Abstract
Background
The extent to which the presence and extent of subclinical atherosclerosis by coronary computed tomography angiography influences a potential mortality benefit of statin is unknown. We evaluated the relationship between statin therapy, mortality, and subclinical atherosclerosis.
Methods
In the CONFIRM study, patients with normal or non-obstructive plaque (<50% diameter stenosis) for whom data on baseline statin use was available were included. Coronary artery calcium (CAC) was quantified using the Agatston score. The extent of non-obstructive coronary atherosclerosis was quantified using the segment involvement score (SIS). 8,016 patients were followed for a median of 2.5 years with analysis of all-cause mortality and major adverse cardiac events (MACE) including all-cause mortality, myocardial infarction, unstable angina, target vessel revascularization, and coronary artery disease-related hospitalization.
Results
1.2% of patients experienced all-cause mortality. Patients not on baseline statin therapy had a stepwise increased risk of all-cause mortality by CAC (relative to CAC = 0; CAC 1–99: hazard ratio [HR] 1.65, CAC 100–299: HR 2.19, and CAC≥300: HR 2.98) or SIS (relative to SIS = 0; SIS 1: HR 1.62, SIS 2–3: 2.48 and SIS≥4: 2.95). Conversely, in patients on baseline statin therapy, there was no significant increase in mortality risk with increasing CAC (p value for interaction = 0.049) or SIS (p value for interaction = 0.007). The incidence of MACE was 2.1%. Similar to the all-cause mortality, the risk of MACE was increased with CAC or SIS strata in patient not on baseline statin therapy. However, this relation was not observed in patient on baseline statin therapy.
Conclusion
In individuals with non-obstructive coronary artery disease, increased risk of adverse events occurs with increasing CAC or SIS who are not on baseline statin therapy. Statin therapy is associated with a mitigation of risk of cardiac events in the presence of increasing atherosclerosis, with no particular threshold of disease burden.
Introduction
Coronary artery calcium (CAC) scoring is a robust method for risk prediction of major adverse cardiac events (MACE), and current societal guidelines recommend a threshold of ≥300 Agatston units for consideration of statin treatment [1]. Coronary computed tomographic angiography (CCTA) is a contrast-enhanced anatomic imaging method that permits direct visualization of both calcified and non-calcified atherosclerotic plaque that also allows for effective prognostication of risk of MACE [2–7]. In patients with non-obstructive coronary artery disease (CAD) by CCTA, the comparative effect of statin therapy on MACE for individuals with evident CAC or atherosclerotic plaque by CCTA is unknown. Thus, in a prospective multinational cohort of individuals undergoing CAC and CCTA without obstructive CAD, we sought to identify whether there was a threshold of CAC- and CCTA-identified CAD wherein statin therapy was associated with reduced mortality risk.
Materials and methods
Study population
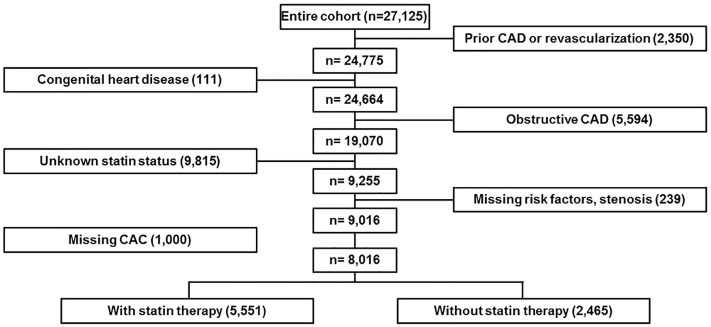
Details of the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter) study have been described elsewhere [8]. In brief, 27,125 consecutive patients enrolled in this global multicenter cardiac CT registry underwent coronary CCTA at 12 cluster sites in 6 countries (Canada, Germany, Italy, Korea, Switzerland, United States) between February 2003 and December 2009. Patients with a history of myocardial infarction or coronary revascularization (coronary artery bypass and/or percutaneous coronary intervention) (n = 2,350), or congenital heart disease (n = 111) were excluded from analysis. A further 16,648 patients were excluded including those with obstructive CAD (≥50% luminal diameter stenosis) as diagnosed by CCTA (n = 5,594), and those with missing data regarding the use of statins (n = 9,815), risk factors (n = 239), or CAC (n = 1000) were also excluded. A total of 8,016 patients met the inclusion criteria and comprised the study sample (Fig 1). The Institutional Review Board of Weil Cornell Medical College approved the study and its procedures, including coordination with other ethics committees. Each of the contributing centers received ethics approval from their respective institutional review boards, and written informed consent was obtained from the study participants.
Fig 1. Flow diagram for patient enrollment.
A total of 8,016 patients met the inclusion criteria.
Study variables
At the time of CCTA examination, patient’s information was prospectively collected and recorded in site-specific case report forms (CRFs). Patients treated for or with a prior diagnosis of hypertension, diabetes, or dyslipidemia, a family history of premature CAD or a history of smoking were categorized as having that cardiovascular risk factor. Specifically, systemic arterial hypertension was defined as a documented history of high blood pressure or treatment with antihypertensive medication. Diabetes mellitus was defined as diagnosis of diabetes confirmed previously by a physician and/or use of insulin or oral hypoglycemic agents. Dyslipidemia was defined as known but untreated dyslipidemia or current treatment with lipid-lowering medications. A family history of premature CAD was defined as a primary relative with a diagnosis early in life (i.e., mother <65 years of age or father <55 years of age). A positive smoking history was defined as current smoking or cessation of smoking within 3 months of examination. Self-reported use of statin medication was evaluated at the time of enrolment.
Definition of CCTA measures
Image data were acquired by CT scanners of ≥64-detector rows. Patient preparation, acquisition, and interpretation of CCTA and CAC score data were performed in accordance with the Society of Cardiovascular Computed Tomography Guidelines [9]. For the present analysis, coronary stenoses were defined as none (0% stenosis without plaque) and non-obstructive (1–49% diameter stenosis) CAD. The CAC score was determined based on the scoring system described by Agatston et al. [10]. The CAC score was categorized into 4 strata as: 0, 1–99, 100–299, and ≥300 according to current guidelines [11]. The extent of atherosclerotic burden was determined by a segment-involvement score (SIS) based on a 16-segment coronary model, which reflects the number of coronary segments possessing atherosclerotic plaque (minimum = 0; maximum = 16) [12]. SIS was also categorized as 0, 1, 2–3, and ≥4 segments in the current study population.
Patient follow-up
Primary endpoint was all-cause mortality and secondary endpoint was major adverse cardiac events (MACE). According to the study protocol, MACE was defined as all-cause mortality, myocardial infarction, unstable angina, target vessel revascularization, and CAD-related hospitalization. Event data were ascertained at each local institution by direct patient query, through medical records at non-US sites or national all-cause mortality records at US sites. Data coordinating center and independent biostatistician checked the database to enhance data quality, and they only knew the participants only by study identifier number.
Statistical methods
Continuous variables are presented as means with standard deviations, and categorical variables as counts with proportions. Between-group differences according to statin use were compared by use of a Wilcoxon rank-sum test for continuous variables, and chi-square test for categorical variables. Unadjusted comparisons of the primary outcome according to the presence and magnitude of the CAC and SIS scores stratified by statin therapy were performed using Kaplan-Meier survival curves with log-rank tests. A multivariable Cox proportional regression model reporting hazard ratios with 95% confidence intervals (95% CI) was employed to examine differences in the risk of all-cause mortality and MACE according to statin therapy, while adjusting for age, gender, and traditional cardiovascular risk factors such as hypertension, diabetes mellitus, dyslipidemia, family history and current smoking. All statistical analyses were performed using SPSS (version 19.0.0, IBM, New York). A two-tailed p value <0.05 was considered statistically significant.
Results
Study population
Of 8,016 patients, the incidence of all-cause mortality was 1.2% (99 events) and that of MACE was 2.1% (165 events) during a median follow-up of 2.5 years. Baseline characteristics of the study cohort are presented in Tables 1 and 2. Patients on baseline statin therapy tended to be older and have more CAD risk factors (p <0.001 for all) compared with those who were not on statin therapy. Both higher CAC and SIS scores were associated with older age as well as a higher prevalence of hypertension, diabetes mellitus, and dyslipidemia.
Table 1. Baseline characteristics.
| Overall | Without statin | With statin | p value | |
|---|---|---|---|---|
| (N = 8016) | (N = 5551) | (N = 2465) | ||
| Age | 57.1±11.8 | 55.6±12.2 | 60.7±10.2 | <0.001 |
| Male gender | 4152 (51.8) | 2895 (52.2) | 1257 (51.0) | 0.338 |
| Hypertension | 3930 (49.0) | 2513 (45.3) | 1417 (57.5) | <0.001 |
| Diabetes mellitus | 978 (12.2) | 530 (9.5) | 448 (18.2) | <0.001 |
| Dyslipidemia | 4544 (56.7) | 2500 (45.0) | 2044 (82.9) | <0.001 |
| Family history | 1982 (24.7) | 1294 (23.3) | 688 (27.9) | <0.001 |
| Current smoking | 1277 (15.9) | 917 (16.5) | 360 (14.6) | 0.031 |
| Body mass index | 26.3±4.7 | 26.3±4.8 | 26.3±4.7 | 0.688 |
| Renal insufficiency | 16 (0.2) | 10 (0.2) | 6 (0.2) | 0.591 |
| Peripheral vascular disease | 112 (1.4) | 83 (1.5) | 29 (1.2) | 0.205 |
| Cerebrovascular disease | 73 (0.9) | 51 (0.9) | 22 (0.9) | 0.965 |
| Total cholesterol | 191.8±43.0 | 192.4±42.9 | 190.3±43.1 | 0.089 |
| LDL cholesterol | 118.0±35.8 | 118.3±36.3 | 117.3±34.6 | 0.332 |
| HDL cholesterol | 53.6±16.3 | 53.9±16.6 | 53.1±15.6 | 0.066 |
| CAC | 65.6±242.1 | 46.8±198.6 | 108.1±314.9 | <0.001 |
| SIS | 1.0±1.7 | 0.7±1.5 | 1.5±2.0 | <0.001 |
LDL, low-density lipoprotein; HDL, high-density lipoprotein; CAC, coronary artery calcium; SIS, segment involvement score.
Table 2. Baseline characteristics by CAC or SIS categories.
| CAC 0 | CAC 1–99 | CAC 100–299 | CAC ≥300 | p value | SIS 0 | SIS 1 | SIS 2–3 | SIS ≥4 | p value | |
|---|---|---|---|---|---|---|---|---|---|---|
| (N = 4858) | (N = 2060) | (N = 623) | (N = 475) | (N = 4969) | (N = 1254) | (N = 1097) | (N = 696) | |||
| Age | 53.5±11.5 | 60.9±9.9 | 65.1±9.1 | 68.0±9.4 | <0.001 | 54.0±11.6 | 60.3±10.4 | 62.3±9.9 | 65.6±10.1 | <0.001 |
| Male gender | 2273 (46.8) | 1190 (57.8) | 381 (61.2) | 308 (64.8) | <0.001 | 2343 (47.2) | 698 (55.7) | 668 (60.9) | 443 (63.6) | <0.001 |
| Hypertension | 2128 (43.8) | 1136 (55.1) | 366 (58.7) | 300 (63.2) | <0.001 | 2204 (44.4) | 665 (53.0) | 611 (55.7) | 450 (64.7) | <0.001 |
| Diabetes mellitus | 423 (8.7) | 338 (16.4) | 111 (17.8) | 106 (22.3) | <0.001 | 461 (9.3) | 173 (13.8) | 198 (18.0) | 146 (21.0) | <0.001 |
| Dyslipidemia | 2561 (52.7) | 1277 (62.0) | 422 (67.7) | 284 (59.8) | <0.001 | 2620 (52.7) | 782 (62.4) | 684 (62.4) | 458 (65.8) | <0.001 |
| Family history | 1176 (24.2) | 507 (24.6) | 169 (27.1) | 130 (27.4) | 0.219 | 1195 (24.0) | 290 (23.1) | 322 (29.4) | 175 (25.1) | 0.001 |
| Current smoking | 757 (15.6) | 327 (15.9) | 103 (16.5) | 90 (18.9) | 0.279 | 777 (15.6) | 202 (16.1) | 174 (15.9) | 124 (17.8) | 0.532 |
| Body mass index | 26.4±4.8 | 26.0±4.5 | 26.2±5.0 | 26.2±4.7 | 0.012 | 26.4±4.7 | 26.2±4.9 | 26.1±4.9 | 25.9±4.6 | 0.007 |
| Renal insufficiency | 9 (0.2) | 5 (0.2) | 1 (0.2) | 1 (0.2) | 0.968 | 8 (0.2) | 3 (0.2) | 5 (0.5) | 0 | 0.201 |
| Peripheral vascular disease | 70 (1.4) | 22 (1.1) | 9 (1.4) | 11 (2.3) | 0.259 | 66 (1.3) | 22 (1.8) | 11 (1.0) | 13 (1.9) | 0.242 |
| Cerebrovascular disease | 38 (0.8) | 17 (0.8) | 8 (1.3) | 10 (2.1) | 0.187 | 33 (0.7) | 16 (1.3) | 12 (1.1) | 12 (1.7) | 0.201 |
| Total cholesterol | 194.5±45.0 | 187.7±39.8 | 183.8±37.0 | 189.6±37.1 | <0.001 | 194.2±45.1 | 187.3±42.1 | 187.3±34.5 | 187.2±36.6 | <0.001 |
| LDL cholesterol | 119.8±37.3 | 115.6±33.1 | 112.2±31.3 | 116.0±32.5 | <0.001 | 119.8±38.0 | 114.1±31.7 | 114.9±29.2 | 115.6±31.5 | <0.001 |
| HDL cholesterol | 54.4±16.6 | 52.2±15.9 | 52.9±16.4 | 52.4±13.8 | <0.001 | 54.0±16.4 | 53.6±16.9 | 53.0±15.8 | 52.2±15.1 | 0.115 |
| CAC | 0 | 29.9±27.4 | 174.9±56.3 | 748.1±671.9 | <0.001 | 9.7±123.5 | 45.4±141.8 | 121.3±239.9 | 413.8±538.8 | <0.001 |
| SIS | 0.2±0.6 | 1.4±1.4 | 3.0±2.0 | 4.5±2.5 | <0.001 | 0 | 1.0±0.0 | 2.4±0.5 | 5.4±1.7 | <0.001 |
LDL, low-density lipoprotein; HDL, high-density lipoprotein; CAC, coronary artery calcium; SIS, segment involvement score.
CAC and statin therapy
In the overall population, there was a stepwise increased risk of all-cause mortality by strata of CAC after adjustment for covariates (Table 3). This association was influenced by the presence of baseline statin therapy (Fig 2, Table 3). Specifically, the stepwise relationship between increasing CAC and increased mortality was preserved in patients not on baseline statin therapy. However, there was no significant association between individual strata of CAC and all-cause mortality after adjustment for clinical variables, although there was a borderline association of increased risk for CAC≥300 (HR = 3.05, 95% CI 0.92–10.09, p = 0.07). As compared to patients taking statins, patients not on statin therapy had significantly higher risks of all-cause mortality according to increasing CAC strata except for those with CAC ≥300 (p value for interaction = 0.049).
Table 3. Adjusted association between all-cause mortality, CAC, SIS, and baseline statin therapya.
| Overall population | Without statin therapy | With statin therapy | ||||
|---|---|---|---|---|---|---|
| Hazard ratio (95% CI) |
p value | Hazard ratio (95% CI) |
p value | Hazard ratio (95% CI) |
p value | |
| CAC 0 | 1.00 | 1.00 | 1.00 | |||
| CAC 1–99 | 1.29 (0.76–2.17) |
0.346 | 1.65 (0.92–2.95) |
0.097 | 0.56 (0.17–1.91) |
0.357 |
| CAC 100–299 | 1.90 (1.00–3.61) |
0.052 | 2.19 (1.04–4.65) |
0.041 | 1.19 (0.34–4.19) |
0.789 |
| CAC ≥300 | 2.86 (1.55–5.27) |
<0.001 | 2.98 (1.44–6.16) |
0.004 | 3.05 (0.92–10.09) |
0.068 |
| SIS 0 | 1.00 | 1.00 | 1.00 | |||
| SIS 1 | 1.54 (0.85–2.78) |
0.154 | 1.62 (0.81–3.24) |
0.171 | 1.37 (0.44–4.29) |
0.586 |
| SIS 2–3 | 2.25 (1.32–3.83) |
0.003 | 2.48 (1.34–4.61) |
0.004 | 1.62 (0.56–4.71) |
0.375 |
| SIS ≥4 | 2.07 (1.13–3.77) |
0.019 | 2.95 (1.50–5.81) |
0.002 | 0.84 (0.21–3.33) |
0.800 |
CAC, coronary artery calcium; SIS, segment involvement score.
aAdjusted for age, male gender, hypertension, diabetes mellitus, dyslipidemia, family history and current smoking.
Fig 2. Kaplan-Meier survival curves for all-cause mortality-free survival.
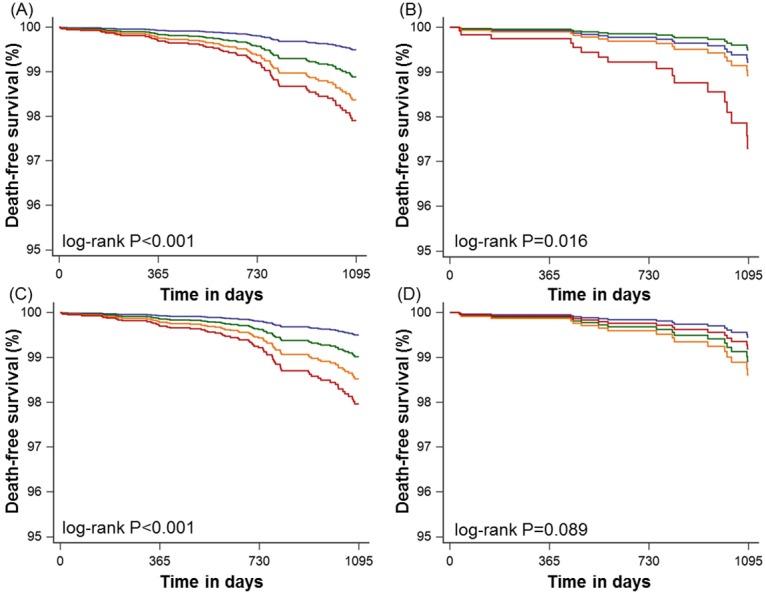
(A) coronary artery calcium score categories for patients without statin therapy, (B) coronary artery calcium score categories for patients with statin therapy, (C) segment involvement score categories for patients without statin therapy, and (D) segment involvement score categories for patients with statin therapy. Blue, green, orange, and red lines indicate 0, 1–99, 100–299, and ≥300 coronary artery calcium score categories. Blue, green, orange, and red lines indicate 0, 1, 2–3, and ≥4 segment involvement score categories.
Although the risk of MACE was increased by strata of CAC in the overall population, this finding was attenuated according to the baseline statin therapy (Table 4).
Table 4. Adjusted association between major adverse cardiac events (MACE)a, CAC, SIS, and baseline statin therapyb.
| Overall population | Without statin therapy | With statin therapy | ||||
|---|---|---|---|---|---|---|
| Hazard ratio (95% CI) |
p value | Hazard ratio (95% CI) |
p value | Hazard ratio (95% CI) |
p value | |
| CAC 0 | 1.00 | 1.00 | 1.00 | |||
| CAC 1–99 | 1.62 (1.07–2.45) |
0.022 | 2.15 (1.30–3.56) |
0.003 | 0.76 (0.36–1.59) |
0.462 |
| CAC 100–299 | 2.64 (1.60–4.37) |
<0.001 | 2.54 (1.28–5.01) |
0.007 | 2.16 (1.03–4.55) |
0.042 |
| CAC ≥300 | 4.63 (2.87–7.45) |
<0.001 | 4.91 (2.65–9.11) |
<0.001 | 3.84 (1.81–8.13) |
<0.001 |
| SIS 0 | 1.00 | 1.00 | 1.00 | |||
| SIS 1 | 2.22 (1.43–3.47) |
<0.001 | 1.82 (1.02–3.24) |
0.043 | 2.65 (1.30–5.43) |
0.008 |
| SIS 2–3 | 2.84 (1.85–4.37) |
<0.001 | 3.13 (1.86–5.27) |
<0.001 | 1.95 (0.91–4.18) |
0.088 |
| SIS ≥4 | 3.48 (2.18–5.55) |
<0.001 | 3.19 (1.75–5.82) |
<0.001 | 3.54 (1.67–7.48) |
0.001 |
CAC, coronary artery calcium; SIS, segment involvement score.
aMACE was defined as a composite of all-cause mortality, myocardial infarction, unstable angina, target vessel revascularization, and coronary artery disease-related hospitalization
bAdjusted for age, male gender, hypertension, diabetes mellitus, dyslipidemia, family history and current smoking.
SIS and statin therapy
In the overall population, there was a stepwise increased risk of all-cause mortality by increasing strata of SIS after adjustment of covariates (Table 3). Compared to patients with SIS = 0, patients with SIS >1 was associated with higher risk of all-cause mortality (p <0.05). This association was influenced by the presence of baseline statin therapy (Fig 2, Table 3). Relative to those with SIS = 0 not taking baseline statins, the adjusted risk of all-cause mortality increased stepwise with increasing SIS, with significantly increased mortality hazard for SIS 2–3 and SIS ≥4. Conversely, this stepwise association was attenuated by the presence of baseline statin therapy (p value for interaction = 0.007). An increased mortality hazard was not observed in patients with any degree of SIS on baseline statin therapy.
A stepwise increased risk of MACE by increasing strata of SIS was also observed in the overall population (Table 4). Compared to patients with SIS = 0, patients with SIS ≥1 was associated with higher risk of MACE (p <0.05). Relative to those with SIS = 0 not taking baseline statins, the adjusted risk of MACE was significantly increased in patients with SIS ≥1. However, this association was abated in patients with statin therapy.
Discussion
In this prospective multinational cohort study of individuals undergoing CCTA, we identified a stepwise increased risk of all-cause mortality for individuals with increasing atherosclerotic burden despite the absence of anatomically obstructive CAD. Importantly, this association was modified by the presence or absence of baseline statin therapy. In contrast to individuals not on baseline statin therapy, the baseline use of statins was associated with a mitigation of increased mortality risk despite the presence or burden of non-obstructive atherosclerosis. These findings support the notion that statins may be beneficial in even patients with lower degrees of subclinical atherosclerosis as detected by CCTA.
Prior evidence has demonstrated that a substantial proportion of cardiac events arise from non-obstructive coronary stenoses [13, 14]. For instance, the PROSPECT (Providing Regional Observations to Study Predictors of Events in the Coronary Tree) study observed that many cardiac events arise from angiographic non-culprit lesions, especially those with high plaque burden and thin-cap fibroatheroma detected by gray-scale intravascular ultrasound [15]. Longitudinal data has further demonstrated an increased event risk in patients with non-obstructive CAD as detected by invasive angiography or CCTA [16, 17]. Accordingly, the present investigation of patients with non-obstructive CAD observed an incremental occurrence of mortality according to increasing CAC or SIS in patients not on statin therapy. These findings are clinically significant, in that most conventional testing (e.g. stress testing) for CAD may not detect non-obstructive atherosclerosis.
In the past decade, numerous randomized controlled trials have documented that statin therapy not only prevents cardiovascular events but also Finimproves survival in patients with varying degrees of clinical CAD, although these trials did not specifically study patients with anatomically non-obstructive CAD [18–21]. Statins are the leading candidate for pharmacologic prevention in such patients based on the observation that statins could slow disease progression and elicit stabilization of vulnerable plaque [22, 23]. Hoffmann et al. [24] evaluated the influence of statins on plaque progression by volumetric measurement using CCTA, and found that statins significantly slowed the growth of non-calcified plaques after adjusting for LDL-C levels and cardiac risk factors. It can be argued that the importance of statin therapy in non-significant stenosis was demonstrated in the FAME 2 (Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2) study, in which patients who had been deferred with functionally non-significant lesions were treated to the target of LDL-C <70 mg/dl with clinical outcomes as favorable as those associated with revascularization [25]. As well as plaque stabilization and regression, statins act beneficially through different pleiotropic effects on inflammation, fibrosis, endothelial function, thrombosis, and coagulation. Via these mechanisms, statin might also contribute to the reduction in all-cause mortality.
In light of this evidence, recent guidelines suggest that high CAC (i.e., greater than 300 Agatston units) should be taken into incorporated into statin decision-making in certain primary prevention settings [1]. The results of the present study suggest potential benefit for patients with even lower degrees of CAC or non-obstructive CAD by CCTA [26]. Importantly, we identified no lower limit of CAC wherein statin therapy did not mitigate mortality risk. These findings suggest that a binary cutoff of CAC≥300 for guiding statin treatment may not be warranted, as those with lower scores appear to also derive significant risk attenuation. Furthermore, this attenuation of risk was also observed in patients with SIS>1 on baseline statins, which extends the hypothesis that any degree of atherosclerosis by CCTA should factor into statin decision-making.
In the use of statin for the primary prevention of cardiovascular disease, there is still the issue of gender-dependent efficacy. Recent meta-analysis including 174,000 patients showed the effect of statin therapy on mortality and cardiac events were comparable among women and men, matched for cardiovascular risk [27]. When we analyzed the association between adverse events and statin according to gender, similar benefit for men and women was shown (p value for interaction = 0.127).
This study is not without limitations. Because specific causes of death for each patient were not uniformly available at all sites, this does not include the cause of death and was based on the all-cause mortality not cardiovascular death. Although coronary heart disease remains the most common cause of death in developed countries, it is not possible to enucleate the proportion of deaths which are originated from cardiovascular cause. However, this endpoint is not affected by bias from misclassification of cause of death. And risk factors such as hypertension, diabetes mellitus, dyslipidemia and smoking can contribute to all-cause mortality via additional non-cardiovascular mechanisms. Therefore, the primary endpoint of this study can be an appropriate endpoint to follow. Information regarding statin use only was available for the baseline time point. Analysis according to the treatment patterns of statin can be useful to understand the mitigation of cardiac events. However, data were lacking with regards to statin type and dosage, treatment indication, and duration of therapy. Further, changes in statin medication use that may have occurred beyond baseline CCTA were unavailable. However, that post-test initiation of statins in patients with newly discovered atherosclerosis would likely have resulted in a greater attenuation in risk and a reduction in differences. It is further doubtful that patients on statins at baseline with had evidence of atherosclerotic plaque by CCTA would have had their treatment stopped. Finally, there was the lack of follow-up CCTA to evaluate the progression (or regression) of atherosclerotic burden or change of plaque composition based on statin therapy. In a previous publication, statin use was associated with an increased prevalence and burden of coronary plaques possessing calcium [28]. However, the serial association of plaque composition type to the longitudinal effect of statin was not also addressed. Repeat CCTA for such reasons is not clinically recommended at this point. Although the observational design of the study renders our findings hypothesis-generating, the large multinational cohort increases the generalizability of these findings and augments the paucity of available literature on this topic. Additional large-scale randomized controlled trials designed to evaluate the impact of early statin therapy on outcomes in patients with non-obstructive CAD by CCTA appear warranted. Also, fractional flow reserve (FFR) CT can be useful to overcome the limitation of CCTA to detect coronary stenosis. Current CT has decreased accuracy in the setting of significant calcification and can’t evaluate lesion-specific ischemia. Therefore, FFR CT-based temporal change of anatomy and physiology can be helpful to clarify the effect of statin in CAD.
In conclusion, in this prospective multinational study of patients presenting with anatomically non-obstructive CAD, a heightened risk of adverse cardiac events including all-cause mortality was observed with increasing CAC and SIS among patients not on statin therapy at baseline. This stepwise risk was attenuated among patients on baseline statin therapy after adjustment for clinical covariates. Although we await further confirmation, the current findings are promising in that statin therapy may be associated with mitigating the risk of adverse cardiac events among non-obstructive CAD patients, with no particular threshold of atherosclerotic disease burden.
Supporting information
This shows the rationale and design of study.
(DOCX)
(PDF)
Data Availability
CONFIRM registry is a multinational multi-centers observation study that collects data from 12 centers in 6 countries, and the right to the raw material is in each center and the entire PI is Dr. James Min. The researcher was authorized to use the optional material applicable to this study in the entire registry group under consultation with Dr. Min for the idea of the submission. Therefore, anyone who wants to use the study data can contact the PI of this study, Dr. Min (jkm2001@med.cornell.edu), or 1st author Dr. Yun-Kyeong Cho (mk1997@dsmc.or.kr).
Funding Statement
Dr. James K. Min is supported by the National Institute of Health (Bethesda, MD, USA) under grant number R01HL115150 (https://www.nih.gov/grants-funding). This research was also supported by the Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (MSIP) under grant No. 2012027176 to HJC (http://english.msip.go.kr/). This study was also funded, in part, by a generous gift from the Dalio Institute of Cardiovascular Imaging (New York, NY) and the Michael Wolk Foundation (New York, NY) (https://hearthealth.weillcornell.org/about-us/dalio-institute).
References
- 1.Stone NJ, Robinson J, Lichtenstein AH, Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2013. 10.1161/01.cir.0000437738.63853.7a .24222016 [Google Scholar]
- 2.de Azevedo CF, Hadlich MS, Bezerra SG, Petriz JL, Alves RR, de Souza O, et al. Prognostic value of CT angiography in patients with inconclusive functional stress tests. JACC Cardiovascular imaging. 2011;4(7):740–51. 10.1016/j.jcmg.2011.02.017 . [DOI] [PubMed] [Google Scholar]
- 3.Habib PJ, Green J, Butterfield RC, Kuntz GM, Murthy R, Kraemer DF, et al. Association of cardiac events with coronary artery disease detected by 64-slice or greater coronary CT angiography: a systematic review and meta-analysis. International journal of cardiology. 2013;169(2):112–20. 10.1016/j.ijcard.2013.08.096 . [DOI] [PubMed] [Google Scholar]
- 4.de Graaf MA, Broersen A, Ahmed W, Kitslaar PH, Dijkstra J, Kroft LJ, et al. Feasibility of an automated quantitative computed tomography angiography-derived risk score for risk stratification of patients with suspected coronary artery disease. Am J Cardiol. 2014;113(12):1947–55. 10.1016/j.amjcard.2014.03.034 . [DOI] [PubMed] [Google Scholar]
- 5.Bittencourt MS, Hulten E, Ghoshhajra B, O’Leary D, Christman MP, Montana P, et al. Prognostic value of nonobstructive and obstructive coronary artery disease detected by coronary computed tomography angiography to identify cardiovascular events. Circulation Cardiovascular imaging. 2014;7(2):282–91. 10.1161/CIRCIMAGING.113.001047 . [DOI] [PubMed] [Google Scholar]
- 6.Min JK, Labounty TM, Gomez MJ, Achenbach S, Al-Mallah M, Budoff MJ, et al. Incremental prognostic value of coronary computed tomographic angiography over coronary artery calcium score for risk prediction of major adverse cardiac events in asymptomatic diabetic individuals. Atherosclerosis. 2014;232(2):298–304. 10.1016/j.atherosclerosis.2013.09.025 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmed K, Jeong MH, Chakraborty R, Hong YJ, Sim DS, Hwang SH, et al. Percutaneous coronary intervention with drug-eluting stent implantation vs. coronary artery bypass grafting for multivessel coronary artery disease in metabolic syndrome patients with acute myocardial infarction. Circ J. 2012;76(3):721–8. . [DOI] [PubMed] [Google Scholar]
- 8.Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah MH, Berman DS, et al. Rationale and design of the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter) Registry. Journal of cardiovascular computed tomography. 2011;5(2):84–92. 10.1016/j.jcct.2011.01.007 . [DOI] [PubMed] [Google Scholar]
- 9.Raff GL, Abidov A, Achenbach S, Berman DS, Boxt LM, Budoff MJ, et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. Journal of cardiovascular computed tomography. 2009;3(2):122–36. 10.1016/j.jcct.2009.01.001 . [DOI] [PubMed] [Google Scholar]
- 10.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. Journal of the American College of Cardiology. 1990;15(4):827–32. . [DOI] [PubMed] [Google Scholar]
- 11.Greenland P, LaBree L, Azen SP, Doherty TM, Detrano RC. Coronary artery calcium score combined with Framingham score for risk prediction in asymptomatic individuals. JAMA: the journal of the American Medical Association. 2004;291(2):210–5. 10.1001/jama.291.2.210 . [DOI] [PubMed] [Google Scholar]
- 12.Min JK, Shaw LJ, Devereux RB, Okin PM, Weinsaft JW, Russo DJ, et al. Prognostic value of multidetector coronary computed tomographic angiography for prediction of all-cause mortality. J Am Coll Cardiol. 2007;50(12):1161–70. 10.1016/j.jacc.2007.03.067 . [DOI] [PubMed] [Google Scholar]
- 13.Abdulla J, Asferg C, Kofoed KF. Prognostic value of absence or presence of coronary artery disease determined by 64-slice computed tomography coronary angiography a systematic review and meta-analysis. The international journal of cardiovascular imaging. 2011;27(3):413–20. 10.1007/s10554-010-9652-x . [DOI] [PubMed] [Google Scholar]
- 14.Nakazato R, Arsanjani R, Achenbach S, Gransar H, Cheng VY, Dunning A, et al. Age-related risk of major adverse cardiac event risk and coronary artery disease extent and severity by coronary CT angiography: results from 15 187 patients from the International Multisite CONFIRM Study. European heart journal cardiovascular Imaging. 2014;15(5):586–94. 10.1093/ehjci/jet132 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stone GW, Maehara A, Lansky AJ, de Bruyne B, Cristea E, Mintz GS, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364(3):226–35. Epub 2011/01/21. 10.1056/NEJMoa1002358 . [DOI] [PubMed] [Google Scholar]
- 16.Schulman-Marcus J, B OH, Gransar H, Lin F, Valenti V, Cho I, et al. Sex-Specific Associations Between Coronary Artery Plaque Extent and Risk of Major Adverse Cardiovascular Events: The CONFIRM Long-Term Registry. JACC Cardiovascular imaging. 2016;9(4):364–72. 10.1016/j.jcmg.2016.02.010 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maddox TM, Stanislawski MA, Grunwald GK, Bradley SM, Ho PM, Tsai TT, et al. Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA: the journal of the American Medical Association. 2014;312(17):1754–63. 10.1001/jama.2014.14681 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344(8934):1383–9. . [PubMed] [Google Scholar]
- 19.Gutierrez J, Ramirez G, Rundek T, Sacco RL. Statin therapy in the prevention of recurrent cardiovascular events: a sex-based meta-analysis. Archives of internal medicine. 2012;172(12):909–19. 10.1001/archinternmed.2012.2145 . [DOI] [PubMed] [Google Scholar]
- 20.Mills EJ, Rachlis B, Wu P, Devereaux PJ, Arora P, Perri D. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. Journal of the American College of Cardiology. 2008;52(22):1769–81. 10.1016/j.jacc.2008.08.039 . [DOI] [PubMed] [Google Scholar]
- 21.Taylor FC, Huffman M, Ebrahim S. Statin therapy for primary prevention of cardiovascular disease. JAMA: the journal of the American Medical Association. 2013;310(22):2451–2. 10.1001/jama.2013.281348 . [DOI] [PubMed] [Google Scholar]
- 22.Zeb I, Li D, Nasir K, Malpeso J, Batool A, Flores F, et al. Effect of statin treatment on coronary plaque progression—A serial coronary CT angiography study. Atherosclerosis. 2013;231(2):198–204. 10.1016/j.atherosclerosis.2013.08.019 . [DOI] [PubMed] [Google Scholar]
- 23.Otagiri K, Tsutsui H, Kumazaki S, Miyashita Y, Aizawa K, Koshikawa M, et al. Early intervention with rosuvastatin decreases the lipid components of the plaque in acute coronary syndrome: analysis using integrated backscatter IVUS (ELAN study). Circulation journal: official journal of the Japanese Circulation Society. 2011;75(3):633–41. . [DOI] [PubMed] [Google Scholar]
- 24.Hoffmann H, Frieler K, Schlattmann P, Hamm B, Dewey M. Influence of statin treatment on coronary atherosclerosis visualised using multidetector computed tomography. European radiology. 2010;20(12):2824–33. 10.1007/s00330-010-1880-x . [DOI] [PubMed] [Google Scholar]
- 25.De Bruyne B, Pijls NH, Kalesan B, Barbato E, Tonino PA, Piroth Z, et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med. 2012;367(11):991–1001. Epub 2012/08/29. 10.1056/NEJMoa1205361 . [DOI] [PubMed] [Google Scholar]
- 26.Chow BJ, Small G, Yam Y, Chen L, McPherson R, Achenbach S, et al. Prognostic and therapeutic implications of statin and aspirin therapy in individuals with nonobstructive coronary artery disease: results from the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter registry) registry. Arterioscler Thromb Vasc Biol. 2015;35(4):981–9. Epub 2015/02/14. 10.1161/ATVBAHA.114.304351 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cholesterol Treatment Trialists C, Fulcher J, O’Connell R, Voysey M, Emberson J, Blackwell L, et al. Efficacy and safety of LDL-lowering therapy among men and women: meta-analysis of individual data from 174,000 participants in 27 randomised trials. Lancet. 2015;385(9976):1397–405. Epub 2015/01/13. 10.1016/S0140-6736(14)61368-4 . [DOI] [PubMed] [Google Scholar]
- 28.Nakazato R, Gransar H, Berman DS, Cheng VY, Lin FY, Achenbach S, et al. Statins use and coronary artery plaque composition: results from the International Multicenter CONFIRM Registry. Atherosclerosis. 2012;225(1):148–53. Epub 2012/09/18. 10.1016/j.atherosclerosis.2012.08.002 . [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This shows the rationale and design of study.
(DOCX)
(PDF)
Data Availability Statement
CONFIRM registry is a multinational multi-centers observation study that collects data from 12 centers in 6 countries, and the right to the raw material is in each center and the entire PI is Dr. James Min. The researcher was authorized to use the optional material applicable to this study in the entire registry group under consultation with Dr. Min for the idea of the submission. Therefore, anyone who wants to use the study data can contact the PI of this study, Dr. Min (jkm2001@med.cornell.edu), or 1st author Dr. Yun-Kyeong Cho (mk1997@dsmc.or.kr).