous materials will make children with immunodeficiency disease more susceptible to infections.
The prevalence of septicemia detected over the years has increased, partly due to the advancement of medical technology and an increase in the number of people with a life-threatening immunodeficiency, where they can be survived [9]. The most common cause of catheter-related sepsis is gram-positive bacteria, especially coagulase-negative staphylococci (CoNS), and gram-negative bacteria [6]. Children’s bacteremia can lead to complications such as severe sepsis, septic shock, and ultimately death.
The severity of mortality rate from septic shock depends on the following factors, such as the location of infection, bacterial pathogens, and multifocal dysfunction and host immune responses.
It should be noted that severe sepsis is still one of the leading causes of death in children. Recent data indicate therapeutic strategies at improving sepsis outcomes in children with a mortality rate of about 10%. Infants, especially those who are shown as having a low birth weight and children with chronic medical conditions are at the highest risk of severe sepsis [7] [8] [9]. The mortality rate of the child’s patients who undergo bone marrow transplantation is higher than that of other patients with septic shock. It should be taken into consideration that severe sepsis encompasses a large national cost, where the median admission period is 31 days for children; while for infants, the median admission period is 53 days. The highest incidence of severe sepsis was observed among infants and the lowest among children aged 5to14 [10].
Despite the advances in drugs and vaccinations, sepsis can usually lead to septic shock and eventually death. This disease remains a problem of pediatric medicine. Regarding the importance of sepsis, the present study was designed to identify the most common risk factors for reducing morbidity and mortality and treatment costs. The frequency of risk factors for bacteremia in children under 15 years of age was determined in Bahrami Hospital during 2013-2016.
Material and Methods
This descriptive and cross-sectional study was conducted to determine the frequency of risk factors for bacteremia in children under the age of 15 in Bahrami Hospital. Patient information was collected based on the evidence in hospital records. All the necessary specifications were recorded in information forms, which included age, gender, gestational age, weight, the cause of hospitalisation, hospitalisation date, discharge date or death, blood and urine culture results, cerebrospinal fluid, a graph of the chest, Positive clinical signs and routine blood tests.
This retrospective study was conducted on patients diagnosed with bacteremia in Tehran’s Bahrami Hospital in Tehran during the years 2013 to 2016. It should be noted that Bahrami Hospital is classified in the third level of care and many of its patients are referenced from other medical centres in Tehran and other cities. Patients are admitted to the intensive care unit at the age of 1 month to 15 years. The possibility of non-invasive monitoring and mechanical ventilation is provided for all patients.
In this study, patients (aged > 15 months < 15 years) were diagnosed with septic sepsis or septic shock at the time of admission. Exclusion criteria included the history of surgery during hospitalisation or having underlying conditions such as malignancy or immune compromised patient with bacteremia. All patients were evaluated for many factors such as underlying variables, duration of the disease, previous medical history, and previous use of the drug, symptoms based on the definitions of sepsis, as well as the initial infection site, tests, positive culture responses, therapeutic response and the ultimate fate. Of all children referring to the treatment centre, 84 samples were examined. The number of patients in this study was determined by the census. Declaration of Helsinki was applied for all patients as a statement of ethical principles for medical research. Furthermore, no additional financial or spiritual burden was imposed on patients, and all information was remained confidential.
All the analyses were performed using EpiInfo (version 6, Centers for Disease Control and Prevention, Atlanta, GA, U.S.A.). Mean, and proportions were compared by Student t-test and chi-squared. P < 0.05 was considered to be statistically significant.
Results
The children studied consisted of 46 boys (54.2%) and 38 girls (45.8%). In terms of age, 24.1%of subjects (20 patients) were enrolled as young as one to three months old, 49.4% (41 subjects) were three months to three years, and the remaining 26.5% (22 individuals) included children with 3 to 15 years of age (Figures 1 and 2). The average length of stay in hospitals (ALOS) was calculated to be 15.30 ± 8.75.
Figure 1.
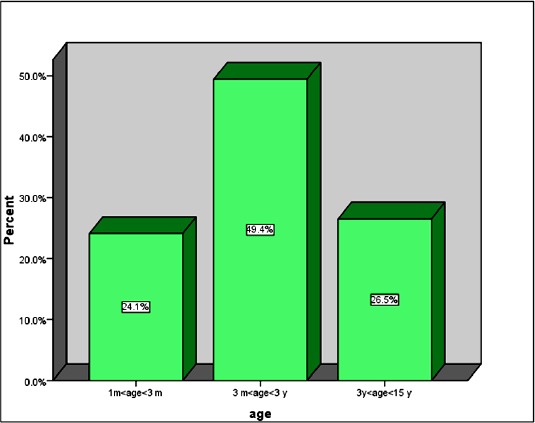
Frequency of different age groups in this study
Figure 2.
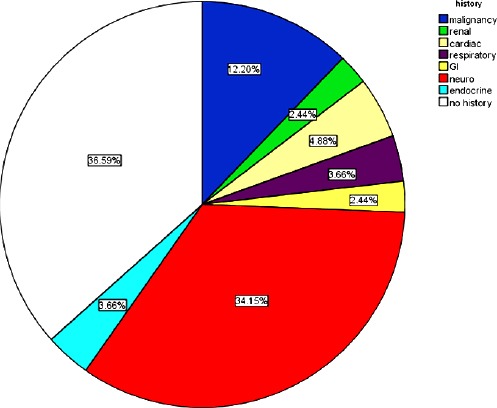
Frequency of underlying illness in patients
Table 1 and Figure 2 show the list patient with bacteremia.
Table 1.
Frequency of underlying illness in patients
| Underlying disease | Number | Per cent |
|---|---|---|
| Malignancy | 10 | 12.2 |
| Kidney | 2 | 2.4 |
| Cardiac | 4 | 4.9 |
| Respiratory | 3 | 3.7 |
| Digestive | 2 | 2.4 |
| Endocrine and Metabolic | 3 | 3.7 |
| Nervous | 28 | 34.1 |
| No underlying illness | 32 | 36.6 |
| Total | 84 | 100 |
The results revealed that 63.6% of the patients had an underlying disease, followed by neurological diseases (34.1%) and malignancies (12.2%), and less than one-quarter of the patients exhibited growth impairment, which growth fell below 5% of the growth curve.
A peripheral venous catheter (PVC) was used for 52.4% of children, followed by nasogastric tube (7.7%), intubation (14.7%) and urinary catheter (4.9%), (Figure 3). A record of blood intake was found in 11.2% of the subjects.
Figure 3.
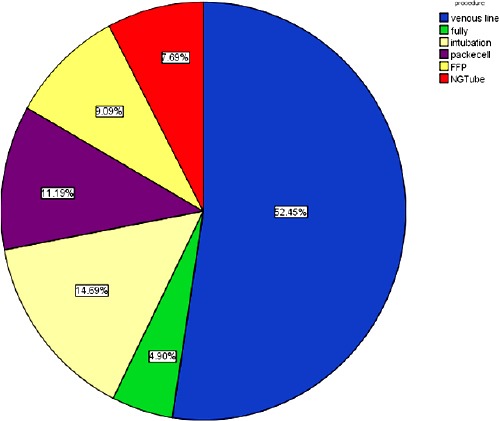
Frequency of methods used for blood intake
Positive cultures were reported in 35.7% of subjects. The frequency of microorganisms reported from positive blood cultures was as follows: Enterobacter was observed in 81.48% of positive cultures, followed by Escherichia coli (11.11%), Klebsiella (3.70%) and CoNS (3.70%). It is worth noting that 50% of patients were admitted to the general ward, followed by infectious diseases section and the pediatric intensive care unit (PICU). Regarding the positive results of blood cultures, a number of clinical symptoms were recorded in patients including fever (34.0%), respiratory symptoms (19.7%), coughing (12.8%), respiratory distress (6.9%), gastrointestinal symptoms (20.7%), diarrhea (7.9%), vomiting (12.8%), torpidity (12.8%), dermal signs (1.5%), (Figure 4)
Figure 4.
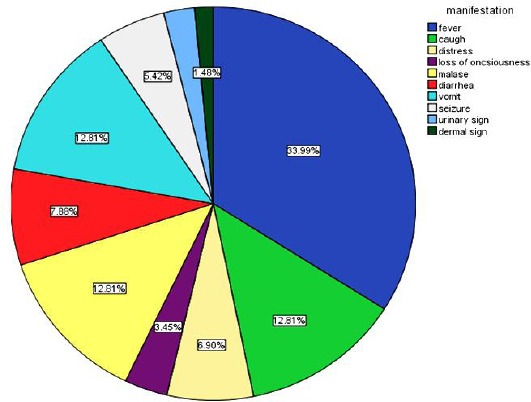
Frequency of clinical symptoms in patients
The results of the present study indicated that 23.5% of the cases received antibiotics, while 12% have taken an immunosuppressant drug the remaining 96.4% received the vaccine.
Given laboratory findings, WBCs changes reached to fewer than 3,000/μl in 13.3% of subjects, 64% showed an increased WBCs level, ranging from 3,000 to 15,000. Moreover, the remaining 25.3% showed WBC count ≥ 15,000/μL.
Our data revealed platelet numbers equal to 150,000 platelets for 30.1% of the subjects, followed by platelets ranging from 150,000 to 500,000 (56.6%) and platelets greater than 500,000 (13.3%). Furthermore, 50% of patients revealed an erythrocyte sedimentation rate (ESR) > 30 mm/hr. The remaining 50% of the cases showed ESR less than 25 mm/hr. It should be noted that mortality in our patients was calculated at 37.8%.
The following information was obtained in the investigation of dead children; about 26.7% of the cases were male deaths. Also, the number of cases in age groups is as follows: between 1-3 months of age (26.7%), 3 months to 3 years (48%), and between 3 -15 years of age (25.3%). Regarding underlying illness, malignancy was seen in 11.3% of patients, followed by kidney complications (2.8%), neurological complications (39.4%), and no underlying disease (35.2%). On the other hand, based on the blood culture, 12.5% of the deaths showed E. coli, while most of them (79.2%) revealed enterobacter
Other findings based on the medical records of dead children included fever (84%), abnormal white blood cell (38.4%; leukocytosis, leukopenia), abnormal platelet (43.4%; thrombocytopenia, thrombocytosis), blood intake (1.3%), immunosuppressive drug (12.5%) and history of antibiotic use (24.7%).
Discussion
According to the results of this study, sepsis was more prevalent in the age group of 3 months to 3 years, and the disease in boys was about 10% higher than in girls, underlying disease was observed in 63.6% of cases and neurological diseases were also the most common conditions.
As other study indicated, sepsis was more common in infants from 1 month to 1 year old in Bahrami Hospital. Similar to our study, the prevalence of disease among boys was about 10% higher than girls. In the study above, malignancies and then kidney disease were the most common underlying disorders among patients [11]. While the current study demonstrated that neurological diseases are the most common underlying disorders that show changes in recent years among those referred to the centre because the location of the study in the two studies was the same.
A study reported sepsis prevalence in 2% of all hospitalised subjects. The mentioned study revealed that 83% of patients had underlying diseases and hematologic disorders or neoplasms has been found to be the most common underlying disorder. Furthermore, based on the study above, Gram-positive bacteria accounted for 68% of the septic-influencing organisms, with the most frequent occurrence of Staphylococcus aureus (18%). The mortality due to gram-negative bacteria was higher than that of gram-positive [12].
The largest epidemiological report of severe sepsis in children has been derived from cohort studies conducted in the United States, in which the annual incidence of severe sepsis in children (under age 20) is as follows: the incidence of sepsis in children under one year of age has been determined to be 9.7%, which is much higher in comparison with 0.25 to 0.5 in the age group of one year to 19 [13].
It has also been shown in the study above that incidence of severe sepsis in children with concomitant illnesses is more common than other children. However, despite the increasing trend in severe sepsis, the death rate has dropped from 10.3% to 8.9%. This reported data from 42 United States hospitals affirm the increasing prevalence of sepsis and a reduction in the risk of death [13].
Based findings of a previous study, Klebsiella B has been reported to be the most commonly isolated organism (43.75%) from children under the age of 10 years with sepsis, followed by Staphylococcus aureus (18.75%) [8]. They also stated that the highest prevalence was in children aged 10 to 5 years and male to female ratio was determined to be 1.28:1.0. Symptoms of bacteremia are different, where depending on the age and underlying disorders, the duration of the disease, and certain microorganisms. Children between 3 months and 3 years may have fever and evidence of an upper or lower respiratory tract infection, or an unlikely infectious site and bacteremia. Most studies show that the risk of bacteremia can develop with increasing body temperature, and when the body temperature reaches 41°C, approximately 25% of these patients may develop a broad array of bacteremia [9].
The incidence of invasive infections, sepsis and septic shock in children (0 to 15 years old) has increased in the Australian and New Zealand care units over a 12-year period. Severe infections are associated with about one-quarter of ICU deaths among children. In 2002-2008, the mortality rate from invasive and septic infections decreased by about one third, compared with 2008 to 2013, and septic shock mortality dropped by one fifth, which did not have a significant difference compared with the overall improvement in the overall survival of children admitted to ICUs due to non-infectious causes [9] [10] [13].
Therefore, severe infections have an important impact on the health of children and impose significant pressure on health systems. As studies have shown, ICU admission due to sepsis and septic shock is costly, may also have adverse outcomes in the long term, such as neurological complications and disability and death [14].
The incidence of severe sepsis in the United States increased from 0.56 to 0.89 per 1,000 children between 2000 and 2005, while the mortality of sepsis remained unchanged at 9%. this increase in the age group of newborns was more than other age groups, and this data was not consistent with our findings [15].
Base on a study, pediatric patients with hematologic and malignant diseases who had sepsis, included determining the risk factors for mortality after the development of sepsis. The results of the study above indicated that more than half (52.9%) of the isolates from sepsis-related death belonged to Gram-positive cocci resistant to β-lactam antibiotics. In mentioned study, it has been revealed that relapse history, history of the underlying disease, and high C reactive protein concentration at the onset of fever could be a key factor for mortality in patients with sepsis [16]. Sepsis is the leading cause of 5.6% of deaths in adult patients with trauma, but about 33% of brain damage has been shown a safe interrupt the neural axis. While TBI is a major cause of death in the pediatric population, it remains unclear whether children with neuroprotection similar to that of adults are at higher risk for sepsis. Therefore, a study was conducted to determine the relationship between traumatic brain injury (TBI) and sepsis in children under the age of 18 years between 2001 and 2012. Initial results of this study showed that 63.9% of children with any type of TBI were identified, and sepsis was reported in 1.0% of children, compared with 2.8% of children without this complication [17].
In our study, 34.1% of the studied population had sepsis with neurological disorders. These results are in line with our study of the prevalence of sepsis in children under the age of 18 in patients with a variety of neurological diseases. In a cross-sectional study, tachycardia, mental changes, abnormal condition and temperature were the highest regarding clinical and diagnostic symptoms of sepsis. The white blood cell count had the highest changes in laboratory tests [18].
In the present study, in 34.0% of cases, fever was observed in the clinical symptoms during admission. Respiratory symptoms (12.8% cough, 6.9% respiratory distress) were recorded in 19.7%, followed by gastrointestinal symptoms (20.7%, diarrhea 7.9%, vomiting 12.8%), lethargy (12.8%), and dermal signs (1.5%). According to laboratory finding, abnormal white blood cell was seen in 38.4% of subjects in the present study (leukocytosis, leukopenia), followed by abnormal platelet (43.4%; thrombocytopenia, thrombocytosis), blood intake (1.3%), immunosuppressive drug (12.5%), antibiotic use (24.7%) and history of vaccination (96.4%).
Severe sepsis remains very common in children and accounts for about 8% of all children with severe depression. Although the absolute number of cases of severe sepsis is 10-fold lower than adults [4] [19], the prevalence of 8.2% in PICU patients is highly similar to the proportion of adults suffering from severe sepsis. These results demonstrated that 16-bed PICU is probably to be treating one child suffering from severe sepsis at least. Also, hospital mortality, which is often much lower, was determined as 25% in this study and is higher than estimated prevalence in previous epidemiological studies, where examined hospital data retrospectively [20]. Coexisting diseases, immunosuppressive diseases, and kidney diseases have the highest mortality rate in previous studies among children. However, the present study has the highest mortality rate for neurological diseases, but it cannot be determined whether the death was attributed to sepsis or a condition associated with an underlying disorder. In one-third of children with developing the disease, progressive organ dysfunction and severe functional disability are common in nearly one-fifth of sepsis survivors [20] [21] [22] [23] [24].
In the previous study at the same centre in 2010-2011, most of the organisms isolated from blood culture were gram-positive bacteria (CoNS and S. aureus), [11]. In our study, the gram-negative bacteria Enterobacter and Escherichia coli were the most commonly isolated microorganisms isolated from blood culture in patients. Regarding the results, intravascular and urinary catheters were the most leading causes of sepsis in admitted children.
Urinary tract infections can be considered as causes of sepsis among these patients. The bacteria of the UTI are faecal microbial flora found in the perineum and periurethral, where enter the bladder through the urethra. In uncircumcised babies, pathogenic bacteria can enter the urinary tract from the fore skin flora. The sensitivity of girls to urinary tract infection is due to the shorter urinary tract and the closeness of the perina to the urethral duct and colonisation of the perineal region with intestinal organisms. Colonization with E. coli and enterococci decreases during the first year of life and is naturally negligible after 5 years of age. In early childhood, Enterobacteria and Enterococci are normal periurethral flora, which can also be opportunistic agents of infections. E. coli is the dominant gram-negative bacteria in young girls, while in boys, E.coli and Proteus have this condition [22] [23] [24].
Children are at risk of UTI due to the colonisation of E. coli, enterococci and Proteus in the surrounding area of ureter up to 5 years old. The use of urinary catheters increases the likelihood of UTI, which can justify an increase in infections reported with E. coli and enterococci in the present study. To prove it, there is a need for other studies to review the positive blood cultures as well as to control the conditions when using the urinary catheter regarding sterilisation conditions. It can be concluded that the hospital mortality rate in the present study was 37.8%, which suggested a significant increase compared to the previous survey at the centre [11], which was 6.1%, indicating the importance of severe sepsis as a major public health problem, even in children. This finding contrasts with reports from epidemiological studies that report infectious death rates of children at about 10.4%. The results of this study were consistent with other studies but also differed in parts that could be explained by the nature of sepsis, its underlying factors, the population studied, and the health and diagnostic standards.
Our study was conducted in a General Pediatric Hospital, that the most common causes of sepsis were recorded in the age group of three months to three years old. Regarding underlying illnesses, neurological disorders were at the top and growth disturbances were estimated in more than a quarter of patients. This information will help us to pay special attention to these patients. Given dead children, the most common age range of the disease was found to be between 3 months and 3 years in the current study. Regarding underlying diseases and microorganisms, malignancies and Enterococcus were found to be the most common cause of disease, respectively, which similar results were obtained compared to the previous survey at the same centre [11].
Finally, it can be concluded that the evaluation of sepsis in each health centre is necessary to identify its risk factors to control and reduce the frequency of sepsis and to reduce mortality, morbidity and medical expenses.
The limitation of the current study was small sample size because only 84 patients had inclusion criteria.
Author’s contributions
SYM, AR, LKH, and AI equally participated in experimental design, data collection, writing and revision of the manuscript.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Gray J, Gossain S, Morris K. Three-year survey of bacteremia and fungemia in a pediatric intensive care unit. The Pediatric infectious disease journal. 2001;20:416–21. doi: 10.1097/00006454-200104000-00009. https://doi.org/10.1097/00006454-200104000-00009 PMid:11332667. [DOI] [PubMed] [Google Scholar]
- 2.Watson RS, Carcillo JA, Linde-Zwirble WT, Clermont G, Lidicker J, Angus DC. The epidemiology of severe sepsis in children in the United States. American journal of respiratory and critical care medicine. 2003;167:695–701. doi: 10.1164/rccm.200207-682OC. https://doi.org/10.1164/rccm.200207-682OC PMid:12433670. [DOI] [PubMed] [Google Scholar]
- 3.Norton EB, Archibald LK, Nwanyanwu OC, et al. Clinical predictors of bloodstream infections and mortality in hospitalised Malawian children. The Pediatric infectious disease journal. 2004;23:145–51. doi: 10.1097/01.inf.0000109258.82988.40. https://doi.org/10.1097/01.inf.0000109258.82988.40 PMid:148721;81. [DOI] [PubMed] [Google Scholar]
- 4.Elward AM, Fraser VJ. Risk factors for nosocomial primary bloodstream infection in pediatric intensive care unit patients: a 2-year prospective cohort study. Infection Control. 2006;27(06):553–60. doi: 10.1086/505096. https://doi.org/10.1086/505096 PMid:16755473. [DOI] [PubMed] [Google Scholar]
- 5.Pound CM, Johnston DL, Armstrong R, Gaboury I, Menon K. The morbidity and mortality of pediatric oncology patients presenting to the intensive care unit with septic shock. Pediatric blood & cancer. 2008;51:584–8. doi: 10.1002/pbc.21670. https://doi.org/10.1002/pbc.21670 PMid:18623196. [DOI] [PubMed] [Google Scholar]
- 6.Aiken AM, Mturi N, Njuguna P, et al. Risk and causes of paediatric hospital-acquired bacteraemia in Kilifi District Hospital, Kenya: a prospective cohort study. Lancet. 2011;378:2021–27. doi: 10.1016/S0140-6736(11)61622-X. https://doi.org/10.1016/S0140-6736(11)61622-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Area CGftSoSiPiB. Clinical study on sepsis in 2 pediatric intensive care units in Beijing. Zhonghua er like za zhi Chinese journal of paediatrics. 2012;50:178. PMid:22801197. [PubMed] [Google Scholar]
- 8.Tiwari DK, Golia S, Sangeetha K, Vasudha C. A study on the bacteriological profile and antibiogram of bacteremia in children below 10 years in a tertiary care hospital in Bangalore, India. Journal of clinical and diagnostic research: JCDR. 2013;7:2732. doi: 10.7860/JCDR/2013/6682.3701. PMid:24551625 PMCid: PMC3919345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bass JW, Steele RW, Wittler RR, et al. Antimicrobial treatment of occult bacteremia: a multicenter cooperative study. The Pediatric infectious disease journal. 1993;12:466–73. doi: 10.1097/00006454-199306000-00003. https://doi.org/10.1097/00006454-199306000-00003 PMid:8345978. [DOI] [PubMed] [Google Scholar]
- 10.McCarthy P. Controversies in pediatrics-what tests are indicated for the child under 2 with fever. Pediatrics. 1979;64:PR51–PR6. [Google Scholar]
- 11.Rahbarimanesh A, Mobedi M, Alizade Taheri P. Sepsis risk factors in children: a brief report. Tehran University Medical Journal. 2012;70:264–269. [Google Scholar]
- 12.Oda K, Matsuo Y, Nagai K, Tsumura N, Sakata Y, Kato H. Sepsis in children. Pediatrics International. 2000;42:528–33. doi: 10.1046/j.1442-200x.2000.01281.x. https://doi.org/10.1046/j.1442-200x.2000.01281.x PMid:11059544. [DOI] [PubMed] [Google Scholar]
- 13.Thompson GC, Kissoon N. Sepsisin Canadian children: A national analysis using administrative data. Clinical epidemiology. 2014;6:461. doi: 10.2147/CLEP.S72282. https://doi.org/10.2147/CLEP.S72282 PMid:25525390 PMCid: PMC4266244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schlapbach LJ, Straney L, Alexander J, et al. Mortality related to invasive infections, sepsis, and septic shock in critically ill children in Australia andNew Zealand, 2002–13: a multicentre retrospective cohort study. The Lancet Infectious Diseases. 2015;15:46–54. doi: 10.1016/S1473-3099(14)71003-5. https://doi.org/10.1016/S1473-3099(14)71003-5. [DOI] [PubMed] [Google Scholar]
- 15.Hartman ME, Linde-Zwirble WT, Angus DC, Watson RS. Trends in the epidemiology of pediatric severe sepsis. Pediatric Critical Care Medicine. 2013;14:686–93. doi: 10.1097/PCC.0b013e3182917fad. https://doi.org/10.1097/PCC.0b013e3182917fad PMid:23897242. [DOI] [PubMed] [Google Scholar]
- 16.Sano H, Kobayashi R, Iguchi A, et al. Risk factors for sepsis-related death in children and adolescents with hematologic and malignant diseases. Journal of Microbiology, Immunology and Infection. J Microbiol Immunol Infect. 2017;50:232–38. doi: 10.1016/j.jmii.2015.04.002. https://doi.org/10.1016/j.jmii.2015.04.002 PMid:26055687. [DOI] [PubMed] [Google Scholar]
- 17.Thompson GC. Sepsis in Children Admitted to Hospital Following Traumatic Brain Injury. In2014 AAP National Conference and Exhibition 2014. American Academy of Pediatrics [Google Scholar]
- 18.Thompson GC, Macias CG. Recognition and Management of Sepsis in Children: Practice Patterns in the Emergency Department. The Journal of Emergency Medicine. 2015;49:391–9. doi: 10.1016/j.jemermed.2015.03.012. https://doi.org/10.1016/j.jemermed.2015.03.012 PMid:26093939. [DOI] [PubMed] [Google Scholar]
- 19.Ellison AM, Ota KV, McGowan KL, Smith-Whitley K. Epidemiology of bloodstream infections in children with sickle cell disease. Pediatr Infect Dis J. 2013;32:560–3. doi: 10.1097/INF.0b013e318286c75b. https://doi.org/10.1097/INF.0b013e318286c75b PMid:23340560. [DOI] [PubMed] [Google Scholar]
- 20.Weiss SL, Fitzgerald JC, Pappachan J, et al. Global epidemiology of pediatric severe sepsis: thesepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med. 2015;191:1147–57. doi: 10.1164/rccm.201412-2323OC. https://doi.org/10.1164/rccm.201412-2323OC PMid:25734408 PMCid: PMC4451622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cruz AT, Perry AM, Williams EA, Graf JM, Wuestner ER, Patel B. Implementation of goal-directed therapy for children with suspected sepsis in the emergency department. Pediatrics. 2011;127(3):e758–e66. doi: 10.1542/peds.2010-2895. https://doi.org/10.1542/peds.2010-2895 PMid:21339277. [DOI] [PubMed] [Google Scholar]
- 22.Larsen GY, Mecham N, Greenberg R. An emergency department septic shock protocol and care guideline for children initiated at triage. Pediatrics. 2011;127:e1585–92. doi: 10.1542/peds.2010-3513. https://doi.org/10.1542/peds.2010-3513 PMid:21576304. [DOI] [PubMed] [Google Scholar]
- 23.Paul R, Neuman MI, Monuteaux MC, Melendez E. Adherence to PALS sepsis guidelines and hospital length of stay. Pediatrics. 2012;130(2):e273–e80. doi: 10.1542/peds.2012-0094. https://doi.org/10.1542/peds.2012-0094 PMid:22753559. [DOI] [PubMed] [Google Scholar]
- 24.Weiss SL, Fitzgerald JC, Balamuth F, et al. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Critical care medicine. 2014;42:2409. doi: 10.1097/CCM.0000000000000509. https://doi.org/10.1097/CCM.0000000000000509 PMid:25148597; PMCid: PMC4213742. [DOI] [PMC free article] [PubMed] [Google Scholar]


