Abstract
Background
The reader confidence and diagnostic accuracy of coronary CT angiography (CCTA) can be compromised by the presence of calcified plaques and stents causing blooming artifacts. Compared to conventional invasive coronary angiography(ICA), this may cause an overestimation of stenosis severity leading to false positive results. In a pilot study we tested the feasibility of a new coronary calcium image subtraction algorithm in relation to reader confidence and diagnostic accuracy.
Materials and Methods
Forty-three patients underwent clinically indicated ICA and CCTA using a 320–detector row CT. Median Agatston score was 510. Two datasets were reconstructed: a conventional CCTA (CCTAconv) and a subtracted CCTA (CCTAsub), where calcifications detected on non-contrast images were subtracted from the CCTA. Reader confidence and concordance with ICA for identification of >50% stenosis were recorded. We defined target segments on CCTAconv as motion free coronary segments with calcification/stent and low reader confidence. The impact of CCTAsub was assessed. No approval from the ethics committee was required according to Danish law.
Results
A total of 76 target segments were identified. The use of coronary calcium image subtraction improved the reader confidence in 66% of these segments. In target segments specificity (86% vs. 65%, p<0.01) and positive predictive value (71% vs. 51%, p=0.03) were improved using CCTAsub compared to CCTAconv, without loss in negative predictive value.
Conclusions
Our initial experience with coronary calcium image subtraction suggests that it is feasible and could lead to an improvement in reader confidence and diagnostic accuracy for identification of significant coronary artery disease.
Keywords: Coronary, Subtraction, CT, CCTA, Angiography
1.1Introduction
Coronary CT Angiography (CCTA) is an established method for the evaluation of patients with suspected coronary artery disease(CAD).1;2 The method is suitable to exclude coronary atherosclerosis, but has shown less diagnostic accuracy in the presence of severe coronary calcification or implanted stents. These appear larger on CT than they are due to blooming artifacts, which may cause low reader confidence and overestimation of coronary stenosis severity with false positive results.3–5 This again may lead to more futile downstream diagnostic tests. As a result of the reduced performance, patients with high coronary calcium score are frequently excluded from examination with CCTA. As coronary calcifications are relatively common in patients with chest pain syndromes in need of diagnostic evaluation, this limitation may affect a large proportion of patients referred for CCTA.6
Volumetric CT Digital Subtraction Angiography(CTDSA) allows for the subtraction of coronary calcium and stents(CCTAsub). A contrast scan and a corresponding non-contrast scan are registered and subtracted. The result is a 3D volume in which coronary calcifications and stents have been removed leaving the contrast-enhanced blood in the lumen as the only high intensity material. First experiences with CTDSA were made by Yoshioka et al and Tanaka et al, who found that CTDSA may improve the evaluation of calcified segments on CCTA.7–9
In a pilot study setting we aimed to investigate the feasibility of CTDSA and the possible improvement in reader confidence and diagnostic accuracy of coronary segments with severe calcifications and stents using invasive coronary angiography(ICA) as reference.
2.1Materials and Methods
Between September 2012 and March 2013, patients suspected of CAD, undergoing sequential CCTA and ICA as part of clinical diagnostic evaluation at Rigshospitalet, Copenhagen or at the National Institute of Health, Maryland were retrospectively screened and included if they had Agatston Score>50. Exclusion criteria were kidney dysfunction, atrial fibrillation, implanted cardiac device and heart rate>75bpm during the scan. The Danish Committee System on Health Research Ethics deemed that this retrospective, anonymized analysis of clinically acquired coronary calcium scans and CCTA was exempt from additional institutional review. IRB from NIH was approved(Clinicaltrials.gov:NCT01621594).
The CCTA image reader confidence and diagnostic accuracy of CCTA to identify a>50% coronary artery stenosis using conventional image data(CCTAconv) and CCTAsub was assessed in coronary artery target segments using ICA as a reference. A coronary artery target segment was defined as a motion free coronary segment with poor CCTA reader confidence due to stent or calcium blooming artifacts.
2.2Invasive Coronary Angiography
Clinically indicated ICA was obtained according to clinical routine and international guidelines. All patients had ICA performed within 30 days of the CT-scan. Evaluation of the presence of obstructive CAD(defined as>50% luminal diameter stenosis) was performed visually according to clinical practice in target segments in a standard 17-segment model10, by an expert reader unaware of the CT findings.
2.3CT Image Acquisition
CCTA was performed using a 320-detector row CT scanner (Aquilion ONE, Toshiba, Japan) with 0.5-mm detector elements and a rotation time of 350ms. The software included a dose reduction technology (Adaptive Iterative Dose Reduction 3D, AIDR3D). The protocol consisted of a non-contrast scan followed by a contrast-enhanced scan, according to a standard acquisition protocol. This represents a two-breathhold subtraction approach.9
For each patient, tube voltage and tube current were determined using the automated exposure control function (SUREExposure) with a target image noise level of SD 33 or 55 for non-contrast scan and SD 33 or 40 for contrast scan. Depending on BMI either 100kV or 120kV was used for both scans. The scans were obtained in diastolic phase using the prospective scan mode and were reconstructed at 0.5mm slice thickness and 0.25mm interval with an FC03 algorithm and AIDR3D for subtraction. The non-contrast scan was additionally reconstructed with 3mm slice thickness and 3mm interval with an FC12 algorithm for evaluation of Agatston score. The effective radiation dose was estimated based on the dose-length-product (DLP, mGy*cm).11
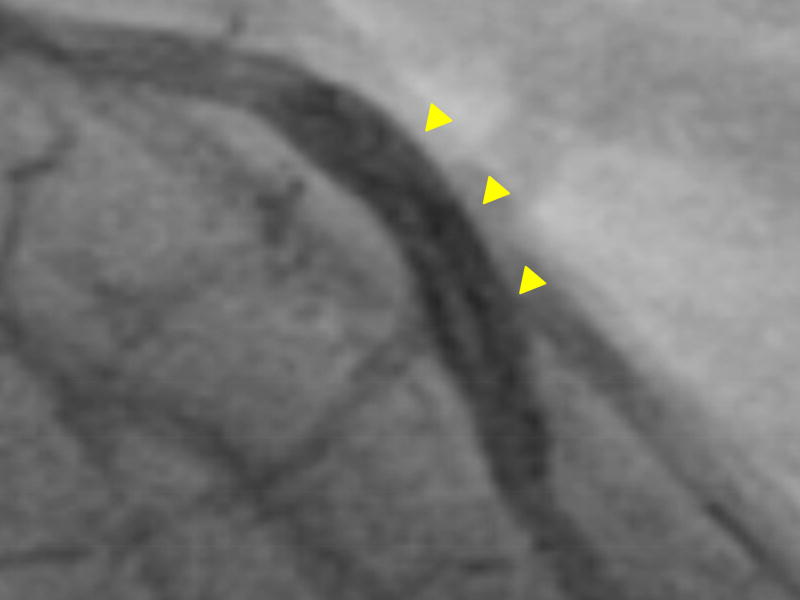
2.4CT Image Post Processing: Alignment and Subtraction
Accurate registration and subtraction of coronary images was performed using a dedicated algorithm, CTDSA, on the scanner console.12 For CTDSA two sets of volumetric data were required: with and without contrast enhancement of the coronary artery lumen. Following sequential image acquisition the two datasets were aligned using a combined rigid and non-rigid-registration algorithm and the registered pre-contrast volume was subtracted from the post-contrast volume(figure 1). The result was a 3D image volume in which coronary calcifications and stents had been removed leaving the contrast-enhanced blood in the lumen as the only high intensity material(figure 2).
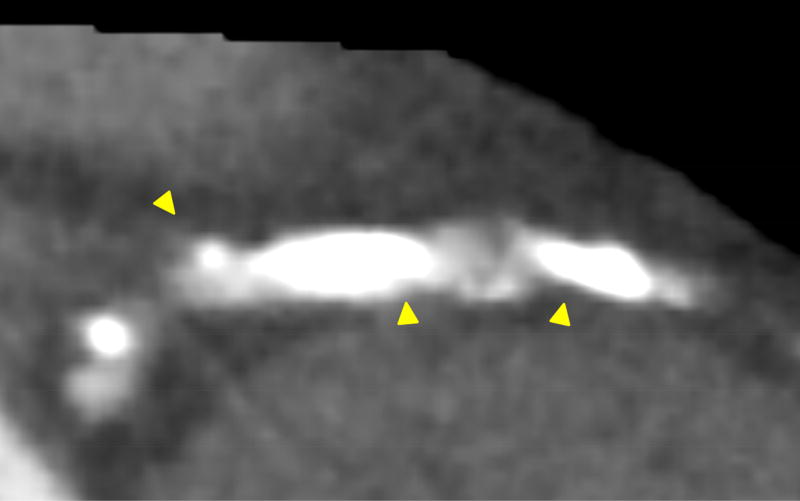
Figure 1.
Step #1: Non-rigid registration between contrast and non-contrast image. Step #2: Registered non-contrast image is subtracted from registered contrast image, resulting in a subtracted image.
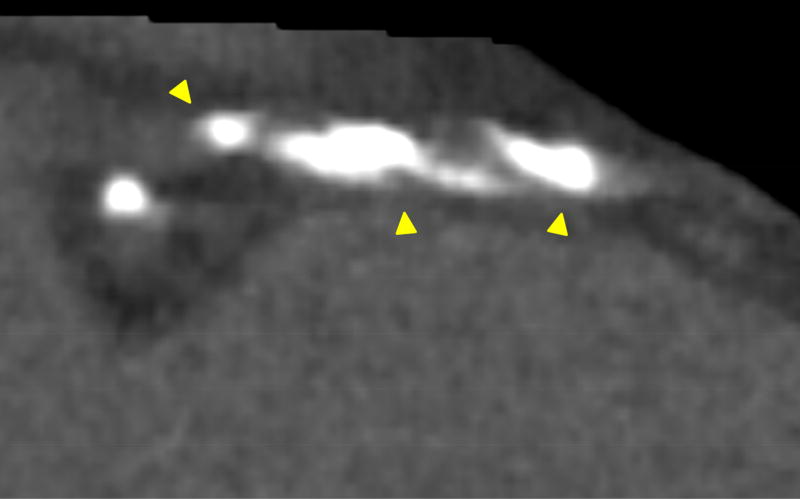
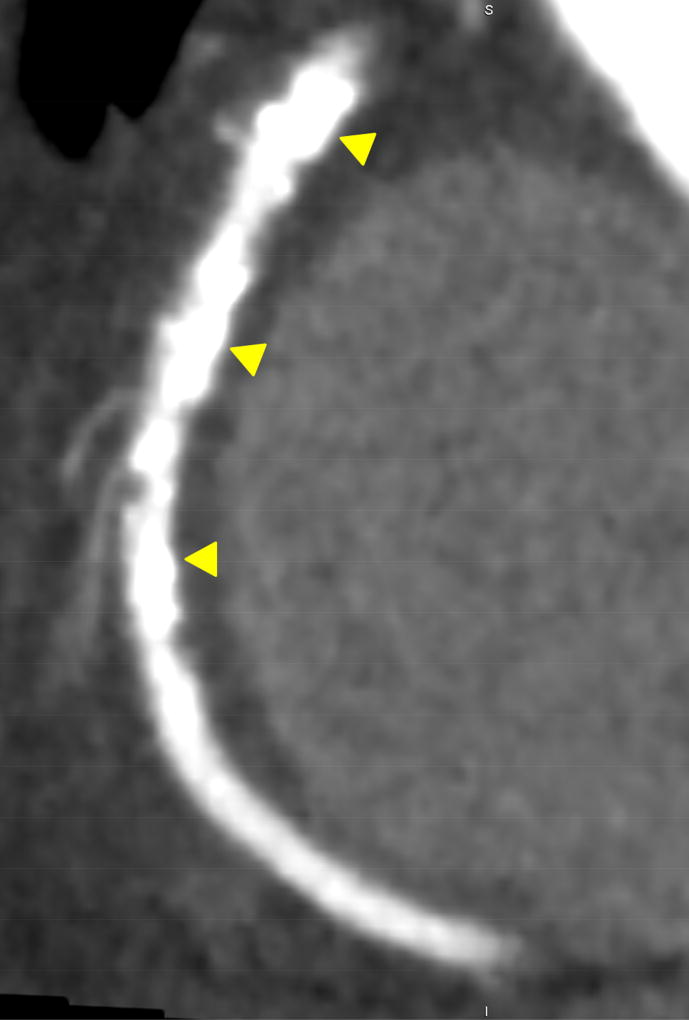
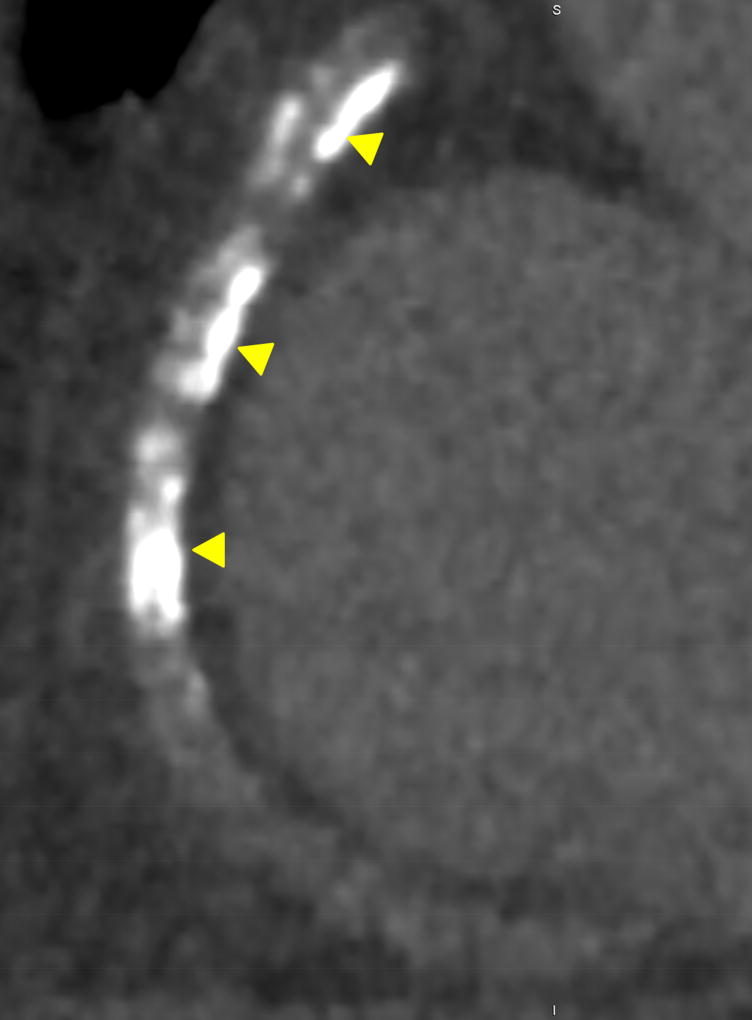
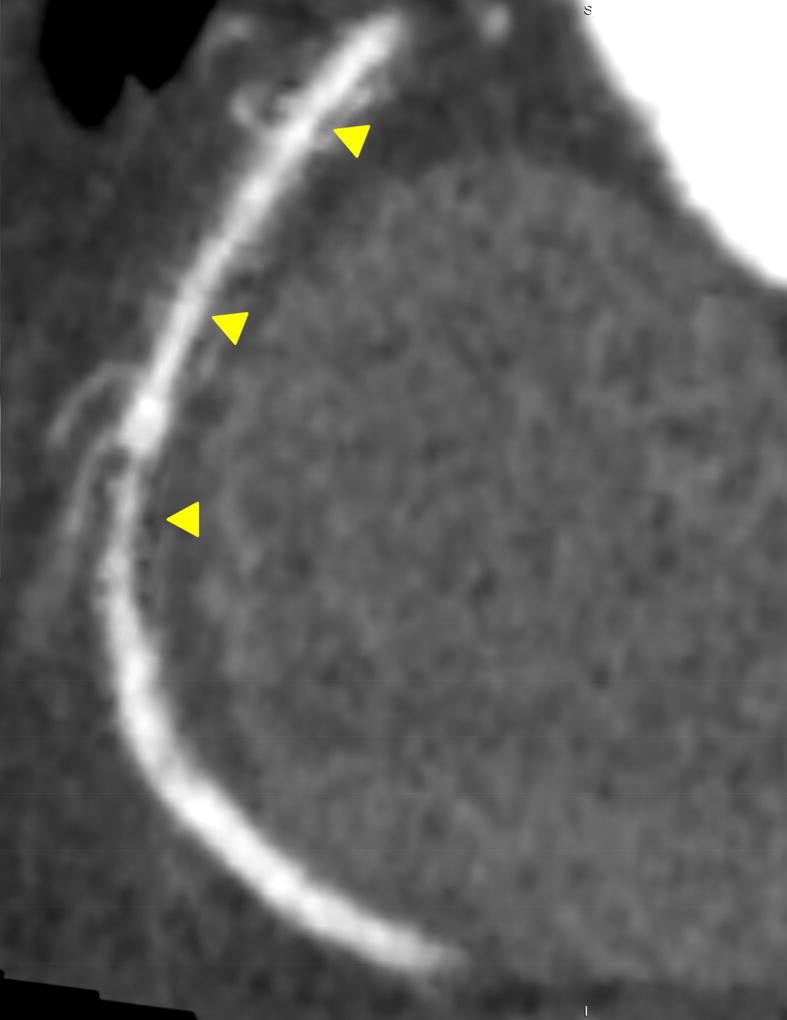
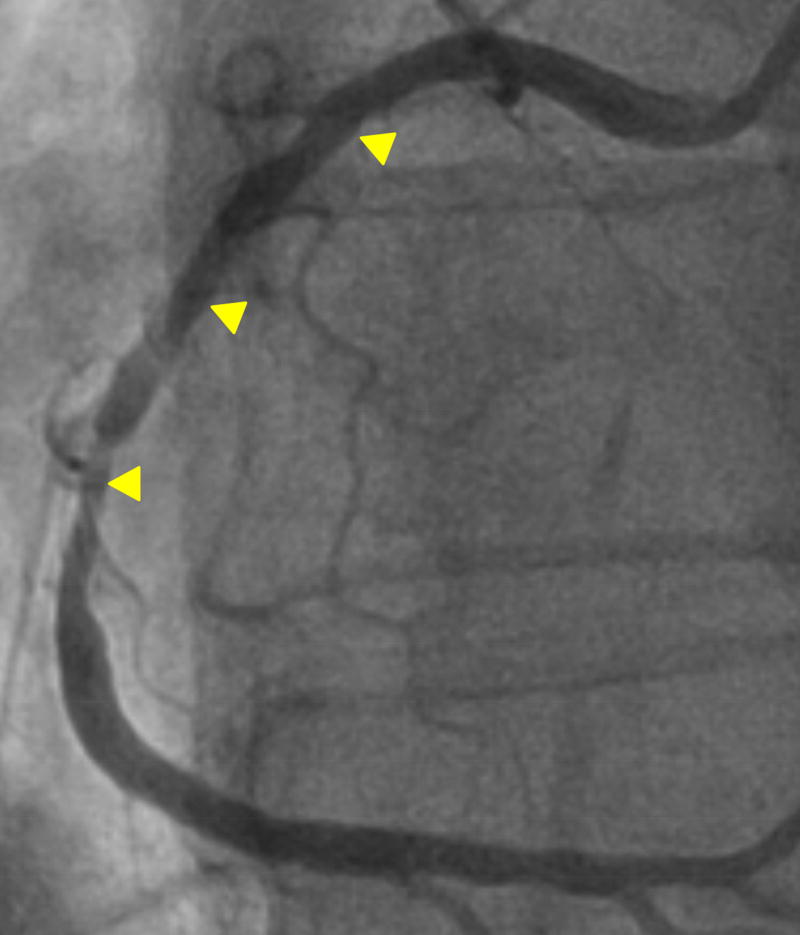
Figure 2.
In panel A a severely calcified right coronary artery can be seen. After performing subtraction (using the contrast and non-contrast image in panel A and B), a diagnostic image is obtained (Panel C), which closely resembles the invasive coronary angiogram (panel D). Panel E–H illustrate the corresponding subtraction process for a stented left anterior descending coronary artery. Similar to panel A-D, the non-diagnostic stent became interpretable after subtraction. Arrows indicate position of calcium and subtraction.
2.5CT Image Assessment
CCTAconv images were analyzed with commercial software(Vitrea6.3, Vital Images, USA) by one experienced reader using a 17-segment model10 with respect to presence of calcium/stents, obstructive CAD (defined as>50% luminal area stenosis), reader confidence, motion-artifacts and image noise-level. Noise-level was measured as the standard deviation of the mean HU in a circular ROI of 200mm2 in Aorta. Reader confidence was assessed on a 3-point scale with respect to evaluability of stenosis significance in a calcium/stent lesion (1=non-diagnostic: blooming throughout lumen, 2=partially-diagnostic: blooming in more than 50% of lumen, 3=diagnostic). CCTAsub images were analyzed four weeks later blinded to the results of the CCTAconv reading and were assessed for the same parameters in addition to presence of mis-registration artifacts. Mis-registration artifacts occurring from the alignment process were detected by comparing the CCTAsub and CCTAconv images(figure 3). Calcium scores were obtained by Agatstons method.13
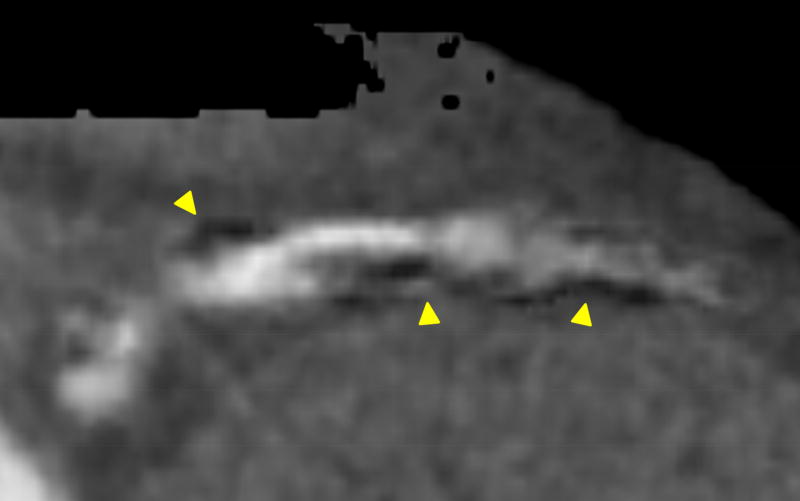
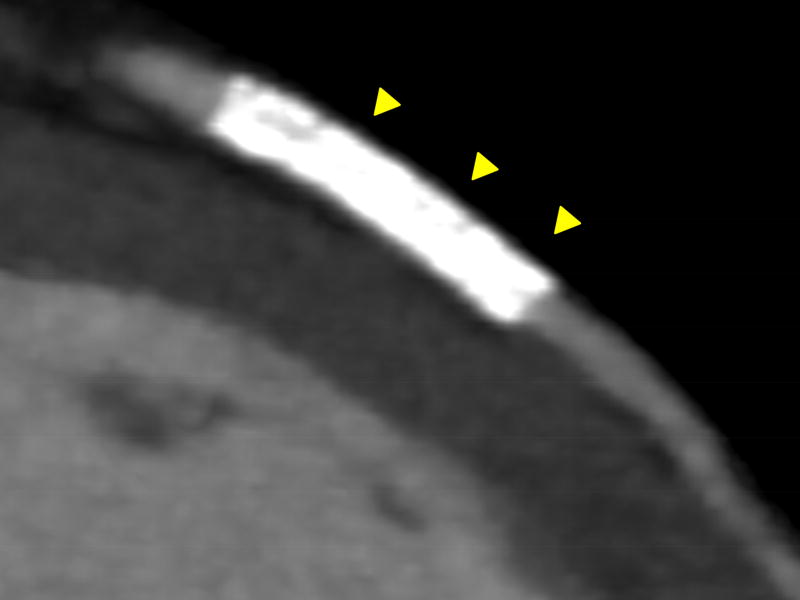
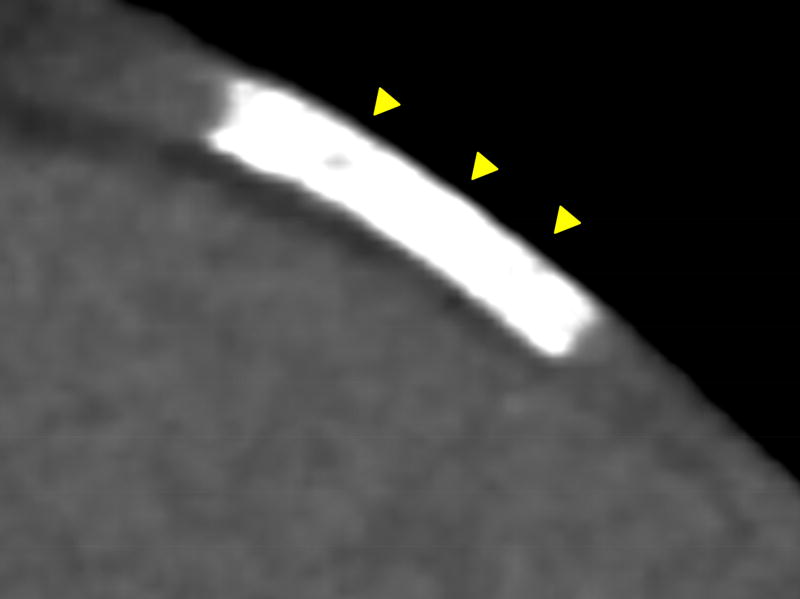
Figure 3.
Shows example of misregistration artifact. Calcium in contrast (A) and non-contrast (B) images is not identical. Therefore misregistration artifacts ocur in the resulting subtraction image (C). Calcium and artifacts are indicated by arrows.
2.6Accuracy and Reader Confidence Calculations
Accuracy and reader confidence was calculated for all target segments. Subgroup-analyses according to level of calcification (Agatston score>600)9, due to especially compromised diagnostic accuracy on CCTAconv in the presence of severe calcification4, and for proximal segments, as these are clinically most important segments. Proximal segments were defined as left main, proximal and mid left anterior descending artery, proximal and mid right coronary artery, and proximal left circumflex artery.
2.7Statistical Analyses
For data analysis, a commercially available software program was used (SAS9.3, SAS,USA). Data are presented as mean value with 95%-confidence interval or as amounts and percentage. P-values for comparison between diagnostic tests were calculated by McNemars test for sensitivity and specificity and by estimation in a multinomial distribution for predictive values. Delta Reader Confidence was calculated as reader confidence of CCTAconv minus reader confidence of CCTAsub.
3.1Results
Demographics of the 43 included patients are shown in table 1. The median radiation dose for the entire CT procedure was 4.6mSv. Seventy-six target segments were identified, including 67 calcified and 9 stent-segments (all drug eluting stents, diameter range:2.5–3.5mm, length range:8–28mm, drug eluting stents). ICA identified a significant coronary stenosis in 25(33%) target segments. Mean image noise was 28±6 HU in contrast images and 34±12HU in subtracted images(p<0.001). Mis-registration artifacts were recorded in 36 target segments(47%).
Table 1.
| Patient Demographics (n = 43) | |
|---|---|
| Women, n (%) | 15 (35) |
| Age years, mean (CI) | 67 (63–70) |
| BMI kg/m2, mean (range) | 29 (20–41) |
| >1 Risk factor, n (%) | 41 (95) |
| HR bpm, mean (CI) | 57 (55–59) |
| CACS total, median (range) | 510 (33–6995) |
| CACS < 600, n (%) | 20 (26%) |
| CACS > 600, n (%) | 56 (74%) |
CACS; coronary artery calcium score according to Agatston. CI; 95%-confidence interval. HR bpm; heart ratemeasured in beats per minute during CT-scan. BMI kg/m2; body mass index calculated as weight in kilograms divided by height in meters squared. Risk factors were: smoking, diabetes mellitus, hypertension, and hypercholesterolemia.
Based on CCTAsub images reader confidence was improved in 66%(50/76) of all target segments(table 2), 61%(41/67) of segments with calcification and in 100%(9/9) of the segments with coronary stents. Accuracy calculations for all target segments showed that specificity and PPV were significantly improved using CCTAsub as compared to CCTAconv, without loss in NPV(table 3).
Tabel 2.
Reader Confidence For All Target Segments, and for Sub-groups
| All target segments | CACS>600 | Prox. segm. | |
|---|---|---|---|
| Total | 76 | 56 | 47 |
| Improved | 50 (66%) | 32 (57%) | 32 (68%) |
| Re-class. 1-->2 | 1 | 1 | 1 |
| Re-class. 1-->3 | 3 | 2 | 2 |
| Re-class. 2-->3 | 46 | 29 | 29 |
CACS; coronary artery calcium score according to Agatston. Dist; distal. Prox; proximal. Re-class; Reclassification of segments with low reader confidence (1 or 2) by conventional CT to improved reader confidence (2 or 3) by subtracted CT. Segm; segment.
Table 3.
Accuracy for All Target Segments and Sub-groups
| All Target Segments (n=76) (prev.=33%) | CACS>600 (n=56) (prev.=36%) | Proximal Segments (n=47) (prev.=26%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| CCTAconv | CCTAsub | p-value | CCTAconv | CCTAsub | p-value | CCTAconv | CCTAsub | p-value | |
| Sensitivity, true pos/cond pos (%) | 19/25 (76) | 17/25 (68) | 0.63 | 16/20 (80) | 15/20 (75) | 1.00 | 10/12 (83) | 10/12 (83) | 1.00 |
| Specificity, true neg/cond neg (%) | 33/51 (65) | 44/51 (86) | <0.01 | 19/36 (53) | 31/36 (86) | <0.0001 | 23/35 (66) | 32/35 (91) | <0.01 |
| Positive predictive value, true pos/out pos (%) | 19/37(51) | 17/24 (71) | 0.03 | 17/33 (48) | 15/20 (75) | 0.01 | 10/22 (45) | 10/13 (77) | 0.01 |
| Negative predictive value, true neg/out neg (%) | 33/39 (85) | 44/52 (85) | 1.00 | 19/23 (83) | 31/36 (86) | 0.56 | 23/25 (92) | 32/34 (94) | 0.67 |
CACS; coronary artery calcium score according to Agatston. CI; 95%-confidence intervals. CCTAconv; conventional coronary CT angiogram. CCTAsub; subtracted coronary CT angiogram. Cond: Condition. Neg: Negative. Out: Outcome. Pos: Positive. Prev.; prevalence of >50%stenosis by ICA. P-values for comparison between diagnostic tests were calculated by McNemars test for sensitivity and specificity and by estimation in a multinomial distribution for predictive values.
4.1Discussion
Coronary CT Angiography is an established method to evaluate suspected CAD, but has shown decreased diagnostic accuracy and compromised reader confidence in the presence of severe calcification.4;5 We find that CCTAsub improves reader confidence and improves accuracy relative to CCTAconv, when using ICA as a reference.
Reader confidence on CCTAsub was improved to a diagnostic level in more than 60% of all target segments, which had on CCTAconv been deemed only partly or non-diagnostic. Reader confidence was improved in all of the 9 stent segments, suggesting that the subtraction algorithm performed especially well in coronary stent segments.
Specificity and PPV were improved in CCTAsub as compared to CCTAconv, without loss in NPV. This could imply that subtraction could bring down the number of false positives detected by CCTA. The largest improvement in PPV was seen in proximal segments, which could indicate that subtraction technique is especially suitable here.
Mis-registration artifacts were seen in approximately half of all target segments(36, i.e.47%). This could be caused by differences in location and shape of calcified plaques between the non-contrast and contrast images due to differences in the patient’s breathhold. In clinical practice, the overall reader confidence for diagnosis will most likely be augmented as both contrast and subtracted images will be available for diagnosis. Due to unchanged scan parameters, the radiation dose was the same as for routine clinical CCTA.
An approach with dual energy CT-system allowing reconstruction of virtual non-enhanced images is available and could potentially contribute to subtraction.
The current pilot results appear very promising, but the retrospective nature of data collection, the referral bias and the relatively low number of patients and target coronary segments are important limitations. Consequently a prospective trial–the C-Sub320 trial(Clinical trials.gov: NCT02011061)–has been initiated to overcome these limitations and further elucidate the potential improvements of diagnostic accuracy that may be achieved by the subtraction algorithm.
Highlights.
-
-
Subtraction is a novel technique.
-
-
Designed to more accurately assess stenosis in coronaries with calcium or stents.
-
-
Subtraction appears feasible.
-
-
Subtraction could lead to improvement in reader confidence and diagnostic accuracy.
Acknowledgments
Rigshospitalet and National Institute of Health have received technical support from Toshiba Medical Systems related to the present article. M.R. employee at Toshiba Medical Visualization Systems. A.K. employee at Toshiba Medical Systems. C.S. employee at Toshiba Medical Systems. Activities not related to this article: has received research support from Toshiba Medical Systems. Activities not related to this article: has received research support from Toshiba Medical Systems.
This work was supported in part internally by Interreg IVA. Lene Theil Skovgaard, associate professor at Department of Biostatistics, University of Copenhagen has assisted with the statistical methods.
List of Abbreviations
- CAD
Coronary Artery Disease
- CCTA
Coronary Computed Tomography Angiography
- CCTAconv
Conventional CCTA
- CCTAsub
Subtracted CCTA
- CTDSA
CT Digital Subtraction Angiography
- ICA
Invasive Coronary Angiography
- SD
Standard Deviation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures of Potential Conflicts of Interest: A.E.A. Activities related to this article: none to disclose. K.F.K. Activities related to this article: none to disclose. For the remaining authors no conflicts of interests to disclose.
References
- 1.Schroeder S, Achenbach S, Bengel F, Burgstahler C, Cademartiri F, de FP, George R, Kaufmann P, Kopp AF, Knuuti J, Ropers D, Schuijf J, Tops LF, Bax JJ. Cardiac computed tomography: indications, applications, limitations, and training requirements: report of a Writing Group deployed by the Working Group Nuclear Cardiology and Cardiac CT of the European Society of Cardiology and the European Council of Nuclear Cardiology. Eur Heart J. 2008;29:531–56. doi: 10.1093/eurheartj/ehm544. [DOI] [PubMed] [Google Scholar]
- 2.Mark DB, Berman DS, Budoff MJ, Carr JJ, Gerber TC, Hecht HS, Hlatky MA, Hodgson JM, Lauer MS, Miller JM, Morin RL, Mukherjee D, Poon M, Rubin GD, Schwartz RS. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Catheter Cardiovasc Interv. 2010;76:E1–42. doi: 10.1002/ccd.22495. [DOI] [PubMed] [Google Scholar]
- 3.Carrabba N, Schuijf JD, de Graaf FR, Parodi G, Maffei E, Valenti R, Palumbo A, Weustink AC, Mollet NR, Accetta G, Cademartiri F, Antoniucci D, Bax JJ. Diagnostic accuracy of 64-slice computed tomography coronary angiography for the detection of in-stent restenosis: a meta-analysis. J Nucl Cardiol. 2010;17:470–478. doi: 10.1007/s12350-010-9218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdulla J, Pedersen KS, Budoff M, Kofoed KF. Influence of coronary calcification on the diagnostic accuracy of 64-slice computed tomography coronary angiography: a systematic review and meta-analysis. Int J Cardiovasc Imaging. 2012;28:943–53. doi: 10.1007/s10554-011-9902-6. [DOI] [PubMed] [Google Scholar]
- 5.Vavere AL, Arbab-Zadeh A, Rochitte CE, Dewey M, Niinuma H, Gottlieb I, Clouse ME, Bush DE, Hoe JW, de RA, Cox C, Lima JA, Miller JM. Coronary artery stenoses: accuracy of 64-detector row CT angiography in segments with mild, moderate, or severe calcification--a subanalysis of the CORE-64 trial. Radiology. 2011;261:100–108. doi: 10.1148/radiol.11110537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, Paul N, Clouse ME, Shapiro EP, Hoe J, Lardo AC, Bush DE, de RA, Cox C, Brinker J, Lima JA. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med. 2008;359:2324–36. doi: 10.1056/NEJMoa0806576. [DOI] [PubMed] [Google Scholar]
- 7.Yoshioka K, Tanaka R. Subtraction coronary CT angiography for the evaluation of severely calcified lesions using a 320-detector row scanner. Current Cardiovascular Imaging Reports. 2011;4:437–46. [Google Scholar]
- 8.Tanaka R, Yoshioka K, Muranaka K, Chiba T, Ueda T, Sasaki T, Fusazaki T, Ehara S. Improved evaluation of calcified segments on coronary CT angiography: a feasibility study of coronary calcium subtraction. Int J Cardiovasc Imaging. 2013;29(Suppl 2):75–81. doi: 10.1007/s10554-013-0316-5. [DOI] [PubMed] [Google Scholar]
- 9.Yoshioka K, Tanaka R, Muranaka K. Subtraction coronary CT angiography for calcified lesions. Cardiol Clin. 2012;30:93–102. doi: 10.1016/j.ccl.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Raff GL, Abidov A, Achenbach S, Berman DS, Boxt LM, Budoff MJ, Cheng V, DeFrance T, Hellinger JC, Karlsberg RP. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr. 2009;3:122–36. doi: 10.1016/j.jcct.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 11.McCollough CH, Primak AN, Braun N, Kofler J, Yu L, Christner J. Strategies for reducing radiation dose in CT. Radiol Clin North Am. 2009;47:27–40. doi: 10.1016/j.rcl.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Razeto Marco, Brian Mohr, Kazumasa Arakita, Schuijf Joanne D, Andreas Fuchs, Kühl J Tobias, Chen Marcus Y, Kofoed Klaus F. Accurate, fully-automated registration of coronary arteries for volumetric CT digital subtraction angiography. 2014:9034–90343F-7. [Google Scholar]
- 13.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–32. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]