Abstract
Objective:
We sought to evaluate two approaches with varying time and complexity in engaging adolescents with an Internet-based preventive intervention for depression in primary care. We conducted a randomized controlled trial comparing primary care physician motivational interview (MI, 10–15 minutes) + Internet program versus brief advice (BA, 2–3 minutes) + Internet program.
Setting:
Adolescent primary care patients in the United States, ages 14–21.
Participants:
83 individuals (40% non-white) at increased risk for depressive disorders (sub-threshold depressed mood > 3–4 weeks) were randomly assigned to either the MI group (n=43) or the BA group (n=40).
Main Outcome Measures:
Patient Health Questionnaire (PHQ-A) – Adolescent and Center for Epidemiologic Studies Depression Scale (CES-D).
Results:
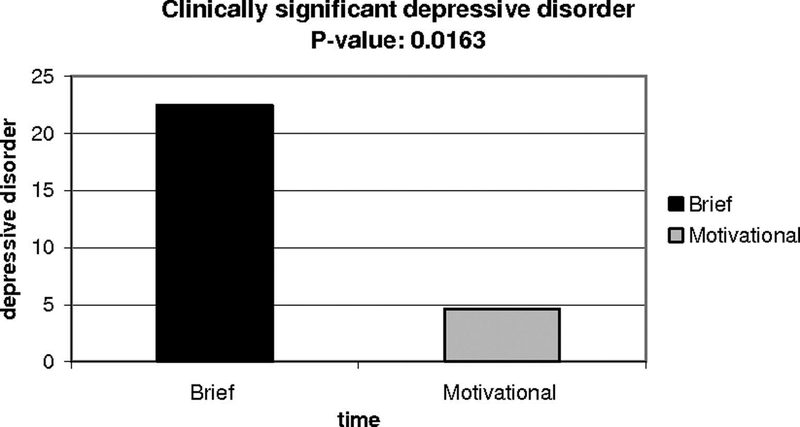
Both groups substantially engaged the Internet site (MI, 90.7% versus BA 77.5%). For both groups, CES-D-10 scores declined (MI, 24.0 to 17.0 p < 0.001; BA, 25.2 to 15.5, p < 0.001). The percentage of those with clinically significant depression symptoms based on CES-D-10 scores declined in both groups from baseline to twelve weeks, (MI, 52% to 12%, p < 0.001; BA, 50% to 15%, p < 0.001). The MI group demonstrated declines in self-harm thoughts and hopelessness and was significantly less likely than the BA group to experience a depressive episode (4.65% versus 22.5%, p = 0.023) or to report hopelessness (MI group of 2% versus 15% for the BA group, p=0.044) by twelve weeks.
Conclusions:
An Internet-based prevention program in primary care is associated with declines in depressed mood and the likelihood of having clinical depression symptom levels in both groups. Motivational interviewing in combination with an Internet behavior change program may reduce the likelihood of experiencing a depressive episode and hopelessness.
Keywords: depressive disorder; adolescents, prevention; Internet; primary care; intervention
Introduction
Depressive disorders have emerged as a major public health problem in developed economies. One quarter of individuals will experience a depressive disorder during adolescence.1 Even with treatment, remission rates remain below 60–70% and educational attainment may be delayed.2, 3 World Health Organization reports and a recent Cochrane review have called for the development of preventive interventions to reduce the burden of this disorder. 4, 5,6 Primary care is a critical setting for identification and treatment of adolescent depression and is a natural setting for preventive interventions. The controversy with regard to black box warnings for suicide risk for selective serotonin reuptake inhibitors (SSRIs) and the lack of availability of promising preventive behavioral approaches (group and individual) have restricted the range of treatment options available to primary care physicians. 7, 8 Internet-based behavioral interventions for anxiety and depression have demonstrated benefits in randomized trials for adults in Australia, the United Kingdom and the Netherlands 9–12 and are recommended as standard practice in the United Kingdom. 13 However, few similar interventions have been developed for adolescents and they have been limited by low levels of participation.14, 15
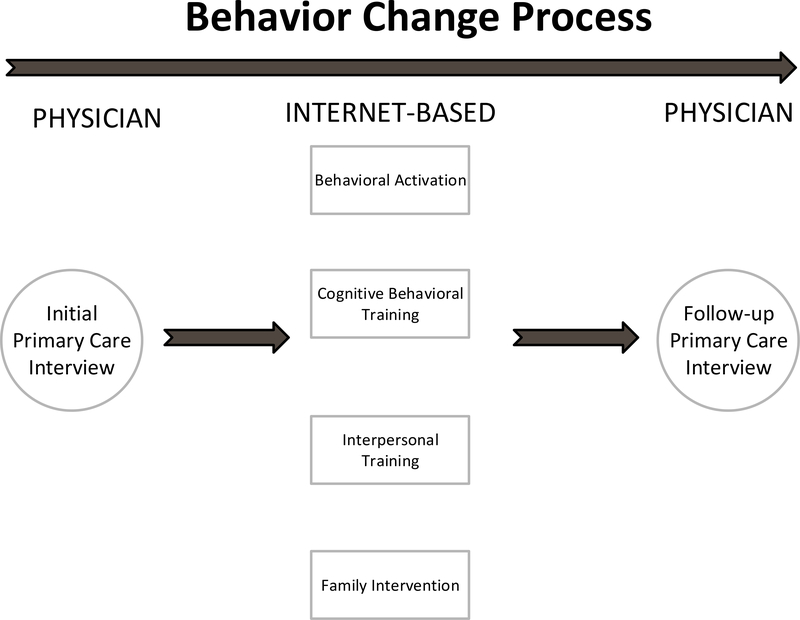
To address the need for a low cost and easily accessible behavioral intervention in primary care, we developed an Internet-based preventive intervention (Figure 1). 16, 17 In this model, the primary care physician utilizes either a brief advice (BA, brief recommendation based on physician authority, 1–3 minutes) or motivational interview (MI, collaborative model on building motivation, 10–15 minutes) approach to engage the adolescent with an Internet-based behavior change/resiliency building intervention (Project CATCH-IT, for Competent Adulthood Transition with Cognitive-behavioral and Interpersonal Training). A pilot study of the MI version of the CATCH-IT intervention demonstrated high levels of Internet component participation and favorable trends (not statistically significant) in three factors (depressed mood, automatic negative thoughts, social support) when using the motivational interview approach. 17 However, we do not know what is the most appropriate method for a primary care physician to actively engage adolescents with an Internet-based behavior change program.
Figure 1:
Intervention Model, where the physician utilizes brief advice or motivational interview techniques to initiate teen engagement with the Internet-based (CATCH-IT) component of the intervention
We examined the relative effectiveness of these two strategies (MI versus BA) on utilization of the Internet intervention and in turn, on symptoms of depressive disorder and mood outcomes. Our first hypothesis was that the BA group participants would be less likely to substantively engage the Internet site. Our second hypothesis was that BA group participants would not demonstrate a significant decline in measures of depressed mood (similar to control groups in other prevention and internet studies) while we would observe a significant decline in the MI group. 11, 14, 18–22 Our third hypothesis was that incidence of depressive disorder and/or depressive episodes would be higher in the BA group than the MI group. We report Internet participation and depressive disorder outcomes for a randomized clinical trial comparing MI + Internet versus BA + Internet in an at risk sample of adolescents.
Methods
Study Design:
We conducted a randomized controlled trial comparing motivational interview (MI) plus Internet intervention (MI group) versus brief advice (BA) plus Internet intervention (BA group) in thirteen primary care sites in the United States (South and Midwest). This was a phase II study intended to determine the form and dose of primary care practitioner (PCP) interview time needed to effectively engage youth with this program. Consequently, no treatment as usual group was included. We compared adolescent baseline outcome measures with those at six and twelve weeks within the MI and BA groups (repeated measures) and also between the MI and BA groups at the same time points (Figure 1). Practices elected to either have their own primary care physicians conduct the interview (N=10 practices, physicians received pro-rated reimbursement of $100.00/adolescent) or have the study principal investigator ((PI), also a primary care physician, N=3 practices) conduct the interview. All protocols were approved by the University of Chicago Institutional Review Board and local site Institutional Review Boards.
Recruitment:
We recruited primary care sites by approaching five major health care organizations (all agreed to participate) and then approached physicians within those organizations. Recruitment of adolescents occurred in both protocols from February 1, 2007, to November 31, 2007. Recruitment was accomplished by screening all adolescents visiting the primary care provider (PCP) for risk of depressive disorder (presence of at least one core symptom of depressive disorder for at least two weeks) 23 as well as through advertisements posted in and around the clinics. Study staff contacted the adolescent by phone to conduct a full eligibility assessment which included the full Patient Health Questionnaire-Adolescent (PHQ-A) assessment (after written informed consent obtained from adolescent and parent). 23 Adolescents were compensated $75.00 (principal investigator performed interview) or $100.00 (own PCP performed interviews, involved one extra visit with study team for consenting, hence higher payment).
Adolescent Inclusion and Exclusion Criteria:
Participants were required to be between the ages of 14–21 years and experiencing persistent sub-threshold depression. Persistent sub-threshold depressed mood was defined as reporting one core symptom of depression: i.e., depressed mood, irritability or loss of pleasure for at least a few days in the last two weeks at two assessment points: 1) the PCP screening and then again at 2) the eligibility assessment (usually 1–2 weeks after initial PCP screening). We sought to include a heterogeneous sample of adolescents representative of those seen in primary care clinics. Adolescents were excluded only if they were undergoing active treatment (within one year of treatment initiation) for major depression (rural physicians could enroll individuals with borderline major depression); expressed frequent suicidal ideation or actual intent; reported prior diagnosis of schizophrenia or bipolar disorder, a pattern of conduct disorder behaviors or met full criteria for major depression, substance abuse, generalized anxiety, panic, or eating disorders based on the Patient Health Questionnaire- Adolescent Questionnaire assessment. The Patient Health Questionnaire is a validated primary care assessment tool used to evaluate common mental disorders based on the Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition (DSM-IV).23 Individuals who reported symptoms but did not meet criteria for conduct disorder, generalized anxiety disorder, or past (rather than present) substance abuse were not excluded. Those found to meet criteria for a mental disorder were referred for treatment.
Primary Care Intervention and Training:
Physicians performed initial and follow-up interviews for each participant (Figure 2). Randomization was blocked in order to assure that each clinician performed an equal or nearly equal number of interviews of each type (BA and MI). Physicians and office staff were trained using a lecture/video example format (1 hour and 15 minutes). In the BA condition the physician takes a directive approach and advises the adolescent that the adolescent is experiencing depressed mood and that the adolescent is at risk for progressing to depressive disorder and refers the adolescent to the CATCH-IT Internet site (1–2 minutes).24 In the MI condition, the physician used a non-directive approach to help the adolescent develop a favorable cost/benefit assessment toward completing the intervention and building resiliency. The MI group also received three motivational phone calls from social worker case managers (three hours of training, licensed clinical social worker).
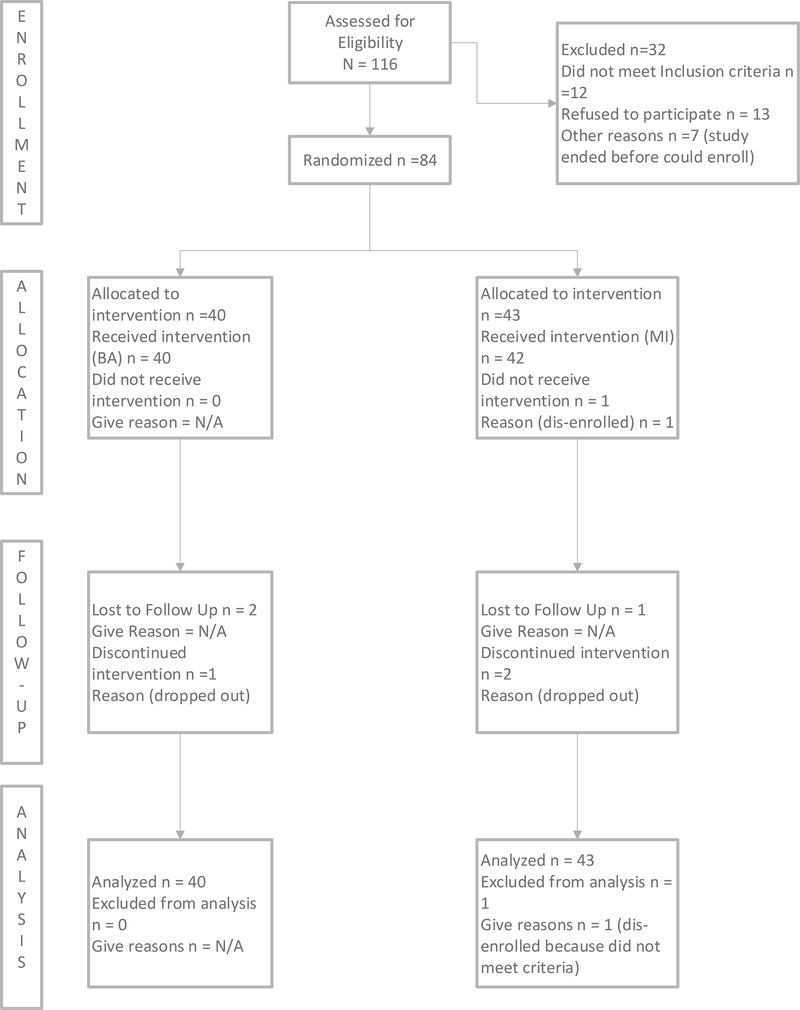
Figure 2:
CONSORT Study Diagram, displaying the progress of all participants through the pilot trial
Internet Intervention:
Both groups received equal and private (secure sign-in) access to the Internet site. All procedures were Health Insurance Portability and Accountability Act (HIPAA) compliant. The intervention is comprised of 14 modules based on Behavioral Activation (BAC), Cognitive Behavioral Therapy (CBT),25, 26 Interpersonal Psychotherapy (IPT),27, 28 and a community resiliency concept model. 29 These components were constructed from manuals with demonstrated efficacy in face to face delivery models using a systematic method based on principles of effective translation of preventive interventions to community settings and instructional design theory. 30, 31,32 Developed by a multi-disciplinary team consisting of primary care physicians, clinical psychologists, psychiatrists and young adults, the intervention was intended to reduce multiple thoughts (dysfunctional thoughts, impaired problems solving, pessimistic expectations), behaviors (procrastination, passivity and avoidance) and interpersonal interactions (indirect communications), thought to increase vulnerability to depressive disorders. CATCH-IT also endeavors to strengthen behaviors (behavioral scheduling of pleasurable activities), thoughts (optimistic appraisals, counter thoughts, effective problem solving), and interpersonal relations (effective social problem solving and building and engaging social support) thought to be protective against depressive disorders. Additionally, acknowledging that risk factors occur within ecological contexts and across multiple domains, a parent workbook which focuses on supporting the development of resiliency in one’s adolescent was provided to the parents of adolescents under the age of 18 in order to enhance the intervention effects. 33
Consent, Enrollment, Randomization and Blinding:
Study staff completed informed consent with adolescents and their parents. Participants were randomized and their group assignment was provided to them after enrollment (consent and complete baseline questionnaire). Participants were stratified by either physician (own primary care physician conducted interviews) and/or by gender (principal investigator conducts interviews) and randomized (using sealed envelopes prepared prior to the start of the study) to receive either the “long interview” (MI) or the “short interview” (BA).
Sample Characteristics:
We obtained information on relevant baseline characteristics to facilitate interpretation of the data. This included; age, ethnicity, birth order, parents marital status and living situation. With regard to adolescent and parent education, we asked, “please indicate the number of years of school completed” with response choices of high school at least 2 years, finished high school, college at least 2 years, and finished college for the adolescent and each parent (adolescent report). In order to understand their past history and experience with depressive disorder, we asked “Have you ever been treated for depression?” with responses that included medication or counseling. In terms of family history of depressive disorder, we asked “Have any of your family members (mother, father, sister, brothers) ever been treated for depression that lasted at least four weeks?”
Assessment of Interview Fidelity and Internet Participation:
We evaluated the fidelity of interview style (BA or MI) using a MI rating system (twenty six taped interviews selected at random, thirteen for each group).34 For the PCP administered interviews, we used audiotapes of the actual interview with the adolescent. In the case of PI administered interviews, we used video tapes with standardized participants. We report these results as a scale that included all the key rated elements (e.g. collaboration, autonomy and MI behaviors). We also report the mean time for each interview. For the Internet component adherence, we report the mean number of minutes on site, mean percentage of exercises completed (defined as number of exercise response fields with any characters typed in/total number of exercise fields, the reported mean is the mean percentage for each participant for those who visited the site), and the number of characters typed for both groups. We report mean number of safety and motivational calls (motivational group only) received by participants in each group.
PHQ-A (DSM-IV) Depressive Disorder and Core Depressive Symptoms Outcomes:
We report depressive disorder based on the Diagnostic and Statistical Manual of Mental Disorders – Fourth Edition (DSM-IV) using the Patient Health Questionnaire – Adolescent (PHQ-A). 23 The PHQ-A derived outcomes include separate categories for current prevalence of major depression, minor depression, dysthymia, or any depressive disorder; and presence of core symptoms in the last two weeks (every day, a few days, or none).
Clinically significant depressive episodes:
We also report cumulative incidence of “clinically significant depressive episodes” which includes all individuals either meeting criteria for major depressive disorder according to the DSM-IV at the assessment points (N=3) or who were diagnosed and treated for depressive disorder by a non-study clinician (N=8). This variable was not defined a-priori but constructed as the study progressed in order to monitor the referral and follow-up of individuals identified as in need of treatment intervention. All individuals who reported worsening depressed mood or demonstrated increasing depressed mood during the study were referred for evaluation and treatment by a mental health specialist in collaboration with their PCP. Subsequent status with regard to evaluation and treatment was obtained in follow-up calls by study staff.
Center for Epidemiologic Studies Depression Scale Outcomes:
We report outcomes derived from the Center for Epidemiologic Studies Depression Score 10-item measure (CESD-10). The reliability and validity of the CES-D has been demonstrated in several studies in adolescent populations. 35 With regard to the CESD-10 (scored as doubled to create a standard 60 point scale), we report the total CESD-10 scores and percentage of individuals above and below standard cut-offs, including asymptomatic and symptom free (females < 14 and males <11) clinically significant depressed mood (CESD-10 > 29 females, > 23 males) and subsyndromyl depressed mood (CES-D-10 14–29 females and 11–23 males).22, 35
PHQ-A Self-harm Risk:
We report adolescent responses with regard to self-harm risk. Self-harm thoughts in the last two weeks included those who responded “yes” to, “Have you often had thoughts that you would be better off dead, or of hurting yourself in some way in the last two weeks?” A second question asked, “Has there been a time in the past month when you have had serious thoughts about ending your life?” Response of “yes” to either of these items was considered endorsing “any self-harm thoughts.” With regard to hopelessness, we report the percentage who responded “yes” to, “In the last two weeks, have you often felt hopeless about the future?”
Data Collection and Training of Personnel:
Outcomes were ascertained through blinded phone assessment interviews (Master’s level social workers or psychologists) at six weeks and twelve weeks post randomization. Each of the assessment callers received an additional four training sessions in the conduct of structured psychiatric interviews and suicide prevention. Assessment callers were blinded to group assignment (worked offsite, no contact with motivational caller) and the effectiveness of blinding was assessed at post-study debriefing.
Data Analysis:
We compared outcomes within groups (MI or BA) between baseline and follow-up (six and twelve weeks) as well as between groups based on an intent-to-treat analysis. If the six week phone assessment call was not completed (N-15) because of difficulty making contact with the adolescents, we used post-study CES-D (self-report) and interview reports (face-to-face debriefing with PI) at 4–6 weeks for study endpoints. For the seven participants who were not available at follow-up at six weeks, we used the most conservative imputation method, last-observation-carried-forward (LOCF) to address missing data. 36 We also performed an additional analysis that did not use imputed data. For categorical outcomes with repeated measures, we used the McNemar’s test, and when relevant (< 5 observations per cell), the exact version. For between-group comparisons, we used the Pearson’s chi-squared test or the Fisher’s exact test when there were < 5 observations per cell. For continuous outcomes, we used paired t-tests for within group comparisons between different time points and analysis of variance (ANOVA) for between group comparisons at the same time points. We used logistic regression or analysis of covariance (ANCOVA) to adjust for any significant differences between groups at any time points for baseline differences in demographics and depressed mood. For continuous between-group data with non-normal distribution, we used the Mann-Whitney test for comparisons. Stata Version 10.0 (College Station, TX, 2008) was used for all analyses.
Sample Size and Stopping Rules:
The original sample size calculations (N=46 in each group, N=92 total) were based on differences in CESD-10 scores of 12.5 versus 8.5 with an estimated standard deviation value of 6.5 with 80% power and alpha=0.05.17 The stopping rules included a clear advantage being demonstrated in one study or conversely, safety concerns in either arm. The Data Safety and Monitoring Board met quarterly to review interim analyses, including all main outcomes and safety monitoring.
Results
Sample Characteristics:
We evaluated 116 individuals for participation of which 103 were eligible and 84 were enrolled and 83 are included in the analyses (Figure 2, one immediately disenrolled because of meeting exclusion criteria). The sample was ethnically diverse (40% non-white) and approximately divided equally by gender (Table 1) with a mean age slightly above 17 years. There were no significant differences between the two randomization groups at baseline in gender, ethnicity, age, education, family or teen variables, past treatment history, family history, or baseline depressed mood/disorder.
Table 1.
Comparison of Baseline Characteristics by Group
| Motivational (n = 43) |
Brief Advice (n = 40) |
Group Comparison | |||
|---|---|---|---|---|---|
| (Mean)/Percent | (SD), N | (Mean)/Percent | (SD), N | p | |
| Gender | .83 | ||||
| Male | 45.45 | 19 | 41.46 | 17 | |
| Female | 54.55 | 24 | 58.54 | 23 | |
| Ethnicity | .56 | ||||
| White | 59.52 | 26 | 60 | 24 | |
| Black | 19.05 | 8 | 32.5 | 13 | |
| Hispanic | 7.14 | 3 | 2.5 | 1 | |
| Asian | 11.9 | 5 | 2.5 | 1 | |
| Native American | 0 | 0 | 0 | 0 | |
| Other | 2.38 | 1 | 2.5 | 1 | |
| Age(yrs) | (17.44) | (2.17) | (17.34) | (1.96) | .89 |
| Family information | |||||
| First born | 45.24 | 19 | 48.65 | 19 | .76 |
| Parents marital status | .72 | ||||
| Married | 59.52 | 26 | 50 | 18 | |
| Divorced | 21.43 | 9 | 19.44 | 7 | |
| Separated | 2.38 | 1 | 2.78 | 1 | |
| Widowed | 0 | 0 | 0 | 0 | |
| Never married | 16.67 | 7 | 27.78 | 10 | |
| Teen living situation | .12 | ||||
| At home with parents | 61.9 | 26.00 | 76.32 | 29 | |
| Alone | 0.00 | 0 | 5.26 | 2 | |
| With friends or roommates | 26.19 | 11 | 10.53 | 4 | |
| Other | 11.9 | 5 | 7.89 | 3 | |
| Father’s education | .12 | ||||
| High school at least 2 yrs.’ | 2.63 | 1 | 11.43 | 4 | |
| Finished high school | 26.32 | 10 | 40 | 14 | |
| College at least 2 yrs. | 18.42 | 7 | 5.71 | 2 | |
| Finished college | 52.63 | 20 | 42.86 | 15 | |
| Mother’s education | .99 | ||||
| High school at least 2 yrs. | 7.69 | 3 | 5.56 | 2 | |
| Finished high school | 25.64 | 10 | 27.78 | 10 | |
| College at least 2 yrs. | 28.21 | 11 | 25 | 9 | |
| Finished college | 38.46 | 15 | 41.67 | 15 | |
| Teen’s education | .92 | ||||
| High school at least 2 yrs. | 57.89 | 22 | 60 | 21 | |
| Finished high school | 13.16 | 5 | 11.43 | 4 | |
| College at least 2 yrs. | 28.95 | 11 | 25.71 | 9 | |
| Finished college | 0 | 0 | 2.86 | 1 | |
| Depression history | |||||
| History of depression or emotional disorder | |||||
| treatment | 26.19 | 41 | 29.73 | 37 | .73 |
| Family history of depression | 45.24 | 19 | 60.53 | 23 | .17 |
| PHQ-A DSM-IV depressive disorder outcomes | |||||
| Depressive disorder any PHQ-A | |||||
| Major depression | 2.7 | 1 | 5.26 | 2 | .58 |
| Minor depression | 10.81 | 4 | 5.26 | 2 | .38 |
| Dysthymia depressed mood > half days last 6 months | 2.7 | 1 | 0 | 0 | .31 |
PHQ-A, Patient Health Questionnaire-Adolescent assessment; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders—Fourth Edition
Assessment of Interview Fidelity and Internet Participation:
As shown in Table 2, interview fidelity ratings (physicians) and Internet participation levels (adolescents) were high in both groups. As expected, ratings of the MI fidelity scale demonstrated high fidelity to the MI model in the MI group (4.5 (SD =0.83) out of a possible 5.0 score) while the BA interviews demonstrated low adherence to the MI model (1.02, SD=0.07), and this comparison was statistically significant (p=0.003). Similarly, the MI interview length was signficantly longer than the interview for the BA group (p=0.002). Preliminary qualitative review of the taped interviews revealed many adolescents provided only very short response to open-ended MI questions. With regard to hypothesis one, the MI group spent more time on site and typing more characters in the exercises as can be seen in Table 2. The mean number of safety calls was similar in both groups.
Table 2.
Assessment of Interview Fidelity and Internet Participation
| Motivational |
Brief Advice |
||||
|---|---|---|---|---|---|
| Comparison Mean/(Percent) | SD, (N) | Mean/(Percent) | SD, (N) | p | |
| Interview | |||||
| Motivational Interview Fidelity Rating | |||||
| Scale (ex 0) | 4.21 | 0.83 | 1.02 | 0.07 | 0.003 |
| Interview length (min) | 5.96 | 1.90 | 1.79 | 0.45 | 0.002 |
| Percentage visiting the site | (90.7) | (38) | (77.5) | (31) | 0.13 |
| Mean time on site (min) | 143.70 | 109.05 | 98.40 | 124.60 | 0.02 |
| Mean percentage of exercises completed | (61) | (37) | (67) | (23) | 0.11 |
| Number characters typed into exercises | 3532.74 | — | 1915.90 | 2326.00 | 0.004 |
| Telephone calls | |||||
| Number safety calls | 2.08 | 1.09 | 2.11 | 0.94 | 0.60 |
| Number motivational calls | 2.23 | 0.92 | NA | NA | NA |
Depressive Disorder Related Outcomes in Pre/Post Comparisons:
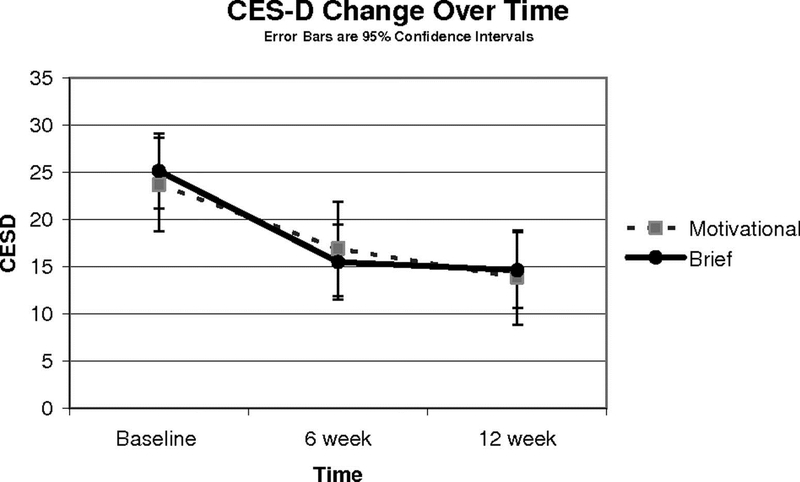
The entire sample (Table 3), the MI group (Table 4), and the BA group (Table 5) all demonstrated significant reductions in overall measures of depressed mood (CESD-10 total score; see Figure 3) and the prevalence of symptoms (PHQ-A score) at six weeks that were sustained at twelve weeks after enrollment (hypothesis two). With regard to DSM-IV mental disorders, the incidence of major depression declined for all participants from baseline to twelve weeks (Table 3). For all participants, comparisons between baseline to six weeks and baseline to twelve weeks, there was a signficant change (decline) in the prevalence of DSM-IV depressive disorder core symptoms. For both groups, CESD-10 symptoms declined below standard cutoff values for clinically significant depressive symptoms. The percentage of those with clinically significant depression symptoms based on CESD-10 scores significantly declined in both groups from baseline to twelve weeks (MI, 52% versus 12%, p=<0.001; BA, 50% versus 15%, p<0.001). The prevalence of depressive disorder (major, minor, and combined) remained low throughout the follow-up period (not significantly different from baseline, except for major depression for all participants, 4% versus 2%, p=0.047). Results did not differ meaningfully when imputed missing data was excluded. With regard to blinding, post-study debriefing revealed that callers were unaware of the randomized trial design or group assignment.
Table 3.
Baseline and 6 and 12 Weeks Outcomes for All Participants (N 83)
| Baseline |
6 wk |
12 wk |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| (Mean)/ Percentage | (SD), N | (Mean)/ Percentage | (SD), N | p Value, Baseline vs 6 wk | (Mean)/ Percentage | (SD), N | p Value, Baseline vs 12 wk | p Value, 6 wk vs 12 wk | |
| Mood measures | |||||||||
| CESD-10 score | (24.46) | (12.35) | (16.46) | (16.46) | <.001 | (14.79) | (9.64) | <.001 | .06 |
| PHQ-A score | (7.35) | (3.83) | (4.83) | (4.83) | <.001 | (4.52) | (4.37) | <.001 | .35 |
| PHQ-A DSM-IV depressive disorder outcomes | |||||||||
| Depressive disorder any PHQ-A | 11 | 9 | 4 | 3 | .29 | 5 | 3 | .69 | 1.00 |
| Major depression | 4 | 3 | 3 | 2 | .56 | 2 | 1 | .047 | .06 |
| Minor depression | 8 | 6 | 1 | 1 | .27 | 3 | 2 | .24 | .20 |
| Dysthymia depressed mood > half days last 6 mo | 3 | 1 | 0 | 0 | 1.00 | 0 | 0 | 1.00 | NA |
| PHQ-A DSM-IV core depressive symptoms outcomes | <.001 | <.001 | .15 | ||||||
| Core symptoms every day | 28 | 21 | 11 | 8 | 7 | 4 | |||
| Core symptoms every other day | 68 | 59 | 44 | 35 | 50 | 43 | |||
| No core symptoms | 4 | 3 | 46 | 38 | 43 | 36 | |||
| CESD-10 outcomes | <.001 | .03 | .02 | ||||||
| Clinically significant depressed mood CESD >29 women, >23 men | 51 | 42 | 23 | 19 | 13 | 11 | |||
| Subsyndromyl depressed mood CESD 14—29 women, 11—23 men | 30 | 25 | 34 | 28 | 37 | 31 | |||
| Symptom free CESD <14 women, <11 men | 19 | 16 | 43 | 36 | 49 | 41 | |||
| PHQ-A self-harm risk | |||||||||
| Self-harm thoughts last 2 wks | 13 | 10 | 4 | 3 | .07 | 3 | 2 | .047 | .03 |
| Serious thoughts of suicide last month | 7 | 5 | 3 | 2 | .69 | 2 | 1 | .03 | .03 |
| Any self-harm thoughts | 16 | 12 | 5 | 4 | .04 | 3 | 2 | .02 | .03 |
| Hopelessness | 30 | 22 | 19 | 14 | .01 | 12 | 7 | .01 | .12 |
CESD, Center for Epidemiologic Studies Depression Scale; PHQ-A, Patient Health Questionnaire-Adolescent assessment; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders—Fourth Edition.
Table 4.
Baseline and 6 and 12 Week Outcomes for the Motivational Interview Group (N 43)
| Baseline |
6 wk |
12 wk |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| (Mean) / Percentage | (SD), N | (Mean)/ Percentage |
(SD), N | p Value, Baseline vs 6 week | (Mean)/ Percentage |
(SD), N | p Value, Baseline vs 12 wk | p Value, 6—12 wk | |
| Mood measures | |||||||||
| CESD-10 score | (24.03) | (12.3) | (17.55) | (11.67) | <.001 | (14.91) | (8.85) | <.001 | .03 |
| PHQ-A score | (7.53) | (3.35) | (4.69) | (3.48) | <.001 | (4.64) | (4.59) | <.001 | .92 |
| PHQ-A DSM-IV depressive disorder outcomes | |||||||||
| Depressive disorder any PHQ-A | 12 | 5 | 3 | 1 | .25 | 6 | 2 | 1.00 | 1.00 |
| Major depression | 3 | 1 | 3 | 1 | 1.00 | 3 | 1 | .25 | .50 |
| Minor depression | 10 | 4 | 0 | 0 | .21 | 3 | 1 | .30 | .28 |
| Dysthymia depressed mood > half days last 6 mo | 3 | 1 | 0 | 0 | .32 | 0 | 0 | NA | NA |
| P Q-A DSM-IV core depressive symptoms outcomes | 07 | 0 | 17 | 61 | |||||
| Core symptoms every day | 30 | 12 | 8 | 3 | 7 | 2 | |||
| Core symptoms every other day | 68 | 30 | 54 | 23 | 54 | 25 | |||
| No core symptoms | 3 | 1 | 38 | 16 | 40 | 16 | |||
| CESD-10 outcomes | 0 | 0 | .02 | 0 | <.001 | .01 | |||
| Clinically significant depressed mood CESD >29 women > 23 men | 52 | 23 | 26 | 12 | 12 | 5 | |||
| Subsyndromyl depressed mood CESD 14—29 women, 11—23 men | 24 | 10 | 38 | 16 | 43 | 18 | |||
| Symptom free CESD <14 women, <11 men | 24 | 10 | 36 | 15 | 45 | 19 | |||
| PHQ-A self-harm risk | 0 | ||||||||
| Self-harm thoughts last 2 wks | 11 | 4 | 3 | 1 | .50 | 3 | 1 | .13 | .25 |
| Serious thoughts of suicide last month | 8 | 3 | 0 | 0 | .50 | 3 | 1 | .25 | .25 |
| Any self-harm thoughts | 14 | 5 | 3 | 1 | .25 | 6 | 2 | .06 | .25 |
| Hopelessness | 27 | 10 | 21 | 8 | .22 | 3 | 1 | .02 | .02 |
CESD, Center for Epidemiologic Studies Depression Scale; PHQ-A, Patient Health Questionnaire-Adolescent assessment; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders—Fourth Edition.
Table 5.
Baseline and 6 and 12 Week Outcomes for the Brief Advice Group (N 40)
| Baseline |
6 wk |
12 wk |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| (Mean) / Proportion | (SD), N | (Mean)/ Proportion |
(SD), N | p Value, Baseline vs 6 wk | (Mean)/ Proportion |
(SD), N | p Value, Baseline vs 12 wk | p Value, 6—12 wk | |
| Mood measures | |||||||||
| CESD-10 score | (25.19) | (12.57) | (15.52) | (11.03) | <.001 | (14.88) | (10.53) | <.001 | .64 |
| PHQ-A score PHQ-A DSM-IV depressive disorder outcomes |
(7.13) | (4.34) | (5) | (4.34) | .01 | (4.5) | (4.18) | .003 | .27 |
| Depressive disorder any PHQ-A | 10 | 4 | 6 | 2 | 1.00 | 4 | 1 | .63 | 1.00 |
| Major depression | 5 | 2 | 3 | 1 | 1.00 | 1 | 0 | .13 | .50 |
| Minor depression | 5 | 2 | 3 | 1 | .54 | 4 | 1 | .37 | .37 |
| Dysthymia depressed mood > half days last 6 mo | 0 | 0 | 0 | 0 | NA | 0 | 0 | NA | NA |
| PHQ-A DSM-IV core depressive symptoms outcomes | 0 | 0 | <.001 | 0 | .11 | .08 | |||
| Core symptoms every day | 26 | 10 | 13 | 5 | 7 | 2.00 | |||
| Core symptoms every other day | 68 | 26 | 32 | 12 | 48 | 20.00 | |||
| No core symptoms | 5 | 2 | 55 | 23 | 45 | 18.00 | |||
| CESD-10 outcomes | 0 | 0 | .01 | 0 | <.001 | .75 | |||
| Clinically significant depressed mood CESD >29 women >23 men | 50 | 20 | 20 | 8 | 15 | 6 | |||
| Subsyndromyl depressed mood CESD 14—29 women, 11—23 men | 35 | 14 | 30 | 12 | 33 | 13 | |||
| Symptom free CESD <14 women, <11 men | 15 | 6 | 50 | 20 | 53 | 21 | |||
| PHQ-A self-harm risk | 0 | 0 | 0 | ||||||
| Self-harm thoughts last 2 wks | 16 | 6 | 5 | 2 | .45 | 4 | 1 | .63 | .50 |
| Serious thoughts of suicide last month | 6 | 2 | 5 | 2 | 1.00 | 1 | 0 | .25 | .50 |
| Any self-harm thoughts | 19 | 7 | 8 | 3 | .45 | 4 | 1 | .38 | .50 |
| Hopelessness | 31 | 11 | 18 | 6 | .18 | 15 | 6 | .56 | .22 |
CESD, Center for Epidemiologic Studies Depression Scale; PHQ-A, Patient Health Questionnaire-Adolescent assessment; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders—Fourth Edition
Figure 3:
Depressed Mood (CES-D Scale) by Intention to Treat over
Self-harm Risk:
There was a significant decline in self-harm thoughts and hopelessness for all participants from baseline to six weeks and from six weeks to twelve weeks which is shown in Table 3. There was a change in percentage reporting “any self-harm thoughts” of borderline significance in the MI group (Table 4) (MI, 14% versus 3%, p=0.06) but not for the BA group (Table 5), 19% versus 4%, p=0.38). The percentage of those reporting hopelessness declined for both the MI group and BA groups between baseline and twelve weeks, but was statistically significant only for the MI group. For all participants, hopelessness declined significantly between baseline and six weeks and baseline and twelve weeks, and there was not a statistically significant trend toward further decline between six and twelve weeks.
Intent-to-treat Between-Group Comparisons:
Primary depressive disorder and symptom outcomes at six and twelve weeks were similar between groups, with the exception of prevalence of hopelessness at twelve weeks and the cumulative incidence of clinically significant depressive disorder at twelve weeks (hypothesis three). There was a significant difference in the percentage of those reporting hopelessness at twelve weeks favoring a lower percentage in the MI group of 2% versus 15% for the BA group (p=0.044). For depressive outcomes, the primary difference between the two groups was in the cumulative prevalence of clinically significant depressive episodes as assessed by clinicians which was significantly lower in the MI group at 4.65% versus 22.5% for the BA group (p=0.02, Figure 4). The protective effect of MI persisted for clinically significant depressive episodes (OR 0.068; 95% CI: 0.007, 0.61) after adjustment for demographic factors, baseline depressed mood, prior history of depression treatment and family history of depression. The relationship between MI group and lower likelihood of hopelessness did not persist after adjustment for demographic factors.
Figure 4:
Cumulative Incidents of clinically significant depressive disorder
Effect Size:
Baseline to six week effect sizes were in the moderate to large range. For PHQ-A score, effect sizes were 0.74 (95% CI: 0.43, 1.05) for all participants, 0.94 (95% CI: 0.49, 1.36) for the MI group and 0.58 (95% CI: 0.14, 1.03) for the BA group. With regard to the CESD-10, effect sizes were 0.69 (95% CI: 0.38, 1.0) for all participants, 0.56 (95% CI: 0.14, 0.96) for the MI group and 0.82 (95% CI: 0.35, 1.27) for the BA group. Effect sizes were similar for baseline to twelve week comparisons.
Adverse Events:
There was one suicide attempt (one week after enrollment) in the BA arm. This individual did not report suicidal ideation during the assessment and the event was classified as non-research related due to prior suicide attempts and psychiatric hospitalizations. The Data Safety and Monitoring Board elected to stop enrollment at 84 (intended N=96) because they believed that individuals with past psychiatric hospitalizations or attempts should not be enrolled. They did not want to change inclusion/exclusion criteria late into the study. Also, after reviewing the data, they believed that the major study endpoints had been reached (significant pre/post changes in measures of depressed mood in both groups) and that a significant trend had emerged favoring the MI group for a lower cumulative incidence of clinically signficant depressive episodes.
Discussion
Using a randomized controlled trial design, we evaluated the relative effectiveness of two versions of a primary care/Internet-based intervention intended to prevent depressive disorders in a diverse group of adolescents in thirteen US primary care practices. There was excellent adherence to the primary care interventions by physicians and participation in the Internet intervention by adolescents in both groups. Contrary to expectations, hypothesis two was not confirmed. Both groups demonstrated substantial declines in depressed mood by two instruments. These gains were sustained at twelve weeks after randomization. Nearly half the sample was asymptomatic at six weeks, prevalence of clinically significant depressed mood dropped by more than half, and the incidence of any depressive disorder remained low. MI participants demonstrated a higher levels of time on site and characters typed were less likely to report hopelessness or to have experienced a clinically significant depressive episode by twelve weeks. This provided partial support to hypotheses one and three.
The high level of participation in a mental health intervention (preventive or treatment) for adolescents in primary care that is reported in this study is a new finding. Measures of engagement in this study were much higher than those observed in free-standing Internet-based health and behavior change interventions. These studies report that 30–50% visit Internet sites and most use it for less than 10 minutes.14, 15 The percentage of adolescents in this study visiting the Internet site at least once (90.7% in the MI group and 77.5% in the BA group) compares favorably with the 30% rate of attendance to at least one psychotherapy session in a well designed and executed finding in a primary care chronic disease model intervention study.37
The finding that the BA group participated at levels only modestly less than those in the MI group contrasted with our expectations set out in hypothesis one. This participation by the BA group participants could be explained by the strength of non-specific aspects of the physician-patient relationship in persuading adolescents, the perceived authority of the physician from the adolescent perspective, high intrinsic levels of motivation in adolescents who entered the study, the relatively short version of the MI that was used, receipt of safety calls by both groups (unintentionally acting as prompts to visit the Internet site), many MI participants not receiving MI phone calls, or even the experience of the financial incentive. While motivational interviewing has demonstrated benefits in reducing smoking, drug use and promoting pro-health behaviors in adolescents, many of these interventions are longer than the one used in this study (>1 hour versus our 5–10 minutes).38, 39 While physicians may have completed the manualized MI as directed with high “fidelity”, the short length of the interview and observation that many adolescents provided only very short responses suggests that this “abreviated” MI lacked some of the persuasive power of the more extended version that would be more ideal for study settings. Similarly, BA has demonstrated superiority over usual care in multiple studies and this benefit may be reflected in these data.24
The substantial declines in depressed mood and in the prevalence of clinically significant symptoms and the increase in the percentage of asymptomatic individuals in both groups is another addition to the literature relating to adolescents. The finding that there was significant decline in depressed mood with moderate to large pre/post effect sizes with a stand-alone Internet-based preventive intervention in primary care is also a new finding among adolescents. The levels of depressed mood at baseline are consistent with adolescents at risk for depressive disorders (as identified in other studies in medical settings),20 and with adults enrolled in Internet interventions,11, 12 and are somewhat higher than those in school-based interventions.40, 41 The decline in CESD-10 scores (pre/post with moderate to large effect sizes) are comparable to those demonstrated in successful targeted preventive interventions using face-to-face group psychotherapy (this intervention was based on the same manual) 20, 42 and with the MoodGym, Bluepages,11 and Beating the Blues Internet-based interventions for adults,12 and greater than those reported in school-based interventions.22, 41 Although there was no control group in this study (treatment as usual (TAU) and attention, wait list or supportive counseling) to whose experience we could compare with the two active treatment arms, the control groups in the above referenced studies demonstrate minimal change over six to twelve week intervals after randomization.
The possible protective effect of motivational interviewing in reducing the cumulative incidence of clinically significant depressive episodes and twelve week prevalence of hopelessness is a new contribution and is worthy of replication. This finding could result from the enhancement of motivation to employ coping skills when confronting stressors or the modestly higher levels of participation in the Internet intervention. The coupling of a primary care MI with self-directed behavior change has been demonstrated to be effective in engaging adults with workbook-based programs for depression and alcohol abuse and motivational interviewing may reduce excacerbation of problem drinking.43–45 The potential benefit of motivational interviewing in reducing excacerbation of unwanted behaviors and symptoms may explain why the groups differed little on standard mood measures, but the BA group appears to have had more elevations of depressed mood into the clinically significant range. This may be consistant with the finding that purely “curricular” (e.g., classroom) universal preventive programs have often not proved efficacious for adolescents whereas the same program in an interactive group model targeting mild to moderately depressed adolescents is efficacious.20, 46 Perhaps establishment of personal relevance (symptom levels) and motivation (face-to-face engagement) for prevention are necessary and essential steps for utilizing curricular learning to build affect regulation skills.
The primary strength of this study was the incorporation of the intervention into a variety of practice settings with high fidelity, and the recruitment of a diverse group of adolescents with symptom levels consistent with those found in other preventive studies in adolescents and Internet treatment studies in adults. Limitations in terms of internal validity include difficulty in obtaining timely data collection for adolescents who are often dificult to make phone contact with and reluctant to complete study questionnaires, the possibility of a favorable response bias by adolescents in all groups (i.e., becoming invested in “prevention” and thereby under-reporting symptoms) and inability to blind study staff with exception of phone callers. Another limitation is the use of the Patient Health Questionnaire- Adolescents (PHQ-A) 23 rather than the Kiddie-Schedule for Affective Disorders and Schizophrenia (KSADS) which is more commonly used studies of depressive disorders in children. 47 We selected the PHQ-A because of its ease of use in primary care settings. As with any study, there may be the possibility of a Hawthorne effect where the act of participation resulted in favorable changes. A non-a-priori measure of the clinically significant depressive episode variable is an additional limitation. Similalry, long-term follow-up will be needed to determine if this difference persists (multi-year follow-up in progress).
The reader should consider several elements of the study design in interpreting these results. In terms of external validity, the physician and clinic settings were selected via contact with major healthcare organizations and may have resulted in recruitment of clinicians most pre-disposed to successful implementation of psychosocial interventions. These physician were not only likely more motivated than most, but may have been stronlgy invested in the success of the intervention based on financial incentives and recruitment into the study by respected peers and be more psycho-socially oriented than most PCPs. Similarly, the adolescents may have been more motivated than most, both by their recuitment by their physician, but also by virtue of a financial incentive and, as suggested above, very invested in a favorable outcome for the study. Similarly, the short nature of the interview with many teens offering only short responses suggests they may share broad similarities in response to the intervention with other adolescents.
Conclusions
In conclusion, implementation of an Internet-based intervention for depression prevention in primary care was associated with declines in depressed mood scores, a decrease in prevalence of clinically meaningful symptom levels, and low prevalence of depressive disorder. For clinicians, the results suggest that motivational interviewing and brief advice may both be useful in engaging adolescents with mental health disorders with interventions and that motivational interviewing may confer an added protective benefit in reducing the incidence of depressive episodes. For policy makers, an Internet-based approach may offer a low-cost way to implement depression prevention in community settings. For researchers, randomized trials comparing varying degrees of face-to-face contact coupled with Internet interventions may be essential for developing the optimal delivery model – one with the best cost/benefit ratio and that yields the most effective results. Further research, including development of more engaging Internet models, and randomized clinical trials with a treatment-as-usual care control group, will be critical in determining the full benefit of this approach. A version of the Internet intervention for use by physicians and the general public is available at http://catchit-public.bsd.uchicago.edu.
Acknowledgements:
Supported by a NARSAD Young Investigator Award, Robert Wood Johnson Foundation Depression in Primary Care Value Grant and a career development award from the National Institutes of Mental Health (NIMH K-08 MH 072918–01A2)
Footnotes
Disclosures: Benjamin W. Van Voorhees has served as a consultant to Prevail Health Solutions, Inc and the Hong Kong University to develop Internet-based interventions.
Clinical Trial Registry (clinicaltrials.gov): # NCT00152529 and NCT00145912
References
- 1.Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety. 1998; 7(1):3–14. [DOI] [PubMed] [Google Scholar]
- 2.March J, Silva S, Petrycki S, et al. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents With Depression Study (TADS) randomized controlled trial. Jama. 2004;292(7):807–820. [DOI] [PubMed] [Google Scholar]
- 3.Wilcox-Gok V, Marcotte DE, Farahati F, Borkoski C. Early onset depression and high school dropout In: Marcotte DE, V W-G, eds. The Economics of Gender and Mental Illness. Amsterdam: Elsevier; 2004. [Google Scholar]
- 4.Bramesfeld A, Platt L, Schwartz FW. Possibilities for intervention in adolescents’ and young adults’ depression from a public health perspective. Health Policy. December 2006;79(2–3):121–131. [DOI] [PubMed] [Google Scholar]
- 5.Saxena S, Jane-Llopis E, Hosman C. Prevention of mental and behavioural disorders: implications for policy and practice. World Psychiatry. February 2006;5(1):5–14. [PMC free article] [PubMed] [Google Scholar]
- 6.Bower P, Garralda E, Kramer T, Harrington R, Sibbald B. The treatment of child and adolescent mental health problems in primary care: a systematic review. Fam Pract. August 2001;18(4):373–382. [DOI] [PubMed] [Google Scholar]
- 7.Gibbons RD, Brown CH, Hur K, et al. Early evidence on the effects of regulators’ suicidality warnings on SSRI prescriptions and suicide in children and adolescents. Am J Psychiatry. September 2007;164(9):1356–1363. [DOI] [PubMed] [Google Scholar]
- 8.Richardson LP, Katzenellenbogen R. Childhood and adolescent depression: the role of primary care providers in diagnosis and treatment. Curr Probl Pediatr Adolesc Health Care. January 2005;35(1):6–24. [DOI] [PubMed] [Google Scholar]
- 9.Kaltenthaler E, Shackley P, Stevens K, Beverley C, Parry G, Chilcott J. A systematic review and economic evaluation of computerised cognitive behaviour therapy for depression and anxiety. Health Technology Assessment. 2002;6(22):1–89. [DOI] [PubMed] [Google Scholar]
- 10.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychol Med March 2007;37(3):319–328. [DOI] [PubMed] [Google Scholar]
- 11.Christensen H, Griffiths KM, Jorm AF. Delivering interventions for depression by using the internet: randomised controlled trial. Bmj January 31 2004;328(7434):265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavanagh K, Shapiro DA, Van Den Berg S, Swain S, Barkham M, Proudfoot J. The effectiveness of computerized cognitive behavioural therapy in routine care. Br J Clin Psychol. November 2006;45(Pt 4):499–514. [DOI] [PubMed] [Google Scholar]
- 13.Tylee A. Identifying and managing depression in primary care in the United kingdom. J Clin Psychiatry. 2006;67 Suppl 6:41–45. [PubMed] [Google Scholar]
- 14.Christensen H, Griffiths KM, Korten A. Web-based cognitive behavior therapy: analysis of site usage and changes in depression and anxiety scores. J Med Internet Res. Jan-Mar 2002;4(1):E3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Santor DA, Poulin C, LeBlanc JC, Kusumakar V. Online health promotion, early identification of difficulties, and help seeking in young people. J Am Acad Child Adolesc Psychiatry. January 2007;46(1):50–59. [DOI] [PubMed] [Google Scholar]
- 16.Van Voorhees BW, Ellis JM, Gollan JK, et al. Development and Process Evaluation of a Primary Care Internet-Based Intervention to Prevent Depression in Emerging Adults. Prim Care Companion J Clin Psychiatry. 2007;9(5):346–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Voorhees BW EJ, Stuart S, Fogel J, Ford D,. Pilot study of a primary care depression prevention intervention for late Adolescents. Canadian Child and Adolescent Psychiatry Review. May 2005;14(2):40–43. [PMC free article] [PubMed] [Google Scholar]
- 18.Clarke G, Reid E, Eubanks D, et al. Overcoming depression on the Internet (ODIN): a randomized controlled trial of an Internet depression skills intervention program. J Med Internet Res. December 2002;4(3):E14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clarke GN. Adolescent use of web-based depression treatment programs. Portland, OR; 2002. [Google Scholar]
- 20.Clarke GN, Hornbrook M, Lynch F, et al. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Arch Gen Psychiatry. December 2001;58(12):1127–1134. [DOI] [PubMed] [Google Scholar]
- 21.Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. J Consult Clin Psychol. June 2006;74(3):401–415. [DOI] [PubMed] [Google Scholar]
- 22.Possel P, Horn AB, Groen G, Hautzinger M. School-based prevention of depressive symptoms in adolescents: a 6-month follow-up. J Am Acad Child Adolesc Psychiatry. August 2004;43(8):1003–1010. [DOI] [PubMed] [Google Scholar]
- 23.Johnson JG, Harris ES, Spitzer RL, Williams JB. The patient health questionnaire for adolescents: validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J Adolesc Health. March 2002;30(3):196–204. [DOI] [PubMed] [Google Scholar]
- 24.Lancaster T, Stead L. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2004(4):CD000165. [DOI] [PubMed] [Google Scholar]
- 25.Clarke GN. The coping wIth stress course adolescent: workbook. Portland, OR: Kaiser Permanente Center for Health Research; 1994. [Google Scholar]
- 26.Jacobson NS MC, Dimdjian S. Behavioral Activation Treatment for Depression: Returning to Contextual Roots. Clinical Psychology: Science and Practice. Fall 2001;8(3). [Google Scholar]
- 27.Mufson L DK, Moreau D, Weissman MM. Interpersonal Psychotherapy fo Depressed Adolescents. New York, New York: Guilford Press; 2004. [Google Scholar]
- 28.Stuart SRM. Interpersonal Psychotherapy A Clinicians Guide. New York, New York: Oxford University Press; 2003. [Google Scholar]
- 29.Bell CC. Cultivating resiliency in youth. J Adolesc Health. 2001;29(5):375–381. [DOI] [PubMed] [Google Scholar]
- 30.Nation M, Crusto C, Wandersman A, et al. What works in prevention. Principles of effective prevention programs. Am Psychol. 2003;58(6–7):449–456. [DOI] [PubMed] [Google Scholar]
- 31.Wandersman A, Florin P. Community interventions and effective prevention. Am Psychol. 2003;58(6–7):441–448. [DOI] [PubMed] [Google Scholar]
- 32.Gagne RMBL, Wager WW. Principles of Instructional Design. Fort Worth, TX: Harcourt Brace Jovanovich College Publishers; 1992. [Google Scholar]
- 33.Beardslee WR, Gladstone TR, Wright EJ, Cooper AB. A family-based approach to the prevention of depressive symptoms in children at risk: evidence of parental and child change. Pediatrics. 2003;112(2):e119–131. [DOI] [PubMed] [Google Scholar]
- 34.Bennett GA, Roberts HA, Vaughan TE, Gibbins JA, Rouse L. Evaluating a method of assessing competence in Motivational Interviewing: a study using simulated patients in the United Kingdom. Addict Behav. January 2007;32(1):69–79. [DOI] [PubMed] [Google Scholar]
- 35.Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149–166. [DOI] [PubMed] [Google Scholar]
- 36.Baron G, Ravaud P, Samson A, Giraudeau B. Missing data in randomized controlled trials of rheumatoid arthritis with radiographic outcomes: a simulation study. Arthritis Rheum. January 15 2008;59(1):25–31. [DOI] [PubMed] [Google Scholar]
- 37.Jaycox LH, Miranda J, Meredith LS, Duan N, Benjamin B, Wells K. Impact of a primary care quality improvement intervention on use of psychotherapy for depression. Ment Health Serv Res. 2003;5(2):109–120. [DOI] [PubMed] [Google Scholar]
- 38.McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction. January 2004;99(1):39–52. [DOI] [PubMed] [Google Scholar]
- 39.Erol S, Erdogan S. Application of a stage based motivational interviewing approach to adolescent smoking cessation: The Transtheoretical Model-based study. Patient Educ Couns. February 25 2008. [DOI] [PubMed] [Google Scholar]
- 40.Possel P, Baldus C, Horn AB, Groen G, Hautzinger M. Influence of general self-efficacy on the effects of a school-based universal primary prevention program of depressive symptoms in adolescents: a randomized and controlled follow-up study. J Child Psychol Psychiatry. September 2005;46(9):982–994. [DOI] [PubMed] [Google Scholar]
- 41.Horowitz JL, Garber J, Ciesla JA, Young JF, Mufson L. Prevention of depressive symptoms in adolescents: a randomized trial of cognitive-behavioral and interpersonal prevention programs. J Consult Clin Psychol. October 2007;75(5):693–706. [DOI] [PubMed] [Google Scholar]
- 42.Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention. Journal of American Academic Child and Adolescent Psychiatry. March 1995;34(3):312–321. [DOI] [PubMed] [Google Scholar]
- 43.Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res. January 2002;26(1):36–43. [PubMed] [Google Scholar]
- 44.Katon W, Rutter C, Ludman EJ, et al. A randomized trial of relapse prevention of depression in primary care. Arch Gen Psychiatry. 2001;58(3):241–247. [DOI] [PubMed] [Google Scholar]
- 45.Willemse GR, Smit F, Cuijpers P, Tiemens BG. Minimal-contact psychotherapy for sub-threshold depression in primary care. Randomised trial. Br J Psychiatry. 2004;185:416–421. [DOI] [PubMed] [Google Scholar]
- 46.Clarke G, Hawkins W, Murphy M, Sheeber L. School based primary prevention of depressive symptomology in adolescents: findings from two studies. School Psychology Quarterly. 1993;8(255–263). [Google Scholar]
- 47.Ambrosini PJ. Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS). J Am Acad Child Adolesc Psychiatry. 2000;39(1):49–58. [DOI] [PubMed] [Google Scholar]