Abstract
Objectives. To examine the effect of patient navigation models on changes in housing status and its subsequent effects on HIV outcomes for 700 people living with HIV (PLWH) who were unstably housed with co-occurring substance use and psychiatric disorders across 9 demonstration sites in the United States between the years of 2013 and 2017.
Methods. Self-reported housing status was collected at baseline, and at 6 and 12 months during the intervention. HIV outcomes included linkage and retention in care, antiretroviral therapy prescription, and viral suppression collected via chart review.
Results. In the 12 months after the intervention, 59.6% transitioned to more stable housing. Compared with those who became or remained unstably housed, participants with greater stability achieved significantly higher rates of retention (adjusted odds ratio [AOR] = 2.12; 95% confidence interval [CI] = 1.11, 4.05), were more likely to be prescribed antiretroviral therapy (AOR = 2.06; 95% CI = 1.62, 2.63), and had higher rates of viral suppression (AOR = 1.62; 95% CI = 1.03, 2.55).
Conclusions. The use of patient navigators to create a network of services for PLWH who are unstably housed can improve housing stability and lead to improvements in HIV-related outcomes.
Recent data on the progress toward the goals of the National HIV/AIDS Strategy for 2020 found that homelessness rose among people living with HIV (PLWH), from 7.9% to 9.0%, moving away from the objective to reduce homelessness to no more than 5%.1 This trend is alarming given the strong evidence that stable housing is associated with reduced HIV risk behaviors, increased engagement in care, better adherence to antiretroviral therapy, and improved survival.2–8 Finding strategies to reverse this trend is paramount given that housing or shelter is a priority need affecting an estimated one third of out-of-care PLWH.9
The Health Resources and Services Administration Special Projects of National Significance Initiative “Building Medical Homes for Multiply Diagnosed HIV-Positive Homeless Populations” (HRSA Homeless Initiative) was designed to address the growing unmet need for housing and reduce the disparity in viral suppression rates among PLWH who experience homelessness, in accordance with the National HIV/AIDS Strategy’s objective to support comprehensive, coordinated patient-centered care for PLWH.1,10,11 The HRSA Homeless Initiative had 4 primary goals: (1) improve timely entry, engagement, and retention in HIV care and supportive services; (2) build and maintain sustainable linkages to mental health, substance use treatment, and HIV primary care; (3) increase access to stable or permanent housing; and (4) create a patient-centered medical home (PCMH) for PLWH who experience homelessness. Nine sites were funded to create this PCMH and common elements included (1) the use of dedicated navigators or care coordinators (“patient navigators”) to outreach and provide intensive individual and system coordination to reduce barriers to care and treatment and address unmet housing, food, and other needs; (2) mobile interdisciplinary care teams or colocation of services in shelter clinics or substance use treatment facilities to increase access to comprehensive HIV care and behavioral health services; and (3) partnerships with housing providers to obtain housing and housing assistance. The intervention was adapted to meet the specific needs of the population served and the local context. Some sites also provided funding for short-term emergency housing assistance.
Limited evidence exists for the effectiveness of PCMH models on HIV health outcomes for PLWH who experience homelessness.12 Studies have shown that navigation and case management models can increase engagement in care for PLWH exiting jails or at discharge from hospitalization.13–16 For PLWH experiencing homelessness, patient navigators can play a key role in the PCMH by forging relationships with providers, supporting patient self-management of their illness, and assisting with housing stability.17 We aimed to assess the HRSA Homeless Initiative on housing status and subsequent effects on HIV health outcomes for PLWH who experience homelessness.
METHODS
This was a prospective, nonrandomized study with a convenience sample of PLWH recruited from 9 sites across the United States. Eight sites were located in urban areas, and there was 1 rural site. The host organizational settings were 2 federally qualified community health centers (CommWell Health, Dunn, NC, and Family Health Centers of San Diego, San Diego, CA), 3 public health departments (San Francisco Department of Public Health, San Francisco, CA; City of Pasadena Public Health Department, Pasadena, CA; and Multnomah County Health Department, Portland, OR), 1 comprehensive HIV/AIDS service organization (Prism Health North Texas, Dallas, TX), and 3 outpatient or mobile clinics associated with large university-based or hospital systems (Harris Health System, Houston, TX; University of Florida Center for HIV/AIDS, Research, Education, and Service, Jacksonville, FL; and Yale University School of Medicine, New Haven, CT). All 9 sites were Ryan White Comprehensive Care agencies and provided HIV primary medical services at the time of enrollment.
Eligibility criteria for all sites included PLWH who were (1) aged 18 years or older, (2) history or current diagnosis of a substance use or mental health disorder, and (3) experiencing homelessness or unstable housing as defined by the US Department of Housing and Urban Development.18 Participants were recruited and screened via referrals from institutions (hospitals and other treatment facilities, jails, prisons), community agencies working with people experiencing homelessness, and review of clinic records for persons who were out of care or had a detectable viral load. Participants were enrolled and followed up to 12 months from September 2013 through February 2017. Data were collected via interview and medical chart review at baseline and 6 and 12 months after enrollment. Those enrolled were able to provide informed written consent for participation.
Intervention
As part of the medical home, patient navigators were clinical and nonclinical professional and peer staff who served as the member of the HIV care team responsible for linking PLWH to housing and health care services. All navigators were trained in principles of harm reduction, trauma-informed care, and motivational-interviewing techniques. Patient navigators provided practical services, such as obtaining IDs to access services, assistance with obtaining federally subsidized cell phones to keep track of appointments, education and support to reduce risk behaviors and promote medication adherence, linkages with private landlords and other social service providers to obtain housing and housing assistance, transportation assistance to medical and social service appointments, and referrals and linkages to substance use and mental health treatment. Patient navigators were distinct from and often worked collaboratively with the HIV medical case manager or a housing case manager. Further details of the intervention have been published elsewhere.17
Evaluation
Study staff consented participants into the study and completed an interview on paper or directly into an electronic form by using REDCap version 8.6.4 (Vanderbilt University, Nashville, TN) within 7 days of signing a consent form. Navigators completed daily forms to describe the types of services performed, location of services, and the length of time of the encounters. Study staff also conducted medical chart review to extract data on primary care visits, viral load and CD4 laboratory tests, prescription of antiretroviral therapy, and other comorbidities including psychiatric disorders. Pharmacy records were not available for this study.
To guide our evaluation, we used the Behavioral Health Model for Vulnerable Populations framework to identify the factors that have an impact on the HIV care continuum for our study population.19 Predisposing factors included sociodemographic factors, length of time being homeless, incarceration in the past 12 months, trauma history, and depression. Enabling resources included insurance status, social support, self-efficacy, barriers to care, and unmet needs for substance use treatment, mental health treatment, transportation, legal assistance, medication assistance, and food insecurity. Need factors reflected baseline severity of illness, physical and mental health functioning, and viral suppression.
Measures
The dependent variables were based on HRSA-defined measures for the HIV care continuum. Linked to care was defined as at least 1 HIV primary care visit within 90 days of enrollment for participants who were newly diagnosed or had been out of care for more than 6 months at the time of enrollment (n = 259). Retained in care was defined as 2 HIV primary medical appointments at least 90 days apart in the 12-month observation period; prescribed antiretroviral therapy in the past 6 months included receipt of existing and new prescriptions; and viral suppression was defined as the final viral load test at less than 200 copies per milliliter in the 12-month observation period.
The independent variable was change in housing status, defined by the type of places stayed in accordance with HRSA-defined criteria.20 Unstable housing was defined as emergency shelters or staying in public places not meant for human habitation (e.g., street, vehicle, abandoned building), jail or prison, shelter, or living in a hotel or motel for emergency purposes paid for by a program. Temporary housing included staying with friends or family, in a transitional or a temporary setting, a residential treatment facility, a skilled nursing or rehabilitation center, or a motel paid for by oneself. Stable housing included a rented or owned room or apartment paid for by self or permanent supported housing or subsidized housing through Housing Opportunities for Persons With HIV/AIDS (HOPWA) or other subsidy programs. Housing status changes were assessed during the 6- or 12-month follow-up periods. We collapsed changes in housing status from 3 to 2 categories to reflect (1) those who became or remained unstably housed versus (2) those who maintained or improved housing stability (i.e., stayed in temporary housing or moved into stable housing).
Other covariates included the predisposing, enabling, and need factors mentioned previously. Food insecurity was assessed with a dichotomized variable whether a person had barely anything to eat for 2 or more days in the past 30 days. Substance use risk was measured by using the World Health Organization’s Alcohol, Smoking and Substance Involvement Screening Test and categorized as low, moderate (problem behavior), or high (addictive behavior).21 Depression risk was assessed by using the 10-item Center for Epidemiological Studies–Depression Scale,22 with a score of 10 or greater indicating moderate to severe depression. Social support was assessed with a 5-item scale to examine types of support available in the past 4 weeks with higher scores indicating greater social support.23 Self-efficacy was measured across 3 domains: (1) ability to obtain health information and resources, (2) ability to get help when needed, and (3) ability to communicate with a health care provider. Each item was scored on a 10-item scale ranging from 1 = “Not confident at all” to 10 = “Totally confident.”24 Unmet need was determined from a list of services needed but unable to obtain during the previous 6 months. Barriers to care included personal, organization, and structural barriers to obtaining HIV primary care.25
Data Analysis
Of the 909 clients who were enrolled in the study, this sample included 700 participants with available interview and chart data analyzed for the outcomes of linked to care, retained in care, prescribed antiretroviral therapy, and viral suppression. We first performed univariate and bivariate statistical analyses to describe the characteristics of study participants and associated changes in housing status. We conducted propensity score–based analysis to balance the distributions of baseline variables by change in housing status on HIV health outcomes. Study site and baseline covariates that were associated with the bivariate analyses in housing status (P < .20) were included in the propensity scores. We then used the propensity scores to construct inverse probability weights that were applied in a logistic regression model of each HIV health outcome with the change in housing status. These models accounted for site clustering by using generalized estimating equations with exchangeable working correlation for data sets with a small number of clusters.26 We conducted all analyses in SAS version 9.4 (SAS Institute, Cary, NC).
RESULTS
As shown in Table 1, the majority of participants were male and persons of color (Hispanic or African American/Black), and the mean age was 43 years (SD = 10.5). At baseline, approximately 83% were unstably housed and 33% were recently incarcerated. Moderate to high risk of substance use was reported in 20.6% for opioids, 33.9% for amphetamines, 50.1% for cocaine, and 41.1% for alcohol. Approximately three quarters of participants reported moderate to severe depressive symptoms. Approximately 40% reported experiencing trauma, including physical injury or sexual assault. The average social support score was 11.3 (SD = 5.2), indicating little or some support in the past 4 weeks. Approximately 58% reported barely having food to eat in the past 30 days. Participants reported an average of 3.5 (SD = 2.3) unmet needs for services. The average number of barriers to accessing health care was 3.3 (SD = 3.2). On average, participants had been living with HIV for 11.0 (SD = 8.8) years, and almost half (49.9%) were virally suppressed at baseline.
TABLE 1—
Characteristics of Participants by Change in Housing Status: Health Resources and Services Administration Special Projects of National Significance “Building a Medical Home for Multiply Diagnosed HIV-Positive Homeless Populations” Initiative, in 9 US Sites, 2013–2017
| Baseline Characteristics | Total, No. (%) or Mean ±SD | Became or Remained Unstably Housed, No. (%) or Mean ±SD | Maintained or Improved Housing Stability, No. (%) or Mean ±SD | P |
| Total | 283 (40.4) | 417 (59.6) | ||
| Gender | .14 | |||
| Male | 516 (73.7) | 212 (74) | 304 (72.9) | |
| Female | 150 (21.4) | 53 (18.7) | 97 (23.3) | |
| Transgender or other | 34 (4.9) | 18 (6.4) | 16 (3.8) | |
| Race/ethnicity | .30 | |||
| African American/Black | 327 (46.9) | 127 (45.2) | 200 (48.1) | |
| Hispanic | 144 (20.7) | 58 (20.6) | 86 (20.7) | |
| White | 177 (25.4) | 70 (24.9) | 107 (25.7) | |
| Other (including multiracial) | 49 (7.0) | 26 (9.3) | 23 (5.5) | |
| Age, y | 43.5 ±10.5 | 43.7 ±10.1 | 43.4 ±10.9 | .68 |
| ≤ 30 | 110 (15.7) | 36 (12.7) | 74 (17.7) | .11 |
| 31–54 | 492 (70.3) | 211 (74.6) | 281 (67.4) | |
| ≥ 55 | 98 (14.0) | 36 (12.7) | 62 (14.9) | |
| Education | .19 | |||
| < high school | 225 (32.2) | 101 (35.9) | 124 (29.7) | |
| High school | 229 (32.8) | 84 (29.9) | 145 (34.8) | |
| > high school | 244 (35.0) | 96 (34.2) | 148 (35.5) | |
| Housing status | < .001 | |||
| Unstable | 579 (82.7) | 262 (92.6) | 317 (76.0) | |
| Temporary | 121 (17.3) | 21 (7.4) | 100 (24.0) | |
| Number of years homeless | 6.28 ±8.16 | 7.59 ±8.80 | 5.39 ±7.58 | .005 |
| Recent incarceration (past 12 mo) | 231 (33.3) | 108 (38.2) | 123 (29.5) | .02 |
| Trauma history, lifetime | ||||
| Physical injury, harm | 304 (43.5) | 135 (47.7) | 169 (40.6) | .06 |
| Sexually assaulted | 281 (40.3) | 103 (36.4) | 178 (43.0) | .08 |
| Social support score | 11.3 ±5.2 | 10.7 ±5.0 | 11.7 ±5.3 | .01 |
| Self-efficacy score | ||||
| Getting information | 8.7 ±2.3 | 8.5 ±2.4 | 8.8 ±2.2 | .08 |
| Obtaining help | 5.7 ±2.4 | 5.5 ±2.5 | 5.9 ±2.4 | .07 |
| Communicating with physician | 8.7 ±2.0 | 8.5 ±2.3 | 8.9 ±1.8 | .02 |
| No health insurance | 256 (36.7) | 95 (33.6) | 161 (38.6) | .19 |
| Food insecurity | 406 (58.4) | 189 (67.3) | 217 (52.4) | < .001 |
| Number of unmet needs | 3.5 ±2.3 | 3.9 ±2.3 | 3.2 ±2.2 | < .001 |
| Number of barriers to care | 3.3 ±3.2 | 3.9 ±3.4 | 2.9 ±3.0 | < .001 |
| Moderate to high risk for substance use | ||||
| Alcohol | 288 (41.1) | 124 (43.8) | 164 (39.3) | .23 |
| Cocaine | 351 (50.1) | 158 (55.8) | 193 (46.3) | .01 |
| Opioids | 144 (20.6) | 73 (25.8) | 71 (17.0) | .005 |
| Amphetamines | 237 (33.9) | 120 (42.4) | 117 (28.1) | < .001 |
| Moderate to severe depressive symptoms (CES-D ≥ 10) | 522 (74.7) | 214 (75.6) | 308 (74.0) | .63 |
| Time living with HIV, y | 11.0 ±8.8 | 11.2 ±8.9 | 10.9 ±8.8 | .68 |
| Health-related quality of life | ||||
| Physical composite score | 37.8 ±12.3 | 36.8 ±12.5 | 38.5 ±12.1 | .07 |
| Mental composite score | 34.9 ±12.9 | 34.3 ±3.2 | 35.3 ±12.8 | .31 |
| Virally suppressed (HIV-1 RNA < 200 copies/mL) | 309 (49.9) | 106 (42.6) | 203 (54.9) | .002 |
Note. CES-D = Center for Epidemiological Studies–Depression Scale.
Changes in Housing Status
Table 1 describes the changes in housing status and predictors over time. Approximately two thirds (59.6%) were able to transition from unstable housing to more stable housing through either temporary or permanent supportive housing in the postintervention period. Baseline factors significantly associated with becoming stably housed included lower levels of illicit substance use, higher rates of viral suppression, fewer years of experiencing homelessness, lower rates of recent incarceration, fewer unmet needs and barriers to care, greater self-efficacy, and higher social support.
HIV Health Outcomes and Changes in Housing Status
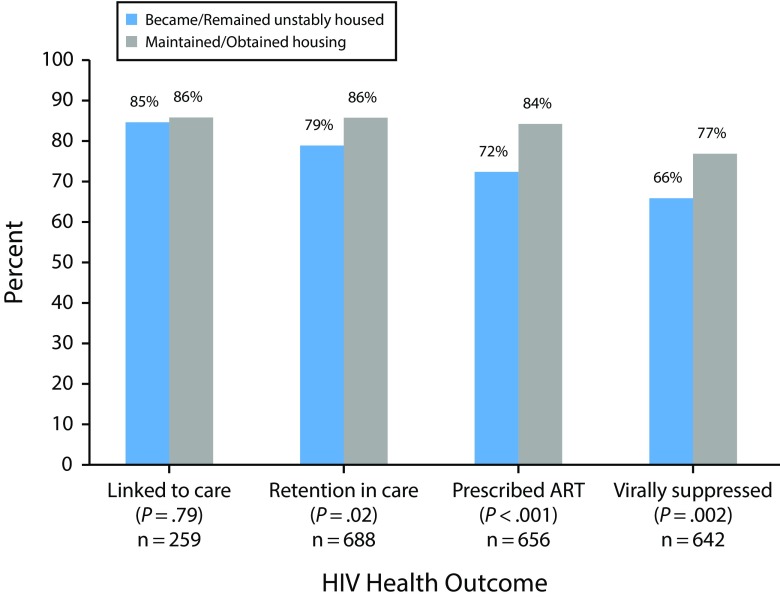
Overall, 85.3% (n = 259) of participants who were newly diagnosed or out of care were linked to care and, among all participants, 82.9% (n = 688) were retained in care, 79.4% (n = 656) were prescribed antiretroviral therapy, and 72.6% (n = 642) reached viral suppression. Figure 1 describes the HIV care continuum by change in housing status. Participants who stabilized their housing were significantly more likely to be retained in care (86% vs 79%; P = .02), more likely to be prescribed antiretroviral therapy (84% vs 72%; P < .001), and had higher rates of viral suppression (77% vs 66%; P = .002).
FIGURE 1—
Change in Housing Status by HIV Health Outcomes: Health Resources and Services Administration Special Projects of National Significance “Building a Medical Home for Multiply Diagnosed HIV-Positive Homeless Populations” Initiative, in 9 US Sites, 2013–2017
Note. ART = antiretroviral therapy.
In multivariate analysis, participants who achieved stabilized housing were twice as likely to be retained in care (n = 596; adjusted odds ratio [AOR] = 2.12; 95% confidence interval [CI] = 1.11, 4.05), prescribed antiretroviral therapy (n = 570; AOR = 2.06; 95% CI = 1.62, 2.63), and to reach viral suppression (n = 559; AOR = 1.62; 95% CI = 1.03, 2.55) compared with those who became or remained unstably housed after adjusting for other covariates. There were no statistically significant findings between changes in housing stability and being linked to care (n = 208; AOR = 1.81; 95% CI = 0.87, 3.04).
DISCUSSION
This study suggests that patient navigation models are a promising strategy to stabilize housing and improve health outcomes for PLWH who are unstably housed with co-occurring mental health and substance use disorders. Two thirds of program participants were able to transition to more stable housing and more than two thirds reached viral suppression. Our rates were comparable or exceeded current national rates for viral suppression of 80.0% for PLWH in care and 57.9% among all PLWH.27
This study contributes to and provides additional evidence supporting the role of patient navigation interventions for PLWH who are unstably housed.28,29 Buchanan et al. found PLWH who received intensive case management and permanent supportive housing upon hospital discharge had improved survival and improved viral suppression rates.28 Recent studies of released prisoners with HIV have similarly found that patient navigation services with transitional case management have successfully been associated with linkage to and retention in care, including higher levels of viral suppression.30,31 Other studies also found positive associations with case management and adherence to treatment and improvements in CD4 cell counts for PLWH experiencing homelessness.29 To our knowledge, this study is one of the largest studies of a community-based sample of persons experiencing homelessness and the first to show a positive effect of these interventions on retention in care and viral suppression for this vulnerable population.
We found that, even among those who remained unstably housed, 66% were able to achieve viral suppression. Homelessness is ascribed as a barrier for health care providers in their decision to prescribe antiretroviral therapy32; however, this emerging evidence questions guidelines to defer antiretroviral therapy initiation until a person’s housing circumstances are improved.33 The HRSA mobile care and navigation interventions were able to bring necessary medical care and psychosocial services to those clients to reduce barriers and enhance access to care and treatment regardless of housing status. This study also highlights the need to broaden the HIV care continuum definition of being “in care” to include “bringing care” outside of a brick-and-mortar clinic when working with this population. The results show that navigation services could help to close the gap in health outcomes between stably housed versus unstably housed PLWH.
Limitations
There are limitations to our study. First, although the 9 study sites represented diverse geographic regions, this was a prospective study of a convenience sample of PLWH who were unstably housed. The lack of control or comparison groups does not allow us to assess a direct causal relationship between the HRSA interventions, changes in housing status, and HIV health outcomes. In developing our analysis, we adjusted for baseline characteristics and site only and did not include time-dependent variables. Some variables could be potential mediators with changes in housing status (i.e., changes in self-efficacy).
Second, our analysis was limited to participants who had both chart and survey data, and we recognize that persons who were lost to follow-up may be less likely to return to HIV care and may have poorer health outcomes.
Third, our measure of housing status was self-reported based on types of places stayed in the previous 6 or 12 months between interviews. We were not able to verify the information with housing systems’ data. We may be underreporting the rates of unstable housing in the population. Frequently, patient navigators were helping clients with various housing activities so there was validation for clients’ housing self-reports at most sites. We were not able to assess other housing factors that are important to consider, including perceptions of safety and housing quality.
Finally, we did not assess for differences in the environmental context, (i.e., housing affordability and availability or rent or income burden) at each site and impact on client outcomes. We accounted for site clustering in our propensity score analysis and in our final models. However, future studies should examine other environmental factors to gain a better understanding of their impact on health outcomes.
Public Health Implications
To achieve improved housing and health outcomes for their clients, the HRSA navigation models prioritized system-wide coordination in addition to intensive individual navigation and care coordination. System collaboration included and extended beyond HIV care providers to reach other local stakeholders, such as hospitals and emergency departments, corrections, health departments, other social services, landlords, and property managers. Methods to enhance system-level coordination included (1) the use of standardized tools for communication, referral systems, and client assessments; (2) regular meetings between health care and housing providers; and (3) emergency housing support. Although we were unable to assess the direct impact of these system changes on study participants’ HIV health outcomes, these partnerships likely were contributing factors to our results. Future research studies should attempt to measure and evaluate the effect of system coordination on HIV health outcomes.
For many clients, the lack of housing opportunities is only 1 barrier associated with better HIV health outcomes. Homelessness affects a client’s capacity to access many different types of service providers. We found that adaptations to traditional HIV health care and social service delivery models are necessary. Mobile teams and dedicated staff members—such as peer navigators, care coordinators, community health workers, and medical providers, moved beyond clinic walls and were able to engage and retain clients who are unstably housed. These mobile staff are critical members of the HIV workforce for improving HIV health outcomes for vulnerable populations.34,35
Even when clients are linked to care and a pathway to housing is offered, we found that a fair proportion (40%) of our sample was unable to access or maintain housing. Reasons included structural factors, such as affordability and availability in the local markets. Personal choice is another factor as some participants reported feeling unsafe in shelters or residential facilities. In some instances, social, mental health, and substance use issues make housing and health care a lower-priority need. Persons living with HIV who live in community settings may find it hard to leave the social support they have found on the street. It is important for administrators and staff to recognize these scenarios and to create individualized treatment plans that meet the clients’ self-defined needs. The HRSA Homeless Initiative offers a framework in which PLWH can get their psychosocial and medical needs met. Although some clients may remain unstably housed, people were still motivated to care for their health. The patient navigator as part of the medical home team supported this motivation by assisting with retention in behavioral health and medical care and adhering to treatment necessary to become or remain virally suppressed.
Providing housing does not immediately change a client’s ability to retain housing and reach viral suppression. Previous studies have shown that this transition time to and from homelessness is critical and associated with severity of drug use and mental illness, which affect HIV health outcomes.36 During this transition, patient navigators can provide emotional, harm-reduction, and life-skills support to the newly housed client. Our study shows that 12 months of intensive support may be sufficient for some PLWH to reach a measure of housing independence and reentry into traditional clinic care, yet a fair proportion need longer support. Even after obtaining permanent housing, a client may need regular check-ins from a patient navigator or similar care team member to continue to access and use medical care and adhere to treatment. Future studies should examine the pathways and mechanisms, including the role of patient navigation services that motivate a person to seek and maintain housing and adhere to treatment.
Conclusions
Our findings indicate that participants were able to improve their housing status and achieve positive outcomes along the HIV continuum of care. By using team-based approaches that included patient navigators and collaborating with housing, HIV primary medical, and behavioral health providers, these programs were able to break down barriers to care. Addressing the unmet need for housing services led to better continuity of care. However, even when PLWHs did not change their housing status, they can achieve viral suppression if given the appropriate level of care navigation and support. These findings suggest that the reorganization of health systems to provide mobile and responsive care can improve housing and health outcomes for PLWH who are at risk for homelessness or housing instability.
ACKNOWLEDGMENTS
This project is supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) under grant U90HA24974, Special Projects of National Significance Initiative “Building a Medical Home for Multiply Diagnosed HIV-Positive Homeless Populations.” No percentage of this project was financed with nongovernmental sources.
The authors of this article thank the staff and clients at our fellow HRSA demonstration sites. We also thank Emily Sisson for her assistance with data analysis, Carole Hohl and Jo Ann Whitlock Davich for review of the article, and Marena Sullivan for assistance with article preparation and submission.
Note. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the US government.
HUMAN PARTICIPANT PROTECTION
All participants were properly instructed and indicated that they consented to participate by signing informed consent paperwork. The research and findings presented in this article were approved by the institutional review board at Boston University Medical Campus and the institutional review boards for the participating 9 study sites.
REFERENCES
- 1.Department of Health and Human Services, Office of HIV/AIDS and Infectious Disease Policy. National HIV/AIDS Strategy for the United States updated to 2020: 2017 progress report. Available at: https://www.aids.gov/federal-resources/national-hiv-aids-strategy/overview. Accessed May 25, 2018.
- 2.Aidala AA, Wilson MG, Shubert V et al. Housing status, medical care, and health outcomes among people living with HIV/AIDS: a systematic review. Am J Public Health. 2016;106(1):e1–e23. doi: 10.2105/AJPH.2015.302905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lim S, Nash D, Hollod L et al. Influence of jail incarceration and homelessness patterns on engagement in HIV care and HIV viral suppression among New York City adults living with HIV/AIDS. PLoS One. 2015;10(11):e0141912. doi: 10.1371/journal.pone.0141912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Milloy MJ, Marshall BD, Montaner J et al. Housing status and the health of people living with HIV/AIDS. Curr HIV/AIDS Rep. 2012;9(4):364–374. doi: 10.1007/s11904-012-0137-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Milloy MJ, Kerr T, Bangsberg DR et al. Homelessness as a structural barrier to effective antiretroviral therapy among HIV-seropositive illicit drug users in a Canadian setting. AIDS Patient Care STDS. 2012;26(1):60–67. doi: 10.1089/apc.2011.0169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwarcz SK, Hsu LC, Vittinghoff E et al. Impact of housing on the survival of persons with AIDS. BMC Public Health. 2009;9(1):220. doi: 10.1186/1471-2458-9-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007;11(6 suppl):85–100. doi: 10.1007/s10461-007-9246-3. [DOI] [PubMed] [Google Scholar]
- 8.Kidder DP, Wolitski RJ, Campsmith ML et al. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007;97(12):2238–2245. doi: 10.2105/AJPH.2006.090209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maulsby C, Enobun B, Batey DS et al. A mixed-methods exploration of the needs of people living with HIV (PLWH) enrolled in access to care, a national HIV linkage, retention and re-engagement in medical care program. AIDS Behav. 2018;22(3):819–828. doi: 10.1007/s10461-017-1809-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. HIV/AIDS Bureau Special Projects of National Significance Program. Funding opportunity announcement. Building a Medical Home for HIV-Positive Multiply Diagnosed Homeless Populations Initiative – Evaluation and Technical Assistance Center. (CFDA) No. 93.928. Rockville, MD: US Department of Health Resources and Services Administration; 2012.
- 11.Doshi RK, Milberg J, Jumento T et al. For many served by the Ryan White HIV/AIDS Program, disparities in viral suppression decreased, 2010–14. Health Aff (Millwood) 2017;36(1):116–123. doi: 10.1377/hlthaff.2016.0655. [DOI] [PubMed] [Google Scholar]
- 12.Pappas G, Yujiang J, Seiler N et al. Perspectives on the role of patient-centered medical homes in HIV care. Am J Public Health. 2014;104(7):e49–e53. doi: 10.2105/AJPH.2014.302022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Myers JJ, Kang Dufour MS, Koester KA et al. The effect of patient navigation on the likelihood of engagement in clinical care for HIV-infected individuals leaving jail. Am J Public Health. 2018;108(3):385–392. doi: 10.2105/AJPH.2017.304250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cunningham WE, Weiss RE, Nakazono T et al. Effectiveness of a peer navigation intervention to sustain viral suppression among HIV-positive men and transgender women released from jail: the LINK LA randomized clinical trial. JAMA Intern Med. 2018;178(4):542–553. doi: 10.1001/jamainternmed.2018.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giordano TP, Cully J, Amico KR et al. A randomized trial to test a peer mentor intervention to improve outcomes in persons hospitalized with HIV infection. Clin Infect Dis. 2016;63(5):678–686. doi: 10.1093/cid/ciw322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Metsch LR, Feaster DJ, Gooden L et al. Effect of patient navigation with or without financial incentives on viral suppression among hospitalized patients with HIV infection and substance use: a randomized clinical trial. JAMA. 2016;316(2):156–170. doi: 10.1001/jama.2016.8914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarango M, de Groot A, Hirschi M et al. The role of patient navigators in building a medical home for multiply diagnosed HIV-positive homeless populations. J Public Health Manag Pract. 2017;23(3):276–282. doi: 10.1097/PHH.0000000000000512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Homeless Emergency Assistance and Rapid Transition to Housing: Defining “homeless.” Department of Housing and Urban Development, Office of the Assistant Secretary for Community Planning and Development, 24 CFR Parts 91, 582, and 583 (2011).
- 19.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 20.Health Resources and Services Administration. 2017 Annual Ryan White HIV/AIDS Program Services Report (RSR) instruction manual. Available at: https://targethiv.org/sites/default/files/file-upload/resources/2017_RSR_Manual_Final_HAB_Approved_508.pdf. Accessed November 5, 2018.
- 21. Alcohol, Smoking and Substance Involvement Screening Test. Version 3.1. Geneva, Switzerland: World Health Organization; 2010.
- 22.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 23.National Institute for Drug Abuse. Seek, Test, Treat and Retain for vulnerable populations: data harmonization measure social support subscale. Available at: http://www.drugabuse.gov/sites/default/files/sttrfiles/AccesstoCareVP.pdf. Accessed October 1, 2012.
- 24.Lorig K, Stewart A, Ritter P Outcome measures for health education and other health care interventions. Thousand Oaks, CA: Sage Publications; 1996: 24–25, 41–45.
- 25.Kalichman SC, Catz S, Ramachandran B. Barriers to HIV/AIDS treatment and adherence among African‐American adults with disadvantaged education. J Natl Med Assoc. 1999;91(8):439–446. [PMC free article] [PubMed] [Google Scholar]
- 26.Fay MP, Graubard BI. Small‐sample adjustments for Wald‐type tests using sandwich estimators. Biometrics. 2001;57(4):1198–1206. doi: 10.1111/j.0006-341x.2001.01198.x. [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2015. HIV Surveillance Supplemental Report. 2017;22(2) Available at: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed November 30, 2017. [Google Scholar]
- 28.Buchanan D, Kee R, Sadowski LS et al. The health impact of supportive housing for HIV-positive homeless patients: a randomized controlled trial. Am J Public Health. 2009;99(suppl 3):S675–S680. doi: 10.2105/AJPH.2008.137810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kushel MB, Colfax G, Ragland K et al. Case management is associated with improved antiretroviral adherence and CD4+ cell counts in homeless and marginally housed individuals with HIV infection. Clin Infect Dis. 2006;43(2):234–242. doi: 10.1086/505212. [DOI] [PubMed] [Google Scholar]
- 30.Loeliger KB, Meyer JP, Desai MM, Ciarleglio MM, Gallagher C, Altice FL. Retention in HIV care during the 3 years following release from incarceration: a cohort study. PLoS Med. 2018;15(10):e1002667. doi: 10.1371/journal.pmed.1002667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Loeliger KB, Altice FL, Desai MM, Ciarleglio MM, Gallagher C, Meyer JP. Predictors of linkage to HIV care and viral suppression after release from jails and prisons: a retrospective cohort study. Lancet HIV. 2018;5(2):e96–e106. doi: 10.1016/S2352-3018(17)30209-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weiser J, Brooks JT, Skarbinski J et al. Barriers to universal prescribing of antiretroviral therapy by HIV care providers in the United States 2013–2014. J Acquir Immune Defic Syndr. 2017;74(5):479–487. doi: 10.1097/QAI.0000000000001276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harris RA, Xue X, Selwyn PA. Housing stability and medication adherence among HIV-positive individuals in antiretroviral therapy: a meta-analysis of observational studies in the United States. J Acquir Immune Defic Syndr. 2017;74(3):309–317. doi: 10.1097/QAI.0000000000001213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bradford JB, Coleman S, Cunningham W. HIV system navigation: an emerging model to improve HIV care access. AIDS Patient Care STDS. 2007;21(suppl 1):S49–S58. doi: 10.1089/apc.2007.9987. [DOI] [PubMed] [Google Scholar]
- 35.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57(8):1164–1171. doi: 10.1093/cid/cit420. [DOI] [PubMed] [Google Scholar]
- 36.Zelenev A, Marcus RM, Kopelev A et al. Patterns of homelessness and implications for HIV health after release from jail. AIDS Behav. 2013;17(suppl 2):S181–S194. doi: 10.1007/s10461-013-0472-6. [DOI] [PMC free article] [PubMed] [Google Scholar]