ABSTRACT
The aim of this study was to develop and test models for non–uptake of three doses of diphtheria-tetanus-pertussis containing vaccines (DTP3) among children of women living with HIV in sub-Saharan Africa. The study used demographic and health survey data from 27 sub-Saharan African countries that have the required HIV and immunization data sets. Multivariable logistic regression models were used to assess the relationship between individual and contextual factors associated with non-uptake of DTP3 among the children. At the individual level, the odds of non-uptake of DTP3 decreased with formal education, increasing age and access to media. The full model shows that the odds of non-uptake of DTP3 is increased among unemployed women, those living in communities with high illiteracy rate and in countries with low adult literacy level. For a child who moved to another country or community with a higher probability of DTP3 non-uptake, the median increase for the odds of DTP3 non-uptake would be 2.24% and 1.22% respectively for country and community. This study shows that individual and contextual factors contributed significantly to non-uptake of DTP3 among the children of women living with HIV. Interventions should be focused on women living with HIV who are young mothers, unemployed women, those without formal education, individuals living in communities with high illiteracy rate and in countries with low adult literacy rate. The use of mass media tools and creation of more employment opportunities for HIV-infected women could improve vaccination coverage among their children.
Keywords: diphtheria-tetanus-pertussis, HIV, vaccine-preventable diseases, sub-Saharan Africa, demographic health survey
Introduction
Research studies have shown that routine vaccination coverage is inadequate in several African countries and unable to meet national targets for Global Vaccine Action Plan (GVAP).1–3 Sub-Saharan Africa with high HIV prevalence needs adequate vaccination coverage especially among the HIV-infected and HIV-exposed children because they are highly susceptible to severe forms of some vaccine-preventable diseases with resultant increased risk of mortality.4,5 The children of HIV-infected mothers are at risk of mortality than the non-exposed children because HIV-positive mothers may not take their children for vaccination as scheduled due to generalized weakness and non-availability of transport fees to get to the healthcare facilities.6,7 Vaccination of both HIV-infected and uninfected children also played critical role towards achieving the Millennium Development Goal 4 targeted in reducing deaths in children less than five years of age.8 Attaining Sustainable Development Goal 3.8 is also connected to vaccination strategies especially with the achievement of Universal Health Coverage via vaccines for all age groups.9
Studies showed that children born to HIV-infected mothers were less likely to get all the basic vaccination according to schedule through the avoidance of the health facilities in community owing to stigma and discrimination.6,7,10 The association between maternal HIV status and childhood vaccination is of public health significance in countries with high HIV prevalence. However, there are uncertainty and limited information on factors that influence the association between maternal HIV status and childhood vaccination coverage in sub-Saharan Africa.10
It has been established that there is an association between maternal education and vaccine uptake, however, this varies across different regions and settings across the world.11 Studies show that the odds of childhood vaccination are greater in children whose mothers have secondary or higher education.11,12 Poor socioeconomic status and non-empowerment of women are important factors that are related to poor uptake of childhood vaccination.12 Immunization coverage is low in urban poor and deprived neighbourhood. These neighbourhoods also have the hallmark of poor mother and child healthcare services, maternal illiteracy, poor household socioeconomic status and gender inequality.13
The per capita gross domestic product (GDP) is a factor in the usage of vaccines in the low income countries that has high mortality rates due to vaccine-preventable diseases. It is expected that good vaccine uptake in these countries will be cost-effective on the long run and this depends largely on the cost of vaccination programme with respect to GDP.14 Vaccination plays an important role in economic growth. It has an impact on country’s healthcare with resultant reduction in mortality and morbidity, thereby contributing to the GDP.15
Initiatives such as the Global Alliance for Vaccines and Immunization (GAVI), WHO-UNICEF Global Immunization Vision and Strategy, the Global Vaccine Action Plan (GVAP), and others have contributed towards achieving universal access to immunization.3 However, there is dearth of information concerning interventions or programmes specifically targeted at improving vaccination coverage for HIV-infected and HIV-exposed uninfected children in Africa. Vaccination programmes tend to target all children irrespective of their HIV status or that of their mothers, although HIV-infected and HIV-exposed uninfected children are more prone to vaccine-preventable diseases.16
A multilevel study is specifically needed to evaluate the independent contributions of individual, community, and country-level factors to non-vaccination among the children of HIV-infected women in sub-Saharan African countries. We therefore initiated this study to develop and test models for non-uptake of vaccines among the children of HIV-infected mothers. Receipt of three doses of diphtheria-tetanus-pertussis containing vaccines (DTP3) is a widely-accepted surrogate measure of full childhood immunization coverage.17 The DTP-containing vaccine used in sub-Saharan Africa is a pentavalent vaccine that provides immunity against diphtheria, tetanus, pertussis, hepatitis B, and Haemophilus influenzae type b. These five infectious diseases lead to significant morbidity and mortality in children especially in countries with poor vaccination coverage.
Results
Sample characteristics
Table 1 shows the summary of individual, community, and country characteristics and DTP3 coverage among the children of HIV-positive mothers. A total of 5,537 children aged 12–23 months, within 2841 communities and from 27 countries in sub-Saharan Africa were involved in this study. About one-fourth of the children of HIV-infected mothers did not receive DTP3 prior to the survey. The numbers of male and female children were fairly evenly distributed.. Table 1 shows that there was an association between DTP3 uptake and variables such as age, level of education, employment status, access to media, wealth index and illiteracy rate. The table also shows that DTP3 vaccination is not significantly associated with years of survey. Country-level characteristics were shown in Table 2. The surveys were conducted between 2003 and 2016 in the included countries with the years 2013 and 2014 having five surveys each.
Table 1.
Summary of characteristics at different levels and DTP3 uptake among children of HIV-positive mothers.
| DTP3 uptake |
|||||
|---|---|---|---|---|---|
| Variables | Sample size | Percentage | No* | Yes* | p-value |
| DTP3 non-uptake | 1,350 | 24.4 | |||
| DTP3 uptake | 4,187 | 75.6 | |||
| Years of survey | |||||
| 2003–2010 | 1,230 | 22.2 | 275 (20.4) | 955 (22.8) | 0.061 |
| 2010–2011 | 4,307 | 77.8 | 1,075 (79.6) | 3,232 (77.2) | |
| Individual-level factors | |||||
| Gender | |||||
| Female | 2,734 | 49.4 | 673 (49.8) | 2,061 (49.2) | 0.688 |
| Male | 2,803 | 50.6 | 677 (50.2) | 2,126 (50.8) | |
| Age (in years) | |||||
| 15–24 | 1,352 | 24.4 | 355 (26.3) | 997 (23.8) | 0.003 |
| 25–34 | 2,828 | 51.1 | 710 (52.6) | 2,118 (50.6) | |
| 35–49 | 1,357 | 24.5 | 285 (21.1) | 1,072 (24.5) | |
| Education | |||||
| No education | 855 | 15.4 | 315 (23.3) | 540 (12.9) | 0.000 |
| Primary | 2,363 | 42.7 | 541 (40.1) | 1,822 (43.5) | |
| Secondary+ | 2,319 | 41.9 | 494 (36.6) | 1,825 (43.6) | |
| Employment status | |||||
| Unemployed | 2,093 | 37.8 | 552 (40.9) | 1,541 (36.8) | 0.007 |
| Employed | 3,444 | 62.2 | 798 (59.1) | 2,646 (63.2) | |
| Wealth index | |||||
| Poorer | 1,514 | 27.3 | 397 (29.4) | 1,117 (26.7) | 0.000 |
| Middle | 1,694 | 30.6 | 447 (33.1) | 1,247 (29.8) | |
| Richer | 2,329 | 42.1 | 492 (37.5) | 1,823 (43.5) | |
| Access to media | |||||
| Nil | 1,302 | 23.5 | 398 (29.5) | 904 (21.6) | 0.000 |
| Access to 1 outlet | 1,697 | 30.7 | 418 (31.0) | 1,279 (30.6) | |
| Access to 2 outlets | 1,578 | 28.5 | 347 (25.7) | 1,231 (29.4) | |
| Access to all outlets | 960 | 17.3 | 187 (13.9) | 773 (18.5) | |
| Community-level factors | |||||
| Place of residence | |||||
| Urban | 2,477 | 44.7 | 603 (44.7) | 1,874 (44.8) | 0.953 |
| Rural | 3,060 | 55.3 | 747 (55.3) | 2,313 (55.2) | |
| Poverty rate | |||||
| Low | 3,421 | 61.8 | 805 (59.6) | 2,616 (62.5) | 0.061 |
| High | 2,116 | 38.2 | 545 (40.4) | 1,571 (37.5) | |
| Unemployment rate | |||||
| Low | 2,816 | 50.9 | 675 (50.0) | 2,141 (51.1) | 0.468 |
| High | 2,721 | 49.1 | 675 (50.0) | 2,046 (48.9) | |
| Illiteracy rate | |||||
| Low | 3,609 | 65.2 | 804 (59.6) | 2,805 (67.0) | 0.000 |
| High | 1,928 | 34.8 | 546 (40.4) | 1,382 (33.0) | |
* The values for DTP3 uptake are absolute counts (percentage).
Table 2.
The country-level characteristics of the 27 included countries.
| Country | Year of survey | GDP per capita (US$) | Adult literacy rate | Health expenditure per capita (US $) |
|---|---|---|---|---|
| Angola | 2016 | 3110.8 | 66.0 | 179.4 |
| Burkina Faso | 2010 | 649.7 | 34.6 | 35.2 |
| Burundi | 2011 | 285.7 | 61.6 | 21.6 |
| Cameroon | 2011 | 1032.6 | 71.3 | 58.7 |
| Chad | 2015 | 664.3 | 22.3 | 37.1 |
| Congo DR | 2014 | 444.5 | 77.0 | 19.1 |
| Cote d’Ivoire | 2012 | 1526.2 | 43.9 | 88.4 |
| Ethiopia | 2003 | 706.8 | 39.0 | 26.6 |
| Gabon | 2012 | 7179.3 | 82.3 | 321.3 |
| Gambia | 2013 | 473.2 | 42.0 | 30.7 |
| Ghana | 2014 | 1513.5 | 71.5 | 57.9 |
| Guinea | 2012 | 508.1 | 32.0 | 37.3 |
| Kenya | 2009 | 1455.4 | 78.7 | 77.7 |
| Lesotho | 2014 | 998.1 | 76.6 | 105.1 |
| Liberia | 2013 | 455.4 | 42.9 | 46.3 |
| Malawi | 2016 | 300.8 | 62.1 | 29 |
| Mali | 2013 | 780.5 | 33.1 | 47.8 |
| Namibia | 2012 | 4140.5 | 88.3 | 499 |
| Niger | 2013 | 363.2 | 15.5 | 24.4 |
| Rwanda | 2015 | 702.8 | 68.3 | 52.5 |
| Sao T&P | 2009 | 1756.1 | 90.1 | 165.6 |
| Senegal | 2011 | 958.1 | 42.8 | 49.5 |
| Sierra Leone | 2013 | 496 | 32.4 | 85.9 |
| Swaziland | 2007 | 2775.2 | 83.1 | 247.9 |
| Togo | 2014 | 578.5 | 63.8 | 33.9 |
| Zambia | 2014 | 1178.4 | 83.0 | 85.9 |
| Zimbabwe | 2015 | 1008.6 | 88.7 | 57.7 |
Congo DR- Congo Democratic Republic, GDP: gross domestic product, Sao T&P: Sao Tome and Principe; US$: United States Dollars
GDP – Low-income economies are defined as those with a GDP per capita of $1,025 or less; lower middle-income economies: $1,026 – $4,035; upper middle-income economies: $4,036 – $12,475; Adult literacy rate – low: ≤ 50.0; high: ≥ 50.1; Health expenditure – low: ≤ 100.0; Average: ≥ 100.1.
(Source: World Bank, United Nations Development Programme)
Measures of associations (fixed effects)
Table 3 shows the results of different models. At the individual level, the odds of non-uptake of DTP3 decreased with formal education, increasing age and access to media. At community level, the odds of DTP3 non-uptake increased with being resident in communities with high illiteracy rate. The full model shows that the odds of the children of women living with HIV not receiving DTP3 vaccination increased with being unemployed, such that the children of unemployed women were 17% more likely not to take DTP3 (OR = 1.171, 95% CrI 1.012 to1.372). The odds of not completing the vaccination schedule decreased with older maternal age, such that children of women aged 35–49 years were 29% less likely to miss DTP3 compared to children of women aged 15–24 years old (OR = 0.711, 95% CrI 0.584 to 0.856). Other factors that decreased the odds of not completing the vaccination schedule were formal education and access to media (Table 3).
Table 3.
Factors associated with non-uptake of DTP3-containing vaccines by children of HIV-infected women identified by multilevel multivariate logistics regression models.
| Model 1a |
Model 2b |
Model 3c |
Model 4d |
Model 5e |
|
|---|---|---|---|---|---|
| OR (95% Crl) | OR (95% Crl) | OR (95% Crl) | OR (95% Crl) | OR (95% Crl) | |
| Fixed-effect | |||||
| Individual-effect factors | |||||
| Male (vs female) | 0.961 (0.844–1.095) | 0.959 (0.838–1.091) | |||
| Age (in completed years) | |||||
| 15–24 | 1 (reference) | 1 (reference) | |||
| 25–34 | 0.932 (0.793–1.089) | 0.937 (0.793–1.087) | |||
| 35–49 | 0.699 (0.574–0.844)* | 0.706 (0.575–0.849)* | |||
| Wealth index | |||||
| Poorer | 1 (reference) | 1 (reference) | |||
| Middle | 1.094 (0.907–1.307) | 1.055 (0.860–1.286) | |||
| Richer | 0.880 (0.718–1.076) | 0.830 (0.639–1.069) | |||
| Education | |||||
| No education | 1 (reference) | 1 (reference) | |||
| Primary | 0.700 (0.564–0.860)* | 0.768 (0.612–0.957)* | |||
| Secondary+ | 0.656 (0.519–0.831)* | 0.719 (0.566–0.927)* | |||
| Not employment | 1.149 (0.990–1.327) | 1.172 (1.001–1.365)* | |||
| Access to media | 0.899 (0.828–0.974)* | 0.893 (0.826–0.962)* | |||
| Community-level factors | |||||
| Rural (vs urban) | 1.085 (0.903–1.288) | 0.965 (0.795–1.182) | |||
| High (vs low) poverty rate | 0.999 (0.943–1.056) | 0.965 (0.899–1.032) | |||
| High (vs low) unemployment rate | 0.992 (0.950–1.041) | 0.980 (0.924–1.042) | |||
| High (vs low) illiteracy rate | 1.099 (1.050–1.152)* | 1.052 (0.995–1.110) | |||
| Country-level factors | |||||
| Middle (vs low) GDP | 1.496 (0.531–2.920) | 1.561 (0.585–3.046) | |||
| High (vs low) Adult literacy rate | 0.482 (0.207–1.139) | 0.489 (0.230–0.936)* | |||
| Average (vs low) Health expenditure | 2.289 (0.665–6.258) | 2.235 (0.570 −5.480) | |||
| Random effects | |||||
| Country-level | |||||
| Variance (95 Crl) | 0.852 (0.457–1.503) | 0.785 (0.415–1.420) | 0.826 (0.439–1.478) | 0.732 (0.371–1.371) | 0.723 (0.364–1.347) |
| ICC (%) | 20.57 | 19.26 | 20.06 | 18.18 | 17.83 |
| MOR ((%, 95% Crl) | 2.40 | 2.32 | 2.37 | 2.25 | 2.24 |
| Explained variation (%) | Reference | 7.90 | 3.10 | 14.20 | 15.20 |
| Community-level | |||||
| Variance (95 Crl) | 0.002 (0.000–0.004) | 0.002 (0.001 to 0.003) | 0.003 (0.001–0.005) | 0.003 (0.001–0.005) | 0.042 (0.014–0.072) |
| ICC (%) | 20.61 | 19.30 | 20.12 | 18.24 | 18.87 |
| MOR ((%, 95% Crl) | 1.04 | 1.04 | 1.05 | 1.05 | 1.22 |
| Explained variation (%) | Reference | −10.50 | −68.70 | −70.40 | −2679.90 |
| Model fit statistics | |||||
| DIC | 5641 | 5593 | 5629 | 5640 | 5584 |
DIC – Deviance Information Criterion; ICC – intra-cluster correlation; MOR – median odds ratio; OR- odds ratio; CrI – credible interval.
aModel 1 is null model, baseline model without any determinant variable. bModel 2 is additionally adjusted for individual-level factors.
cModel 3 is additionally adjusted for community-level factors. dModel 4 is additionally adjusted for country-level factors.
eModel 5 is additionally adjusted for individual-, community-, and country-level factors.
*: p < 0.05
There was also significant association between non-uptake of DTP3 and countries with low adult literacy rate (Table 3). Countries such as Burkina Faso, Chad, Cote d’Ivoire, Ethiopia, Gambia, Guinea, Liberia, Mali, Niger, Senegal and Sierra Leone which are mainly West African countries are the ones with low adult literacy rate (Table 2). Women living with HIV in these countries are less likely to have their children vaccinated with DTP3.
Measures of variations (random effects)
In model 1 (unconditional model), there was a significant variation in the odds of non-vaccination with DTP3 of the children of HIV-infected mothers across the countries (σ2 = 0.852, 95% CrI 0.457 to 1.503) and across the communities (σ2 = 0.002, 95% CrI 0.000–0.004) (as shown in Table 3). The intra-country and intra-community correlation coefficients show that 20.57% and 20.61% of the variance in odds of non-uptake of DTP3 are linked to country- and community-level factors respectively. The variance in odds of not being vaccinated with DTP3 were also attributable to the country- and community-level factors respectively. From the full model (Model 5), it is assumed that a child who moved to another country or community with a higher probability of DTP3 non-uptake, the median increase in the odds of DTP3 non-uptake would be 2.24% and 1.22% respectively.
Discussion
Main findings
This study demonstrated that individual, community and country contexts in which the children of HIV-infected mothers live are closely associated with non-uptake of DTP3. These factors are significant in explaining the variations in non-uptake of DTP3 in the children of HIV-infected mothers in the selected sub-Saharan African countries. Non-uptake of DTP3 is less likely in children of women living with HIV who were employed, within the age group 35–49 years, educated and with access to media. It could then be extrapolated that the children of HIV-infected women who were unemployed, younger, uneducated, and without access to media are more likely to miss out on DTP3 uptake. DTP3 non-uptake is also associated with the children of HIV-infected women living in communities with high illiteracy level and in countries with low adult literacy rate. Some of these findings are in conformity with an earlier South African study.18 These findings show that the unemployed status of HIV-infected mothers contributes to their children being incompletely vaccinated. The inability of the unemployed and poorer mothers to source funds for transport to health centres for scheduled vaccinations may be a vital reason for the non-uptake of the vaccines.19,20 Unemployment leads to poverty, and studies have shown that the more the poverty level of a household, the more likely it is that its children would be incompletely vaccinated.21 Lack of basic resources leads to poor health seeking behaviour and deprivation of required immunization, and subsequently being exposed to vaccine-preventable diseases.21
The low likelihood of the younger HIV-infected mother, possibly having her first child, to take her child for vaccination may be as the result of lack of information concerning the importance of immunization. The older women, having cared for many children, are likely to know the importance of immunization.21,22 This study shows that education plays a major role in improving vaccination coverage. The probability of a child of an HIV positive mother not taking DTP3 is reduced in women with any form of formal education compared to their uneducated counterparts. This gives credence to similar studies on immunization in the general population in some African countries.19–21,23 Many of the countries that have low adult literacy rate are also among the countries that are in dire need of support by GAVI in order to meet their individual national targets for immunization.24 All of these show that literacy level has a significant impact on vaccination coverage and national immunization programmes. Furthermore, our findings demonstrated clustering effects of non-uptake of vaccinations at community and country levels. This implies that HIV exposed children from the same communities were inclined to have similar vaccination status and are subjected to similar contextual characteristics within the communities.25
Policy implications
There is a need for an evidence-based methodology to investigate why various immunization programmes are not reaching the expected targets. Understanding the factors responsible for successful implementation of immunization programmes among HIV-exposed children in sub-Saharan Africa is crucial for policy making. Appropriate approaches are needed to tackle various identified gaps of immunization programmes specifically among HIV-exposed children. Evidence-based approaches are also needed to manage scarce resources needed for various health interventions and thereby preventing diseases.26,27 The findings from this multilevel analysis show that mothers who were educated, older, employed and having access to media were less likely not to have had their children vaccinated with DTP3. These findings also imply that lack of education, youthfulness, unemployment and, lack of access to print and electronic media are possibly significant contributory factors to the problem of non-uptake of life-saving vaccines among the children of women living with of HIV in sub-Saharan Africa. Non-uptake of DTP3 was also found to cluster within communities, thus escalating the risk of vaccine-preventable diseases among the HIV-exposed and infected children.
Public health interventions should be designed specifically for women living with HIV who are young mothers, unemployed women and those without formal education. The remedial interventions should also focus on HIV-infected women who are resident in communities with high illiteracy rate in Africa. Our findings shows that access to media reduces non-uptake, therefore, intervention such as the use of mass media system should be in place in the areas with need. The use of multimedia intervention has been proven to be effective and useful for childhood immunization programmes among sub-Saharan African countries and could be specially adopted for the HIV-exposed and infected children.28 The use of interactive clinician-delivered communication tools has been found to improve mothers’ knowledge and understanding of good health.29
Immunization activities should be promoted among HIV-infected parents right from the time of the antenatal care and also integrated as part of a broader prevention of mother to child transmission programme.30 Interventions that provide parents, caregivers and other community members with information on the benefit of immunization may improve childhood vaccination coverage in the communities and the countries.31,32There should be renewed efforts to educate the girl child in Africa as it has been proven that been educated improves vaccination uptake. Special attention is needed in countries with high rate of illiteracy since this factor also impact negatively on vaccines uptake. Factors like wealth index, residency, gender and GDP were not associated with DTP3 non-uptake and therefore warrants lesser attention in terms of interventions and policy changes.
Limitations and strengths of this study
DHS are considered as very reliable source of population health data in the Low and Middle Income countries. DHS are large nationally represented surveys involving every section/region of the included countries and with high rates of responses. The surveys were however subjected to social desirability and recall bias. DHS being cross-sectional studies, the data cannot be used to assess causal relationships between the variables. The included surveys were conducted at different times across the countries within a 13 year timeframe, however, Table 1 shows that this did not impact negatively on the study findings.
Conclusion
This study shows that individual and contextual factors contributed significantly to non-uptake of DTP3 among the children of HIV-infected women across sub-Saharan Africa. Policy making regarding childhood vaccination and public health interventions targeted at improving childhood immunization uptake among HIV-exposed and HIV-infected children should incorporate all the contributory factors during the planning, designing and implementation. The interventions should be developed with focus on young mothers, unemployed women, those without formal education and those living in communities with high illiteracy rate. Particular attention should also be given to women living with HIV who are residents of African countries with low adult literacy rate. The use of mass media tools will help improve the mothers’ knowledge and understanding of immunization good health. Efforts should also be made to create more employment opportunities for the unemployed women living with HIV.
Methods
Study design
This study consisted of secondary data analyzes of the cross-sectional population-based demographic health surveys (DHS) from 27 sub-Saharan African countries namely: Angola, Burkina Faso, Burundi, Cameroun, Chad, Democratic Republic of the Congo, Cote d’Ivoire, Ethiopia, Gabon, Gambia, Ghana, Guinea, Kenya, Lesotho, Liberia, Malawi, Mali, Namibia, Niger, Rwanda, Sao Tome and Principe, Senegal, Sierra Leone, Swaziland, Togo, Zambia and Zimbabwe. Only 27 African countries with available DHS HIV and vaccination data sets were included in this studies.
Sampling technique
The DHS were conducted in different African countries with focus on health, demographic, socioeconomic and environmental indicators from a representative sample of women and men in households across the included countries. The DHS sampling frame is made up of enumeration areas (clusters) established in each of these countries. Two stage probabilistic sampling method was also used for survey cluster selection.
Data collection
Data were collected by the use of standardized questionnaires and these were administered to various respondents by trained interviewers. The implementation of the surveys were spear headed in each country by respective National Ministry/Department of Health or other responsible agencies with technical assistance from MEASURE DHS, ICF International, Calverton, Maryland, USA. Development partners such as the United States Agency for International Development (USAID), Global Fund to Fight AIDS, Tuberculosis and Malaria (Global Fund), etc. provided some of the needed funds for the project. This study included countries that collected data on uptake three doses of diphtheria-tetanus-pertussis containing vaccines (DTP3) as well as HIV voluntary counselling and testing in the participating women up to November, 2017.
The participating women were aged between 15 and 49 years and tested during the household survey after consenting to be tested for HIV. Field staff with the required skills and experiences were recruited to work as interviewers. The interviewers were trained according to the DHS training procedures. The interviewers identified members of the household eligible for biomarker collection. The interviewers explained the purpose of the HIV testing to eligible respondents and were assured of their confidentiality prior to the test. HIV data was collected from eligible consenting women after the completion of their individual interview. The interviewers collected respondent’s finger-prick dried blood spot blood samples for laboratory HIV testing. The DHS data collection and analysis used programme protocol specifically designed to include the outcomes like laboratory HIV test and other data attributed to each participating respondents. The women were asked detailed information on their children vaccination history and the vaccination cards were also checked to verify the mother’s claims.
Ethical consideration
The data used for this study were obtained from an existing DHS database. All the identifier information were also removed, thereby the data cannot be traced to a particular individual. Each DHS was approved by the respective National Health Research Ethics Committees of the participating countries and Institutional Review Boards of the ICF International, Calverton and the Centers for Disease Control and Prevention, Atlanta, USA.
Outcome variable
The outcome is defined as a binary variable with the value of ‘1ʹ if there was no uptake of DTP3 and ‘0ʹ if there was an uptake among children aged 12–23 months at any time before the survey as reported on their vaccination cards or by their mothers during interview. The analysis is limited to the children of HIV-infected mothers.
Determinant variables
Individual level factors
The study included the following individual-level factors in the models: the child’s gender (male or female), the age of the mother in completed years (15 to 24, 25 to 34, 35 and above), educational status of the mother (no basic education, primary, secondary or higher), employment status of the mother (whether unemployed or employed), and wealth index (poorer, middle or richer).
Community-level factors
The following community-level factors were included in the model: neighbourhood poverty rate (percentage of households that are below 20% of wealth index), illiteracy rate (that is the percentage of women without formal education within the community), unemployment rate (percentage of women who are unemployed in the community) and place of residence (either urban or rural). The rates were classified as either low or high.
Country-level factors
The following country-level factors were included in the model: gross domestic product per capita, adult literacy rate and health expenditure per capita. These data were obtained from the World Bank Data.33 The country-level variables were also categorized into either low or high in order to assess nonlinear effects and for easy interpretation of results for policy decision making.
Statistical analyzes
The statistical analyzes were done with STATA 14.0 (Stata Statistical Software: Release 14. College Station, TX: StataCorp LP).34 The distribution of respondents were expressed as percentages. Pearson Chi-Square was used to assess the relationship between DTP3 uptake and various variables. Multivariable logistic regression models were used to analyze the association between individual and contextual factors associated with non-uptake of third dose of DTP3 vaccines among the children of women living with HIV. A 3-level model for binary response reporting non-uptake of DTP3 vaccination among the children of women living with HIV (level 1), in a particular community (level 2) and living in a particular country (level 3). Figure 1 shows the conceptual framework for the models at different levels. The conceptual framework will guide towards understanding the objectives of this study.
Figure 1.
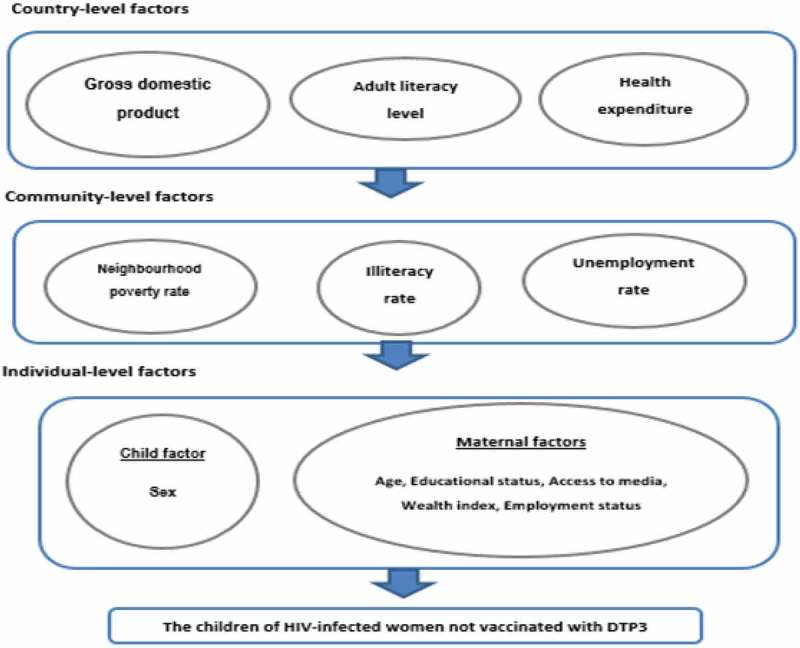
Conceptual framework showing the factors determining non-uptake of DTP3-containing vaccines by the children of HIV-infected mothers.
The study used five models namely:
First model: empty null model, an unconditional model without any explanatory variables
Second model: for only individual-level factors
Third model: for only community-level factors
Fourth model: for only country-level factors
Fifth model (Full model): that controlled for individual-, community- and country-level factors simultaneously.
The fixed effects (measure of association) results were reported as odds ratios (ORs) with their corresponding 95% credible intervals (CrIs). The random effects (measures of variation) results such as variance, intra-cluster correlation (ICC), and median odds ratio (MOR) were also reported. The MLwinN software, version 3.01 was used for model fit analyzes35,36 while Wald test37 was used to calculate the statistical significance of covariates. The significance tests were two-tailed and significance defined at the 5% α- level.
Biography
OOA and OAU conceived the study. OOA did the data analysis, interpreted the results and wrote the initial manuscript. OAU assisted with the data analysis. OAU and CSW reviewed and edited the manuscript. All authors read and approved the final version of the manuscript.
Funding Statement
Olatunji O. Adetokunboh and Charles S. Wiysonge are supported by the National Research Foundation of South Africa and the South African Medical Research Council. Olalekan A. Uthman is supported by the National Institute of Health Research using Official Development Assistance funding. The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, the National Institute for Health Research.
Abbreviations
- AIDS:
Acquired Immunodeficiency Syndrome
- CrIs:
Credible intervals
- DHS:
Demographic health survey
- DTP:
Diphtheria-tetanus-pertussis
- GAVI:
Global Alliance for Vaccines and Immunization
- GDP:
Gross domestic product per capita
- GVAP:
Global Vaccine Action Plan
- HIV:
Human Immunodeficiency Virus
- OR:
Odds ratios
- US$:
United States Dollar.
- WHO:
World Health Organization
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Acknowledgments
We are grateful for the MEASURE DHS for releasing the data for this study.
References
- 1.Tao W, Petzold M, Forsberg BC.. Routine vaccination coverage in low-and middle-income countries: further arguments for accelerating support to child vaccination services. Glob Health Action. 2013;6(1):0–8. PMID: 23639178. doi: 10.3402/gha.v6i0.20343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tchidjou HK, Vescio MF, Sanou Sobze M, Souleyman A, Stefanelli P, Mbabia A, Moussa I, Gentile B, Colizzi V, Rezza G.. Low vaccine coverage among children born to HIV infected women in Niamey, Niger. Hum Vaccin Immunother. 2016;12(2):540–544. PMID:26237156. doi: 10.1080/21645515.2015.1069451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization Global vaccine action plan 2011-2020. Geneva (Switzerland): WHO; 2013. [accessed 2017 Dec 15]. http://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/ [Google Scholar]
- 4.Heffernan RT, Barrett NL, Gallagher KM, Hadler JL, Harrison LH, Reingold AL, Khoshnood K, Holford TR, Schuchat A. Declining incidence of invasive streptococcus pneumoniae infections among persons with AIDS in an era of highly active antiretroviral therapy, 1995 – 2000. J Infect Dis. 2005;191(12):2038–2045. PMID: 15897989. doi: 10.1086/430356. [DOI] [PubMed] [Google Scholar]
- 5.Ormsby CE, De La Rosa-Zamboni D, Vázquez-Pérez J, Ablanedo-Terrazas Y, Vega-Barrientos R, Gómez-Palacio M, Murakami-Ogasawara A, Ibarra-Ávalos JA, Romero-Rodríguez D, Ávila-Ríos S, et al. Severe 2009 pandemic influenza A (H1N1) infection and increased mortality in patients with late and advanced HIV disease. AIDS. 2011;25(4):435–439. PMID: 21139486. doi: 10.1097/QAD.0b013e3283434844. [DOI] [PubMed] [Google Scholar]
- 6.Mast TC, Kigozi G, Wabwire-Mangen F, Sewankambo N, Serwadda D, Gray R, Wawer M, Black R. Immunisation coverage among children born to HIV-infected women in Rakai district, Uganda: effect of voluntary testing and counselling (VCT). AIDS Care. 2006;18(7):755–763. PMID: 16971285. doi: 10.1080/09540120500521053. [DOI] [PubMed] [Google Scholar]
- 7.Eley B. Immunization in patients with HIV infection: are practical recommendations possible? Drugs. 2008;68(11):1473–1481. PMID: 18627205. doi: 10.2165/00003495-200868110-00001. [DOI] [PubMed] [Google Scholar]
- 8.United Nations The millennium development goals report. Geneva (Switzerland): United Nations 2015; 2015. [accessed 2017 Dec 10]. http://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).pdf [Google Scholar]
- 9.ICSU, ISSC Review of the sustainable development goals: the science perspective. Paris, France: International Council for Science (ICSU); 2015. [accessed 2018 Jan 5]. https://www.icsu.org/cms/2017/05/SDG-Report.pdf [Google Scholar]
- 10.Joint United Nations Programmes on HIV/AIDS World AIDS campaign 2002-2003: A conceptual framework and basis for action: HIV/AIDS stigma and discrimination. Geneva (Switzerland): UNAIDS; 2002. [accessed 2018 Jan 5]. http://data.unaids.org/publications/irc-pub02/jc891-wac_framework_en.pdf [Google Scholar]
- 11.Forshaw J, Gerver SM, Gill M, Cooper E, Manikam L, Ward H. 2017. The global effect of maternal education on complete childhood vaccination: A systematic review and meta-analysis. BMC Infect Dis. 17:1–16. doi: 10.1186/s12879-017-2757-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan MT, Zaheer S, Shafique K. 2017. Maternal education, empowerment, economic status and child polio vaccination uptake in Pakistan: A population based cross sectional study. BMJ Open. 7:2012–2013. doi: 10.1136/bmjopen-2016-013853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Devasenapathy N, Jerath SG, Sharma S, Allen E, Shankar AH, Zodpey S. 2016. Determinants of childhood immunisation coverage in urban poor settlements of Delhi, India: A cross-sectional study. BMJ Open. 6:e013015. doi: 10.1136/bmjopen-2016-013015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grimwood K, Lambert SB, Milne RJ. Rotavirus infections and vaccines: burden of illness and potential impact of vaccination. Paediatric Drugs. Internet. 2010;12:235–256. http://www.ncbi.nlm.nih.gov/pubmed/20593908 [DOI] [PubMed] [Google Scholar]
- 15.Quilici S, Smith R, Signorelli C. 2015. Role of vaccination in economic growth. J Market Health Policy. 3:1–8. doi: 10.3402/jmahp.v3.27044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization WHO recommendations for routine immunization.2018[accessed 2018 May 20]. http://www.who.int/immunization/policy/Immunization_routine_table1.pdf?ua=1 [Google Scholar]
- 17.Machingaidze S, Wiysonge CS, Hussey GD. Strengthening the expanded programme on immunization in Africa: looking beyond 2015. PLoS Med. 2013;10:1–5. PMID: 23526886. doi: 10.1371/journal.pmed.1001405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ndirangu J, Bärnighausen T, Tanser F, Tint K, Newell ML. Levels of childhood vaccination coverage and the impact of maternal HIV status on child vaccination status in rural KwaZulu-Natal, South Africa. Trop Med Int Health. 2009;14(11):1383–1393. PMID:19737375. doi: 10.1111/j.1365-3156.2009.02382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wiysonge CS, Uthman OA, Ndumbe PM, Hussey GD. Individual and contextual factors associated with low childhood immunisation coverage in Sub-Saharan Africa: A multilevel analysis. PLoS One. 2012;7(5):e37905 PMID: 22662247. doi: 10.1371/journal.pone.0037905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tesfaye F, Tamiso A, Birhan Y, Tadele T. Predictors of immunization defaulting among children age 12-23 months in Hawassa Zuria District of Southern Ethiopia. Int J Public Health Sci. 2014;3(3):185–193. [Google Scholar]
- 21.Adedokun ST, Uthman OA, Adekanmbi VT, Wiysonge CS. Incomplete childhood immunization in Nigeria: a multilevel analysis of individual and contextual factors. BMC Public Health. 2017;17(1):236 PMID: 28270125. doi: 10.1186/s12889-017-4137-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ibnouf A, Van Den Borne H, Maarse J. Factors influencing immunisation coverage among children under five years of age in Khartoum State, Sudan. South African Family Practice. 2007;49(8):14–14f. doi: 10.1080/20786204.2007.10873611. [DOI] [Google Scholar]
- 23.Uthman OA, Adedokun ST, Olukade T, Watson S, Adetokunboh O, Adeniran A, Oyetoyan SA, Gidado S, Lawoko S, Wiysonge CS. Children who have received no routine polio vaccines in Nigeria: who are they and where do they live? Hum Vaccin Immunother. 2017;13(9):2111–2122. PMID:28665749. doi: 10.1080/21645515.2017.1336590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Global Alliance for Vaccines and Immunisation GAVI annual report 2016. 2017. [accessed 2017 Dec 27]. http://www.gavi.org/progress-report/
- 25.Merlo J. A brief conceptual tutorial of multilevel analysis in social epidemiology: linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. 2005;59(6):443–449. PMID:15911637. doi: 10.1136/jech.2004.023473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wiysonge CS, Lavis JN, Volmink J. Make the money work for health in sub-Saharan Africa. Lancet. 2009;373(9670):1174 PMID:19345830. doi: 10.1016/S0140-6736(09)60685-1. [DOI] [PubMed] [Google Scholar]
- 27.Wiysonge CS, Volmink J. Strengthening research capacity. Lancet. 2002;359(9307):713 PMID:11879902. doi: 10.1016/S0140-6736(02)07798-X. [DOI] [PubMed] [Google Scholar]
- 28.Grilli R, Ramsay C, Minozzi S. Mass media interventions: effects on health services utilisation. Cochrane Database Syst Rev. 2002;(1):CD000389 PMID:11869574. doi: 10.1002/14651858.CD000389. [DOI] [PubMed] [Google Scholar]
- 29.Trevena LJ, Davey HM, Barratt A, Butow P, Caldwell P. A systematic review on communicating with patients about evidence. J Eval Clin Pract. 2006;12(1):13–23. PMID:16422776. doi: 10.1111/j.1365-2753.2005.00596.x. [DOI] [PubMed] [Google Scholar]
- 30.Adetokunboh OO, Oluwasanu M. Eliminating mother-to-child transmission of the human immunodeficiency virus in sub-Saharan Africa: the journey so far and what remains to be done. J Infect Public Health. 2016;9(4):396–407. PMID: 26194038. doi: 10.1016/j.jiph.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 31.Oyo-Ita A, Wiysonge C, Oringanje C, Nwachukwu CEC, Oduwole O, Meremikwu MM. Interventions for improving coverage of childhood immunisation in low- and middle-income countries (Review). Cochrane Database Syst Rev. 2016;7:CD008145 PMID:27394698. doi: 10.1002/14651858.CD008145.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wiysonge CS, Young T, Kredo T, McCaul M, Volmink J. Interventions for improving childhood vaccination coverage in low- and middle-income countries. S Afr Med J. 2015;105(11):892–893. PMID:26632308. doi: 10.7196/SAMJ.2015.v105i11.10177. [DOI] [PubMed] [Google Scholar]
- 33.World Bank The world bank data. [accessed 2017. accessed December 22, 2017 Dec 22]. http://data.worldbank.org/ [Google Scholar]
- 34.StataCorp Stata statistical software: release 14. College Station (TX): StataCorp LP; 2015. [Google Scholar]
- 35.Larsen K, Petersen JH, Budtz-Jrgensen E, Endahl L. Interpreting parameters in the logistic regression model with random effects. Biometrics. 2000;56(3):909–914. PMID:10985236. [DOI] [PubMed] [Google Scholar]
- 36.Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol. 2005;161(1):81–88. PMID: 15615918. doi: 10.1093/aje/kwi017. [DOI] [PubMed] [Google Scholar]
- 37.Rasbash J, Steele F, Browne W, Prosser B. A user’s guide to MLwiN. Bristol, UK: Centre for Multilevel Modelling, University of Bristol; 2015. [Google Scholar]


