Abstract
Cancer is one of the important causes of morbidity and mortality in India. Globally, out of 14 million diagnosed new cancer cases slightly more than 1 million were from India. Population Based Cancer Registries (PBCRs) plays a vital role in formulating cancer control plans as well as in monitoring their success. The article identifies challenges and opportunities for the PBCRs in India. Major challenges of PBCRs in India are-low coverage, urban dominance, quality assurance in data, less awareness among rural people, lack of follow-up and survival data, timeliness, high cost of registration, non-linkage of PBCR with other PBCRs and Hospital Based Cancer Registries (HBCRs) and generalization of estimates at country level. Expansion of cancer atlas project, real time data collection, entering Aadhar number (UID) during registration and establishing linkage among various PBCRs and PBCRs with HBCRs will improve cancer registration and its quality on a short-term basis. However, the opportunity of development new PBCRs in linkage with existing Health and Demographic Surveillance System (HDSS) will increase coverage as well as sustainability of PBCRs in India.
Keywords: Cancer, population based cancer registries (PBCRs), India
Introduction
Cancer is one of the important causes of morbidity and mortality in India. Globally, out of 14 million diagnosed new cancer cases slightly more than 1 million were from India (Mallath et al., 2014). Similarly, out of 8 million cancer deaths occurred worldwide, 700,000 cancer deaths occurred in India (Ferlay et al., 2015). According to the projection done by IARC, GLOBOCAN estimates that the cancer burden of India will nearly double in the next 20 years (Ferlay et al., 2015). Cancer incidence and mortality are rising rapidly worldwide, particularly in low and middle income countries. There is an overwhelming need for countries to adopt and implement cancer control actions. Yet only 1 in 5 low and middle income countries have the necessary data to drive policy (IARC GICR, 2018).
Cancer registries are key elements of a cancer control programme for data collection, analysis, interpretation and health policy implementation. It includes systemic collection, storage, analysis, interpretation and reporting of cancer related data. The two main types of cancer registry are Population Based Cancer Registries (PBCRs) and Hospital Based Cancer Registries (HBCRs). The Bombay Cancer Registry was first PBCR of India established by the Indian cancer society Bombay (now called Mumbai) in 1963 (Gajalakshmi et al., 2001). Mumbai (Tata memorial center) became the first IARC regional hub for Asia region in 2011. Three satellite registries, Pune (1972), Aurangabad (1978) and Nagpur (1983) were subsequently established at Maharashtra. Realizing cancer as significant public health problem, the National Cancer Registry Programme (NCRP) was commenced by the Indian Council of Medical Research (ICMR) with a network of cancer registries across the country in December 1981 (Gajalakshmi et al., 2001). It was started with three PBCRs at Bangalore, Chennai and Mumbai and three HBCRs at Chandigarh, Dibrugarh and Thiruvananthapuram. With recent establishment of new PBCRs at Patiala, Naharalagun, Pasighat, Noida and Silchar at present a total of 31 PBCRs and 29 HBCRs are functioning in India (NCDIR, 2016-17). HBCR in true sense is longitudinal clinical record of cancer patient information in a hospital. PBCR is responsible for collecting data on all new cancer cases in a well defined population. Hence, HBCRs are important in administrative and clinical functions. However; PBCRs can measure cancer incidence, its trend and mortality and have a unique role in planning and evaluating cancer control plans and reducing the cancer burden in the community (Bray et al., 2015).
Cancer registration in PBCRs
Purpose of PBCR is to record/capture all the cancer cases diagnosed in a clearly defined geographical area. Active case finding methods are used for the registration of the cancer cases. The denominator (population covered) for cancer registry is collected from census data. The data for cancers is collected from three major sources –hospitals/clinics, diagnostic departments (radiology and pathology) and from death certificates. Once the cancer patient is identified by the registry person, the address is verified first, if the patient resides in the area covered under PBCR then the detail data is taken. The desired information [personal identifiers, demographic variables, date of diagnosis, the most valid basis of diagnosis, tumor site and morphology, extent of disease and treatment (s) received captured] using a “common core proforma” which is a standardized format for all cancer registries. Matching is done to limit the overlapping of cancer cases from the three sources. Then, all the cancer cases are coded according to the International Classification of Diseases for Oncology (ICD-O) and data are entered into customized computerized database. The duplicates are removed for current year and previous years after sorting with sex, name, address and disease-wise. Quality control checks are used to improve the data quality. Standardization of population is done with world population. The morbidity and mortality indicators of cancers are estimated, tabulated and report is published (Figure 1).
Figure 1.
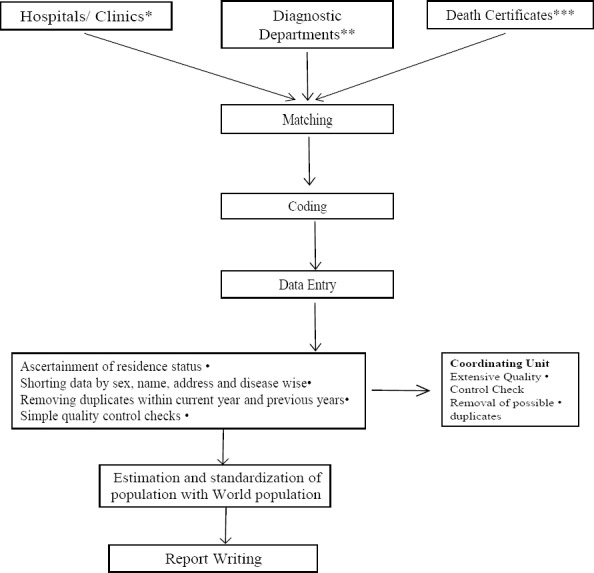
Flow- Diagram of Cancer Registration in PBCR. * Main Cancer Hospitals, Govt. Hospitals, Private Hospitals, Nursing Homes etc. ** Pathology labs and Radiology Department. *** from Vital Registration, local Municipality Corporation etc.
Challenges of PBCRs
The major challenges related to PBCRs are summarized in Panel-1.
Panel 1.
Challenges of PBCRs
| Low Coverage |
| Urban Dominance |
| Low awareness among rural population of India |
| Quality assurance for data |
| Lack of follow-up and survival data |
| Timeliness |
| High cost of registration in PBCRs |
| No linkage of PBCR with other PBCRs and HBCRs |
| Generalisation of estimates at country level (the data collected from existing PBCRs is not representative* of India) |
| Other pitfalls (Privacy and confidentiality, Political commitment and non-availability PBCRs data in public domain) |
The established PBCRs are unevenly distributed compared to population distribution and geographical diversity, for example, some populous state like Uttar Pradesh, Bihar, Andhra Pradesh, Rajasthan and Odisha have no PBCRs. Therefore, the sample, from which data are collected, is not representative of India.
Low Coverage
In the USA and Europe the number of PBCR has increased widely in the last four decades compared to Asia and Africa (Keshtmand and Zendehdel, 2011). There are 40% to 100% coverage of PBCR in high income countries, however the coverage hardly reaches 30% in low and middle income countries (Keshtmand and Zendehdel, 2011). Currently, there are more than 700 PBCRs (Bray et al., 2015) covering 21% (Parkin, 2006) of the world population, however, in India the coverage is only 10% (PBCR, 2018). The coverage is only 0.1% of the rural population of India (Gajalakshmi et al., 2001).Hence the data related to cancer are missing from large part the country.
Urban Dominance
More than two-third (68%) of the population lives in rural India (World Bank, 2015). In India, there are only two PBCRs which are currently covering only rural population and 11 PBCRs which cover both urban and rural populations (PBCR, 2018). The compiled data from PBCRs have urban dominance as majority of data is collected from urban area of India.
Low awareness among people in rural India
Cancer registrations in rural areas are more challenging. The people can die due to cancer without access to health care. The cause of mortality data is unavailable due to lack of medical certification of deaths (Chatterjee et al., 2016). Lack of awareness about the cancers remains the key. Distance from appropriate health services and lower socioeconomic classes add more to it. Hence, the under reporting cancer cases are common.
Lack of follow-up and survival data
The numerator for PBCRs should be interpreted with caution. Cancer registries document captures cancer events (hospital admission) rather than people who have cancer. In active follow-up, the registry contacts the persons regularly till the patient is alive. This is quite expensive and not practiced in India. Sometimes, there is passive follow-up in PBCRs and they are trying to match old cases to remove from death certificate. A person can suffer multiple primary cancers and registered multiple times in the registry database (Izquierdo and Schoenbach, 2000). The name is used as most common identifier. The name of a person may change when marriage occurs or due to any social reasons. There may be spelling mistake when a large proportion of the population is illiterate. This can be aggravated when the name is translated to English for entry in the database. When a patient visited multiple facilities for a second opinion, there is duplication of records. The subsequent report from different hospital may be recurrence of original tumor or new primary tumor in the same organ. Merging the information coming from diverse sources is tedious and difficult (Dos and Silva, 1999). Hence, it is essential to have inbuilt mechanism to avoid multiple registration and enable to link the concerned individual if entered again in the registry.
Quality assurance in data
In many Indian hospitals, the low quality medical records add more to the problem. Most of the time, the concerned registry staff has to go through all hospital records and death certificate to identify cancer cases as there is a lack of proper ICD-O and ICD-10 coding in many hospitals. The active home visit to identify the missing data for hospital cases and to interview the family members of patients diagnosed by “death certificate only” is still not practiced in most PBCRs of India. The way in which a registry operates depends, inevitably, on local conditions and on the material resources available. The data (cancer cases) collected from death record depends upon the quality and maintenance of death certificates. Few indicators of quality check- age unknown, unknown duration of stay, microscopic verification, and the clinical extent of disease before treatment, unspecified site/sub-site, and unspecified histology-are still far from good quality data (NCRP, 2018).
Timeliness
Timely reliable cancer incidence data are vital for cancer control program. In India, the publication of cancer registries report is often delayed. Currently, the NPCR-CDC and SEER have latest cancer information as of 2012 – 2014 (NCRP, 2018). There are gross differences even within registries especially with data coming from specialized and non-specialized medical institutions (Chatterjee et al., 2016). The lag period is due to lack of real time data collection and deficit in training staff at PBCRs (NCRP, 2018). There is a need to expand real time data collection and validation for all PBCRs.
High cost of registration in PBCRs
Setting of new cancer registries consumes enormous cost and the cost of registration through PBCRs is high, which lead to development of Cancer Atlas project (NCRP, 2001). Strengthening of departments of pathology, providing orientation and training in cancer registration, and online data entry with the help of web-based design were key feature of this project. Unlike the working of PBCRs, no systematic attempt was made to actively visit every diagnostic and treatment center (NCRP, 2001). Cancer Atlas was developed for whole Punjab state (NCRP, 2018). Currently, only Punjab and Haryana (NCRP, 2018) are covered under cancer atlas project and other PBCRs follow the conventional method of registration which had high cost.
No linkage of PBCR with other PBCRs and HBCRs
The data for cancers is collected from facilities, clinician or pathologist and from death certificates. Once the cancer patient is identified by the registry person, the address is verified first, if the patient resides in the area covered under PBCR then data was collected in core proforma. The data is not collected if the patient resides outside the area covered under PBCR. The opportunity is missed to be registered in PBCR due to lack of linkage among various cancer registries. Similarly, all the cancer cases registered under HBCRs is also not registered in PBCRs due to lack of linkage.
Validity/Generalization of estimates at country level
Currently the cancer incidence of the country is estimated from the compiled data of PBCRs. However, this is not a valid method of estimation because of the sample from which data is collected is not representative of India (Dhar, 2018). The established PBCRs are unevenly distributed compared to population distribution and geographical diversity, for example, some populous state like Uttar Pradesh, Bihar, Andhra Pradesh, Rajasthan and Odisha have no PBCRs (Chatterjee et al., 2016) Therefore, the sample, from which data are collected, is not representative of India.
Other pitfalls
Legislation related to data confidentiality and data protection with respect to cancer registration has already introduced in many countries (Coleman et al., 1992) There is a need to look into the confidentiality and privacy aspects of cancer registration in India. Political commitment and financing remains crosscutting issues for the development of PBCRs in India. In India, only 10% population (PBCR, 2018) is covered under PBCRs with the exception of Punjab state which is covered fully (100%) under PBCR (Punjab PBCR, 2013). Non-availability of PBCRs data in the public domain is the potential reason for the under-utilization of the data for research purposes (Dhar, 2018). On the other hand, there has been extensive utilization of data from other sources of health information (like, Census, SRS, NFHS, DLHS, etc.) owing to their availability in public domain (Dhar, 2018).
Opportunities
PBCRs provide vital inputs for cancer control activities. There is a growing requirement for the local planning and development of PBCRs. The ultimate goal being the scaling of PBCRs covering whole India. PBCRs must be established uniformly over the country, keeping in mind the population distribution and geographical diversity. The establishment and maintenance of new PBCRs require huge financial investment. The cost of registration per case under cancer atlas project was very low compared to case registration in PBCRs (NCRP, 2018). This huge deduction was mainly due to absence of active visit to every diagnostic and treatment center. That is where the linking of medical data from medical institutions, hospitals and cancer treatment centers with PBCRs comes of immense help. According to NCRP data, 85-90% of cancers have a microscopic diagnosis (NCRP, 2001). The expansion of cancer atlas projects covering all pathology and radiology department of medical colleges and major cancer hospitals is absolutely essential to improve cancer registration on a short-term basis.
Ensuring quality data, i.e. estimate of appropriate and unbiased burden of cancer with minimum cost is the crucial aspect for the development of PBCR. The opportunity of linking of PBCRs with Demographic Surveillance System (DSS) and Health and Demographic Surveillance System (HDSS) fulfills this. Health and Demographic Surveillance System (HDSS) have an existing robust mechanism which gathers longitudinal demographic and health data for a dynamic cohort of the total population in a specified geographic area. Sample Registration System (SRS) is a national level DSS system which measures birth, death and other fertility indicators along with the cause of death through verbal autopsies (SRS, Census of India., 2018). Continuous (longitudinal) enumeration of vital events and its half-yearly independent retrospective survey creates an ideal platform to collect the cancer morbidity and mortality data. Similarly, integration of Rural Health Training Centers (RHTCs) and Urban Health Training Canters (UHTCs) (Deshpande, 2015) with medical colleges having HDSS remains another potential for the establishment of PBCRs with little additional investment. RHTCs and UHTCs also should have the opportunity to train and teach the health professions which will help in the major development in cancer epidemiology. Sustainability is another key aspect of PBCRs that can be ensured if we explain the possibility of linking DSS with PBCR. Hence, a well functioning Cancer Surveillance Program (CSP) needs a linkage of cancer registry, especially the population registry with a programme level which is still lacking in India. There is a need to link the information generated from registry with policy formation. If cancer cases can be registered with their Aadhar number, Unique Identity Number (UID), of the patient, then it will strengthen the data base of PBCRs and minimize the multiple entry and quite helpful for removing the duplicates during matching stage and quality checks.
During an active visit to the hospitals, the data are not collected if the patient resides in the area which is not covered under PBCR. Hence the linkage among PBCRs will help to transfer the data to the existing other PBCR depending upon the residency. This will help to minimize the missing of cancer cases even if they avail treatment from distant part of the country. Availability of real time data will minimize errors and save time to a great extent. Also, a comprehensive account of various sources of registration is necessary to avoid repetition of registrations and to identify the number of cases with their residential address unknown.
Under the District Cancer Control Program, creating awareness about various cancers and screening of the patient is done at the district level and then the patients are referred to nearby wings of cancer hospital (241 hospitals) for treatment to bridge the geographical barrier.
The majority of cancer cases in India is diagnosed at their advanced stage. Therefore, mortality is high (Desai, 2002). Health education for the rural population and the creation of an infrastructure for cancer management is essential. Political commitment will play a key role in the improvement of existing PBCRs and establishment of new PBCRs. Availability of PBCRs data in the public domain will increase its utilization for research purposes.
To conclude, PBCRs are potentially a great asset for cancer epidemiology of India. Addressing the challenges of PBCRs will generate; locally relevant, appropriate cancer control plans which will further enable us to prepare feasible cancer control plans for the whole country.
References
- 1.Bray F, Znaor A, Cueva P, et al. IARC Technical Publication. Vol. 43. Lyon: IARC; 2015. Planning and developing population-based cancer registration in low- and middle-income settings. [PubMed] [Google Scholar]
- 2.Chatterjee S, Chattopadhyay A, Senapati SN, et al. Cancer registration in India- current scenario and future perspectives. Asian Pac J Cancer Prev. 2016;17:3687–96. [PubMed] [Google Scholar]
- 3.Coleman MP, Muir CS, Ménégoz F. Confidentiality in the cancer registry. Br J Cancer. 1992;66:1138–49. doi: 10.1038/bjc.1992.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Desai PB. Cancer control efforts in the Indian subcontinent. Jpn J Clin Oncol. 2002;32:13–6. doi: 10.1093/jjco/hye139. [DOI] [PubMed] [Google Scholar]
- 5.Deshpande SR. Rural and urban health training centres of medical colleges in India: A prescription for their revamp. Natl Med J India. 2015;28:141–3. [PubMed] [Google Scholar]
- 6.Dhar M. A critical review of evolution of cancer registration in India. J Tumor Med Prev. 2017;2:1–9. [Google Scholar]
- 7.Dos I, Silva S. Cancer epidemiology: Principle and methods. The role of cancer registries. International Agency for Research on Cancer, 150 cours Albert Thomas, 69372 Lyon cédex 08, France Numbers. 1999:385–403. [Google Scholar]
- 8.Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortalityworldwide: sources, methods and major patterns in Globocan 2012. Int J Cancer. 2015;136:359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 9.Gajalakshmi V, Shanta V, Swaminathan R. Cancer registration in India. Asian Pac J Cancer Prev. 2001;2:13–20. [PubMed] [Google Scholar]
- 10.IARC. Global initiative for cancer registry development, making cancer data count. WWW page. 2018. [Last accessed July 19 2018]. URL: http://gicr.iarc.fr/
- 11.Izquierdo JN, Schoenbach VJ. The potential and limitations of data from population-based state cancer registries. Am J Public Health. 2000;90:695–8. doi: 10.2105/ajph.90.5.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keshtmand G, Zendehdel K. Fostering population-based cancer registries in developing countries. Basic Clin Cancer Res. 2011;3:5–13. [Google Scholar]
- 13.Mallath MK, Taylor DG, Badwe RA, et al. The growing burden of cancer in India: epidemiology and social context. Lancet Oncol. 2014;15:205–12. doi: 10.1016/S1470-2045(14)70115-9. [DOI] [PubMed] [Google Scholar]
- 14.National cancer registry programme. Development of an atlas of cancer in India. WWW page. 2001. [Last accessed July 19, 2018]. URL: http://www.ncdirindia.org/ncrp/ca/about.aspx#top .
- 15.National cancer registry programme. Three-year report of population based cancer registries 2012-2014 WWW page. 2016. [Last accessed July 19, 2018]. URL: http://ncdirindia.org .
- 16.NCDIR, Indian Council of Medical Research. Annual report (2016-17) WWW page. [Last accessed July 19, 2018]. URL: http://www.ncdirindia.org .
- 17.National cancer registry programme. WWW page. 2018. [Last accessed July 19, 2018]. URL: http://www.ncrpindia.org .
- 18.Parkin DM. The evolution of the population-based cancer registry. Nat Rev Cancer. 2006;6:603–12. doi: 10.1038/nrc1948. [DOI] [PubMed] [Google Scholar]
- 19.PBCR Home. WWW page. 2018. [Last accessed July 19, 2018]. URL: http://www.pbcrindia.org/
- 20.Population based cancer registries at Chandigarh and SAS Nagar, Sangrur, Mansa Districts Punjab State, India. Cancer burden in Chandigarh and Punjab state first year report (2013). WWW page. [Last accessed July 19, 2018]. URL: http://pbhealth.gov.in .
- 21.Sample registration, census of India. WWW page. 2018. [Last accessed July 19, 2018]. URL: http://censusindia.gov.in .
- 22.World bank rural population data. WWW page. 2015. [Last accessed 11 Jan 2018]. URL: http://data.worldbank.org/indicator/SP.RUR.TOTL.ZS .


