Abstract
AIM:
This study aimed to compare the effects of dexmedetomidine and propofol in controlling the hemodynamic response following intubation of patients’ candidate intubation in the emergency department
METHODS:
A total of 114 patients were randomly assigned to one of 2 groups to receive one of the following treatments: dexmedetomidine 0.4 µg/kg (Group D, n = 57) and propofol 1–1.5 mg/kg/h (Group P, n = 57). Hemodynamic data such as the systolic blood pressure, diastolic blood pressure, arterial oxygen saturation and heart rate (HR) were recorded from the entrance to operation room to 5, 10 and 15 min after tracheal intubation
RESULTS:
Compared with group D, group P exhibited increases in mean arterial blood pressure (MAP), and systolic blood pressure significantly at all times and immediately after the endotracheal intubation. Moreover, the mean diastolic blood pressure changes due to tracheal intubation in group P were significantly more than group D immediately after the intubation. Furthermore, the mean heart rate changes immediately and 5 min after tracheal intubation was significantly higher in group P
CONCLUSION:
Our data suggest that the benefits of dexmedetomidine more than propofol in hemodynamic stability because propofol was associated with more variability in systolic/diastolic blood pressure, HR and MAP after endotracheal intubation.
Keywords: Dexmedetomidine, Propofol, Hemodynamic responses, intubation
Introduction
Laryngoscopy and tracheal intubation can cause tachycardia, high blood pressure, heart rate abnormalities, increased catecholamines concentration, myocardial ischemia, increased myocardial oxygen demand and increased intracranial pressure. On the other hand, it has been determined that stimulation is very severe due to laryngoscopy and intubation, as well as cutting the skin by the surgeon and can cause sympathetic stimulation, increased blood pressure and tachycardia in people whose sympathetic responses are not sufficiently slowed. These factors may cause potentially deadly risks such as cardiac ischemia, myocardial infarction and hemorrhagic cerebrovascular accident (CVA), so these issues enhance the importance of prescribing in patients [1]. Many drugs have been used to block hemodynamic responses such as opioids [2], vasoconstrictor drugs [3], beta receptor blockers [4] alpha receptor blockers [5] and benzodiazepines [6]. General anaesthesia includes those that may reduce blood pressure and reduce myocardial contractions, vasodilatation, and weaken the activity of the autonomic nervous system [7] [8] [9]. The unwanted side effects of intubation into the trachea cause such reactions as increased blood pressure and tachycardia and dis-arrhythmia [10] [11].
Dexmedetomidine is a highly selective alpha-2 adrenoreceptor agonist [12]. This drug is used as an adjuvant in general anaesthesia with central supportive effects, stabilises the hemodynamic state of the patient and has anaesthetic and analgesic effect [13] [15], which reduces the need for opioids and their complications [16] and decreases Stress response and quality recovery [17]. One of the ways to reduce hemodynamic changes, in addition to muscle anaesthetic and paralysis, is to provide sufficient depth of anaesthesia with fast-acting intravenous drugs that can provide quick and easy anaesthesia in the short term [18]. One of the major concerns in general anaesthesia is the hemodynamic stability in the patient is optimally based on the type and technique of surgery [19]. Compared to other anaesthetic drugs, Propofol has a faster return on alertness to the patient with minimal effects on the central nervous system, which inhibits increased heart rate and blood pressure in response to airway induction due to tracheal intubation, and thus changes can be made. Hemodynamically reduces the intubation [7]. In both of our medications, we are confronted with a drop in blood pressure and bradycardia, and both drugs control the effects of intubation on hemodynamic in large measure, in the meantime, we were looking for better drug combinations with fewer effects on hemodynamics in patients. And while controlling the hemodynamic responses induced by intubation, preventing excessive hypertension in the patient & apos;s heart and preventing hemodynamic imbalance.
Considering that so far no study has been done with this aim, we decided to conduct a study comparing the effect of propofol and dexmedmotidine on hemodynamic changes in patients undergoing intubation in the emergency department.
Methods
This study included a double-blind, randomised, clinical trial on emergency patient candidates in the emergency department of Vali-e-Asr Hospital. The clinical trial study data dated from 2015 to 2017. The clinical trial began in 2016 until the present. This research was performed at the Department of Emergency at our institution, and the registration number from the Iranian Registry of Clinical Trials is IRCT2016102520258N14 with the date of registration (2016-10-31). All procedures were done by the Helsinki declaration 1964, and its later amendments or comparable ethical standards in the emergency department of Vali-e-Asr Hospital and all experimental protocols were approved by the Ethics Committee of Shahid Beheshti University of Medical Sciences. All eligible patients provided written informed consent before entering this study.
Inclusion criteria
All patients who are candidates for intubation for one of the following reasons:
Protection pulmonary
↓PaO2/FiO2 (↓SpO2)
Pulmonary toileting
Positive pulmonary ventilation (PPV)
Positive end-expiratory pressure (PEEP)
Exclusion criteria
All patients who have been referred to the emergency department for suicide (due to drug interactions);
All patients who have been attempted more than twice for intubation.
Patients with multiple fractures of the upper and lower jaw and the possibility of severe intubation and kidney of patients with a probability of intubation, which is likely to be given several times a laryngoscopy.
All patients with a specific drug allergy to propofol and doxedemotomidine.
Sampling method
Sampling method according to the type of clinical study. The purposeful sampling method was used. Using random numbers, 114 patients were randomly divided into two equal groups of 57 (Propofol and Dexmedetumidine), respectively. All patients who had the inclusion criteria were using a random number table they were completely randomized into two groups of 57 patients with dimethomidine propofol (taking into account paired and random numbers).
A group of 114 patients were randomly divided into two groups of Propofol and Dexmedetomidine. For all patients, 2-3 micrograms/kg of fentanyl plus 2-3 mg/kg of lidocaine 2% were given intravenously as well as 2-3 mg of midazolam at first. Also, in both groups succinylcholine was given at a dose of 1 mg it was also given on kilograms. Then, for group 1 (group dexmedmotidine) 0.4 μg/kg dx dimethomidine and group 2 (propofol group), 1 to 1.5 mg/kg propofol was given to control hemodynamic responses of patients and prepared for intubation. Syringe volume in two groups was 10 Then, for both groups, the tracheal tube was selected and sprayed with lidocaine and after injection of the drugs by the resident responsible for the design and preparation for intubation of the patient by a resident of the largesic and intubate design, and finally the fixation tube And connected to the ventilator. The drugs were injected to patients for intravenous administration (dimethomidine and propofol) in syringes that were prepared by the researcher of Emergency Medicine in charge of the plan, and the volume was the same (10 cc). Then, according to the above explanations, the patients with Intubation candidates were contacted by emergency room researcher at the emergency department of Vali Asr Hospital. All of these patients had cryptography for inclusion in the study and had no exits from the study, the hemodynamic symptoms of the patients before and after the intubation (hemodynamic symptoms of patients including systolic blood pressure and diastolic blood pressure, and arterial blood pressure and heart rate and oxygen saturation) Resident co-registered.
This study was a double-blind study and patients were blinded to intubation and were not aware that the drugs were already prepared by the Resident of Emergency Medicine, and each of the syringes with the same volumes The cover was covered in a fridge and injected into the syringes during the injection of drugs in accordance with Nos. 1 and 2, and the resident researcher of the project, who was completely harmed by drugs and groups, informed the patients and developed a questionnaire for patients including their hemodynamic and demographic questions Completed. All the information obtained from the patients in the questionnaire of the project was registered and completed by the resident researcher.
Calculating sample size and number:
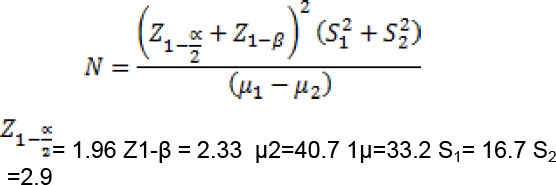
N = 57 individuals in each group-the total number of samples was 114. (S1, S2, μ1, μ2 were calculated according to reference number 18); Z1-α/2 = 1.96, Z1-β = 2.33.
Finally, the information obtained from the questionnaires was analysed by statistical software SPSS 20 and analysed in tables, and diagrams Statistical analysis was performed and the effect of two drugs dexmedmotidine and propofol on the control of hemodynamic response in patients after intubation was analysed.
Results
According to Table 1, there was a significant difference between the two groups in terms of average changes in MAP at different times, so that according to P = 0.00001, MAP changes in the Propofol group were significantly more than in the group of dexmodutomidine, and more simply in patients In the dexmodutomidine group, they were more stable after intubation.
Table 1.
Comparison of MAP changes in patients with emergency intubation candidates in two groups: Peropofol and Dexmedmotidine
| Average MAP changes | Peropofol group | Dexmedmotidine group | P-value |
|---|---|---|---|
| Immediately after intubation | 6.46 ± 4.6 | 9.4 ± 1.1 | P = 0.00001 |
| 5 min after intubation | 4.22 ± 1.5 | 1.2 ± 2.0 | P = 0.00001 |
| 10 min after intubation | 1.24 ± 5.4 | 7.9 ± 1.2 | P = 0.00001 |
| 15 min after intubation | 5.21 ± 8.3 | 1.8 ± 7.1 | P = 0.0001 |
According to Table 2, there was a significant difference between the two groups regarding mean SBP changes at different times, so that according to P = 0. 001, SBP changes were significantly more in the propofol group than in the dexmedmotidine group. In other words, patients in the dexmedmotidine group were more stable after intubation.
Table 2.
Comparison of mean systolic pressure changes (SBP) in patients with an emergency intubation candidate in two groups of peropofol and dexmedmotidine
| Average SBP changes | Peropofol group | Dexmedmotidine group | P-value |
|---|---|---|---|
| Immediately after intubation | 7.25 ± 8.5 | 1.13 ± 1.4 | P = 0.001 |
| 5 min after intubation | 2.14 ± 1.6 | 8.4 ± 1.2 | P = 0.001 |
| 10 min after intubation | 3.23 ± 2.4 | 8.13 ± 1.5 | P = 0.01 |
| 15 min after intubation | 9.21 ± 9.3 | 1.12 ± 8.4 | P = 0.01 |
There was a significant difference between the two groups in terms of average diastolic arterial pressure (DAP) changes immediately after intubation, and DAP changes were significantly higher in the propofol group after intubation than in the dexmodutomidine group (P = 0.01), but at other times after intubation 5, 10 and 15 minutes later), no significant difference was observed between the two groups (P ≥ 0.05) (Table 3).
Table 3.
Comparison of changes in mean diastolic pressure (DAP) in patients with emergency intubation candidates in two groups of peropofol and dexmedetomidine
| Average DAP changes | Peropofol group | Dexmedmotidine group | P-value |
|---|---|---|---|
| Immediately after intubation | 8.15 ± 8.4 | 3.10 ± 1.4 | P = 0.01 |
| 5 min after intubation | 1.1 ± 58.0 | 07.1 ± 64.0 | P ≥ 0.05 |
| 10 min after intubation | 3.2 ± 97.0 | 1.2 ± 1.1 | P ≥ 0.05 |
| 15 min after intubation | 9.7 ± 1.3 | 1.7 ± 2.4 | P ≥ 0.05 |
In terms of mean heart rate, there was a significant difference between the two groups immediately and 5 minutes after intubation, and the changes in heart rate immediately and 5 minutes after intubation in the propofol group were significantly higher than that of the dexamethymidine group (P = 0.0001), but in other times after intubation (10 and 15 minutes later), there was no significant difference between the two groups (P ≥ 0.05) (Table 4).
Table 4.
Comparison of mean heart rate changes (PR) in patients with emergency intubation candidates in two groups: Peropofol and Doxedemotomidine
| Average PR changes | Peropofol group | Dexmedmotidine group | P-value |
|---|---|---|---|
| Immediately after intubation | 6.22 ± 6.5 | 3.2 ± 4.1 | P = 0.0001 |
| 5 min after intubation | 9.11 ± 4.4 | 7.0 ± 12.0 | P = 0.001 |
| 10 min after intubation | 1.13 ± 8.3 | 8.12 ± 7.2 | P ≥ 0.05 |
| 15 min after intubation | 8.8 ± 7.3 | 4.9 ± 9.2 | P ≥ 0.05 |
There was no significant difference between the two groups regarding the mean oxygen saturation percentage at different times before and after intubation. Both groups are identical (P ≥ 0.05) (Table 5).
Table 5.
Comparative of changes in mean oxygen saturation (SPO2) in patients with emergency intubation candidates in two groups of Peropofol and Dexmedetomidine
| Average SpO2 changes | Peropofol group | Dexmedmotidine group | P-value |
|---|---|---|---|
| Immediately after intubation | 58.0 ± 23.0 | 49.0 ± 13.0 | P ≥ 0.05 |
| 5 min after intubation | 1.1 ± 85.0 | 4.1 ± 27.0 | P ≥ 0.05 |
| 10 min after intubation | 4.1 ± 56.0 | 02.1 ± 45.0 | P ≥ 0.05 |
| 15 min after intubation | 3.1 ± 33.0 | 40.1 ± 28.0 | P ≥ 0.05 |
There was no significant difference between the two groups regarding mean age and percentage of sexual intercourse. Both groups are identical (P ≥ 0.05) (Table 6).
Table 6.
Comparison of the mean age and gender prevalence of patients with emergency intubation candidates in the two groups of peropofol and dexmedmotidine
| Groups | Peropofol group | Dexmedmotidine group | P-value |
|---|---|---|---|
| Mean age | 5.45 ± 2.1 | 2.48 ± 8.1 | P ≥ 0.05 |
| Male frequency | 57.1% | 56.4% | P ≥ 0.05 |
Discussion
Achieving appropriate drug combinations for intubating patients with emergency intubation is one of the goals of emergency medicine and anesthesiologists. An appropriate drug combination that prevents tachycardia and dysrhythmia and hypertension caused by laryngoscopy and endotracheal intubation and it has always been the attention of the experts [1] [2]. Laryngoscopy and endotracheal intubation can cause tachycardia, hypertension, dysrhythmia, increased concentrations of catecholamines and even myocardial ischemia. In many cases, intubation of emergency patients has been accompanied by an increase in ICP. Therefore, the drug compounds that can control these changes are very important and considerable [1] [2] [3] [6]. These drugs include opioids, BZDs, barbiturates and alphabucers [1] [2] [3] [4] [6], while occasionally the administration of these drugs to endotracheal intubation leads to hemodynamic changes in patients [1] [6] [7] [9].
In this study, we compared the effects of dexmedmotidine and propofol on the control of hemodynamic responses after intubation of patients who were candidates for emergency intubation. The results of this study were that the mean of MAP changes immediately after intubation and at different times after intubation was significantly higher in the propofol group than in the dexmedmodyntidine group. Also, changes in systolic and diastolic blood pressure and heart rate at different times after intubation in the propofol group were greater than that of the Dexmedmotidine group. Therefore, these results indicate that the hemodynamic changes in patients with emergency intubation in the propofol group were significantly higher than that of the dexmedmodine group. In previous studies, the results are similar to those of our study. In a study by Chalam et al., in 2015, it was found that there was a significant difference between the two groups regarding MPA changes in systolic blood pressure And diastolic and heart rate was absent. In this study, patients were compared in the two groups of 50 patients with dimethomidine and propofol, which showed no significant difference between the hemodynamic changes of the two unrecognised, but better patients in the dexamethymidine tolerance group and better airway maintenance and autonomic ventilation in patients [20]. However, the results obtained in this study were not consistent with our study. In our study, hemodynamic changes were significantly lower in the dexedotomidine group than in the propofol group. But changes in SpO2 in our study, like the above study, did not show a significant difference between the two groups. The reason for this difference may be that in our study, hemodynamic changes after intubation have been investigated in patients undergoing emergency intubation. In the study of Jalam et al., This comparison was performed in patients in the operating room in the form of awaked intubation and with airway block. Another study by Blokoglo and colleagues in 2013 compared the effects of dexmeditomidine plus propofol and doxedmotomidine with autoimide and doxedmotidine with thiopental on intubation of patients without loosening. 76 patients were divided into three groups and compared to each other. The results of this study showed that there was no significant difference in the hemodynamic changes between the 3 groups (P > 0.005). However, the need for muscle relaxant after intubation in the group consisting of dimethomidine and propofol was less than the other two groups which seem to be better than the two above-mentioned doses of dimethomidine and propofol [21].
The results obtained in this study were not consistent with our study, so in our study, hemodynamic changes in the dexmedmodyntidine group were less than that of the prophylaxis group. The reason for the difference in the results of these two studies is that in the study of Blokoglo and colleagues, the combination of two drugs, including dimethomidine-propofol and doxedmotomidine-auto anti and doxedmotidine-thiopental, were used, while in our study, doxmodetomidine and propofol were compared with each other alone. However, in both studies, patients with emergency intubation candidates were examined, and only the lack of changes in SpO2 between the studied groups was similar in the results of our study and Blokoglo was similar. In a study by Chang et al., in 2014 on children with patents Cardiac Heart Surgery Applicant. This study aimed to compare the effects of dexmeditoimidine and propofol on hemodynamic responses and SpO2 changes induced by intubation. The result of this study was that the hemodynamic changes induced by intubation in the dimethomidine group were lower than the propofol group (P = 0.01) In this study, 114 children were randomly divided into two groups of propofol and dexmedetomidine. The results of the comparison of the two groups were that changes in blood pressure and heart rate in the propofol group after intubation and after sternotomy was more than the group of dexmedotomidine (P < 0.01). The final result of this study indicated that dexmedmotomidine had a better effect on hemodynamic control in children undergoing cardiac surgery than Propofol [22]. The results of this study were completely consistent with our study. In our study, the hemodynamic changes induced by intubation in the dimethomidine group were lower than the propofol group. In both studies, there was no significant difference in SpO2 changes. It should be noted that despite our study on adult subjects who were candidates for emergency intubation and the study of Cheng et al., On children who were candidates for cardiac surgery, the final results were almost consistent. Another study by Karimian et al., in 2006 aimed at comparing the effect of propofol and ketamine on hemodynamic changes in patients during intubation and induction of anaesthesia. The final result was that there was a significant difference between hemodynamic changes after intubation and induction of anaesthesia between the two groups could not be seen. Hemodynamic stability was found to be greater in the ketamine group than Propofol [23]. In simple terms, the use of ketamine has led to less hemodynamic changes in patients. Approximately the results of this study were consistent with our study. In our study, hemodynamic changes induced by intubation in the propofol group were more than the group of dexmedotomidine. By comparing the results of our study and the above studies, we can say that the use of Dexmedmotidine, as a sedative drug, improves hemodynamic stability during intubation of patients. Dexmedetomidine is a high-quality selective agonist that is used as an adjuvant in general anaesthesia and contributes to the sustained hemodynamic status of patients with central sympathetic effects [12] [13] [15]. In addition to anesthetic and sedative effects, the anti-Has a pain and reduces the need for opioids and reduces stress responses and releases catecholamines [13] [15] [16]. These beneficial effects of dexmedmotidine have led to its use as a high hemodynamic stability stabilizer when Intubation of patients. For intubation of patients, dexmedmotvydine as an agonist has been shown to lead to appropriate hemodynamic stability in patients. Dexmedetomidine is in fact an agonist with rapid intravenous effects that can, in addition to anti-anxiety and sedative effects, reduce the responses resulting from the release of catecholamines. One of the important issues during the intubation of patients, both in the operating room and in the emergency room, is the creation of an optimal condition with hemodynamic stability, which seems to lead to optimal conditions for patients during intubation in view of the use of doxedemotomidine [19] [18]. Propofol also has fast and fairly fast and fast-moving effects compared to other anesthetic drugs and also has the least effect on the CNS, and by inhibiting hypertension and heart rate, it reduces responses from stimulation of intubation [22]. However, in our study, the hemodynamic changes induced by intubation in the propofol group were greater than that of the dimethomidine group. Therefore, the hemodynamic stability of patients in the Dexmedmotidine group was higher.
In conclusion, the results of this study showed that comparison of the MAP and systolic and diastolic blood pressure and heart rate in patients with emergency intubation candidates in the group of dexmedmotomidine was lower than that of propofol, but changes in SpO2 in the two groups did not have a significant difference.
Ethics approval and consent to participate
Ethics approval for this study was obtained from the Shahid Beheshti University of Medical Sciences Ethics Board. Written informed consent was obtained from each patient included in the study,
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
Abbreviations: MAP = Mean arterial blood pressure; HR = Heart rate; PPV = Positive pulmonary ventilation; PEEP = Positive end-expiratory pressure; CVA = Cerebrovascular accident; DAP = Diastolic arterial pressure
References
- 1.Kovac A. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1996;8(8):63–79. doi: 10.1016/0952-8180(95)00147-6. https://doi.org/10.1016/0952-8180(95)00147-6. [DOI] [PubMed] [Google Scholar]
- 2.Crawford D, Fell D, Achola K, Smith G. Effect of alfentanil on the presser and catecholamine responses to tracheal intubation. Br J Anaesth. 1987;59(6):707–12. doi: 10.1093/bja/59.6.707. https://doi.org/10.1093/bja/59.6.707 PMid:3111508. [DOI] [PubMed] [Google Scholar]
- 3.Stoelting R. Attenuation of blood pressure response to laryngoscopy and tracheal intubation with sodium nitropruside. Anesth Analg. 1979;58(2):116–9. https://doi.org/10.1213/00000539-197903000-00011 PMid:571234. [PubMed] [Google Scholar]
- 4.Vucevic M, Purdy G, Ellis F. Esmolol hydrochloride for the management of the cardiovascular stress response to laryngoscopy and tracheal intubation. Br J Anaesth. 1992;68(5):529–30. doi: 10.1093/bja/68.5.529. https://doi.org/10.1093/bja/68.5.529 PMid:1642945. [DOI] [PubMed] [Google Scholar]
- 5.Curran J, Crowley M, O'Sullivan G. Droperidol and endotracheal intubation. Anaesthesia. 1980;35(3):290–4. doi: 10.1111/j.1365-2044.1980.tb05099.x. https://doi.org/10.1111/j.1365-2044.1980.tb05099.x PMid:7396141. [DOI] [PubMed] [Google Scholar]
- 6.Taittonen M, Kirvela O. Cardiovascular and metabolic response to clonidine and midazolam premedication. Eur J Anaesthesia. 1997;14(2):190–6. doi: 10.1046/j.1365-2346.1997.00103.x. https://doi.org/10.1097/00003643-199703000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Miller R, Reves J, Glass P, Lubarsky D, McEvoy M. Miller's Anaesthesia. Philadelphia: Elsevier Churchill Livingstone; 2015. Intravenous non-opioid anaesthetics. [Google Scholar]
- 8.Saricaoglu F, Uzun S, Arun O, Arun F, Aypar U. A clinical comparison of etomidate-lipuro, propofol and admixture at induction. Saudi J Anaesth. 2011;5:62–6. doi: 10.4103/1658-354X.76509. https://doi.org/10.4103/1658-354X.76509 PMid:21655019 PMCid: PMC3101756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weisenberg M, Sessler D, Tavdi M, Gleb M, Ezri T, Dalton J, et al. Dose-dependent hemodynamic effects of propofol induction following brotizolam premedication in hypertensive patients taking angiotensin-converting enzyme inhibitors. J Clin Anesth. 2010;22:190–5. doi: 10.1016/j.jclinane.2009.07.008. https://doi.org/10.1016/j.jclinane.2009.07.008 PMid:20400005. [DOI] [PubMed] [Google Scholar]
- 10.Reagh O, Torres H, Rodríguez N, Gatica S. Alpha-2B adrenergic receptor mediated hemodynamic profile of etomidate. R Health Sci J. 2010;29:91–5. [PubMed] [Google Scholar]
- 11.Sarkar M, Laussen P, Zurakowski D, Shukla A, Kussman B, Odegard K. Hemodynamic responses to etomidate on induction of anesthesia in pediatric patients. Anesth Analg. 2005;101:645–50. doi: 10.1213/01.ane.0000166764.99863.b4. https://doi.org/10.1213/01.ane.0000166764.99863.b4 PMid:16115968. [DOI] [PubMed] [Google Scholar]
- 12.Savola J, Ruskoaho H, Puurunen J, Salonen J, Kärki N. Evidence for medetomidine as a selective and potent agonist at alpha 2-adrenoreceptors. J Auton Pharmacol. 1986;6(3):275–84. doi: 10.1111/j.1474-8673.1986.tb00654.x. https://doi.org/10.1111/j.1474-8673.1986.tb00654.x PMid:2880852. [DOI] [PubMed] [Google Scholar]
- 13.Ebert T, Hall J, Barney J, Uhrich T, Colinco M. The effects of increasing plasma concentrations of dexmedetomidine in humans. Anesthesiology. 2000;93(6):382–94. doi: 10.1097/00000542-200008000-00016. https://doi.org/10.1097/00000542-200008000-00016 PMid:10910487. [DOI] [PubMed] [Google Scholar]
- 14.Gurbet A, Basagan-Mogol E, Turker G, Ugun F, Kaya F, Ozcan B. Intraoperative infusion of dexmedetomidine reduces perioperativeanalgesic requirements. Can J Anaesth. 2006;53(5):646–52. doi: 10.1007/BF03021622. https://doi.org/10.1007/BF03021622 PMid:16803911. [DOI] [PubMed] [Google Scholar]
- 15.Hall J, Uhrich T, Barney J, Arain S, Ebert T. Sedative, amnestic, and analgesic properties of small-dose dexmedetomidine infusions. Anesth Analg. 2000;90(5):699–705. doi: 10.1097/00000539-200003000-00035. https://doi.org/10.1097/00000539-200003000-00035 PMid:10702460. [DOI] [PubMed] [Google Scholar]
- 16.Blaudszun G, Lysakowski C, Elia N, Tramer M. Effect of perioperative systemic alpha2 agonists on postoperative morphine consumption and pain intensity: systematic review and meta-analysis of randomized controlled trials. Anesthesiology. 2012;116(4):1312–22. doi: 10.1097/ALN.0b013e31825681cb. https://doi.org/10.1097/ALN.0b013e31825681cb PMid:22546966. [DOI] [PubMed] [Google Scholar]
- 17.Bekker A, Haile M, Kline R, Didehvar S, Babu R, Martiniuk F, et al. The effect of intraoperative infusion of dexmedetomidine on the quality of recovery after major spinal surgery. J Neurosurg Anesthesiology. 2013;25(1):16–24. doi: 10.1097/ANA.0b013e31826318af. https://doi.org/10.1097/ANA.0b013e31826318af PMid:22824921 PMCid: PMC3557800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sivilotti M, Ducharme J. Randomized double blind study on sedative and hemodynamics during rapid sequence intubation in the emergency department: The Shred study. Ann Emerg Mwd. 1998;31(3):313–24. https://doi.org/10.1016/S0196-0644(98)70341-5. [PubMed] [Google Scholar]
- 19.Yazdi B, Khalili M, Talebi H, Fotovat A, Nikaeen A. Effect of adding ketamine to propofol infusion on hemodynamics and recovery time of patients under cataract surgery. Anesthesiology and Pain. 2011;1:4. [Google Scholar]
- 20.Chalam K. A comparative study of intravenous dexmedetomidine-versus propofol-based sedation for awake fiberoptic intubation along with airway blocks in cervical discectomy patients. Karnataka Anaesthesia Journal. 2015;1(1):21–7. https://doi.org/10.4103/2394-6954.149716. [Google Scholar]
- 21.Bollucuoglu K, Hanci V, Yurtlu S, Okyay D, Ayoglu H, Turan I. Comparison of propofol-dexmedetomidine, tiopental-dexmedetomidine and etomidate-dexmedetomidine combinations'effects on the tracheal intubation conditions without using muscle relaxants. Bratisl Lek Listy. 2013;114(9):514–8. doi: 10.4149/bll_2013_107. https://doi.org/10.4149/BLL_2013_107. [DOI] [PubMed] [Google Scholar]
- 22.Cheng S, Hu D, Hei G. Comparision Dexmedetomidin and propofol in hyeamodynamic response in children with cardiovascular disease in heart surgery. Anesthesiology. 2014 [Google Scholar]
- 23.Karimian M, Emadi S, Nasiri E, Farzin D. Comparision of the effects of different doses of ketamine propofol on heamodynamic chandes of the patients during induction of anesthesia. J Mazandaran UnivMed Sci. 2006;16(54):7–13. [Google Scholar]


