Abstract
In light of the growing antibiotic resistance, the usage of plant-derived antimicrobial agents could serve as an effective alternative treatment against oral infections. The aim of this study was to investigate the antimicrobial and antibiofilm activity of Mediterranean herb extracts against representative oral microorganisms. The extraction procedures and the analysis of the obtained extracts were performed under established experimental conditions. The minimum inhibitory (MIC) and bactericidal (MBC) concentrations of the methanol extracts of Cistus creticus ssp. creticus, Cistus monspeliensis, Origanum vulgare, Rosmarinus officinalis, Salvia sclarea and Thymus longicaulis against eight typical oral bacteria and the fungus Candida albicans were determined. The antibiofilm activity against Streptococcus mutans was also quantified using the microtiter plate test. Overall, all tested extracts inhibited effectively the screened obligate anaerobic microorganisms and in concentrations ≥0.3 mg ml-1 had moderate to high antibiofilm activity comparable to that of chlorhexidine (CHX) against S. mutans. In particular, R. officinalis (MIC: 0.08–5.00 mg ml-1) and S. sclarea (MIC: 0.08–2.50 mg ml-1) showed the highest antibacterial activity, while Cistus spp., R. officinalis and S. sclarea significantly inhibited S. mutans biofilm formation at 0.60, 1.25 and 2.50 mg ml-1, respectively. Porphyromonas gingivalis and Parvimonas micra were high susceptible to O. vulgare (MIC = 0.30 mg ml-1), whereas T. longicaulis eradicated all oral bacteria (MBC: 0.15–2.50 mg ml-1). Nevertheless, C. albicans showed no sensitivity to the tested extracts. In conclusion, the tested plant extracts could serve as alternative natural antibacterial and antibiofilm components against oral infections.
Introduction
The statement of Hippocrates “Natural forces are the true healers of disease” reflects the fact that thousands of years before any synthetic medicaments were known, nature had been widely considered as the only limitless source of healing components. The ultimate intention has always been to use natural products with favorable antimicrobial, anti-inflammatory and antitumoral properties, without side effects at the chosen concentration, for medicinal purposes. Recently, we have therefore seen diverse plant extracts as well as pure natural compounds as part of various treatment protocols in daily medicinal use [1–5]. Especially plant extracts originating from the Mediterranean area belong to the most frequently screened natural resources for application in medicine [6–8].
Although almost about 350,000 plant species have been characterized to date, thousands of unexplored plant species need to be studied for their chemical or biological profile and thus, their potential as a non-pharmacological intervention for diverse diseases [9]. Following the evolution of all living organisms, plants have nowadays developed their own molecular antimicrobial strategies to survive, by producing secondary metabolites with synergistic action such as small antimicrobial peptides, alkaloids, coumarins, flavonoids, phenols, phenolic acids, quinones, saponins, tannins and terpenoids [10, 11]. For instance, the two main components of Origanum vulgare, namely thymol and carvacrol, present synergistic activity against Streptococcus mutans, Streptococcus mitis, Prevotella oris, Prevotella intermedia, Micrococcus luteus and others [12, 13].
Surprisingly, according to a recent review by Sender et al. the ratio between bacterial and host cells in humans is approximately 1:1 [14]. In particular, the oral cavity hosts 700 to 1000 different bacterial species mostly situated on both soft and hard tissues, e.g. teeth, gingiva, tongue, cheeks and palate [15]. Thus, bacterial diseases in oral cavity are more likely polymicrobial infections which etiologically correlate with caries, pulpitis, gingivitis and periodontitis [16]. The complex oral microbial communities are mainly organized in biofilms. During the initial phase of oral biofilm formation, the salivary pellicle is mainly colonized among others by Streptococcus spp., which bind with their receptors to host proteins like α-amylase, immunoglobulins, fibronectin, lactoferrin and α2-macroglobulin [17, 18]. It was shown that S. mutans strains in biofilms are up to 70,000 times more acid tolerant than their planktonic counterparts [19].
Taking the constantly increasing ineffectiveness of antibiotics into consideration, the necessity to develop new efficient treatment strategies against oral diseases has raised interest in natural products. For instance, nosocomial infections caused by Acinetobacter baumannii need an alternative treatment as carbapenem resistances have raised. The plant Scutellaria baicalensis seems to have one promising compound named norwogonin which showed antibacterial effects against A. baumannii [20] and Actinidia deliciosa methanol extract reduced its production of bacterial biofilm components [21]. Because of their secondary metabolism, natural products such as plants yield chemical reactions with significant pharmaceutical effects on various microorganisms. As a result, numerous natural extracts or their main compounds have been screened all over the world, indicating that herbs can improve the oral health [22]. Various plant products such as coffee, grape, cranberry juice, tea (green-, cistus-, black tea) have been tested for their potential to treat caries, periodontitis and periimplantitis [23, 24]. Especially Mediterranean herbs seem to have a high efficacy against representative oral microorganisms [24, 25].
Thus, the goal of the present report was to examine the antimicrobial and antibiofilm activity of six Mediterranean natural herb extracts against representative oral microorganisms in vitro. More precisely, the methanol extracts of Cistus creticus ssp. creticus, Cistus monspeliensis, Origanum vulgare, Rosmarinus officinalis, Salvia sclarea and Thymus longicaulis were tested against eight typical oral pathogenic microorganisms and the fungus Candida albicans. Additionally, two reference strains, namely Staphylococcus aureus and Escherichia coli, residents on skin and intestinal mucosa, respectively, were investigated. The antibiofilm effect of the extracts against Streptococcus mutans was also examined. Hence, three antimicrobial assays were applied: the minimal inhibitory concentration (MIC) assay, the minimal bactericidal concentration (MBC) assay and the biofilm plate assay. The null hypothesis was assumed that the tested extracts have no significant antimicrobial and antibiofilm impact on the screened microbial species.
Materials and methods
Extraction process
Aerial plant parts of the six different plant species were collected from various places of the Greek periphery. Cistus creticus L. (Cistaceae, Lat.: 35o 23′17.76″ N, Long.: 24o 54′50.89″ E, Elevation: 181 m) and Cistus monspeliensis L. (Cistaceae, Lat.: 35o 17′29.13″ N, Long.: 25o 32′15.33″ E, Elevation: 63 m) were collected from Crete, Origanum vulgare L. (Lamiaceae, Lat.: 37o 16′42.22″ N, Long.: 22o 40′34.36″ E, Elevation: 599 m) from Peloponnese, Rosmarinus officinalis L. (Lamiaceae, Lat.: 37o 58′07.98″ N, Long.: 23o 47′11.34″ E, Elevation: 253 m) and Thymus longicaulis C. Presl. (Lamiaceae, Lat.: 38o 11′02.26″ N, Long.: 23o 15′19.86″ E, Elevation: 1361 m) from Attiki and Salvia sclarea L. (Lamiaceae, Lat.: 39o 52′54.37″ N, Long.: 20o 38′01.89″ E, Elevation: 449 m) from Epirus. The collection sites were on public land. The University of Athens, being a public Institute, reserves the right to collect a small amount of plants for research purposes. No permits or permissions were required to collect samples from these public land areas. A small amount was collected for the needs of the investigation and the plants were not endangered or protected species. A voucher specimen of each plant is deposited at the herbarium of the Department of Pharmacognosy and Natural Products Chemistry, Faculty of Pharmacy, National and Kapodistrian University of Athens under the following numbers: C. creticus—KL 057, C. monspeliensis—KL 060, O. vulgare—F 009, R. officinalis—KL 163, T. longicaulis—P-K 011, S. sclarea–In 023. Collected plants were grinded (SCIS, Allenwest-Eac ltd) into fine homogeneous powders and extracted with ultrasound assisted the extraction (UAE). An Elma S 100H (Elmasonic) instrument was used with methanol (100%) as extraction solvent for 15 min at room temperature and ratio plant per solvent 1/10 (w/v). Extraction procedure was repeated twice for each sample. Methanol was evaporated to dryness under reduced pressure using a rotary evaporator (Buchi Rotavapor R-200) at 40°C.
High performance thin layer chromatography (HPTLC) analysis
A Camag HPTLC instrumental setup was used for generating the fingerprinting of the various extracts. Extracts’ solutions were prepared by dissolving 10 mg of each extract in 1 ml of methanol. The samples of the plant extracts were applied onto 20 × 10 cm TLC plates (silica gel 60, F254, Merck) using the Automatic TLC sampler (ATS4, CAMAG) under the control of the software platform VisionCats 2.3 (Camag) with the following standard settings: 6 tracks with 8 mm bands, 8 mm distance from the lower edge, 20 mm from the left and right edges, and 10.4 mm between the different tracks. The application volume of the samples was 8 μl. The plates were developed with an automatic development chamber (ADC2) using standard settings: 20 min chamber saturation with filter paper, 10 min of plate conditioning at 33% relative humidity (MgCl2) and 5 min of plate drying. Dichloromethane, methanol, water (70:30:4; v/v/v) and ethyl acetate, methanol, formic acid, water (50:10:7:1; v/v/v/v) were used as the mobile phases. Images at 254 nm and 366 nm were recorded on a Visualizer 2 Documentation System (CAMAG, Muttenz, Switzerland).
UPLC-HRMS & HRMS/MS analysis
UPLC-HRMS/MS analysis was performed on an AQUITY system (Waters) connected to a LTQ-OrbitrapR XL hybrid mass spectrometer (Thermo Scientific) equipped with an electrospray ionization (ESI) source and operated in negative mode. A UPLC separation gradient was developed in order to efficiently resolve all compounds for a qualitative analysis. The flow rate was set at 0.4 ml min-1 and the solvent system was (A) water 0.1% formic acid and (B) acetonitrile. The elution program was: 2% B for 2 min; 100% B in 18 min; and hold for 2 min. After return back to 2% B in 1 min, column equilibration was performed for 4 min at the end of the run. The injection volume was set to 10 μl and samples were injected at 0.3 mg ml-1 in water-acetonitrile solution (1:1) on a Supelco Ascentis Express C18 (100 x 2.1 mm i.d, 2.7 μm particle size). The HRMS & HRMS/MS data were acquired in negative mode over 100–1000 m/z range. The MS profile was recorded in full scan mode (scan time = 1 micro scans and maximum inject time = 500 ms). The ESI conditions were as follow: capillary temperature 320°C; capillary voltage -40 V; tube lens -120 V; ESI voltage 2.7 kV. Nitrogen was used as sheath gas (40 Au) and auxiliary gas (8 Au). For the HRMS/MS acquisitions, a data-dependent method including the detection (full scan) and fragmentation of the 3 most intense peaks per scan was used. The mass resolving power was 30,000 for both levels and the normalised collision energy (CID) in the ion trap was set to 35.0% (q = 0.25) for the HRMS/MS experiments. Chromatographic and spectrometric features were used for identification of extracts constituents such as retention time (Rt), polarity, accurate m/z, proposed elemental composition (EC), ring double bond equivalent (RDBeq) values as well as HRMS/MS spectra and derived fragmentation motifs. The raw data were acquired and processed with XCalibur 2.2.4 software from Thermo Scientific.
Bacterial and fungal strains
Ten bacterial strains and one C. albicans strain were selected. Eight of the tested bacterial strains and C. albicans are typical residents of the oral cavity. S. aureus and E. coli, in contrast, can be mainly detected on skin and within the intestinal flora, respectively, and served as reference species. Among the selected strains, Streptococcus mutans DSM (German Collection of Microorganisms and Cell Cultures) 20523, Streptococcus sobrinus DSM 20381, Streptococcus oralis ATCC 35037, Enterococcus faecalis ATCC 29212 and S. aureus ATCC 25923 are facultative anaerobic Gram-positive species, whereas E. coli ATCC 25922 is facultative anaerobic but it has a Gram-negative cell wall. Porphyromonas gingivalis W381, Prevotella intermedia MSP34 (clinical isolate), Fusobacterium nucleatum ATCC 25586 and Parvimonas micra ATCC 23195 are obligate anaerobic bacteria. The only used fungus C. albicans DSM 1386 grows both as yeast and filamentous cells. All bacterial and fungal strains were kindly supplied by the Division of Infectious Diseases and the Institute of Medical Microbiology and Hygiene, Faculty of Medicine, University of Freiburg. The microorganisms were deposited at -80°C in basic growth medium containing 15% (v/v) glycerol until their use as formerly described by Jones et al. [26].
Determination of the minimum inhibitory concentration (MIC)
Firstly, an overnight culture of each bacterial and fungal strain was prepared according to the guidelines of Clinical and Laboratory Standards Institute (CLSI) [27, 28]. Each microorganism was plated on Columbia blood agar plates (CBA) or yeast-cysteine blood agar plates (HCB). Facultative anaerobic bacteria and C. albicans were incubated on CBA at 37°C and 5–10% CO2 atmosphere for 24 h. The anaerobic bacteria were plated on HCB at 37°C for 48 h (anaerobic chamber, Anaerocult, Merck Chemicals GmbH, Darmstadt, Germany). A 0.5 / 1 McFarland standard suspension was prepared in 0.9% saline (NaCl) for facultative anaerobic bacteria and C. albicans, respectively. For the microdilution assay, all facultative anaerobic strains and C. albicans were then 1:10 diluted in BBL Mueller Hinton II Broth (Cation-Adjusted) (MHB, BD, Heidelberg, Germany). The anaerobic bacteria were set in Wilkins-Chalgren broth (WCB) as a 0.5 McFarland standard suspension. As previously described (ISO 20776–1: 2006 [29]), the cell density of facultative anaerobic bacteria, fungi and obligate anaerobic bacteria should be about 5 x 105, 5 x 104 and 5 x 106 colony forming units (CFU) per ml, respectively. Afterwards, appropriate volumes of the MHB / WCB microbial cultures were transferred into a 96-well microtiter-plate using a multi-channel pipette.
Preparation of extracts and procedure for MIC testing
The produced natural plant extracts were dissolved in dimethyl sulfoxide (DMSO, Sigma-Aldrich Chemie GmbH, Steinheim, Germany) at a concentration of 100 mg ml-1. All extract solutions in DMSO were screened in a concentration series ranging from 10 mg ml-1 to 0.02 mg ml-1 at dilution levels starting from 10-fold to 5120-fold. Each well of the 96-well microtiter-plate had a total volume of 100 μl. In order to exclude potential antimicrobial effects of the DMSO residuals, a dilution series of DMSO was examined in parallel. Wells containing solely MHB / WCB and a dilution series of 0.1% chlorhexidine (CHX) served as negative and positive controls for bacterial growth, respectively. Additionally, wells containing MHB / WCB and the added microbial strain acted as growth controls. The possibility of contamination was minimized by using sterile MHB / WCB. Thereafter, E. coli, S. aureus, E. faecalis and C. albicans were incubated at 37°C for 18 h, the three streptococci strains at 37°C under 5–10% CO2 atmosphere for 24 h, while anaerobic bacteria were kept at 37°C for 48 h in anaerobic incubation bags (Anaerocult IS, Merck Chemicals GmbH, Darmstadt, Germany). All assays for each bacterial and fungal strain were performed at least in duplicate. The highest MIC values were taken into consideration in case the MIC values of a specific strain were not identical. If the deviation between the two rows showed more than two dilution levels the determination with this extract was repeated. MIC was defined as the lowest concentration of each natural plant extract at which visible inhibition of bacterial growth was induced. The inhibitory impact of DMSO was taken into consideration if bacterial growth was observed in the co-tested DMSO dilution series.
Determination of the minimum bactericidal concentration (MBC)
The minimum bactericidal concentration (MBC) was also assessed according to the CLSI guidelines [27, 28]. After completion of the MIC assay, the 96-well microtiter-plates were further incubated for MBC testing. In brief, 10 μl from each well containing the tested plant extract concentration series were plated on CBA or HCB. In particular, E. coli, S. aureus and E. faecalis were plated on CBA at 37°C for 24 h, streptococci and C. albicans were incubated on CBA at 37°C and 5–10% CO2 atmosphere for two days. The obligate anaerobes were cultivated on HCB at 37°C for five days. To create anaerobic conditions an anaerobic jar and the Anaerocult. A gas generator system (Merck, Darmstadt, Germany) were used. Finally, the CFU were determined visually. The MBC was defined as the concentration at which a three Log decrease in bacterial growth (= 99.9% inhibition) was detected compared to the growth control.
Biofilm plate assay
The biofilm formation test was performed as already described by Al-Ahmad et al. [30]. Initially, a bacterial strain of S. mutans R15-8 (clinical isolate) was cultivated overnight at 37°C under aerobic conditions with 5–10% CO2 in MHB (BD, Heidelberg, Germany) containing 1% saccharose (MHB-S). Polystyrene 96-well tissue-culture plates (Greiner bio-one, Frickenhausen, Germany) were then filled with 100 μl of MHB-S, including ten different concentrations (0.02–10 mg ml-1) of the investigated plant extracts, and 5 μl of the S. mutans overnight culture (108 CFU ml-1) were added to each well. A dilution series of DMSO was examined in parallel. Wells containing solely MHB-S and a dilution series of 0.2% chlorhexidine (CHX) served as negative and positive controls for bacterial growth, respectively. Thereafter, the 96-well plates were incubated for 48 h at 37°C in an aerobic atmosphere with 5–10% CO2. The culture medium was then discarded, and the wells were washed three times with 300 ml phosphate-buffered saline (PBS, Life Technologies, Darmstadt, Germany) per plate to remove non-adherent bacteria. The plates were then air dried and stained with Carbol Gentian Violet solution (Carl Roth GmbH + Co. KG, Karlsruhe, Germany) for microscopy, containing 0.1-<0.25% methyl violet, for 10 min. Excess stain was removed by rinsing the plates with distilled water. Afterwards, the plates were dried for 10 min at 60°C and after dye resolubilization by adding 50 μl of absolute ethanol (99.9% v/v) for analysis (Merck Chemicals GmbH, Darmstadt, Germany) in each well, the optical density was finally measured at 595 nm using the Tecan Infinite 200 plate reader (Tecan, Crailsheim, Germany). All tests were conducted in quadruplicate and the mean values were determined. During the analysis, the antibiofilm effect of each extract on S. mutans was categorized in three different groups with the aid of two different cut-off values: no biofilm production or C1, moderate biofilm production or C2, and high biofilm production or C3. The low cut-off value was estimated by adding three standard deviations of the blank to the negative control. The high cut-off value resulted after the measurement of the low cut-off value for three times.
Statistical analysis
For a descriptive data analysis, the means and standard deviations regarding the optical density (OD) were computed. A two-sample t test was used for pairwise group comparisons between the plant extracts and the controls, namely CHX (positive control) and DMSO (negative control). Scatter plots of the OD values reflecting the level of biofilm inhibition by the plant extracts (low, moderate, high) were finally graphically demonstrated. All calculations were done with the statistical software STATA 14.1.
Results
Phytochemical investigation of the plant species
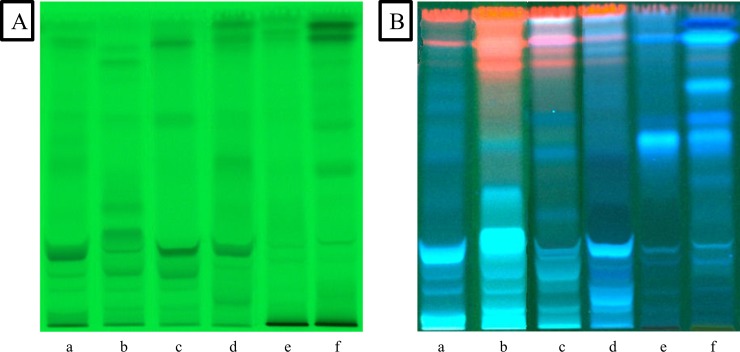
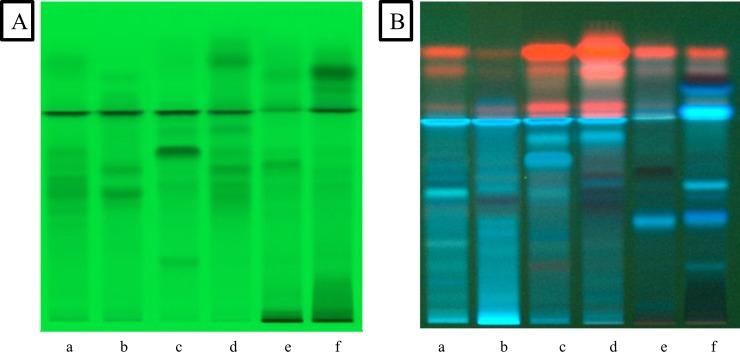
The plants were extracted with methanol using the exhaustive and efficient ultrasound assisted extraction method. For a preliminary phytochemical fingerprinting of the extracts a method was developed with the aid of Camag HPTLC instrumentation. The HPTLC analysis showed that the methanol extracts of the aerial parts of the studied plants contained several bioactive compounds. Two different mobile phases were selected in order to get a better image of the compounds. Visualization of the plates was performed at 254 nm and 366 nm. The chromatograms (Figs 1A–1D and 2A–2D) showed spots, which are characteristic for several Lamiaceae species. In particular, phenolic acids and in particular rosmarinic acid appear as intense fluorescent blue spots in all four plant species (O. vulgare, R. officinalis, T. longicaulis and S. sclarea), while absorbance at 254 nm is typical of flavonoids. The two other plant species belong to the Cistaceae family (C. creticus ssp. creticus and C. monspeliensis). As shown in the HPTLC (Figs 1E, 1F, 2E and 2F), evident is the presence of tannins and some phenolic compounds.
Fig 1.
HPTLC chromatograms of (a) R. officinalis, (b) S. sclarea, (c) O. vulgare, (d) T. longicaulis, (e) C. creticus and (f) C. monspeliensis at 254 nm (A) and 366 nm (B) (mobile phase dichloromethane, methanol, water (70:30:4; v/v/v)).
Fig 2.
HPTLC chromatograms of (a) R. officinalis, (b) S. sclarea, (c) O. vulgare, (d) T. longicaulis, (e) C. creticus and (f) C. monspeliensis at 254 nm (A) and 366 nm (B) (mobile phase ethyl acetate, methanol, formic acid, water (50:10:7:1; v/v/v/v)).
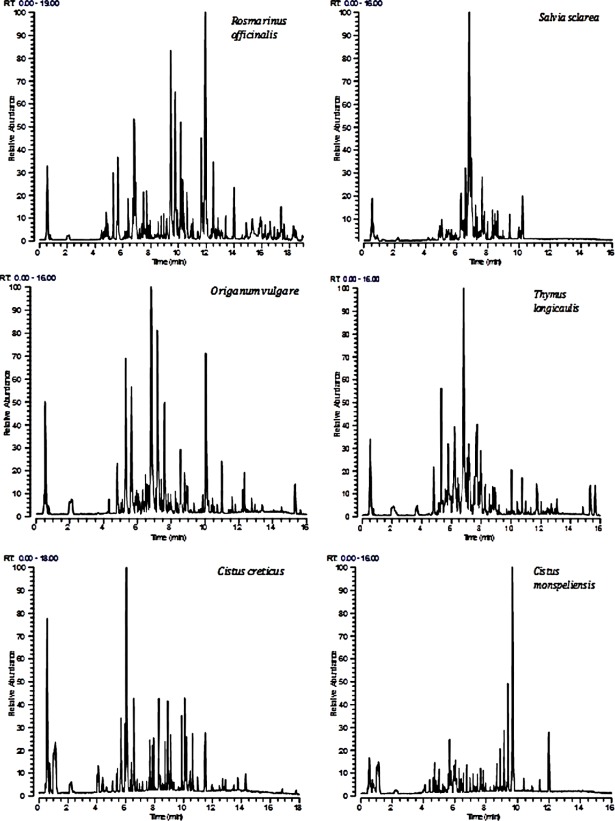
Since the methanol extracts were particularly rich in metabolites of various classes of compounds a more comprehensive characterization of chemical composition of extracts was conducted by LC-HRMS. The methanol extracts were also analyzed by UPLC-ESI-HRMS in order to identify the active compounds of the extracts. Tables 1–6 summarize all the compounds characterized in the above extracts, including retention times (Rt), elemental composition of the detected ions (EC [M-H]-), experimental and theoretical m/z, Delta value (Δm, ppm), rings and double bonds equivalent (RDBeq), MS/MS fragments and identification of putative compounds. Metabolites were assigned by interpreting the mass spectra determined through their MS and MS/MS, taking into account all the data provided by literature [31–42]. Thus, a total of 183 compounds, among them a lot in common in all six extracts, belonging to various metabolite classes, were qualitatively characterized. Forty compounds were detected in R. officinalis, belonging to phenolic acids, flavonoids and triterpenic acids. 7-Methoxyrosmanol, rosmanol isomers and rosmarinic acid were the main metabolites in the methanol extract. Rosmarinic acid was also the major metabolite in the extract of S. sclarea while various flavonoids were also present. Flavonoids and phenolic acids were identified in the extract of O. vulgare. Rosmarinic acid was also in this extract the main metabolite along with salvianolic acids. T. longicaulis was rich in flavonoids and triterpenic acids, while in this extract rosmarinic acid was also the main metabolite. Cistus spp. were particularly rich in phenolic compounds and especially flavonoids. Quercetin 3-O-β-D-glucopyranoside was the major compound in C. creticus. In C. monspeliensis diterpenes were also detected in the methanol extract with cistodioic acid being the major compound. Fig 3 shows the base peak chromatograms (BPCs) of the analyzed extracts.
Table 1. LC(ESI-)HRMS of R. officinalis methanol extract.
| No | Rt (min) |
EC [M-H]- |
Experimental | Theoretical | Δm ppm | RDBeq | Fragments MSMS (m/z) | Category of compound (Identification) |
|---|---|---|---|---|---|---|---|---|
| [M-H]- m/z | ||||||||
| 1 | 0.55 | C7H11O6 | 191.0563 | 191.05614 | 1.01 | 2.5 | 93, 127 | Quinic acid |
| 2 | 2.06 | C9H9O5 | 197.0454 | 197.0455 | -0.53 | 5.5 | 135, 179 | Syringic acid |
| 3 | 5.10 | C8H7O4 | 167.0350 | 167.0350 | 0.49 | 5.5 | 146, 160 | Vanilic acid |
| 4 | 4.64 | C16H17O9 | 353.0871 | 353.0878 | -1.91 | 8.5 | 173, 179 | Chlorogenic acid (Isomer 1) |
| 5 | 4.90 | C16H17O9 | 353.0871 | 353.0878 | -1.91 | 8.5 | nd | Chlorogenic acid (Isomer 2) |
| 6 | 5.06 | C20H27O12 | 459.1501 | 459.1508 | -1.62 | 7.5 | 287, 196, 309, 167, 127 | Paeonolide |
| 7 | 5.63 | C12H17O4 | 225.1132 | 225.1132 | 0.014 | 4.5 | 179 | 12-Hydroxyjasmonic acid |
| 8 | 5.79 | C21H19O12 | 463.0874 | 463.0882 | -1.78 | 12.5 | 419 | 6-Hydroxyluteolin-7-glucoside |
| 9 | 6.0 | C24H25O13 | 521.1295 | 521.1301 | -1.16 | 12.5 | 359 | Rosmarinic acid-3-D-glucoside |
| 10 | 6.10 | C27H29O15 | 593.1506 | 593.1512 | -0.94 | 13.5 | 473, 353, 503, 196 | Luteolin-7-O-rutinoside |
| 11 | 6.37 | C22H21O12 | 477.1036 | 477.1038 | -0.50 | 12.5 | 315, 197, 179,135 | Nepitrin |
| 12 | 6.65 | C22H19O10 | 431.0977 | 431.09784 | -1.44 | 12.5 | 269 | Apigenin-7-O-glucoside |
| 13 | 6.71 | C28H33O15 | 609.1821 | 609.1825 | -0.69 | 12.5 | 461 | Hesperidin |
| 14 | 6.78 | C18H15O8 | 359.0772 | 359.0772 | -0.1 | 11.5 | 161, 179, 197, 135 | Rosmarinic acid |
| 15 | 6.92 | C21H17O12 | 461.0724 | 461.0725 | -0.21 | 13.5 | 285 | Luteolin-3-glucuronide |
| 16 | 7.18 | C27H33O12 | 549.1973 | 549.1977 | -0.77 | 11.5 | 218, 475, 359 | Eucommin A |
| 17 | 7.23 | C29H25O14 | 597.1244 | 597.1250 | -0.98 | 17.5 | 555 | Pterogynoside |
| 18 | 7.43 | C32H29O15 | 653.1501 | 653.1512 | -1.60 | 18.5 | 503, 593, 331 | Feruloylnepitrin |
| 19 | 7.47 | C23H19O13 | 503.0829 | 503.0831 | -0.39 | 14.5 | 285, 399 | Luteolin-3′-O-(2″-O-acetyl)-β-D glucuronide (Isomer 1) |
| 20 | 7.61 | C15H9O6 | 285.0402 | 285.0405 | -0.94 | 11.5 | 146, 190, 262 | Luteolin |
| 21 | 7.73 | C23H19O13 | 503.0827 | 503.0831 | -0.75 | 14.5 | 285, 399 | Luteolin-3′-O-(2″-O-acetyl)-β-D glucuronide (Isomer 2) |
| 22 | 7.97 | C9H7O4 | 179.0352 | 179.0350 | 1.14 | 6.5 | 135, 160 | Caffeic acid |
| 23 | 8.29 | C15H9O5 | 269.0452 | 269.0455 | -1.30 | 11.5 | nd | Apigenin |
| 24 | 8.43 | C16H11O6 | 299.0558 | 299.05561 | -0.98 | 11.5 | 179 | Diosmetin |
| 25 | 9.40 | C17H13O6 | 313.0716 | 313.0718 | -0.63 | 11.5 | nd | Cirsimaritin |
| 26 | 9.43 | C20H25O5 | 345.1708 | 345.1707 | 0.08 | 8.5 | 301, 283 | Rosmanol (Isomer 1) |
| 27 | 9.79 | C20H25O5 | 345.1706 | 345.1707 | -0.35 | 8.5 | 283 | Rosmanol (Isomer 2) |
| 28 | 10.16 | C20H25O5 | 345.1708 | 345.1707 | 0.08 | 8.5 | nd | Rosmanol (Isomer 3) |
| 29 | 11.79 | C19H23O3 | 299.1651 | 299.1653 | -0.66 | 8.5 | 284 | Miltipolone |
| 30 | 11.95 | C21H27O5 | 359.1863 | 359.1864 | -0.24 | 8.5 | 315, 287, 196, 272, 167 | 7-Methoxyrosmanol |
| 31 | 12.52 | C20H23O5 | 343.1549 | 343.1551 | -0.46 | 9.5 | 325, 300, 287, 196, 315 | Rosmadial |
| 32 | 12.82 | C20H27O4 | 331.1912 | 331.1915 | -0.87 | 7.5 | nd | Carnosic acid |
| 33 | 12.84 | C20H27O3 | 315.1963 | 315.1966 | -0.78 | 7.5 | 287, 196, 167 | Rosmaridiphenol |
| 34 | 12.94 | C30H47O4 | 471.3477 | 471.3480 | -0.49 | 7.5 | 287, 196, 453, 287, 196, 167 | Anemosapogenin |
| 35 | 13.50 | C30H47O4 | 471.3476 | 471.3480 | -0.82 | 7.5 | 194, 116, 329 | Augustic acid |
| 36 | 14.01 | C21H29O4 | 345.2068 | 345.2071 | -0,91 | 7.5 | 301, 286 | Methyl carnosate |
| 37 | 15.28 | C30H47O3 | 455.3527 | 455.3531 | -0.82 | 7.5 | 452 | Betulinic acid |
| 38 | 15.32 | C30H47O3 | 455.3524 | 455.3531 | -1.43 | 7.5 | 407 | Oleanolic acid |
| 39 | 15.34 | C30H47O3 | 455.3528 | 455.3531 | -0.62 | 7.5 | 453 | Ursolic acid |
| 40 | 16.27 | C30H45O3 | 453.3369 | 453.3374 | -1.11 | 8.5 | nd | Micromeric acid |
| 41 | 18.23 | C30H47O4 | 471.3474 | 471.3480 | -0.49 | 8.5 | 467 | Benthamic acid |
Table 6. LC(ESI-)HRMS of C. monspeliensis methanol extract.
| No | Rt (min) |
EC [M-H]- |
Experimental | Theoretical | Δm ppm | RDBeq | Fragments MSMS (m/z) |
Category of compound (Identification) |
|---|---|---|---|---|---|---|---|---|
| [M-H]- m/z | ||||||||
| 1 | 0.56 | C7H11O6 | 191.0562 | 191.0561 | 0.61 | 2.5 | 173, 127, 85 | Quinic acid |
| 2 | 0.69 | C7H9O5 | 173.0456 | 173.0455 | 0.18 | 3.5 | nd | Shikimic acid |
| 3 | 1.15 | C13H15O10 | 331.0667 | 331.0671 | 0.57 | 5.5 | nd | Glucogallin |
| 4 | 1.08 | C7H5O5 | 169.0143 | 169.0142 | 0.57 | 5.5 | 125 | Gallic acid |
| 5 | 2.19 | C7H5O4 | 153.0195 | 153.0193 | 1.50 | 5.5 | 109, 71 | Dihydroxybenzoic acid |
| 6 | 2.29 | C13H15O9 | 315.0716 | 315.0722 | -1.87 | 6.5 | 153, 287, 196 | Gentisoil glucoside |
| 7 | 4.06 | C12H13O8 | 285.0611 | 285.0616 | -1.84 | 6.5 | 153, 109 | Uralenneoside |
| 8 | 4.40 | C8H7O5 | 183.0299 | 183.0299 | -0.05 | 5.5 | nd | Methyl gallate |
| 9 | 4.64 | C27H29O17 | 625.1401 | 625.1410 | -1.51 | 13.5 | 463, 301 | Quercetin diglucoside |
| 10 | 5.35 | C27H29O15 | 593.1506 | 593.1512 | -0.94 | 13.5 | 287 | Luteolin-7-O-rutinoside |
| 11 | 5.65 | C21H19O13 | 479.08261 | 479.08261 | -1.04 | 12.5 | 316, 287, 196 | Myricetin-3-O-glucoside |
| 12 | 5.80 | C19H13O12 | 433.0406 | 433.04012 | -1.45 | 13.5 | 301 | Ellagic acid-7-xyloside |
| 13 | 5.95 | C20H17O12 | 449.0721 | 449.0725 | -0.97 | 12.5 | 317, 287, 196 | Myricetin 3'-xyloside |
| 14 | 6.00 | C14H5O8 | 300.9988 | 300.9990 | -0.59 | 12.5 | nd | Ellagic acid |
| 15 | 6.08 | C21H19O12 | 463.0881 | 463.0882 | -0.27 | 12.5 | 301, 151 | Quercetin 3-O-β-D-glucopyranoside |
| 16 | 6.15 | C21H19O12 | 463.0877 | 463.0882 | -1.06 | 12.5 | 316 | Myricetin-3-O-rhamnoside |
| 17 | 6.34 | C20H17O11 | 433.0775 | 433.0776 | -0.41 | 12.5 | 301, 287, 196, 167, 126 | Quercetin 3-alpha-L-arabinofuranoside (Avicularin Isomer 1) |
| 18 | 6.47 | C20H17O11 | 433.0775 | 433.0776 | -0.41 | 12.5 | 301, 287, 196, 167, 126 | Quercetin 3-alpha-L-arabinofuranoside (Avicularin Isomer 2) |
| 19 | 6.55 | C21H19O11 | 447.0928 | 447.0933 | -1.00 | 12.5 | 301 | Isoorientin |
| 20 | 6.74 | C8H7O5 | 293.1390 | 293.1394 | -1.49 | 6.5 | 249, 274, 287, 205, 196 | Propanoic acid methyl ester |
| 21 | 6.95 | C30H25O16 | 625.1188 | 625.1199 | -1.78 | 18.5 | 316, 479 | Myricetin-O-rhamnoside-O-hexoside |
| 22 | 7.61 | C30H25O13 | 593.1294 | 593.1301 | -1.28 | 18.5 | 285, 447 | Kaempferol-O-rhamnoside-O-hexoside |
| 23 | 7.69 | C15H9O7 | 301.0349 | 301.0354 | -1.43 | 11.5 | 178, 151, 196, 287, 71 | Quercetin |
| 24 | 7.79 | C30H25O13 | 593.1291 | 593.1303 | -1.64 | 18.5 | 285, 447 | Kaempferol diglucoside |
| 25 | 8.04 | C17H13O7 | 329.0663 | 329.0667 | -1.00 | 11.5 | 314, 287, 196, 167 | Quercetin dimethyl ether |
| 26 | 9.14 | C18H15O8 | 359.0772 | 359.0772 | -0.08 | 11.5 | 344, 329 | Rosmarinic acid |
| 27 | 9.39 | C20H29O5 | 349.2019 | 349.2020 | -0.32 | 6.5 | 305 | Andrographolide |
| 28 | 9.66 | C20H31O4 | 335.2228 | 335.2228 | 0.16 | 5.5 | 291, 287, 196, 126, 100 | Cistodioic acid |
| 29 | 10.95 | C19H17O8 | 373.0923 | 373.0929 | -1.70 | 11.5 | 358, 287, 196 | Eriostemin |
| 30 | 12.0 | C22H33O5 | 377.2330 | 377.2333 | -0.91 | 6.5 | nd | Laurifolic acid |
Fig 3. LC(ESI-)HRMS chromatograms of the methanol extracts of the tested plants.
Table 2. LC(ESI-)HRMS of S. sclarea methanol extract.
| No | Rt (min) |
EC [M-H]- |
Experimental | Theoretical | Δm ppm | RDBeq | Fragments MSMS (m/z) |
Category of compound (Identification) |
|---|---|---|---|---|---|---|---|---|
| [M-H]- m/z | ||||||||
| 1 | 2.18 | C9H9O5 | 197.0454 | 197.0455 | -0.69 | 5.5 | 179, 153, 72 | Salvianic acid A |
| 2 | 4.86 | C9H7O4 | 179.0350 | 179.0350 | 0.37 | 6.5 | nd | Caffeic acid |
| 3 | 5.34 | C27H29O15 | 593.1501 | 593.1512 | -1.76 | 13.5 | 287, 196, 323, 269, 194 | luteolin-7-O-rutinoside |
| 4 | 5.36 | C16H17O9 | 353.0872 | 353.0878 | -1.57 | 8.5 | 173, 179 | Chlorogenic acid |
| 5 | 5.78 | C15H9O7 | 301.0349 | 301.0354 | -1.43 | 11.5 | nd | Quercetin |
| 6 | 5.79 | C21H17O13 | 477.0670 | 477.0675 | -1.00 | 13.5 | 161, 301, 315, 359 | Quercetin-3-glucuronide (Miquelianin) |
| 7 | 5.80 | C21H17O13 | 477.06670 | 477.06675 | -1.00 | 13.5 | 315, 300, 287, 196 | 6-hydroxyluteolin 7-O-glucuronide |
| 8 | 5.86 | C27H29O16 | 609.1465 | 609.1461 | 0.71 | 13.5 | 301 | Rutin |
| 9 | 6.02 | C14H5O8 | 300.9986 | 300.9990 | -1.30 | 12.5 | nd | Ellagic acid |
| 10 | 6.16 | C21H20O12 | 463.0876 | 463.0876 | -1.32 | 12.5 | 419 | Hyperoside |
| 11 | 6.35 | C24H25O13 | 521.1296 | 521.1301 | -0.93 | 12.5 | 359 | Rosmarinic acid-3-D-glucoside |
| 12 | 6.66 | C7H6O3 | 137.0248 | 137.0244 | 2.76 | 5.5 | 108, 93 | Hydroxybenzoic acid |
| 13 | 6.67 | C21H19O10 | 431.0980 | 431.0984 | -0.87 | 12.5 | 269 | Apigenin 7-O-D-glucoside |
| 14 | 6.72 | C21H17O11 | 445.0775 | 445.0776 | -0.40 | 13.5 | 287, 161, 196, 194, 115 | Apigenin-7-O-β-D glucuronide |
| 15 | 6.79 | C18H15O8 | 359.0770 | 359.0772 | -0.68 | 11.5 | 161, 179, 197 | Rosmarinic acid |
| 16 | 6.92 | C21H17O12 | 461.0725 | 461.0725 | -0.08 | 13.5 | 285 | Luteolin-7-O-β-D glucuronide |
| 17 | 7.11 | C27H21O12 | 537.1035 | 537.1038 | -0.62 | 17.5 | 135, 185, 25, 313, 461 | Salvianolic acid I |
| 18 | 7.18 | C27H21O12 | 473.10855 | 473.10855 | -0.81 | 13.5 | 287, 429, 196, 167 | Apigenin-acetylglucoside |
| 19 | 7.60 | C15H9O6 | 285.0403 | 285.0405 | -0.41 | 11.5 | 133, 151, 197, 213 | Luteolin |
| 20 | 7.76 | C16H11O7 | 315.05063 | 315.05063 | -1.26 | 11.5 | 83, 145, 187 | Rhamnetin |
| 21 | 7.80 | C16H11O6 | 299.0558 | 299.0561 | -1.08 | 11.5 | 285 | Diosmetin |
| 22 | 7.99 | C19H17O8 | 373.0925 | 373.0929 | -1.05 | 11.5 | 135, 175, 179, 197 | Methyl rosmarinate |
| 23 | 8.16 | C36H29O16 | 717.1448 | 717.1461 | -1.85 | 22.5 | 519 | Salvianolic acid B |
| 24 | 8.28 | C15H9O5 | 269.0453 | 269.0455 | -0.73 | 11.5 | 117, 151 | Apigenin |
| 25 | 9.32 | C16H11O6 | 299.0557 | 299.0561 | -1.39 | 11.5 | 299 | Hispidulin |
| 26 | 9.40 | C17H13O6 | 313.0714 | 313.0718 | -1.21 | 11.5 | 298, 196 | Cirsimaritin |
| 27 | 9.45 | C20H25O5 | 345.1702 | 345.1707 | -1.50 | 8.5 | 345 | Epi-rosmanol |
| 28 | 10.19 | C16H11O5 | 283.0610 | 283.0612 | -0.78 | 11.5 | 283 | Genkwanin |
Table 3. LC(ESI-)HRMS of O. vulgare methanol extract.
| No | Rt (min) |
EC [M-H]- |
Experimental | Theoretical | Δm ppm | RDBeq | Fragments MSMS (m/z) |
Category of compound (Identification) |
|---|---|---|---|---|---|---|---|---|
| [M-H]- m/z | ||||||||
| 1 | 0.57 | C7H11O6 | 191.0563 | 191.0561 | 1.01 | 2.5 | 127, 173, 71, 85 | Quinic acid |
| 2 | 2.09 | C9H9O5 | 197.0454 | 197.0455 | -0.69 | 5.5 | 179 | Salvianic acid A |
| 3 | 2.23 | C7H5O4 | 153.0196 | 153.0193 | 1.50 | 5.5 | nd | Dihydroxybenzoic acid |
| 4 | 4.49 | C13H15O8 | 299.0768 | 299.0772 | -1.63 | 6.5 | nd | Hydroxybenzoic acid hexose |
| 5 | 4.86 | C9H7O4 | 179.0350 | 179.0350 | 0.37 | 6.5 | 135, 167, 71 | Caffeic acid |
| 6 | 4.91 | C16H17O9 | 353.0872 | 353.0878 | -1.57 | 8.5 | 173, 179 | Chlorogenic acid |
| 7 | 5.08 | C8H7O4 | 167.0352 | 167.0350 | 1.22 | 5.5 | nd | Vanilic acid |
| 8 | 5.11 | C27H29O16 | 609.1453 | 609.1461 | -1.38 | 13.5 | 489, 287, 196, 519, 167 | Luteolin-6,8-C-dihexose |
| 9 | 5.34 | C27H29O15 | 593.1506 | 593.1512 | -0.94 | 13.5 | 473, 353, 503, 196 | Apigenin-6,8-di-C-hexoside |
| 10 | 5.66 | C21H19O11 | 447.0930 | 447.0933 | -0.52 | 12.5 | 327, 353, 429, 287, 196 | Isoorientin |
| 11 | 5.67 | C9H7O3 | 163.04033 | 163.04033 | 1.60 | 6.5 | nd | p-Coumaric acid |
| 12 | 6.08 | C21H19O10 | 431.0978 | 431.0984 | -1.30 | 12.5 | 341, 311, 287, 196 | Vitexin/Isovitexin |
| 13 | 6.14 | C15H11O7 | 303.0508 | 303.0510 | -0.60 | 10.5 | 287, 196, 96, 71 | Taxifolin |
| 14 | 6.21 | C11H9O7 | 253.0352 | 253.0354 | -0.80 | 7.5 | nd | Chrysin |
| 15 | 6.26 | C21H17O12 | 461.0722 | 461.0725 | -0.68 | 13.5 | 285 | Kaempferol-O glucuronide |
| 16 | 6.31 | C16H13O6 | 301.0717 | 301.0718 | -0.25 | 10.5 | nd | Hesperetin |
| 17 | 6.47 | C27H21O12 | 537.1038 | 537.1038 | -0.05 | 17.5 | 493 | Salvianolic acid I |
| 18 | 6.62 | C27H21O12 | 537.1037 | 537.1038 | -0.28 | 17.5 | 519 | Salvianolic acid H |
| 19 | 6.73 | C21H17O11 | 445.0774 | 445.0776 | -0.47 | 13.5 | 269, 287, 196, 302, 162, 124 | Apigenin 7-O glucuronide |
| 20 | 6.77 | C18H15O8 | 359.0772 | 359.0772 | -0.08 | 11.5 | 197, 161 | Rosmarinic acid |
| 21 | 6.89 | C27H21O12 | 537.1038 | 537.1038 | -0.05 | 17.5 | 493 | Lithospermic acid |
| 22 | 7.19 | C36H29O16 | 717.1456 | 717.14561 | -0.66 | 22.5 | 519, 475 | Salvianolic acid E/B |
| 23 | 7.38 | C26H19O10 | 491.0981 | 491.0981 | -0.58 | 17.5 | 311, 135 | Salvianolic acid C |
| 24 | 7.48 | C15H11O6 | 287.0560 | 287.0561 | -0.49 | 10.5 | 151, 135, 107 | Eriodictyol |
| 25 | 7.61 | C15H9O6 | 285.0403 | 285.0405 | -0.41 | 11.5 | nd | Kaempferol |
| 26 | 7.63 | C15H9O6 | 285.0403 | 285.0405 | -0.41 | 11.5 | nd | Luteolin |
| 27 | 7.94 | C28H31O15 | 607.1664 | 607.1668 | -0.65 | 13.5 | 299 | Diosmin |
| 28 | 8.04 | C17H13O7 | 329.0663 | 329.0667 | -1.00 | 11.5 | 314, 299 | Quercetin dimethyl ether |
| 29 | 8.28 | C15H9O5 | 269.0455 | 269.0455 | -0.16 | 11.5 | nd | Apigenin |
| 30 | 9.02 | C16H13O6 | 301.2018 | 301.2020 | -0.67 | 2.5 | 165, 135, 299 | Dihydro-kaempferide |
Table 4. LC(ESI-)HRMS of T. longicaulis methanol extract.
| No | Rt (min) |
EC [M-H]- |
Experimental | Theoretical | Δm ppm | RDBeq | Fragments MSMS (m/z) |
Category of compound (Identification) |
|---|---|---|---|---|---|---|---|---|
| [M-H]- m/z | ||||||||
| 1 | 2.08 | C9H9O5 | 197.04544 | 197.04544 | -0.53 | 5.5 | 179 | 3,4 Dihydroxyphenylacetic acid |
| 2 | 2.19 | C7H5O4 | 153.0195 | 153.0193 | 1.20 | 5.5 | 109, 71 | Protocatechuic acid |
| 3 | 4.75 | C16H17O9 | 353.0872 | 353.0878 | -1.74 | 8.5 | 173, 179 | Chlorogenic acid |
| 4 | 4.86 | C9H7O4 | 179.0350 | 179.0350 | 0.29 | 6.5 | 135, 71, 167 | Caffeic acid (Isomer I) |
| 5 | 5.13 | C9H7O4 | 179.0350 | 179.0350 | 0.34 | 6.5 | 135, 71, 167 | Caffeic acid (Isomer II) |
| 6 | 5.33 | C27H29O15 | 593.1506 | 593.1512 | -0.94 | 13.5 | 473, 353, 196, 287, 503 | Apigenin diglucoside |
| 7 | 5.68 | C21H19O11 | 447.09308 | 447.09308 | -0.46 | 12.5 | 285 | Luteolin O-Hexoside |
| 8 | 5.75 | C12H19O12 | 463.0879 | 463.0882 | -0.60 | 12.5 | 301 | Quercetin-O-hexoside |
| 9 | 5.77 | C21H19O12 | 463.0881 | 463.0882 | -0.27 | 12.5 | 301, 151 | Quercetin 3-O-glucoside |
| 10 | 6.0 | C27H29O16 | 609.1465 | 609.1461 | 0.71 | 13.5 | 301 | Rutin |
| 11 | 6.12 | C21H21O11 | 449.1087 | 449.1089 | -0.58 | 11.5 | 287, 196, 313 | Eriodictyol O-hexoside |
| 12 | 6.13 | C30H25O13 | 593.1291 | 593.1303 | -1.64 | 18.5 | 285, 196, 167, 478 | Kaempferol diglucoside |
| 13 | 6.20 | C21H19O11 | 447.09308 | 447.09308 | -0.46 | 12.5 | 285 | Luteolin 7-glucoside |
| 14 | 6.28 | C24H25O13 | 521.1299 | 521.1301 | -0.23 | 12.5 | 359, 287, 196 | Rosmarinic acid-3-D-glucoside |
| 15 | 6.81 | C18H15O8 | 359.0769 | 359.0772 | -0.85 | 11.5 | 161, 197, 179, 135 | Rosmarinic acid |
| 16 | 7.65 | C27H21O12 | 537.1036 | 537.1038 | -0.39 | 17.5 | 493 | Lithospermic acid A |
| 17 | 7.96 | C19H17O8 | 373.0926 | 373.0929 | -1.05 | 11.5 | 179 | Methyl rosmarinate |
| 18 | 8.28 | C15H9O5 | 269.0454 | 269.0455 | -0.50 | 11.5 | nd | Apigenin |
| 19 | 11.67 | C30H47O4 | 471.3477 | 471.3480 | -0.49 | 7.5 | 287 | Anemosapogenin |
| 20 | 12.07 | C30H47O4 | 471.3476 | 471.3480 | -0.82 | 7.5 | 287 | Augustic acid |
| 21 | 12.91 | C30H47O4 | 471.3474 | 471.3480 | -0.49 | 7.5 | 287 | Benthamic acid |
| 22 | 15.28 | C30H47O3 | 455.3526 | 455.3531 | -1.05 | 7.5 | 287 | Betulinic acid |
| 23 | 15.63 | C30H47O3 | 455.3528 | 455.3531 | -0.49 | 7.5 | 287 | Oleanolic acid |
| 24 | 15.65 | C30H47O3 | 455.3530 | 455.3531 | -0.15 | 7.5 | 287 | Ursolic acid |
| 25 | 16.29 | C30H45O3 | 453.3369 | 453.3374 | -1.11 | 8.5 | 287, 196 | Micromeric acid |
Table 5. LC(ESI-)HRMS of C. creticus methanol extract.
| No | Rt (min) |
EC [M-H]- |
Experimental | Theoretical | Δm ppm | RDBeq | Fragments MSMS (m/z) |
Category of compound (Identification) |
|---|---|---|---|---|---|---|---|---|
| [M-H]- m/z | ||||||||
| 1 | 0.55 | C7H11O6 | 191.0563 | 191.0561 | 1.01 | 2.5 | 173, 127, 85 | Quinic acid |
| 2 | 0.70 | C7H9O5 | 173.0456 | 173.0455 | 0.18 | 3.5 | nd | Shikimic acid |
| 3 | 0.93 | C13H15O10 | 331.0666 | 331.0671 | -1.45 | 5.5 | nd | Glucogallin |
| 4 | 1.08 | C7H5O5 | 169.0143 | 169.0142 | 0.57 | 5.5 | 125 | Gallic acid |
| 5 | 2.29 | C13H15O9 | 315.0716 | 315.0722 | -1.87 | 6.5 | 153, 287, 196 | Gentisoil glucoside |
| 6 | 2.38 | C15H13O7 | 305.0661 | 305.0667 | -1.78 | 9.5 | 179, 219, 165, 261 | Epigallocatechin |
| 7 | 4.04 | C12H13O8 | 285.0613 | 285.0616 | -1.09 | 6.5 | 153, 109 | Uralenneoside |
| 8 | 4.21 | C34H23O22 | 783.0701 | 783.0686 | 1.81 | 23.5 | nd | Pedunculagin |
| 9 | 4.65 | C15H13O6 | 289.07135 | 289.07135 | -1.42 | 9.5 | nd | Cathechin |
| 10 | 4.67 | C20H19O14 | 483.0714 | 483.0718 | -1.52 | 9.5 | nd | Digaloil-β-D-glucopiranose |
| 11 | 4.80 | C27H21O18 | 633.07220 | 633.07220 | -1.78 | 17.5 | 300, 287, 196, 478 | Strictinin |
| 12 | 4.94 | C21H21O13 | 481.0983 | 481.0988 | -0.90 | 11.5 | 287, 196, 245 | Mirciaphenone B |
| 13 | 5.33 | C27H29O15 | 593.1506 | 593.1512 | -0.94 | 13.5 | 473 | Apigenin diglucoside |
| 14 | 5.64 | C27H29O17 | 625.1401 | 625.1410 | -1.51 | 13.5 | 463, 301 | Quercetin diglucoside |
| 15 | 5.65 | C21H19O13 | 479.08261 | 479.08261 | -1.04 | 12.5 | nd | Myricetin-3-O-glucoside |
| 16 | 5.82 | C19H13O12 | 433.0406 | 433.04012 | -1.38 | 13.5 | 301 | Ellagic acid-7-xyloside |
| 17 | 6.01 | C27H29O16 | 609.1450 | 609.1461 | -1.78 | 13.5 | 287, 301, 196, 478 | Kaempferol diglucoside |
| 18 | 6.06 | C27H29O16 | 609.1446 | 609.1461 | -2.48 | 13.5 | 301 | Rutin |
| 19 | 6.02 | C21H19O12 | 463.0881 | 463.0882 | -0.27 | 12.5 | 301, 151 | Quercetin 3-O-β-D-glucopyranoside |
| 20 | 6.15 | C21H19O12 | 463.0877 | 463.0882 | -1.06 | 12.5 | 316 | Myricetin-3-O-rhamnoside |
| 21 | 6.34 | C14H5O8 | 300.9988 | 300.9990 | -0.59 | 12.5 | nd | Ellagic acid |
| 22 | 6.37 | C27H29O15 | 593.1506 | 593.1512 | -0.94 | 13.5 | 287 | Luteolin-7-O-rutinoside |
| 23 | 6.56 | C21H19O11 | 447.0930 | 447.0933 | -0.73 | 12.5 | 301 | Isoorientin |
| 24 | 7.0 | C30H25O16 | 625.1188 | 625.1199 | -1.78 | 18.5 | 316, 479 | Myricetin-O-rhamnoside-O-hexoside |
| 25 | 7.65 | C30H25O13 | 593.1294 | 593.1301 | -1.28 | 18.5 | 285, 447 | Kaempferol -O-rhamnoside-O-hexoside |
| 26 | 7.81 | C30H25O13 | 593.1291 | 593.1303 | -1.64 | 18.5 | 285, 447 | Kaempferol diglucoside |
| 27 | 8.27 | C15H9O5 | 269.0454 | 269.0455 | -0.39 | 11.5 | nd | Apigenin |
| 28 | 8.72 | C16H11O6 | 299.05585 | 299.05585 | -0.88 | 11.5 | 284, 196 | Kaempferol methylether |
| 29 | 10.08 | C16H11O5 | 283.0611 | 283.0612 | -0.35 | 11.5 | 268 | Apigenin methylether |
| 30 | 10.09 | C16H11O5 | 283.0608 | 283.0612 | -1.32 | 11.5 | 283 | Apigenin methylether |
C. creticus and C. monspeliensis exhibited high antibacterial and antibiofilm activity against obligate anaerobes and S. mutans, respectively
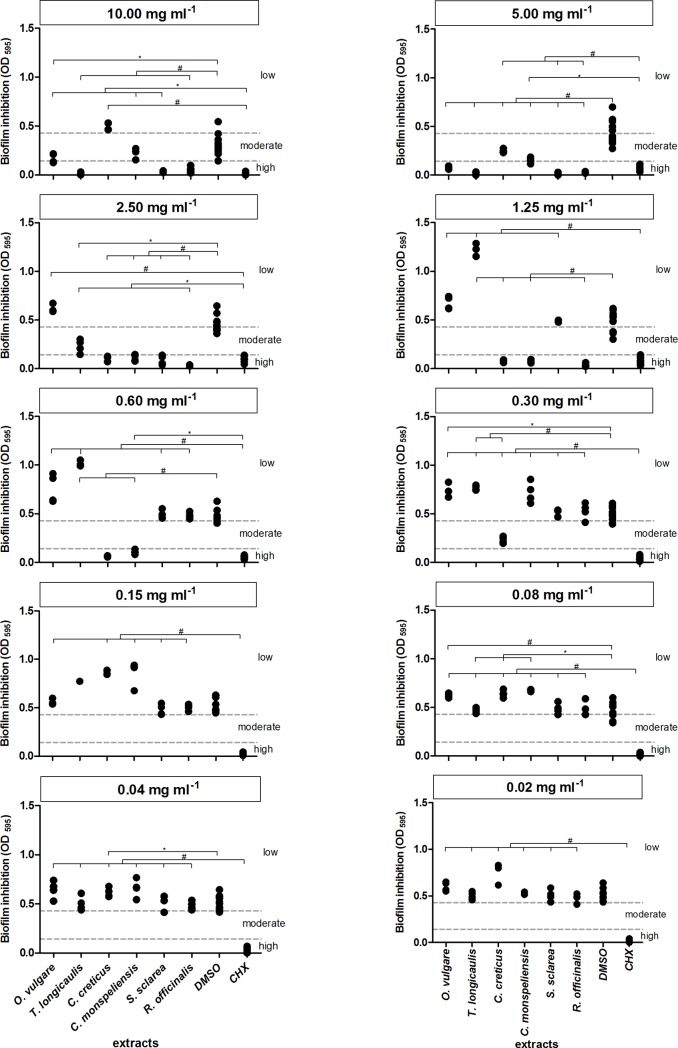
The mean MIC / MBC values for the methanol extract of C. creticus are shown in Table 7. Under its influence, especially the growth of the obligate anaerobes was efficiently reduced at low inhibitory concentrations ranging from 0.08 mg ml-1 (P. gingivalis, P. micra) to 0.60 mg ml-1 (F. nucleatum), while MBC values varied from 0.15 mg ml-1 (P. gingivalis, P. micra) to 0.60 mg ml-1 (P. intermedia, F. nucleatum). Likewise, S. oralis was eliminated at a bactericidal C. creticus concentration of 0.60 mg ml-1. Additionally, the extract was very effective against S. aureus (MIC = 0.60 mg ml-1), whereas it had a moderate effect on S. sobrinus and E. faecalis with a MIC value of 5.00 mg ml-1. No significant antimicrobial effect was observed on S. mutans, C. albicans and E. coli. The biofilm plate assay revealed a moderate reduction of biofilm production as shown in Fig 4. The biofilm formation of S. mutans was significantly inhibited (mean OD595 = 0.231) at a C. creticus concentration of 0.60 mg ml-1 (low cut-off value OD595 = 0.143), while high S. mutans biofilm formation was observed at 0.15 mg ml-1 (high cut-off value OD595 = 0.428).
Table 7. Antimicrobial activity in mg ml-1 of C. creticus methanol extract.
| C. creticus | ||||
|---|---|---|---|---|
| Sample | Methanol extract DMSO (%) | |||
| (in mg ml-1) | MIC | MBC | MIC | MBC |
| Streptococcus mutans DSM 20523 | 5.00 | 10.00 | 5.00 | NA |
| Streptococcus sobrinus DSM 20381 | 5.00 | 10.00 | 20.00 | 20.00 |
| Streptococcus oralis ATCC 35037 | 0.30 | 0.60 | 10.00 | 20.00 |
| Enterococcus faecalis ATCC 29212 | 5.00 | 10.00 | 20.00 | NA |
| Candida albicans DSM 1386 | 10.00 | 10.00 | 10.00 | 20.00 |
| Escherichia coli ATCC 25922 | NA | NA | 20.00 | NA |
| Staphylococcus aureus ATCC 25923 | 0.60 | 2.50 | 20.00 | NA |
| Porphyromonas gingivalis W381 | 0.08 | 0.15 | 20.00 | 20.00 |
| Prevotella intermedia MSP 34 | 0.30 | 0.60 | 5.00 | 5.00 |
| Fusobacterium nucleatum ATCC 25586 | 0.60 | 0.60 | 10.00 | 10.00 |
| Parvimonas micra ATCC 23195 | 0.08 | 0.15 | 10.00 | 20.00 |
NA: No activity observed, MIC or MBC of extracts and DMSO at 10.00 mg ml-1 and 20%, respectively.
MIC = extract concentration at which the OD measurement revealed minimal bacterial growth.
MBC = extract concentration at which a 3-Log reduction (99.9%) of the bacterial growth was induced.
Fig 4. Diagrams depicting the antibiofilm effect of six Mediterranean herb extracts against S. mutans.
The low and high cut-off OD595 values were estimated at 0.143 and 0.428, respectively. High S. mutans biofilm inhibition is exhibited at OD595 values ≤0.143, whereas S. mutans moderate biofilm formation is displayed at 0.143 ≤ OD595 values ≤0.428. DMSO and CHX concentrations are shown for each extract concentration. Hash symbols and asterisks represent statistically significant differences (p < 0.01 and p < 0.05), respectively.
Table 8 summarizes the MIC and MBC values for the methanol extract of C. monspeliensis. In general, C. monspeliensis exhibited significant bactericidal effects against the obligate anaerobes with a MIC range from 0.04 mg ml-1 (P. gingivalis, P. micra) to 0.60 mg ml-1 (F. nucleatum), while the extract had no antimicrobial impact on E. coli and C. albicans. A moderate inhibitory effect was observed for S. mutans (MIC = 2.50 mg ml-1). The MIC and MBC values were estimated at 0.15 mg ml-1 and 0.60 mg ml-1 for S. oralis, whereas E. faecalis was less susceptible to C. monspeliensis (MIC = 5.00 mg ml-1; MBC = 10.00 mg ml-1). The methanol extract of C. monspeliensis had a high inhibitory effect on S. mutans biofilm formation (Fig 4) at a concentration of 0.60 mg ml-1 (mean OD595 = 0.106).
Table 8. Antimicrobial activity in mg ml-1 of C. monspeliensis methanol extract.
| C. monspeliensis | ||||
|---|---|---|---|---|
| Sample | Methanol extract DMSO (%) | |||
| (in mg ml-1) | MIC | MBC | MIC | MBC |
| Streptococcus mutans DSM 20523 | 2.50 | NA | 10.00 | NA |
| Streptococcus sobrinus DSM 20381 | 2.50 | 5.00 | 20.00 | 20.00 |
| Streptococcus oralis ATCC 35037 | 0.15 | 0.60 | 10.00 | 20.00 |
| Enterococcus faecalis ATCC 29212 | 5.00 | 10.00 | 20.00 | NA |
| Candida albicans DSM 1386 | 5.00 | 10.00 | 5.00 | NA |
| Escherichia coli ATCC 25922 | NA | NA | 20.00 | NA |
| Staphylococcus aureus ATCC 25923 | 0.60 | 2.50 | 20.00 | NA |
| Porphyromonas gingivalis W381 | 0.04 | 0.15 | 20.00 | 20.00 |
| Prevotella intermedia MSP 34 | 0.08 | 0.08 | 2.50 | 5.00 |
| Fusobacterium nucleatum ATCC 25586 | 0.60 | 0.60 | 10.00 | 10.00 |
| Parvimonas micra ATCC 23195 | 0.04 | 0.08 | 10.00 | 20.00 |
NA: No activity observed, MIC or MBC of extracts and DMSO at 10.00 mg ml-1 and 20%, respectively.
MIC = extract concentration at which the OD measurement revealed minimal bacterial growth.
MBC = extract concentration at which a 3-Log reduction (99.9%) of the bacterial growth was induced.
R. officinalis and S. sclarea significantly reduced growth of all oral bacteria and biofilm growth of S. mutans
In general, the methanol extract of R. officinalis was extremely effective against all tested pathogens (Table 9). The MIC values ranged from 0.08 mg ml-1 (P. micra) to 5.00 mg ml-1 (E. faecalis), with the highest efficacy among the streptococci on S. oralis at 0.30 mg ml-1. Similarly, the MBC values showed bactericidal effects in a range from 0.15 mg ml-1 (P. micra) to 5.00 mg ml-1 (E. faecalis). The extract had no significant effects on C. albicans and E. coli. The biofilm formation of S. mutans substantially decreased (mean OD595 = 0.038) at a R. officinalis concentration of 1.25 mg ml-1 (Fig 4).
Table 9. Antimicrobial activity in mg ml-1 of R. officinalis methanol extract.
| R. officinalis | ||||
|---|---|---|---|---|
| Sample | Methanol extract DMSO (%) | |||
| (in mg ml-1) | MIC | MBC | MIC | MBC |
| Streptococcus mutans DSM 20523 | 0.60 | 2.50 | 5.00 | NA |
| Streptococcus sobrinus DSM 20381 | 1.25 | 2.50 | 20.00 | NA |
| Streptococcus oralis ATCC 35037 | 0.30 | 0.60 | 20.00 | 20.00 |
| Enterococcus faecalis ATCC 29212 | 5.00 | 5.00 | 20.00 | NA |
| Candida albicans DSM 1386 | 10.00 | 10.00 | 10.00 | NA |
| Escherichia coli ATCC 25922 | 10.00 | 10.00 | 20.00 | NA |
| Staphylococcus aureus ATCC 25923 | 0.60 | 1.25 | 20.00 | NA |
| Porphyromonas gingivalis W381 | 0.15 | 0.30 | 20.00 | 20.00 |
| Prevotella intermedia MSP 34 | 0.30 | 0.60 | 5.00 | 5.00 |
| Fusobacterium nucleatum ATCC 25586 | 1.25 | 1.25 | 10.00 | 20.00 |
| Parvimonas micra ATCC 23195 | 0.08 | 0.15 | 5.00 | 20.00 |
NA: No activity observed, MIC or MBC of extracts and DMSO at 10.00 mg ml-1 and 20%, respectively.
MIC = extract concentration at which the OD measurement revealed minimal bacterial growth.
MBC = extract concentration at which a 3-Log reduction (99.9%) of the bacterial growth was induced.
The mean MIC and MBC values for the methanol extract of S. sclarea are presented in Table 10. The MIC values vary between 0.08 mg ml-1 (P. micra) and 2.50 mg ml-1 (S. sobrinus). S. sclarea extract at 0.15 mg ml-1 induced a 3-Log reduction of P. gingivalis and P. micra, whereas a higher S. sclarea concentration at 5.00 mg ml-1 was needed to eradicate S. mutans and S. sobrinus. E. coli, E. faecalis and C. albicans were not affected by the extract. Significant inhibition of biofilm formation of S. mutans (mean OD595 = 0.088) by S. sclarea was shown at a concentration of 2.50 mg ml-1 (Fig 4).
Table 10. Antimicrobial activity in mg ml-1 of S. sclarea methanol extract.
| S. sclarea | ||||
|---|---|---|---|---|
| Sample | Methanol extract DMSO (%) | |||
| (in mg ml-1) | MIC | MBC | MIC | MBC |
| Streptococcus mutans DSM 20523 | 1.25 | 5.00 | 5.00 | NA |
| Streptococcus sobrinus DSM 20381 | 2.50 | 5.00 | 20.00 | NA |
| Streptococcus oralis ATCC 35037 | 0.60 | 0.60 | 20.00 | 20.00 |
| Enterococcus faecalis ATCC 29212 | 10.00 | 10.00 | 20.00 | NA |
| Candida albicans DSM 1386 | 10.00 | 10.00 | 10.00 | NA |
| Escherichia coli ATCC 25922 | 10.00 | 10.00 | 20.00 | NA |
| Staphylococcus aureus ATCC 25923 | 1.25 | 1.25 | 20.00 | NA |
| Porphyromonas gingivalis W381 | 0.15 | 0.15 | 20.00 | 20.00 |
| Prevotella intermedia MSP 34 | 0.15 | 0.30 | 5.00 | 5.00 |
| Fusobacterium nucleatum ATCC 25586 | 0.60 | 0.60 | 10.00 | 20.00 |
| Parvimonas micra ATCC 23195 | 0.08 | 0.15 | 5.00 | 20.00 |
NA: No activity observed, MIC or MBC of extracts and DMSO at 10.00 mg ml-1 and 20%, respectively.
MIC = extract concentration at which the OD measurement revealed minimal bacterial growth.
MBC = extract concentration at which a 3-Log reduction (99.9%) of the bacterial growth was induced.
O. vulgare and T. longicaulis demonstrated significant bactericidal activity against obligate anaerobes but low antibiofilm activity against S. mutans
The methanol extract of O. vulgare eradicated the tested oral bacteria in a range of MBC values from 0.30 mg ml-1 (P. micra) to 5.00 mg ml-1 for E. faecalis, S. mutans and S. sobrinus, as shown in Table 11. The extract had nearly no antimicrobial impact on C. albicans, E. coli and the obligate anaerobe P. intermedia. The most significant inhibitory effect was induced at a O. vulgare concentration of 0.30 mg ml-1 on P. gingivalis and P. micra and at 0.60 mg ml-1 on S. oralis, respectively. Biofilm formation of S. mutans was significantly reduced (mean OD595 = 0.081) at 5.00 mg ml-1 O. vulgare extract, whereas lower extract concentration had no impact on S. mutans biofilms (Fig 4).
Table 11. Antimicrobial activity in mg ml-1 of O. vulgare methanol extract.
| O. vulgare | ||||
|---|---|---|---|---|
| Sample | Methanol extract DMSO (%) | |||
| (in mg ml-1) | MIC | MBC | MIC | MBC |
| Streptococcus mutans DSM 20523 | 2.50 | 5.00 | 5.00 | NA |
| Streptococcus sobrinus DSM 20381 | 2.50 | 5.00 | 20.00 | NA |
| Streptococcus oralis ATCC 35037 | 0.60 | 1.25 | 10.00 | 20.00 |
| Enterococcus faecalis ATCC 29212 | 5.00 | 5.00 | 20.00 | NA |
| Candida albicans DSM 1386 | 10.00 | 10.00 | 10.00 | 10.00 |
| Escherichia coli ATCC 25922 | 10.00 | 10.00 | 20.00 | NA |
| Staphylococcus aureus ATCC 25923 | 1.25 | 1.25 | 20.00 | NA |
| Porphyromonas gingivalis W381 | 0.30 | 0.60 | 20.00 | 20.00 |
| Prevotella intermedia MSP 34 | 2.50 | 2.50 | 5.00 | 5.00 |
| Fusobacterium nucleatum ATCC 25586 | 1.25 | 1.25 | 10.00 | 10.00 |
| Parvimonas micra ATCC 23195 | 0.30 | 0.30 | 10.00 | 20.00 |
NA: No activity observed, MIC or MBC of extracts and DMSO at 10.00 mg ml-1 and 20%, respectively.
MIC = extract concentration at which the OD measurement revealed minimal bacterial growth.
MBC = extract concentration at which a 3-Log reduction (99.9%) of the bacterial growth was induced.
The antimicrobial activity of T. longicaulis on the tested bacterial strains and C. albicans is displayed in Table 12. The MIC values varied from 0.08 mg ml-1 (P. micra) to 2.50 mg ml-1 (S. sobrinus, E. coli). The MBC values demonstrated the persistence of C. albicans and E. coli in the presence of 10.00 mg ml-1 T. longicaulis methanol extract, whereas all other strains were killed from 0.15 mg ml-1 (P. micra) to 2.50 mg ml-1 (S. sobrinus, E. faecalis). T. longicaulis inhibited strongly biofilm formation by S. mutans at 5.00 mg ml-1 (mean OD595 = 0.013) but also no statistically significant difference to CHX was detected at 2.50 mg ml-1 (Fig 4).
Table 12. Antimicrobial activity in mg ml-1 of T. longicaulis methanol extract.
| T. longicaulis | ||||
|---|---|---|---|---|
| Sample | Methanol extract DMSO (%) | |||
| (in mg ml-1) | MIC | MBC | MIC | MBC |
| Streptococcus mutans DSM 20523 | 0.60 | 1.25 | 5.00 | NA |
| Streptococcus sobrinus DSM 20381 | 2.50 | 2.50 | 10.00 | NA |
| Streptococcus oralis ATCC 35037 | 0.60 | 1.25 | 20.00 | 20.00 |
| Enterococcus faecalis ATCC 29212 | 1.25 | 2.50 | 20.00 | NA |
| Candida albicans DSM 1386 | 5.00 | 10.00 | 10.00 | NA |
| Escherichia coli ATCC 25922 | 2.50 | 10.00 | 20.00 | NA |
| Staphylococcus aureus ATCC 25923 | 0.60 | 0.60 | 20.00 | NA |
| Porphyromonas gingivalis W381 | 0.15 | 0.30 | 20.00 | 20.00 |
| Prevotella intermedia MSP 34 | 0.30 | 0.60 | 2.50 | 2.50 |
| Fusobacterium nucleatum ATCC 25586 | 0.60 | 0.60 | 5.00 | 10.00 |
| Parvimonas micra ATCC 23195 | 0.08 | 0.15 | 5.00 | 10.00 |
NA: No activity observed, MIC or MBC of extracts and DMSO at 10.00 mg ml-1 and 20%, respectively.
MIC = extract concentration at which the OD measurement revealed minimal bacterial growth.
MBC = extract concentration at which a 3-Log reduction (99.9%) of the bacterial growth was induced.
Discussion
In this report all tested extracts effectively inhibited mainly the anaerobic oral microorganisms and in concentrations ≥0.3 mg ml-1 had moderate to high antibiofilm activity against S. mutans comparable to that of CHX. Lamiaceae is a family of great diversity and variety, containing important medicinal herbs with diverse biological properties. Most of the plants are aromatic and possess essential oils; however, they also contain important phenolic compounds. Additionally, Cistus species are widely spread in Europe and some, such as C. monspeliensis and C. creticus are typical components of the Mediterranean flora. Preliminary phytochemical analysis was performed with HPTLC, which is most recent evolution of planar chromatography, specifically tailored for the analysis of natural products. The microtiter plate test is an accepted standard biofilm assay, which has been used frequently in literature due to its practicability. It has the advantages to allow testing of different bacterial species or substances.
To date, most of the studies found in literature [43–45] have mainly reported on the antimicrobial effects of essential oils from C. creticus, C. monspeliensis, O. vulgare, R. officinalis, S. sclarea and T. longicaulis on “non-oral” bacterial pathogens and C. albicans. To the best of our knowledge, this is the first report on the antibacterial and antibiofilm effectiveness of methanol extracts from the aforementioned herbs against various oral pathogens.
In the present report, C. creticus and C. monspeliensis extracts inhibited effectively obligate anaerobes such as P. gingivalis, P. micra and P. intermedia. To date, several studies [43, 45–48] have confirmed the enhanced antimicrobial activity of Cistus spp. against diverse “non-oral” bacteria and fungi. Interestingly, six out of seven labdane-type isolated diterpenes from leaves of C. creticus L. showed inhibitory effects against the Gram-negative Pseudomonas aeruginosa and Klebsiella pneumoniae [43]. As the methanol extract of C. creticus exhibited no significant antimicrobial activity against E. coli in this study, the resulted MIC value was comparable with the relative high MIC ≥3 mg ml-1 of a hexane leaf extract of C. creticus L. [47]. In another report, Bouamama et al. [45] tested C. monspeliensis methanol extract against E. coli and exhibited no activity of the extract accounting for a MIC of 25 mg ml-1.
In general, facultative anaerobic Gram-negative bacteria are more resistant to the Cistus spp. extracts than Gram-positive microorganisms [48], while obligate anaerobes are more sensitive to Cistus spp. treatment. This is due to the fact that the outer bacterial cell membrane of Gram-negative bacteria serves as a dense permeability barrier that hinders the penetration of lipophilic molecules [49, 50]. The Gram-positive bacteria with thicker cell walls than the Gram-negative bacteria also develop defense strategies against antimicrobials such as the production of extracellular proteases and the chemical modification of cell membrane or cell wall [51, 52]. In an earlier in situ report [53], rinsing of the oral cavity with Cistus tea resulted in the reduction of adherent bacteria on enamel surfaces. In the present report, the high antibacterial activity of the Cistus spp. extracts against the Gram-positive S. oralis and S. aureus contradicted the significantly lower susceptibility of S. aureus to C. monspeliensis methanol extract (MIC = 25 mg ml-1) demonstrated by Bouamama et al. [45]. Nevertheless, the hexane leaf extract of C. creticus showed high bacterial growth inhibition of S. aureus and E. faecalis (MIC = 0.5 mg ml-1) in an earlier report by Anastasaki et al. [47]. The conflicting outcomes can be ascribed to the differing extraction methods used. In regard with the antifungal activity, even after the application of high-concentrated extracts, C. albicans could not be effectively killed [43, 45–47].
The tested rosemary and sage extracts significantly reduced the growth of all screened oral bacteria such as streptococci and E. faecalis. Although the methanol extract of R. officinalis reduced S. mutans (MIC = 0.60 mg ml-1) effectively in this report, the inhibition level of S. sobrinus and F. nucleatum (MIC = 1.25 mg ml-1) was moderate. Surprisingly, the phenols carnosic acid and carnosol enabled the activity of various conventional antibiotics against overexpressing efflux pumps in S. aureus strains [54]. In contrast, an rosemary EO tested by Hammer et al. [55] failed to inhibit E. faecalis at 2% (v/v).
In a randomized double-blind placebo-controlled trial a polyherbal mouthwash rinsing containing R. officinalis among three hydroalcoholic extracts, showed a high antibacterial efficacy comparable to 0.2% (w/v) CHX in the treatment of gingivitis [56]. Since new rosemary compounds have been isolated lately [57], further antimicrobial screening of rosemary is required.
The positive antimicrobial effects of S. sclarea methanol extract are in agreement with the MIC values against S. aureus and E. coli revealed by Firuzi et al. [58], but do not correspond to the low antibacterial activity against S. aureus shown by Stagos et al. [59]. The results are in accordance to the low susceptibility shown by Hammer et al. [55]. In the present study, the high antibacterial activity against facultative anaerobic oral pathogens was confirmed [60]. Finally, the main S. sclarea components, the diterpenoids salvipisone and aethiopinone, revealed both bactericidal and antibiofilm activity against S. aureus and S. epidermidis strains [61, 62].
Although the O. vulgare methanol extract effectively killed Gram-negative obligate anaerobes in this study, S. aureus and E. coli were not as susceptible to extract treatment contrary to the outcomes of previous reports on an ethanol extract [63] and an EO [55]. The discrepancies can be attributed to different extraction solvents used, MIC method or different chemical composition of the extract used.
In the present report, T. longicaulis eradicated both Gram-positive and Gram-negative bacteria confirming the results of earlier studies, in which higher amounts of carvacrol accounted for higher antibacterial efficacy than geraniol [64, 65]. The similar inhibitory concentrations of T. longicaulis EO as presented by De Martino et al. [66] disprove the importance of the ratio between oxygenated monoterpenes and monoterpene hydrocarbons. This implies that, beside the fact of using different classification for phenols, the variety of synergistic and additional modes of antimicrobial action can be related to both inactive and weakly active compounds in different quantitative proportions.
There is a limited amount of reports on the antibiofilm activity of the tested plant species [61, 62, 67, 68]. Two main components of S. sclarea, namely salvipisone and aethiopinone, effectively reduced biofilm volume produced by S. aureus and S. epidermidis [61, 62]. Since intraoral bacterial glucosyltransferases (GTases) synthesize main extracellular matrix substrates such as glucan and fructan from sucrose contributing to the bacterial biofilm formation on tooth surfaces, the enhanced inhibitory activity of aqueous and methanol extract of rosemary against GTase of S. sobrinus is noteworthy [67]. This was confirmed by Quave et al. [68] with an ethanol extract, which reduced biofilm production of methicillin-resistant S. aureus. Even P. aeruginosa was eradicated by the EO of O. vulgare spp. Interestingly, in the present study although the OD values of the extracts were generally more scattered compared to the OD values of CHX, extract concentrations ≥0.3 mg ml-1 had moderate to high antibiofilm activity against S. mutans.
In conclusion, all tested Mediterranean herbs inhibited effectively the screened obligate anaerobic oral microorganisms. Thus, the null hypothesis was rejected. The outcome of this microbiological screening encourages further investigations to encounter and develop natural components with antimicrobial and antibiofilm activity against oral pathogens. Due to the increasing incidence of multi-resistant bacteria despite the use of oral disinfectants e.g. chlorhexidine, the application of herb extracts could prove to be an effective alternative treatment strategy against oral pathogens [69, 70]. Interestingly, diverse side effects of conventional oral care products such as allergies, intolerable taste, tooth coloring, toxicity, and antimicrobial resistance have triggered the search for alternative, in best case natural, antimicrobials. The development of natural resources is crucial for developing countries contributing to economic growth and enhancing people’s health at low cost [22, 60, 71, 72]. Overall, methanol extracts from R. officinalis and S. sclarea had the most significant antimicrobial effects against all tested oral pathogens, while Cistus spp. extracts exhibited the highest antibiofilm activity against S. mutans. Thus, combinations of these plant extracts could serve as main antimicrobial components in alternative antibacterial formulations facilitating the prevention of biofilm-related oral diseases such as caries or periodontitis.
Acknowledgments
This study was supported in part by the German Research Foundation (DFG, AL 1179/2-1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. There was no additional external funding received for this study. Bettina Spitzmüller is acknowledged for her technical assistance during the biofilm plate assay, while Marie Follo is thanked for the linguistic contribution to this manuscript.
Abbreviations
- CBA
Columbia blood agar plates
- CFU
colony forming units
- CHX
chlorhexidine
- CLSI
Clinical and Laboratory Standards Institute
- DSM
German Collection of Microorganisms and Cell Cultures
- EO
essential oil
- GTase
glucosyltransferase
- HCB
yeast-cysteine blood agar plates
- MBC
minimal bactericidal concentration
- MHB
BBL Mueller Hinton II Broth-Cation-Adjusted
- MHB-S
MHB containing 1% saccharose
- MIC
minimal inhibitory concentration
- OD
optical density
- PBP
penicillin binding protein
- QS
quorum sensing
- UAE
ultrasound assisted extraction
- WCB
Wilkins-Chalgren broth
Data Availability
All relevant data are within the paper.
Funding Statement
This study was supported in part by the German Research Foundation (DFG, AL 1179/2-1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. There was no additional external funding received for this study.
References
- 1.Borlinghaus J, Albrecht F, Gruhlke MCH, Nwachukwu ID, Slusarenko AJ. Allicin: chemistry and biological properties. Molecules 2014; 19(8):12591–618. 10.3390/molecules190812591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lemstrova R, Melichar B, Mohelnikova-Duchonova B. Therapeutic potential of taxanes in the treatment of metastatic pancreatic cancer. Cancer Chemother Pharmacol 2016; 78(6):1101–11. 10.1007/s00280-016-3058-y [DOI] [PubMed] [Google Scholar]
- 3.Wolf P. Psoralen-ultraviolet A endures as one of the most powerful treatments in dermatology: reinforcement of this 'triple-product therapy' by the 2016 British guidelines. Br J Dermatol 2016; 174(1):11–4. 10.1111/bjd.14341 [DOI] [PubMed] [Google Scholar]
- 4.Chang SY, Park JH, Kim YH, Kang JS, Min M-Y. A natural component from Euphorbia humifusa Willd displays novel, broad-spectrum anti-influenza activity by blocking nuclear export of viral ribonucleoprotein. Biochemical and Biophysical Research Communications 2016; 471(2):282–9. 10.1016/j.bbrc.2016.01.123 [DOI] [PubMed] [Google Scholar]
- 5.Cui J-M, Kang L-P, Zhao Y, Zhao J-Y, Zhang J, Pang X et al. Steroidal Saponins from the Rhizomes of Aspidistra typica. PLoS One 2016; 11(3):e0150595 10.1371/journal.pone.0150595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petiwala SM, Johnson JJ. Diterpenes from rosemary (Rosmarinus officinalis): Defining their potential for anti-cancer activity. Cancer Lett 2015; 367(2):93–102. 10.1016/j.canlet.2015.07.005 [DOI] [PubMed] [Google Scholar]
- 7.Nassiri-Asl M, Hosseinzadeh H. Review of the pharmacological effects of Vitis vinifera (Grape) and its bioactive compounds. Phytother Res 2009; 23(9):1197–204. 10.1002/ptr.2761 [DOI] [PubMed] [Google Scholar]
- 8.Mikaili P, Mojaverrostami S, Moloudizargari M, Aghajanshakeri S. Pharmacological and therapeutic effects of Mentha Longifolia L. and its main constituent, menthol. Anc Sci Life 2013; 33(2):131–8. 10.4103/0257-7941.139059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Plant List. The Plant List; 2013 [cited 2016 Dec 4]. Available from: URL: http://www.theplantlist.org/.
- 10.Breen S, Solomon PS, Bedon F, Vincent D. Surveying the potential of secreted antimicrobial peptides to enhance plant disease resistance. Front Plant Sci 2015; 6:900 10.3389/fpls.2015.00900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gyawali R, Ibrahim SA. Natural products as antimicrobial agents. Food Control 2014; 46:412–29. [Google Scholar]
- 12.Didry N, Dubreuil L, Pinkas M. Activity of thymol, carvacrol, cinnamaldehyde and eugenol on oral bacteria. Pharm Acta Helv 1994; 69(1):25–8. [DOI] [PubMed] [Google Scholar]
- 13.Hernández-Hernández E, Regalado-González C, Vázquez-Landaverde P, Guerrero-Legarreta I, Garcίa-Almendárez BE. Microencapsulation, chemical characterization, and antimicrobial activity of Mexican (Lippia graveolens H.B.K.) and European (Origanum vulgare L.) oregano essential oils. ScientificWorldJournal 2014; 2014:641814 10.1155/2014/641814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sender R, Fuchs S, Milo R. Are We Really Vastly Outnumbered? Revisiting the Ratio of Bacterial to Host Cells in Humans. Cell 2016; 164(3):337–40. 10.1016/j.cell.2016.01.013 [DOI] [PubMed] [Google Scholar]
- 15.Dewhirst FE, Chen T, Izard J, Paster BJ, Tanner ACR, Yu W-H et al. The Human Oral Microbiome. Journal of Bacteriology 2010; 192(19):5002–17. 10.1128/JB.00542-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jenkinson HF, Lamont RJ. Oral microbial communities in sickness and in health. Trends Microbiol 2005; 13(12):589–95. 10.1016/j.tim.2005.09.006 [DOI] [PubMed] [Google Scholar]
- 17.Kolenbrander PE. Oral microbial communities: biofilms, interactions, and genetic systems. Annu Rev Microbiol 2000; 54:413–37. 10.1146/annurev.micro.54.1.413 [DOI] [PubMed] [Google Scholar]
- 18.Scannapieco FA. Saliva-bacterium interactions in oral microbial ecology. Crit Rev Oral Biol Med 1994; 5(3–4):203–48. [DOI] [PubMed] [Google Scholar]
- 19.Welin-Neilands J, Svensäter G. Acid tolerance of biofilm cells of Streptococcus mutans. Appl Environ Microbiol 2007; 73(17):5633–8. 10.1128/AEM.01049-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tiwari V, Roy R, Tiwari M. Antimicrobial active herbal compounds against Acinetobacter baumannii and other pathogens. Front Microbiol 2015; 6:618 10.3389/fmicb.2015.00618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tiwari V, Tiwari D, Patel V, Tiwari M. Effect of secondary metabolite of Actinidia deliciosa on the biofilm and extra-cellular matrix components of Acinetobacter baumannii. Microb Pathog 2017; 110:345–51. 10.1016/j.micpath.2017.07.013 [DOI] [PubMed] [Google Scholar]
- 22.Chinsembu KC. Plants and other natural products used in the management of oral infections and improvement of oral health. Acta Trop 2016; 154:6–18. 10.1016/j.actatropica.2015.10.019 [DOI] [PubMed] [Google Scholar]
- 23.Hotwani K, Baliga S, Sharma K. Phytodentistry: use of medicinal plants. J Complement Integr Med 2014; 11(4):233–51. 10.1515/jcim-2013-0015 [DOI] [PubMed] [Google Scholar]
- 24.Karygianni L, Al-Ahmad A, Argyropoulou A, Hellwig E, Anderson AC, Skaltsounis AL. Natural Antimicrobials and Oral Microorganisms: A Systematic Review on Herbal Interventions for the Eradication of Multispecies Oral Biofilms. Front Microbiol 2015; 6:1529 10.3389/fmicb.2015.01529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karygianni L, Cecere M, Skaltsounis AL, Argyropoulou A, Hellwig E, Aligiannis N et al. High-level antimicrobial efficacy of representative Mediterranean natural plant extracts against oral microorganisms. Biomed Res Int 2014; 2014:839019 10.1155/2014/839019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jones D, Pell PA, Sneath PHA. Maintenance of bacteria on glass beads at -60°C to -76°C In: Kirsop BE, Doyle A, editors. Maintenance of microorganisms and cultured cells: A manual of laboratory methods. 2nd ed London: Academic Press; 1991. p. 45–50. [Google Scholar]
- 27.CLSI. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically: Approved standard. 9th ed Wayne, Pa, USA: CLSI; 2012. (Clinical and Laboratory Standards InstituteM07-A9 = 32,2). [Google Scholar]
- 28.CLSI. Methods for antimicrobial susceptibility testing of anaerobic bacteria: Approved standard. 8th ed Wayne, Pa, USA: CLSI; 2012. (Clinical and Laboratory Standards Institute; vol 32,5). [Google Scholar]
- 29.German Institute for Standardization. Clinical laboratory testing and in vitro diagnostic test systems—Susceptibility testing of infectious agents and evaluation of performance of antimicrobial susceptibility test devices—Part 1: Reference method for testing the in vitro activity of antimicrobial agents against rapidly growing aerobic bacteria involved in infectious diseases (ISO 20776–1:2006); German version EN ISO 20776–1:2006. Berlin: Beuth; 2007 2007–02.
- 30.Al-Ahmad A, Wiedmann-Al-Ahmad M, Auschill TM, Follo M, Braun G, Hellwig E et al. Effects of commonly used food preservatives on biofilm formation of Streptococcus mutans in vitro. Arch Oral Biol 2008; 53(8):765–72. 10.1016/j.archoralbio.2008.02.014 [DOI] [PubMed] [Google Scholar]
- 31.Martins N, Barros L, Santos-Buelga C, Henriques M, Silva S, Ferreira ICFR. Evaluation of bioactive properties and phenolic compounds in different extracts prepared from Salvia officinalis L. Food Chem 2015; 170:378–85. 10.1016/j.foodchem.2014.08.096 [DOI] [PubMed] [Google Scholar]
- 32.Šulniūtė V, Pukalskas A, Venskutonis PR. Phytochemical composition of fractions isolated from ten Salvia species by supercritical carbon dioxide and pressurized liquid extraction methods. Food Chem 2017; 224:37–47. 10.1016/j.foodchem.2016.12.047 [DOI] [PubMed] [Google Scholar]
- 33.Martins N, Barros L, Santos-Buelga C, Silva S, Henriques M, Ferreira ICFR. Decoction, infusion and hydroalcoholic extract of cultivated thyme: antioxidant and antibacterial activities, and phenolic characterisation. Food Chem 2015; 167:131–7. 10.1016/j.foodchem.2014.06.094 [DOI] [PubMed] [Google Scholar]
- 34.Kontogianni VG, Tomic G, Nikolic I, Nerantzaki AA, Sayyad N, Stosic-Grujicic S et al. Phytochemical profile of Rosmarinus officinalis and Salvia officinalis extracts and correlation to their antioxidant and anti-proliferative activity. Food Chem 2013; 136(1):120–9. 10.1016/j.foodchem.2012.07.091 [DOI] [PubMed] [Google Scholar]
- 35.Achour M, Mateos R, Ben Fredj M, Mtiraoui A, Bravo L, Saguem S. A Comprehensive Characterisation of Rosemary tea Obtained from Rosmarinus officinalis L. Collected in a sub-Humid Area of Tunisia. Phytochem Anal 2018; 29(1):87–100. 10.1002/pca.2717 [DOI] [PubMed] [Google Scholar]
- 36.Fernández-Ochoa Á, Borrás-Linares I, Pérez-Sánchez A, Barrajón-Catalán E, González-Álvarez I, Arráez-Román D et al. Phenolic compounds in rosemary as potential source of bioactive compounds against colorectal cancer: In situ absorption and metabolism study. Journal of Functional Foods 2017; 33:202–10. [Google Scholar]
- 37.Tsimogiannis D, Samiotaki M, Panayotou G, Oreopoulou V. Characterization of Flavonoid Subgroups and Hydroxy Substitution by HPLC-MS/MS. Molecules 2007; 12(3):593–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taamalli A, Arráez-Román D, Abaza L, Iswaldi I, Fernández-Gutiérrez A, M et al. LC-MS-based metabolite profiling of methanolic extracts from the medicinal and aromatic species Mentha pulegium and Origanum majorana. Phytochem Anal 2015; 26(5):320–30. 10.1002/pca.2566 [DOI] [PubMed] [Google Scholar]
- 39.Justesen U. Negative atmospheric pressure chemical ionisation low-energy collision activation mass spectrometry for the characterisation of flavonoids in extracts of fresh herbs. Journal of Chromatography A 2000; 902(2):369–79. [DOI] [PubMed] [Google Scholar]
- 40.Martins N, Barros L, Santos-Buelga C, Henriques M, Silva S, Ferreira ICFR. Decoction, infusion and hydroalcoholic extract of Origanum vulgare L.: different performances regarding bioactivity and phenolic compounds. Food Chem 2014; 158:73–80. 10.1016/j.foodchem.2014.02.099 [DOI] [PubMed] [Google Scholar]
- 41.Maggi F, Lucarini D, Papa F, Peron G, Dall'Acqua S. Phytochemical analysis of the labdanum-poor Cistus creticus subsp. eriocephalus (Viv.) Greuter et Burdet growing in central Italy. Biochemical Systematics and Ecology 2016; 66:50–7. [Google Scholar]
- 42.Fernández-Arroyo S, Barrajón-Catalán E, Micol V, Segura-Carretero A, Fernández-Gutiérrez A. High-performance liquid chromatography with diode array detection coupled to electrospray time-of-flight and ion-trap tandem mass spectrometry to identify phenolic compounds from a Cistus ladanifer aqueous extract. Phytochem Anal 2010; 21(4):307–13. 10.1002/pca.1200 [DOI] [PubMed] [Google Scholar]
- 43.Chinou I, Demetzos C, Harvala C, Roussakis C, Verbist JF. Cytotoxic and antibacterial labdane-type diterpenes from the aerial parts of Cistus incanus subsp. creticus. Planta Med 1994; 60(1):34–6. 10.1055/s-2006-959403 [DOI] [PubMed] [Google Scholar]
- 44.Sharifzadeh A, Shokri H. Antifungal activity of essential oils from Iranian plants against fluconazole-resistant and fluconazole-susceptible Candida albicans. Avicenna J Phytomed 2016; 6(2):215–22. [PMC free article] [PubMed] [Google Scholar]
- 45.Bouamama H, Noël T, Villard J, Benharref A, Jana M. Antimicrobial activities of the leaf extracts of two Moroccan Cistus L. species. J Ethnopharmacol 2006; 104(1–2):104–7. 10.1016/j.jep.2005.08.062 [DOI] [PubMed] [Google Scholar]
- 46.Demetzos C, Katerinopoulos H, Kouvarakis A, Stratigakis N, Loukis A, Ekonomakis C et al. Composition and Antimicrobial Activity of the Essential Oil of Cistus creticus subsp. eriocephalus. Planta Med 1997; 63:477–9. 10.1055/s-2006-957742 [DOI] [PubMed] [Google Scholar]
- 47.Anastasaki T, Demetzos C, Perdetzoglou D, Gazouli M, Loukis A, Harvala C. Analysis of labdane-type diterpenes from Cistus creticus (subsp. creticus and subsp. eriocephalus), by GC and GC-MS. Planta Med 1999; 65(8):735–9. 10.1055/s-1999-14095 [DOI] [PubMed] [Google Scholar]
- 48.Sassi AB, Harzallah-Skhiri F, Aouni M. Investigation of Some Medicinal Plants from Tunisia for Antimicrobial Activities. Pharm Biol 2008; 45(5):421–8. [Google Scholar]
- 49.Pagès M-M, Amaral L. Mechanisms of drug efflux and strategies to combat them: challenging the efflux pump of Gram-negative bacteria. Biochim Biophys Acta 2009; 1794(5):826–33. 10.1016/j.bbapap.2008.12.011 [DOI] [PubMed] [Google Scholar]
- 50.Page MGP. The role of the outer membrane of Gram-negative bacteria in antibiotic resistance: Ajax' shield or Achilles' heel? In: Coates ARM, editor. Antibiotic Resistance. Berlin, Heidelberg: Springer; 2012. p. 67–86 [Handbook of Experimental Pharmacology; vol. 211]. [DOI] [PubMed] [Google Scholar]
- 51.Nawrocki K, Crispell E, McBride S. Antimicrobial Peptide Resistance Mechanisms of Gram-Positive Bacteria. Antibiotics 2014; 3(4):461–92. 10.3390/antibiotics3040461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Munita JM, Bayer AS, Arias CA. Evolving resistance among Gram-positive pathogens. Clin Infect Dis 2015; 61 Suppl 2:S48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hannig C, Sorg J, Spitzmüller B, Hannig M, Al-Ahmad A. Polyphenolic beverages reduce initial bacterial adherence to enamel in situ. J Dent 2009; 37(7):560–6. 10.1016/j.jdent.2009.03.017 [DOI] [PubMed] [Google Scholar]
- 54.Oluwatuyi M, Kaatz GW, Gibbons S. Antibacterial and resistance modifying activity of Rosmarinus officinalis. Phytochemistry 2004; 65(24):3249–54. 10.1016/j.phytochem.2004.10.009 [DOI] [PubMed] [Google Scholar]
- 55.Hammer KA, Carson CF, Riley TV. Antimicrobial activity of essential oils and other plant extracts. J Appl Microbiol 1999; 86(6):985–90. [DOI] [PubMed] [Google Scholar]
- 56.Mahyari S, Mahyari B, Emami SA, Malaekeh-Nikouei B, Jahanbakhsh SP, Sahebkar A et al. Evaluation of the efficacy of a polyherbal mouthwash containing Zingiber officinale, Rosmarinus officinalis and Calendula officinalis extracts in patients with gingivitis: A randomized double-blind placebo-controlled trial. Complement Ther Clin Pract 2016; 22:93–8. 10.1016/j.ctcp.2015.12.001 [DOI] [PubMed] [Google Scholar]
- 57.Freires IA, Denny C, Benso B, Alencar SM de, Rosalen PL. Antibacterial Activity of Essential Oils and Their Isolated Constituents against Cariogenic Bacteria: A Systematic Review. Molecules 2015; 20(4):7329–58. 10.3390/molecules20047329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Firuzi O, Miri R, Asadollahi M, Eslami S, Jassbi AR. Cytotoxic, Antioxidant and Antimicrobial Activities and Phenolic Contents of Eleven Salvia Species from Iran. Iranian Journal of Pharmaceutical Research 2013; 12(4):801–10. [PMC free article] [PubMed] [Google Scholar]
- 59.Stagos D, Portesis N, Spanou C, Mossialos D, Aligiannis N, Chaita E et al. Correlation of total polyphenolic content with antioxidant and antibacterial activity of 24 extracts from Greek domestic Lamiaceae species. Food Chem Toxicol 2012; 50(11):4115–24. 10.1016/j.fct.2012.08.033 [DOI] [PubMed] [Google Scholar]
- 60.Bardajί DKR, Reis EB, Medeiros TCT, Lucarini R, Crotti AEM, Martins CHG. Antibacterial activity of commercially available plant-derived essential oils against oral pathogenic bacteria. Nat Prod Res 2016; 30(10):1178–81. 10.1080/14786419.2015.1043630 [DOI] [PubMed] [Google Scholar]
- 61.Kuźma Ł, Różalski M, Walencka E, Różalska B, Wysokińska H. Antimicrobial activity of diterpenoids from hairy roots of Salvia sclarea L.: salvipisone as a potential anti-biofilm agent active against antibiotic resistant Staphylococci. Phytomedicine 2007; 14(1):31–5. 10.1016/j.phymed.2005.10.008 [DOI] [PubMed] [Google Scholar]
- 62.Walencka E, Rozalska S, Wysokinska H, Rozalski M, Kuzma L, Rozalska B. Salvipisone and aethiopinone from Salvia sclarea hairy roots modulate staphylococcal antibiotic resistance and express anti-biofilm activity. Planta Med 2007; 73(6):545–51. 10.1055/s-2007-967179 [DOI] [PubMed] [Google Scholar]
- 63.Coccimiglio J, Alipour M, Jiang M-H, Gottardo C, Suntres Z. Antioxidant, Antibacterial, and Cytotoxic Activities of the Ethanolic Origanum vulgare Extract and Its Major Constituents. Oxid Med Cell Longev 2016; 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gortzi O, Lalas S, Chinou I, Tsaknis J. Reevaluation of antimicrobial and antioxidant activity of Thymus spp. extracts before and after encapsulation in liposomes. J Food Prot 2006; 69(12):2998–3005. [DOI] [PubMed] [Google Scholar]
- 65.Chorianopoulos N, Kalpoutzakis E, Aligiannis N, Mitaku S, Nychas M-J, Haroutounian SA. Essential oils of Satureja, Origanum, and Thymus species: chemical composition and antibacterial activities against foodborne pathogens. J Agric Food Chem 2004; 52(26):8261–7. 10.1021/jf049113i [DOI] [PubMed] [Google Scholar]
- 66.De Martino L, Bruno M, Formisano C, De Feo V, Napolitano F, Rosselli S et al. Chemical composition and antimicrobial activity of the essential oils from two species of Thymus growing wild in southern Italy. Molecules 2009; 14(11):4614–24. 10.3390/molecules14114614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tsai P-J, Tsai T-H, Ho S-C. In vitro inhibitory effects of rosemary extracts on growth and glucosyltransferase activity of Streptococcus sobrinus. Food Chem 2007; 105(1):311–6. [Google Scholar]
- 68.Quave CL, Plano LRW, Pantuso T, Bennett BC. Effects of extracts from Italian medicinal plants on planktonic growth, biofilm formation and adherence of methicillin-resistant Staphylococcus aureus. J Ethnopharmacol 2008; 118(3):418–28. 10.1016/j.jep.2008.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Horner C, Mawer D, Wilcox M. Reduced susceptibility to chlorhexidine in staphylococci: is it increasing and does it matter? J Antimicrob Chemother 2012; 67(11):2547–59. 10.1093/jac/dks284 [DOI] [PubMed] [Google Scholar]
- 70.Meyer B, Cookson B. Does microbial resistance or adaptation to biocides create a hazard in infection prevention and control? J Hosp Infect 2010; 76(3):200–5. 10.1016/j.jhin.2010.05.020 [DOI] [PubMed] [Google Scholar]
- 71.Freires IA, Rosalen PL. How Natural Product Research has Contributed to Oral Care Product Development? A Critical View. Pharm Res 2016; 33(6):1311–7. 10.1007/s11095-016-1905-5 [DOI] [PubMed] [Google Scholar]
- 72.Agrawal V, Kapoor S, Agrawal I. Critical Review on Eliminating Endodontic Dental Infections Using Herbal Products. J Diet Suppl 2017; 14(2):229–40. 10.1080/19390211.2016.1207004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.