Dear Editor,
A 34-year-old previously healthy man presented with a complaint of sudden-onset, progressive low back pain radiating to the lower limbs after running. The symptoms had begun three weeks earlier, with acute worsening during the last four days. The physical examination was normal except for mild lower left limb edema. A lumbosacral magnetic resonance imaging scan showed dilated vessels in the epidural space, intervertebral foramen, and anterior paraspinal space (Figure 1). Complementary abdominal computed tomography angiography of the abdomen showed thrombosis of the inferior vena cava (IVC), common iliac veins, left external iliac vein, and right accessory renal vein (Figure 2). The patient was submitted to mechanical thrombectomy, followed by chemical thrombolysis and long-term anticoagulation therapy, with resolution of symptoms. A control computed tomography scan, obtained six months later, showed patency of the IVC and common iliac veins, together with chronic thrombosis of left internal iliac vein. Further investigations for acquired thrombophilia were negative.
Figure 1.
Magnetic resonance imaging, including a sagittal T1-weighted image (A), a sagittal T2-weighted image (B) and an axial T2-weighted image (C), showing enlargement of the epidural veins with compression of lumbar roots (arrows).
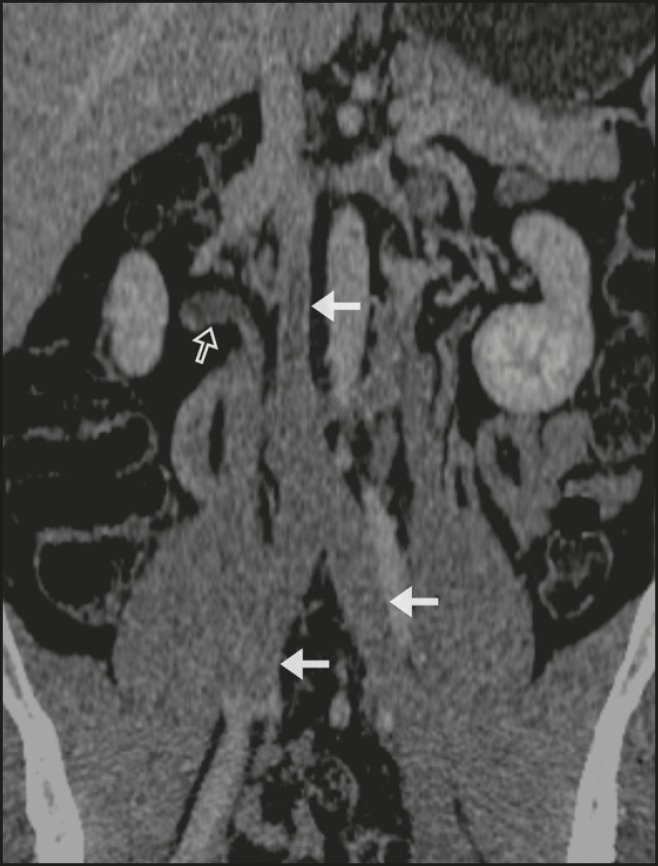
Figure 2.
Abdominal coronal reformatted computed tomography scan showing extensive thrombosis of the IVC, common iliac veins (arrows), left external iliac vein, and right accessory renal vein (open arrow).
Engorgement of the epidural venous plexus secondary to IVC thrombosis is a rare cause of lower back pain by compression of nerve roots, and it is a differential diagnosis to disc-degenerative changes(1,2). Paksoy et al.(3) identified IVC obstruction as a cause of radiculopathy in 0.13% patients who underwent magnetic resonance imaging for the investigation of radicular symptoms mimicking lumbar disc herniation or spinal stenosis; in all of those patients, it was the first episode (of low back pain).
The vertebral venous system consists of the internal vertebral veins or epidural veins (internal network) and the lumbar segmental veins or paravertebral veins (external network), which communicate with the common iliac veins, azygous system, and IVC, through the lumbar segmental veins(1,3). Although it normally presents flow that is ascendant and away from the spinal flow, it can present retrograde flow because of its valveless nature, becoming an alternative pathway between the iliac-caval and azygous systems(3). The internal and external networks communicate through the radicular veins, which have an intimate relationship with the nerve roots and, when engorged, may mimic radicular compression(1-4). Possible causes of engorgement of the epidural veins of the back include vascular malformations of the epidural venous plexus; IVC thrombosis, related to pregnancy or not(5-8); portal hypertension(2); spinal dysraphism(3); epidural lipomatosis(3); Budd-Chiari syndrome(4,9); and intracranial hypotension(2).
Engorgement of epidural vessels should immediately raise the suspicion of cava thrombosis, and the radiologist plays an important role in correlating it with the possible underlying etiologies. Due to its severity, deep venous thrombosis, as seen in this case, must be promptly diagnosed and treated.
REFERENCES
- 1.Hanley Jr EN, Howard BH, Brigham CD, et al. Lumbar epidural varix as a cause of radiculopathy. Spine (Phila Pa 1976) 1994;19:2122–2126. doi: 10.1097/00007632-199409150-00022. [DOI] [PubMed] [Google Scholar]
- 2.Dudeck O, Zeile M, Poellinger A, et al. Epidural venous enlargements presenting with intractable lower back pain and sciatica in a patient with absence of the infrarenal inferior vena cava and bilateral deep venous thrombosis. Spine (Phila Pa 1976) 2007;32:E688–E691. doi: 10.1097/BRS.0b013e318158cf94. [DOI] [PubMed] [Google Scholar]
- 3.Paksoy Y, Gormus N. Epidural venous plexus enlargements presenting with radiculopathy and back pain in patients with inferior vena cava obstruction or occlusion. Spine (Phila Pa 1976) 2004;29:2419–2424. doi: 10.1097/01.brs.0000144354.36449.2f. [DOI] [PubMed] [Google Scholar]
- 4.Bozkurt G, Çil B, Akbay A, et al. Intractable radicular and low back pain secondary inferior vena cava stenosis associated with Budd-Chiari syndrome: endovascular treatment with cava stenting: case report and review of the literature. Spine (Phila Pa 1976) 2006;31:E383–E386. doi: 10.1097/01.brs.0000219516.54500.97. [DOI] [PubMed] [Google Scholar]
- 5.Hirabayashi Y, Shimizu R, Fukuda H, et al. Effects of the pregnant uterus on the extradural venous plexus in the supine and lateral positions, as determined by magnetic resonance imaging. Br J Anaesth. 1997;78:317–319. doi: 10.1093/bja/78.3.317. [DOI] [PubMed] [Google Scholar]
- 6.Gormus N, Ustun ME, Paksoy Y, et al. Acute thrombosis of inferior vena cava in a pregnant woman presenting with sciatica: a case report. Ann Vasc Surg. 2005;19:120–122. doi: 10.1007/s10016-004-0142-2. [DOI] [PubMed] [Google Scholar]
- 7.Hickey BA, Ahuja S. Acute lumbar radiculopathy with weak legs. J Emerg Med. 2014;46:479–481. doi: 10.1016/j.jemermed.2013.09.039. [DOI] [PubMed] [Google Scholar]
- 8.Resorlu H, Koral L, Aylanc N, et al. Thrombosis of the inferior vena cava presenting with findings of radiculopathy. Spine J. 2016;16:e501–e502. doi: 10.1016/j.spinee.2016.01.023. [DOI] [PubMed] [Google Scholar]
- 9.Lee JH, Song WJ, Kang KC. Myelopathy-mimicking symptoms of epidural venous engorgement and syringomyelia due to inferior vena cava stenosis at the thoracolumbar junction in a patient with Budd-Chiari syndrome. J Neurosurg Spine. 2015;23:467–470. doi: 10.3171/2015.1.SPINE14515. [DOI] [PubMed] [Google Scholar]