Abstract
AIM:
To evaluate the feasibility and safety of mini abdominoplasty with liposuction under local tumescent anaesthesia (LA) as the sole anaesthetic modality.
METHODS:
The study included 60 female patients with a mean age of 33.3 ± 5.6 years. Local infiltration using a mixture of 1:1000 epinephrine (1 ml), 2% lidocaine (100 ml) and 0.5% Levobupivacaine (50 ml) in 2500 ml saline was started with Local infiltration started with the abdomen, outer thigh, hips, back, inner thighs and knees. After Mini Abdominoplasty with supplemental liposuction was conducted and application of suction drains wound closure was performed, and the tight bandage was applied. Pain during injection, incision and surgical manipulations was determined. Duration of postoperative analgesia, till oral intake and return home, patients and surgeon satisfaction scores were determined.
RESULTS:
All surgeries were conducted completely without conversion to general anaesthesia. Injection pain was mild in 46 patients, moderate in 10 and hardly tolerated in 4 patients. Incision pain was mild in 16 patients, while 44 patients reported no sensation. During the surgical procedure, 6 patients required an additional dose of LA. Meantime till resumption of oral intake was 1.6 ± 0.9 hours. Meantime till home return was 5.6 ± 2.4 hours. Twelve patients were highly satisfied, 18 patients were satisfied, and these 42 patients were willing to repeat the trial if required. Eight patients found the trial is good and only one patient refused to repeat the trial and was dissatisfied, for a mean total satisfaction score of 3.1 ± 0.9.
CONCLUSION:
Mini Abdominoplasty with liposuction could be conducted safely under tumescent LA with mostly pain-free intraoperative and PO courses and allowed such surgical procedure to be managed as an office procedure. The applied anaesthetic procedure provided patients’ satisfaction with varying degrees in about 97% of studied patients.
Keywords: Local anaesthesia, Mini Abdominoplasty, Liposuction, Pain scores, Satisfaction scoring
Introduction
Limited abdominoplasty is commonly performed under general anaesthesia with endotracheal intubation or manually controlled intravenous anaesthesia. Despite the surgeons’ preference of performing the procedure on patients under general anaesthesia; patients have anxiety over complications due to general anaesthesia. On the other hand, manually controlled infusion of intravenous anaesthesia had disadvantages including inefficient control of anaesthesia [1].
There was the widespread application of local anaesthesia for multiple surgical procedures and was proved effective with advantages extending to the postoperative period; Agbakwuru et al., [2] reported that hydrocelectomy under local anaesthesia and sedation is practicable and was tolerated and accepted by the adult patients. Parirokh et al., [3] found combining an inferior alveolar nerve block, and a buccal infiltration injection provided more effective anaesthesia in mandibular molars with irreversible pulpitis Also, Gun et al., [4] found the application of LA reduces bleeding during rhinoplasty and pain control postoperatively. Chia & Theodorou [5] reported excellent safety profile and short recovery period using laser-assisted liposuction and suction-assisted lipectomy with the patient under local anaesthesia and documented that the awake patient can participate in body positioning and to provide physiologic monitoring.
Through the development of instruments and the introduction of new drugs, various means of anaesthesia for breast surgery have been reported. More frequent use of a local anaesthetic combined with some form of intravenous sedation in office-based facilities has been reported. This change keeps hospital costs down as well as saving time for patients [6] [7].
The current study aimed to evaluate the feasibility and safety of performing reduction mastectomy under tumescent local infiltration anaesthesia as the sole anaesthetic modality.
Methods
The current prospective study was conducted at Anesthesia and General Surgery departments, Kasr Al-Eini University Hospital From Jan 2018 till June 2018. After approval of the study protocol and obtaining fully informed patients’ written consents, patients assigned for Mini Abdominoplasty with liposuction were enrolled in the study.
Patients with hormonal disturbances had body mass index (BMI) > 35 kg/m2 or required other plastic surgeries for contour configuration were excluded from the study. Also, patients had pathologies requiring surgical interference under any anaesthetic technique other than local anaesthesia was not enrolled in the study.
All patients underwent determination of body weight and height and calculation of BMI according to the equation: BMI = Wt (kg)/(Height in meter)2 [8]. A BMI of < 24.9 kg/m2 is considered normal; a person with a BMI of 25-30 kg/m2 is considered overweight but at low risk of serious medical complications, while those with a BMI of > 30, > 35 and > 55 kg/m2 are considered obese, morbidly obese and super-morbidly obese, respectively. Morbidity and mortality rise sharply when the BMI is > 30 kg/m2 [9]. Then, all patients had full clinical examination including general and abdominal examinations and were photographed preoperatively in lateral and front positions. The planned incisions were marked with an irremovable marker pen.
The local anaesthetic solution was prepared using a mixture of 5 ml of 1:1000 of epinephrine, 100 ml of 2% lidocaine, 50 ml of 0.5% Levobupivacaine in a 2500 ml saline solution. All patients were premedicated with midazolam in a dose of 0.05 mg/kg, and ondansetron 4mg and dexamethasone (0.3 mg/kg, maximal dose 8 mg) were administered IV to prevent nausea and vomiting.
Local infiltration started with the abdomen, outer thigh, hips, back, inner thighs and knees. After Mini Abdominoplasty with supplemental liposuction was conducted and application of suction drains wound closure was performed, and the tight bandage was applied.
Evaluated intraoperative data included severity of injection pain, incision pain and pain during surgical manipulation using 4-points verbal analogue scale with 0: no pain, 1: mild pain not required additional dose of LA, 2: moderate pain required additional doses of LA and 3: severe pain not responding to additional doses of LA and required intravenous sedation or conversion to general anaesthesia.
Throughout operative procedure; heart rate, systolic, diastolic and mean blood pressures were non-invasively monitored and recorded before the start of injection of LA (baseline), after full injection, at time of skin incision and closure and after transfer to post-anaesthetic care unit (PACU).
Postoperative evaluation included determination of the duration of analgesia determined as duration elapsed since the time of start of surgery till request of postoperative rescue analgesia. The frequency of postoperative nausea and vomiting (PONV) and requirement of additional doses of antiemetics. Total postoperative hospital stay was determined.
Patients’ satisfaction was evaluated using 5-point satisfaction score with 4: Highly satisfactory and will request a similar anaesthetic procedure whenever required, 3: Satisfactory and will request it once again if required, 2: Good and may request it once again if required, 1: unsatisfactory and may or may not request it once again if required, 0: Dissatisfactory and will not request it once again if required.
Surgical outcome included the frequency of seroma collection, hematoma formation and development of wound infection. Surgeon’ satisfaction was evaluated using a 5-point satisfaction score with 4: Highly satisfactory and will request for similar procedures, 3: Satisfactory and will request it once again if required, 2: Good and may request it once again if required, 1: Bad and will not request it once again if required, 0: unsatisfactory and will not request it once again if required.
Obtained data were presented as mean±SD, ranges, numbers and ratios. Results were analysed using Wilcoxon’s ranked test for unrelated data (Z-test) and Chi-square test (X2 test) for numerical data. Statistical analysis was conducted using the SPSS (Version 15, 2006) for Windows statistical package. P value < 0.05 was considered statistically significant.
Results
The study included 60 female patients with a mean age of 33.3 ± 5.6; 23-43 years. Only 16 patients were overweight, and 44 patients were obese, with a total BMI of 31.7 ± 2.1; range: 26.3-33.9 kg/m2. 14 patients were of ASA grade II, and 46 patients were of ASA grade I, (Table 1).
Table 1.
Patients’ demographic data
| Data | Findings | |||
|---|---|---|---|---|
| Age (years) | Strata | ≤ 25 | 6 (10%) | 23.3 ± 0.6 (23-24) |
| > 25-30 | 12 (20%) | 28 ± 1.1 (26-29) | ||
| > 30-35 | 24 (40%) | 32.5 ± 1.9 (30-35) | ||
| > 35-40 | 8 (13.3%) | 38 ± 1.2 (37-39) | ||
| > 40 | 10 (16.7%) | 42 ± 1 (41-43) | ||
| Total | 60 (100%) | 33.3 ± 5.6 (23-43) | ||
| ASA grade | I | 46 (76.7%) | ||
| II | 14 (23.3%) | |||
| Weight (kg) | 88.5 ± 5.3 (75-95) | |||
| Height (cm) | 167.2 ± 2.9 (162-172) | |||
| BMI (kg/m2) | Strata | 25-30 | 16 (26.6%) | 28.7 ± 1.1 (26.3-29.8) |
| > 30 | 44 (70.4%) | 32.7 ± 1 (30.4-33.9) | ||
| Total | 60 (100%) | 31.7 ± 2.1 (26.3-33.9) | ||
Data are presented as numbers & mean ± SD; percentages & ranges are in parenthesis.
All anaesthetic procedures were conducted uneventfully, and no patient was excluded because of the intraoperative refusal of injection. 46 patients found injection pain was mild, 10 patients found it moderate and only 4 patients found it severe but could be hardly tolerated. On the start of the surgical procedure, 16 patients reported the mild sensation of the incision, while the remaining 44 patients reported no sensation and could not notify if the wound was made or not.
During the surgical procedure, no patient required conversion to general anaesthesia and all surgeries were completed under LA. Only 6 patients required an additional dose of LA; 4 during the procedure and 2 during wound closure, while 26 patients had mild tension pain during the procedure but not required additional anaesthesia and 28 patients had no sensation either during dissection or during wound closure, (Table 2 and Figure 1).
Table 2.
Procedural pain data
| Data | Findings | |
|---|---|---|
| Injection pain | Mild (score = 1) | 46 (76.7%) |
| Moderate (score = 2) | 10 (16.7%) | |
| Severe (score = 3) | 4 (6.6%) | |
| Total score | 1.3 ± 0.6 (1-3) | |
| Incision pain | No (score = 0) | 44 (73.3%) |
| Mild (score = 1) | 16 (26.7%) | |
| Surgical procedural pain | No (score = 0) | 28 (46.7%) |
| Mild (score = 1) | 26 (43.3%) | |
| Moderate (score = 2) | 6 (10%) | |
Data are presented as numbers & mean ± SD; percentages & ranges are in parenthesis
Figure 1.
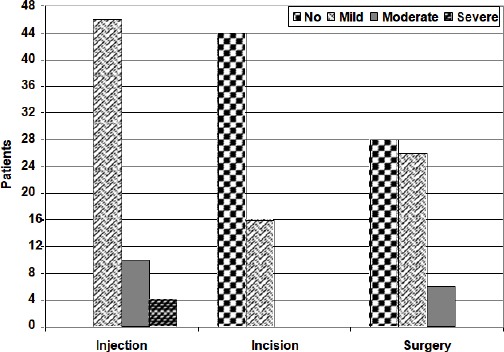
Patients distribution according to pain scores during infiltration anaesthesia and surgery
Throughout the study period, hemodynamic parameters were stable, despite the increased levels detected at the time of start of injection. However, at the time of skin incision, hemodynamic measures started to re-stabilise, and at the time of admission to PACU, all measures were non-significantly different compared to baseline measures, (Table 3).
Table 3.
Mean levels of hemodynamic measures estimated throughout the observation period
| Parameter | Baseline | 1-min after full injection | Skin incision | Wound closure | Admission to PACU |
|---|---|---|---|---|---|
| HR (beat/min) | 86.7 ± 2.2 | 89.7 ± 3.9 | 88 ± 5.6 | 87.5 ± 3.2 | 87.1 ± 2.2 |
| SBP (mmHg) | 107.3 ± 9.1 | 118.9 ± 5.6 | 113.4 ± 3.9 | 108.3 ± 8.6 | 108.8 ± 8 |
| DBP (mmHg) | 72.5 ± 3.8 | 74.4 ± 4.5 | 70 ± 2.9 | 70.5 ± 2.5 | 72.1 ± 3.5 |
| MAP (mmHg) | 84.1 ± 4.8 | 89.2 ± 4.4 | 84.5 ± 2.1 | 83.1 ± 3.5 | 84.3 ± 3.9 |
Data are presented as mean ± SD.
Eight patients (13.3%) complained of postoperative nausea, and one of them had one attack of vomiting, these patients received metoclopramide injection, and their oral intake was postponed till relieve of nausea sensation, while the remaining 52 patients (86.7%) resumed oral intake within their first 2-hr PO. Meantime till resumption of oral intake of 1.6 ± 0.9; 1-4 hours.
A group of 18 patients (30%) did not request rescue analgesia during their PACU stay and were discharged within the first 4-hr PO. 26 patients (43.3%) required PO rescue analgesia once after PACU transfer and were discharged within the first 6-hr PO. Six patients (10%) required two doses of rescue analgesia and were discharged within 9 hours PO. Only 4 patients (6.7%) requested rescue analgesia for three times and had delayed home return till 12 hours PO, (Figure 2).
Figure 2.
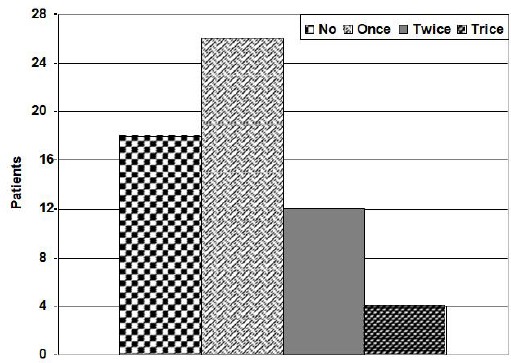
Patients distribution according to the frequency of requests of rescue PO analgesia
Meantime till home return was 5.6 ± 2.4; 3-12 hours. Despite all patients completed their operative course without conversion to general anaesthesia; 24 patients were highly satisfied; 18 patients were satisfied, and these 42 patients were willing to repeat the trial if required. 16 patients found the trial is a good one and may repeat it if required, while only 2 patients refused to repeat the trial and were dissatisfied, for a mean total satisfaction score of 3.1 ± 0.9; range: 1-4, (Table 4 and Figure 3).
Table 4.
Postoperative data
| Data | Findings | |||
|---|---|---|---|---|
| PONV | Yes | Nausea | 6 (10%) | |
| Vomiting | 2 (3.3%) | |||
| No | 52 (86.7%) | |||
| Time till resumption of oral intake (hours) | 1 | 38 (63.3%) | ||
| 2 | 14 (23.3%) | |||
| 3 | 4 (6.7%) | |||
| 4 | 4 (6.7%) | |||
| Total | 1.6 ± 0.9 | |||
| PO hospital stay (hours) | < 6 hours | 42 (70%) | 4.4 ± 0.8 (3-5) | |
| 6-9 hours | 12 (20%) | 8 ± 0.7 (7-9) | ||
| 9-12 hours | 6 (10%) | 10.7 ± 1.5 (9-12) | ||
| Total | 5.6 ± 2.4 (3-12) | |||
| Patients’ satisfaction scoring | Highly satisfied (Score = 4) | 24 (40%) | ||
| Satisfied (Score = 3) | 18 (30%) | |||
| Good (Score = 2) | 16 (26.7%) | |||
| Unsatisfied (Score = 1) | 2 (3.3%) | |||
| Dissatisfied (Score = 0) | 0 | |||
Data are presented as numbers & mean ± SD; percentages & ranges are in parenthesis
Figure 3.
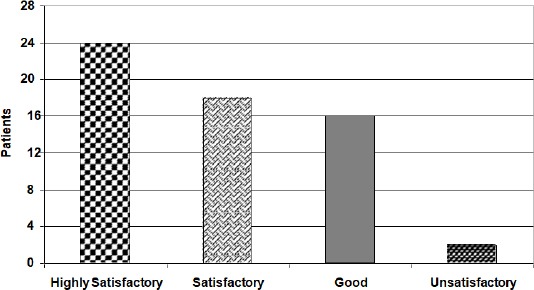
Patients’ distribution according to PO satisfaction by the anaesthetic procedure
Mean duration of wound drainage was 6 ± 1.1; 4-8 days; drain was removed after a mean duration of 4.8 days in 10 patients, and in 18 patients after a mean duration of 6.4 days and in 2 patients wound drainage was delayed for 8 days.
No wound infection or dehiscence was detected and wound healing was complete after a mean duration of 10 ± 1.1; range: 9-12 days; however, in 13 patients wound healing was complete, and stitches were removed on the 9th PO day, in 7 patients wound healing was complete, and stitches were removed on the 10th PO day, in another 7 patients wound healing was complete, and stitches were removed on the 11th PO day and in only 3 patients on the 12th PO day. No seroma was detected before the removal of stitches, (Table 5).
Table 5.
Postoperative wound data
| Data | Findings | ||
|---|---|---|---|
| PO wound drainage (days) | < 6 days | 20 (33.3%) | 4.8 ± 0.4 (4-5) |
| 6-7 days | 36 (60%) | 6.4 ± 0.5 (6-7) | |
| > 7 days | 4 (6.7%) | 8 | |
| Total | 8 ± 2.2 (8-16) | ||
| Duration till complete wound healing | 9 days | 26 (43.4%) | |
| 10 days | 14 (23.3%) | ||
| 11 days | 14 (23.3%) | ||
| 12 days | 6 (10%) | ||
| Total | 20 ± 2.2 (18-24) | ||
Data are presented as numbers & mean ± SD; percentages & ranges are in parenthesis.
Discussion
Tumescent local anesthesia (LA) infiltration was proved effective as the sole anesthetic modality for women undergoing Mini Abdominoplasty with supplemental liposuction as manifested by the findings that all surgeries were conducted completely without conversion to general anaesthesia and the high frequency of patients reporting mild or no pain during skin incision and/or surgical procedure with a minimal number required booster dose of LA during surgery. Additionally, 42 patients were satisfied by the applied anaesthetic procedure and willing to use the same procedure if required later on and the other 16 patients found it good anaesthetic modality and may request it if required, while only 2 patients were unsatisfied and refused similar procedure once again.
Patients attributed their satisfaction to many different causes; the sparing of exposure to general anesthesia and its possible risks, the sense of being awake during surgery, management as office procedure with resumption of oral intake and return home within few postoperative hours, the significant reduction of the cost of anesthesia and subsequent reduction of the hospital resource.
The reported findings supported that previously reported concerning breast surgery under LA; Carlson et al., [10] described unilateral total mastectomy for cancer under LA using the tumescent technique of infiltrating dilute lidocaine with epinephrine and reported no morbidity related to the surgery, patients were discharged 1-4 days after surgery, anaesthesia was adequate in all cases and there was no deviation from the described technique and concluded that the tumescent technique is a safe, effective method for performing a total mastectomy especially in patients who would not be considered candidates for general anaesthesia. Sleth et al., [11] found breast surgery under local infiltration anaesthesia provides adequate perioperative analgesia and is a technically low-risk procedure. Ranieri et al., [12] reported the feasibility of quadrantectomy and sentinel lymph node removal under LA in patients with ultrasound negative axillary lymph nodes. Groetelaers et al., [13] confirmed the safety of the sentinel lymph node biopsy under local anaesthesia in selecting patients for axillary lymph node dissection in breast cancer
Habbema [14] and Habbema & Alons [15] documented that breast liposuction using tumescent LA and powered cannulas is a safe and effective treatment modality for breast reduction. Kitowski et al., [16] retrospectively studied patients had breast cancer surgery including mastectomy, full axillary dissections, and expander or implant reconstruction and found that 74% of patients were able to undergo breast cancer surgery with local or paravertebral block regional anesthesia with no conversions to general anesthesia and no unplanned overnight admissions and only 10% of them developed postoperative nausea or vomiting, and concluded that most elective outpatient breast cancer surgery operations can be performed with the patients given local or regional anesthesia.
Kashiwagi et al., [17] reported that radical surgery for breast cancer could be performed under LA in all of the studied 42 patients and were not demanded to shift from local to general anaesthesia, and none of the serious complications was encountered and concluded that today’s radical operation under LA for breast cancer is a useful procedure as minimally invasive surgery.
The used anaesthetic solution was a mixture of one ml of 1:1000 of epinephrine, 100 ml of 2% lidocaine, 50 ml of 0.5% Levobupivacaine in a 2500 ml saline solution. The addition of adrenaline significantly reduced intraoperative blood loss allowing meticulous dissection of the excised lipoma so minimised seroma formation and so motivated the surgeon’ satisfaction by the applied anaesthetic procedure. In line with these data, Sleth et al., [11] used a similar mixture of lidocaine, ropivacaine and adrenaline during breast surgery and did not require conversion to general anaesthesia or supplementation with LA. Hardwicke et al., [18] reported that a meta-analysis of operative blood loss during reduction mastectomy showed a highly significant drop in operative blood loss in breasts infiltrated with epinephrine with a reduction in the need for blood transfusion and recommended the use of dilute epinephrine infiltration before reduction mammaplasty. In support of adding ropivacaine to the anaesthetic mixture, Manfè et al., [19] compared the efficacy of ropivacaine versus levobupivacaine for postoperative pain control in patients who underwent minor breast surgery and found ropivacaine results in more effective pain relief, while levobupivacaine provided long-term postoperative analgesia
Klein JA [20] found that. Tumescent technique for local anaesthesia improves safety in large-volume liposuction.
Kendler M et al., [21] use electrochemotherapy under local tumescent anaesthesia for treatment of cutaneous metastases particularly in elderly patients, in whom general anesthesia can be difficult because of comorbidity
Coldiron B et al., [22] give guidelines of care for tumescent liposuction.
It could be concluded that bilateral reduction mastectomy could be conducted safely under tumescent LA with mostly pain-free intraoperative and postoperative courses and allowed such surgical procedure to be managed as an office procedure. Moreover, the anaesthetic procedure provided patients’ satisfaction with varying degrees in about 97% of studied patients.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Bitar G, Mullis W, Jacobs W, et al. Safety and efficacy of office-based surgery with monitored anesthesia care/sedation in 4778 consecutive plastic surgery procedures. Plast Reconstr Surg. 2003;111:150–6. doi: 10.1097/01.PRS.0000037756.88297.BC. https://doi.org/10.1097/00006534-200301000-00025 PMid:12496575. [DOI] [PubMed] [Google Scholar]
- 2.Agbakwuru EA, Salako AA, Olajide AO, Takure AO, Eziyi AK. Hydrocelectomy under local anaesthesia in a Nigerian adult population. Afr Health Sci. 2008;8(3):160–2. PMid:19357743 PMCid: PMC2583265. [PMC free article] [PubMed] [Google Scholar]
- 3.Parirokh M, Satvati SA, Sharifi R, Rekabi AR, Gorjestani H, Nakhaee N, Abbott PV. Efficacy of combining a buccal infiltration with an inferior alveolar nerve block for mandibular molars with irreversible pulpitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(3):468–73. doi: 10.1016/j.tripleo.2009.11.016. https://doi.org/10.1016/j.tripleo.2009.11.016 PMid:20219602. [DOI] [PubMed] [Google Scholar]
- 4.Gun R, Yorgancılar E, Yıldırım M, Bakır S, Topcu I, Akkus Z. Effects of lidocaine and adrenaline combination on postoperative edema and ecchymosis in rhinoplasty. Int J Oral Maxillofac Surg. 2011;40(7):722–9. doi: 10.1016/j.ijom.2011.02.022. https://doi.org/10.1016/j.ijom.2011.02.022 PMid:21458231. [DOI] [PubMed] [Google Scholar]
- 5.Chia CT, Theodorou SJ. 1000 consecutive cases of laser-assisted liposuction and suction-assisted lipectomy managed with local anesthesia. Aesthetic Plast Surg. 2012;36(4):795–802. doi: 10.1007/s00266-012-9885-2. https://doi.org/10.1007/s00266-012-9885-2 PMid:22447150. [DOI] [PubMed] [Google Scholar]
- 6.Tahiri Y, Tran de QH, Bouteaud J, et al. General anaesthesia versus thoracic paravertebral block for breast surgery: a meta-analysis. J Plast Reconstr Aesthet Surg. 2011;64:1261–1269. doi: 10.1016/j.bjps.2011.03.025. https://doi.org/10.1016/j.bjps.2011.03.025 PMid:21486711. [DOI] [PubMed] [Google Scholar]
- 7.Kashiwagi S, Asano Y, Watanabe M, Takii M, Morisaki T, Aomatsu N, Nakamura M, Kawajiri H, Takashima T, Onoda N, Ishikawa T, Wakasa K, Hirakawa K. Day surgery of early breast cancer treated with breast-conserving operation following sentinel lymph node navigation biopsy under local anesthesia. Gan To Kagaku Ryoho. 2012;39(12):1914–6. PMid:23267928. [PubMed] [Google Scholar]
- 8.Bray GA. Pathophysiology of obesity. Am J Clin Nutr. 1992;55:488S–94S. doi: 10.1093/ajcn/55.2.488s. https://doi.org/10.1093/ajcn/55.2.488s PMid:1733117. [DOI] [PubMed] [Google Scholar]
- 9.Vella M, Galloway DJ. Laparoscopic adjustable gastric banding for severe obesity. Obes Surg. 2003;13(4):642–8. doi: 10.1381/096089203322190899. https://doi.org/10.1381/096089203322190899 PMid:12935369. [DOI] [PubMed] [Google Scholar]
- 10.Carlson GW. Total mastectomy under local anesthesia: the tumescent technique. Breast J. 2005;11(2):100–2. doi: 10.1111/j.1075-122X.2005.21536.x. https://doi.org/10.1111/j.1075-122X.2005.21536.x PMid:15730454. [DOI] [PubMed] [Google Scholar]
- 11.Sleth JC, Servais R, Saizy C. Tumescent infiltrative anaesthesia for mastectomy: about six cases. Ann Fr Anesth Reanim. 2008;27(11):941–4. doi: 10.1016/j.annfar.2008.08.011. https://doi.org/10.1016/j.annfar.2008.08.011 PMid:19004607. [DOI] [PubMed] [Google Scholar]
- 12.Ranieri E, Larcinese A, Barberi S, Caprio G, Naticchioni E, Civitelli L, Paglicci C, Pagni P, Zancla S, Rengo M, Di Giorgio A. Quadrantectomy and removal of the sentinel lymph node under local anaesthesia in the day hospital setting. Chir Ital. 2008;60(3):391–4. PMid:18709777. [PubMed] [Google Scholar]
- 13.Groetelaers RP, van Berlo CL, Nijhuis PH, Schapers RF, Gerritsen HA. Axillary recurrences after negative sentinel lymph node biopsy under local anaesthesia for breast cancer: a follow-up study after 5 years. Eur J Surg Oncol. 2009;35(2):159–63. doi: 10.1016/j.ejso.2008.07.017. https://doi.org/10.1016/j.ejso.2008.07.017 PMid:18789841. [DOI] [PubMed] [Google Scholar]
- 14.Habbema L. Breast reduction using liposuction with tumescent local anesthesia and powered cannulas. Dermatol Surg. 2009;35(1):41–50. doi: 10.1111/j.1524-4725.2008.34381.x. PMid:19076201. [DOI] [PubMed] [Google Scholar]
- 15.Habbema L, Alons JJ. Liposuction of the female breast: a histologic study of the aspirate. Dermatol Surg. 2010;36(9):1406–11. doi: 10.1111/j.1524-4725.2010.01649.x. https://doi.org/10.1111/j.1524-4725.2010.01649.x PMid:20629687. [DOI] [PubMed] [Google Scholar]
- 16.Kitowski NJ, Landercasper J, Gundrum JD, De Maiffe BM, Chestnut DH, Bottcher ML, Johnson JM, Johnson RL. Local and paravertebral block anesthesia for outpatient elective breast cancer surgery. Arch Surg. 2010;145(6):592–4. doi: 10.1001/archsurg.2010.77. https://doi.org/10.1001/archsurg.2010.77 PMid:20566982. [DOI] [PubMed] [Google Scholar]
- 17.Kashiwagi S, Takashima T, Asano Y, Morisaki T, Aomatsu N, Matsuoka J, Nakamura M, Kawajiri H, Onoda N, Ishikawa T, Hirakawa K. Lumpectomy and sentinel lymph node navigation surgery for breast cancer under local anesthesia. Gan To Kagaku Ryoho. 2011;38(12):2017–9. PMid:22202270. [PubMed] [Google Scholar]
- 18.Hardwicke JT, Jordan RW, Skillman JM. Infiltration of epinephrine in reduction mammaplasty: a systematic review of the literature. Plast Reconstr Surg. 2012;130(4):773–8. doi: 10.1097/PRS.0b013e318262f085. https://doi.org/10.1097/PRS.0b013e318262f085 PMid:23018690. [DOI] [PubMed] [Google Scholar]
- 19.Manfè AZ, Marchesini M, Bortolato A, Feltracco P, Lumachi F. Ropivacaine versus levobupivacaine for minor breast surgery in outpatients: inversion of postoperative pain relief efficacy. In Vivo. 2012;26(6):1075–7. PMid:23160696. [PubMed] [Google Scholar]
- 20.Klein JA. Tumescent technique for local anesthesia improves safety in large-volume liposuction. Plast Reconstr Surg. 1993;92:1085–98. https://doi.org/10.1097/00006534-199311000-00014 PMid:8234507. [PubMed] [Google Scholar]
- 21.Kendler M, Micheluzzi M, Wetzig T, Simon JC. Electrochemotherapy under tumescent local anesthesia for treatment of cutaneous metastases. Dermatolog Surg. 2013;39:1023–32. doi: 10.1111/dsu.12190. https://doi.org/10.1111/dsu.12190 PMid:23464631. [DOI] [PubMed] [Google Scholar]
- 22.Coldiron B, Coleman WP, III, Cox SE, Jacob C, Lawrence N, Kaminer M, Narins RS. ASDS guidelines of care for tumescent liposuction. Dermatol Surg. 2006;32:709–16. doi: 10.1111/j.1524-4725.2006.32159.x. https://doi.org/10.1111/j.1524-4725.2006.32159.x PMid:16706767. [DOI] [PubMed] [Google Scholar]


