Abstract
Introduction
The irrational use of antibiotics is a major driver of antimicrobial resistance. This study aimed to explore how antibiotics were used in secondary and tertiary hospitals in Shaanxi Province, western China from 2013 to 2015.
Method
A retrospective study was conducted with a sample of 16 hospitals in Shaanxi Province (2 tertiary and 14 secondary hospitals; 8 public and 8 private hospitals) using a stratified random sampling method. All of the macro data from these hospitals from 2013 to 2015 were analyzed. All collected data were double-entered and analyzed using Excel 2007.
Results
The percentage of injectable antibiotic prescriptions was 26.6% of all of the antibiotic prescriptions in the secondary hospitals and 14.2% in the tertiary hospitals. Injectable antibiotic prescriptions in private tertiary hospitals (enter %) were more than two times that of public tertiary hospitals (enter %). In both tertiary and secondary hospitals, the percentage of antibiotic prescriptions for outpatients, emergency patients and inpatients were within the scope of the national standards, while the intensity of antibiotic use was higher than the national standard of 40 DDD/100 bed-days. The prophylactic antibiotic use rate in clean surgery was 40.4% in tertiary hospitals and 60.7% in secondary hospitals, which were both higher than the national standard of 30%. The preventive use rate of antibiotics in private tertiary hospitals (55.00%) was more than two times that of public tertiary hospitals (25.90%), and the rate was also higher in private secondary hospitals (61.50%) than in public secondary hospitals (59.70%).
Conclusions
Substantial antibiotic abuse occurred in the sample Chinese hospitals, especially in secondary hospitals. The government should continue to strengthen the administration of antimicrobial use in hospitals. At the same time, medical professional training and interventions for physicians should be conducted to fundamentally reduce the irrational use of antibiotics.
Introduction
Antimicrobial resistance (AMR) has gradually become one of the greatest threats to global public health of the 21st century [1–2]. A report on global AMR surveillance by the WHO showed that we are headed toward a “post-antibiotic age” [3]. In the communiqué of the 2016 G20 summit, AMR was specifically mentioned as a serious threat to public health, economic growth, and global economic stability [4].
Increased AMR rates may lead to prolonged hospitalization, a prolonged duration of treatment, increased treatment costs, and increased mortality [5–6]. A report from the Centers for Disease Control and Prevention (CDC) predicted that approximately 2 million illnesses and 23,000 deaths each year are associated with drug-resistant infections in the United States [7]. The spread of AMR is relatively serious in China [8–9]. In 2015, the national detection rate of erythromycin-resistant Streptococcus pneumoniae and methicillin-resistant Staphylococcus aureus (MRSA) was 35.8% and 91.5%, respectively, according to the surveillance of the national bacterial drug resistance network [10].
The widespread and irrational use of antimicrobial agents is considered the main cause of increased AMR [11–12]. The phenomenon of antibiotic overuse is particularly acute in China compared with other countries [13]. According to a survey of antibiotic use at 48 health care institutions in 2014, the antibiotics prescription rate of hospitalized patients was 77.5%, and only 24.6% of prescriptions were appropriate [14].
To effectively curb AMR and promote the rational use of antimicrobial agents in healthcare settings, the Chinese government launched a national antibiotic stewardship Action Initiative campaign (hereafter referred to as the Action Initiative) in 2011. The Action Initiative aims to control total antibiotic use in hospitals [15]. In China, all hospitals are ranked as tertiary, secondary, or primary health care institutions based on the scale of the hospital (beds), technical level, management level, equipment conditions, scientific research capacity, etc. The target of the Action Initiative includes public secondary and tertiary hospitals.
This campaign protocol clearly defines antibiotic procurement, antimicrobial drug use in hospitalized patients, the outpatient antibiotic prescription rate, the proportion of prophylactic use of antibiotics in clean operations, and so on. A few previous studies evaluated the use of antibiotics in healthcare settings before the campaign [16–17] or assessed the overall impact of the campaign [18]. However, information on the use of antibiotics in secondary and tertiary Chinese hospitals after the campaign is lacking, particularly a comparative study between public and private institutions. This is important because understanding the use of antimicrobial agents in these facilities can provide superior data to support further national policy development.
The aim of this research was to explore how antibiotics were used in secondary and tertiary hospitals in Shaanxi Province, western China between 2013 and 2015 and to compare the use of antibiotics in public and private institutions.
Methods
Hospitals
A retrospective study was conducted in tertiary and secondary hospitals in Xi’an, the capital city of Shaanxi Province. Xi’an is one of the largest inland cities in western China, with a population of 8,249,300 and an area of 10,096.81 square kilometers [19]. A multistratified grouping random sampling method was used to identify the target hospitals. First, we found the total number of secondary and tertiary hospitals in Xi’an by searching the official website of the Shaanxi Provincial Health and Family Planning Commission, and we determined the public and private hospital composition ratio of 1:1. At the same time, we also considered the degree of cooperation of the hospitals. We then randomly selected two tertiary hospitals (one public and one private) and 14 secondary hospitals (seven public and seven private) for a total of 16 hospitals as a sample survey of institutions. We chose the same level hospitals with a similar total number of patients and inpatients per year. The inclusion criteria were: (1) general hospital (excluding specialist hospitals); (2) the hospital had complete medical institution macro data for statistical analysis; and (3) the hospital dean agreed to participate in this study.
Data collection
All medical institution data was collected on a quarterly basis at each selected hospital from January 2013 to December 2015. The information mainly consisted of three parts. Part one included the hospital characteristics. Part two addressed the situation of rational drug use in the hospital. This section contained four prescription indicators, in accordance with WHO/International Network for the Rational Use of Drugs (INRUD) recommendations [20]. Part three was intended to analyze the rational use of antibiotics, including the use of antimicrobial agents among inpatients and the prophylactic use of antimicrobials during clean surgery.
Two investigators were assigned to each medical institution, a graduate student filled out the investigational forms, and a pharmacist reviewed the rationality of the data. All investigators received the same training before the survey. The dean of each hospital gave their verbal consent for participation in this study.
Main measurements
According to the Guidelines for the Clinical Application of Antibacterial Agents [21], descriptions of the indicators related to rational antibacterial use are as follows: (1) the proportion of prescriptions for antibacterial drugs among outpatients, emergency patients, and inpatients (number of prescriptions containing antibacterial agents/total number of prescriptions among outpatients, emergency patients, and inpatients × 100%); (2) the intensity of antimicrobial consumption (total consumption of antibiotics/patient bed-day at the same time × 100); total consumption of antibiotics refers to total the defined daily dose (DDD), which is the average daily dose of adult drugs for primary treatment purposes and is equal to the consumption of an antibacterial drug divided by the DDD; (3) the rate of prophylactic antibacterial agents used during clean surgery (number of prophylactic antibacterial agents used during clean surgery/number of clean surgeries × 100%); (4) the drug selection qualification rate (number of antibacterial agents selected from the drug catalog of prophylactic antibiotic agents/number of prophylactic antibacterials used during clean surgery × 100%); (5) the reasonable rate of antibiotic administration at the time of the first incision (number of reasonable antibiotic agents administered at the time of the first incision/number of prophylactic antibiotic agents used during clean surgery × 100%); (6) reasonable rate of prophylactic treatment with antibiotic agents during clean surgery (number of reasonable treatments with prophylactic antibiotic agents/number of prophylactic antibiotic agents used during clean surgery × 100%)
National and local guidelines
Antibacterial agents were identified according to the WHO Anatomical Therapeutic Chemical (WHO/ATC) Classification System [22]. According to the standards of the “Guiding Principles of the Clinical Application of Antibacterials” issued by the Chinese government in 2015 [23], the number of antibiotics procured are restricted to 35 or 50 in secondary or tertiary hospitals, respectively. The standards also require that the antibiotic prescription rate should be limited to 60%, 20%, and 40% of all prescriptions for hospitalized patients, outpatients, and emergency patients, respectively; the preventive use rate of antibiotics in clean surgery should be reduced to 30% or below; and the intensity of antibiotic use should be less than 40 daily defined doses (DDD) per 100 patient days.
Statistical analysis
All collected data were double-entered using Excel 2007 to confirm the accuracy and conduct the analysis. Continuous variables were represented by means and ranges, and categorical data were expressed in proportions. Income and expenses were expressed in US dollars: 1 USD = 6.39 RMB.
An evaluation team was formed to judge the rational use of antimicrobial agents according to the Chinese “Guiding Principles of the Clinical Application of Antibacterials” of 2015 [23]. This team was composed of two clinical pharmacists who specialized in anti-infection, one attending physician who specialized in infectious diseases, and one attending physician who specialized in respiratory diseases.
Ethical approval
Xi’an Jiaotong University Health Science Center, Shaanxi Provincial Department of Health, the Shaanxi Food and Drug Administration, and all participating hospitals approved the study prior to data collection. The dean of each hospital gave verbal consent for participation in this survey. The requirement for patient consent was waived because there was no contact with patients and patient information was anonymous. Ethical approval for this study was obtained from the Xi’an Jiaotong University Research Ethics Committee.
Results
Characteristics of institutions
The general characteristics of all 16 participating institutions are illustrated in Table 1. The total number of patients per year in public tertiary hospitals was slightly higher than those in private tertiary hospitals; however, in secondary hospitals, the opposite result was found. The medical staff primarily consisted of physicians, physician assistants, pharmacists, and nurses. In tertiary hospitals, the proportion of total income from drug sales was 39.2%, with antibiotic sales accounting for 18.2% of this income. In secondary hospitals, the proportion of total income from drug sales was 38.7%, with antibiotic sales accounting for 14.5% of this income.
Table 1. General characteristics of hospitals.
| Indicators | Tertiary HospitalMean (Range) | Secondary Hospital Mean (Range) | ||||
|---|---|---|---|---|---|---|
| Public | Private | All | Public | Private | All | |
| Beds, No. | 1000 | 800 | 900 | 185(100–316) | 280(100–650) | 233(100–650) |
| Total number of patients per year, No. | 637484 (602776–665332) |
635745 (600264–657656) |
636614 (600264–665332) |
98346 (35457–164240) |
154067 (37762–407362) |
126206 (35457–407362) |
| Inpatients per year, No. | 32113 (31093–32670) |
30953 (28349–32949) |
31533 (28349–32949) |
4623 (648–12450) |
12283 (878–34737) |
8453 (648–34737) |
| Prescribers, No. | 523(486–557) | 335(316–353) | 429(316–557) | 62(30–107) | 102(32–285) | 82(30–285) |
| Nursing staff, No. | 711(690–739) | 538(500–558) | 625(500–739) | 100(31–189) | 166(41–483) | 133(31–483) |
| Pharmacy staff, No. | 64(61–66) | 24(22–27) | 44(22–66) | 14(8–22) | 12(6–29) | 13(6–29) |
| Drug income as a percentage of total income, % | 47.30 (47.10–47.60) |
31.00 (30.00–32.80) |
39.20 (30.00–47.60) |
43.70 (25.60–58.00) |
33.70 (20.90–43.20) |
38.70 (20.90–58.00) |
| Antibiotic sales as a percentage of drug income, % | 18.50 (16.40–19.90) |
17.80 (16.60–18.70) |
18.20 (16.40–19.90) |
13.70 (4.90–18.00) |
15.30 (6.30–25.30) |
14.50 (4.90–25.30) |
Analysis of the amount of antibacterial drugs used and the purchase amount found that all types of antibiotics were used. The most commonly used antibiotics were penicillins, cephalosporins, imidazoles, macrolides and fluoroquinolones (Table 2). Whether in tertiary or secondary hospitals, the highest use of antibacterial drugs in public hospitals was penicillin and in private hospitals was cephalosporin. The order of the amount of antibiotics used was the same in the tertiary and secondary hospitals (Table 3).
Table 2. Most commonly prescribed antibiotic classes in hospitals.
| ATC Code | Antibiotic Class | Antibiotic Sales, g | |||
|---|---|---|---|---|---|
| Tertiary Hospital | Secondary Hospital | ||||
| Public | Private | Public | Private | ||
| J01CA/E/F | Penicillins | 13563341.96 | 702792.00 | 1128799.82 | 1202204.83 |
| J01DA | Cephalosporins | 882636.35 | 1674572.00 | 1502864.00 | 2362429.02 |
| J01XD | Imidazoles | 90443.73 | 528735.00 | 833300.48 | 3536691.28 |
| J01FA | Macrolides | 64783.98 | 448579.00 | 206332.13 | 131111.10 |
| J01MA | Fluoroquinolones | 57498.00 | 162903.00 | 167534.33 | 230708.6 |
Table 3. Highest amount of antibiotic classes used in hospitals.
| ATC Code | Antibiotic Class | Antibiotic Sales Amount, $ | |||
|---|---|---|---|---|---|
| Tertiary Hospital | Secondary Hospital | ||||
| Public | Private | Public | Private | ||
| J01DA | Cephalosporins | 6767190.00 | 5609697.00 | 3695161.00 | 6275265.00 |
| J01CA/E/F | Penicillins | 1121453.00 | 949295.60 | 1139481.00 | 1957685.00 |
| J01MA | Fluoroquinolones | 993839.10 | 612623.10 | 772403.00 | 1612454.00 |
| J01XD | Imidazoles | 451215.60 | 188182.20 | 66891.52.00 | 951813.4.00 |
| J01FA | Macrolides | 177056.00 | 526896.30 | 253853.60 | 581196.4.00 |
Drug prescribing indicators
As shown in Table 4, the percentage of injectable prescriptions was 14.2% in tertiary hospitals, which was lower than the 26.6% in secondary hospitals, and it was 19.7% in private tertiary hospitals, which was far more than the 8.8% in public tertiary hospitals. The percentage of essential medications among the total amount of drugs was 37.9% in tertiary and 61.5% in secondary hospitals. The rate of essential medications in public institutions was lower than that in private institutions, no matter whether in secondary or tertiary hospitals. The average number of drugs per prescription was 2.36 in secondary hospitals, which was slightly higher than that in tertiary hospitals. The average cost per prescription was 22.6 USD in tertiary hospitals, which was higher than the cost in secondary hospitals. The average cost per prescription was nearly the same in public and private secondary hospitals.
Table 4. Indicators of drug prescribing in different levels of hospitals.
| Indicators | Tertiary Hospital | Secondary Hospital | ||||
|---|---|---|---|---|---|---|
| Public | Private | All | Public | Private | All | |
| Drugs prescribed per visit, mean (range) | 1.82(1.55–2.02) | 2.31(2.22–2.37) | 2.07(1.55–2.37) | 2.42(1.10–3.08) | 2.30(1.28–3.47) | 2.36 (1.10–3.47) |
| Cost per visit, mean (range), $ | 22.20 (20.37–23.75) |
23.00 (21.10–25.17) |
22.60 (20.37–25.17) |
15.30 (11.28–30.92) |
15.10 (9.78–21.95) |
15.20 (9.78–30.92) |
| Percentage of injections, % | 8.80 | 19.70 | 14.20 | 26.90 | 26.60 | 26.60 |
| Percentage of essential drugs, % | 32.90 | 42.90 | 37.90 | 60.20 | 63.10 | 61.50 |
Antibiotic use in different levels of hospitals
The results of antibiotic use are shown in Table 5. The number of antibiotic agents procured was 48 in tertiary and 30 in secondary hospitals. In tertiary hospitals, the average percentage of antibiotics prescribed for outpatients, emergency patients, and inpatients was 17.0%, 28.2%, and 54.6%, respectively. The average percentage of antibiotics prescribed for outpatients, emergency patients, and inpatients in secondary hospitals was 20.8%, 31.1%, and 52.2%, respectively. The percentage of antibiotics prescribed for outpatients and emergency patients was higher in private tertiary hospitals than in public tertiary hospitals. In contrast, the percentage of antibiotics prescribed for outpatients was higher in public secondary hospitals than in private secondary institutions. The intensity of antibiotic use was 46.6 DDD/100 bed-days and 48.1 DDD/100 bed-days in tertiary and secondary hospitals, respectively; this was slightly higher in public institutions than in private ones.
Table 5. Indicators of drug prescribing in different levels of hospitals.
| Indicators | Tertiary Hospital | Secondary Hospital | ||||
|---|---|---|---|---|---|---|
| Public | Private | All | Public | Private | All | |
| Antibiotic agents used, No. | 50.00 | 46.00 | 48.00 | 30.00 | 30.00 | 30.00 |
| Outpatients | ||||||
| Percentage of antibiotics, % | 15.00 | 19.20 | 17.10 | 22.40 | 19.30 | 20.80 |
| Emergency | ||||||
| Percentage of antibiotics, % | 28.00 | 28.50 | 28.20 | 31.10 | 31.20 | 31.10 |
| Inpatients | ||||||
| Percentage of antibiotics, % | 58.80 | 50.40 | 54.60 | 49.80 | 54.50 | 52.20 |
| DDD/100 bed-days | 54.10 | 39.10 | 46.60 | 49.00 | 47.20 | 48.10 |
Antibiotic use in Class I incision surgery
Table 6 shows the antibiotic prophylaxis rates in clean surgery for different levels of hospitals. The preventive use rate of antibiotics was 40.4% in tertiary and 60.7% in secondary hospitals, which were both higher than the national standard of 30%. The preventive use rate of antibiotics in private hospitals was higher than in public institutions. Of all the antibiotic prescriptions for clean surgery patients, the reasonable rate of different antibiotics, proper rate of medication time, and rational rate of medication course in tertiary hospitals were higher than those in secondary hospitals. In addition, the rational rate of medication course was only 66.9% in secondary hospitals, which was far lower than that in tertiary hospitals.
Table 6. Antibiotic use in Class I incision surgery.
| Indicators | Tertiary Hospital | Secondary Hospital | ||||
|---|---|---|---|---|---|---|
| Public | Private | All | Public | Private | All | |
| Antibiotic prophylaxis rates (%) | 25.90 | 55.00 | 40.40 | 59.70 | 61.50 | 60.70 |
| Proper antibiotic varieties of prophylaxis (%) | 100.00 | 96.10 | 98.00 | 79.90 | 81.70 | 81.10 |
| Proper medication time of prophylaxis (%) | 100.00 | 99.90 | 100.00 | 82.00 | 81.00 | 82.20 |
| Proper medication course of prophylaxis (%) | 95.10 | 86.30 | 90.70 | 63.80 | 68.60 | 66.90 |
Antibiotic use in different years
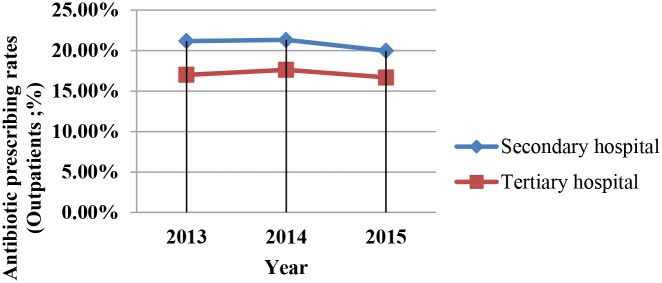
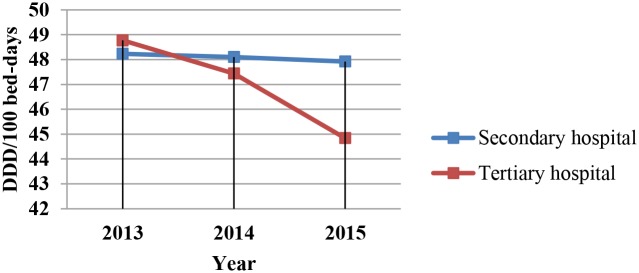
Analysis of the use of antimicrobials in hospitals in different years revealed that DDD per 100 patient days and antibiotic prescription rates for outpatients and emergency patients decreased year by year (Figs 1–3). However, this downward trend varied among the different levels of hospitals. The fastest decline in DDD per 100 patient days during the 3 years was in tertiary hospitals.
Fig 1. Antibiotic prescription rates of outpatients in tertiary and secondary hospitals.
Antibiotic prescription rates of outpatients in Different Levels of Hospitals by Year.
Fig 3. DDD per 100 patient days in tertiary and secondary hospitals.
DDD per 100 patient days in Different Levels of Hospitals by Year.
Fig 2. Antibiotic prescription rates of emergency patients in tertiary and secondary hospitals.
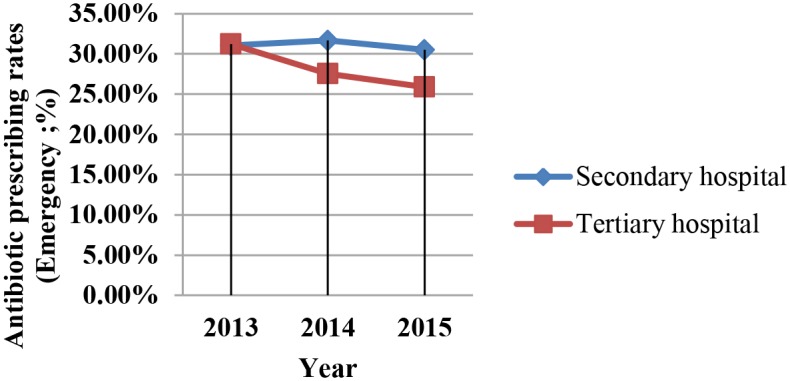
Antibiotic prescription rates of emergency patients in Different Levels of Hospitals by Year.
Discussion
As far as we know, this is the first study to report detailed information about the antibiotic prescribing patterns of public and private hospitals in western China after the implementation of the Action Initiative. Our sample included 16 institutions; 8 public sector hospitals and 8 private ones. This study showed that the reasonable use of antibiotics in tertiary hospitals was superior to that of secondary hospitals. In this survey of Chinese hospitals, antibiotic sales as a percentage of income from drug sales was higher in tertiary hospitals than in secondary hospitals; there was no obvious difference between the public and private sectors. A study of Chinese general hospitals found that antibiotics accounted for approximately 17% to 25% of all drug sales [24], which is slightly higher than our findings. This may be because of differences in time frames and geographical areas between the two studies, or different results regarding the implementation effect of the Action Initiative.
In both tertiary and secondary hospitals, the percentage of antibiotics prescribed for outpatients, emergency patients, and inpatients was within the scope of the national standards. Similar to the results of other published research [25–26], the excessive and improper use of antibiotics has been gradually improving, especially after the Action Initiative began. The percentage of antibiotics prescribed for inpatients in tertiary hospitals decreased from 61.4% to 43.8% after the implementation of the Action Initiative [25].
We found that from 2013 to 2015, the rate of antibiotics prescribed for outpatients and emergency patients declined each year, with this rate decreasing more rapidly in tertiary than in secondary hospitals; this clearly demonstrates the sustained effectiveness of this campaign. We also found that there was no significant difference in antibiotic use indicators between public and private hospitals. These results show an effect of the level of the hospital, whereas the type of hospital had no effect. This may be because in China, all hospitals are graded, and requests for the use of antibacterial drugs in the criteria are the same for public and private hospitals.
Regardless of whether in a secondary or tertiary hospital, the intensity of antibiotic use in this study was higher than the national standard of 40 DDD/100 bed-days, which differs slightly from the results of previous research. A study conducted among 65 general hospitals in China found that after the implementation of the Action Initiative, the intensity of antibiotic consumption was 35.9 DDD/100 bed-days [18]. A study from three wards in the largest tertiary teaching hospital in Ethiopia found that three out of four patients were prescribed antibiotics, and the mean antibiotic consumption was 81.6 DDD/100 bed-days [27]. This difference may be owing to a difference in geographic location. From 2013 to 2015, the intensity of antibiotic use decreased more rapidly each year in tertiary hospitals than in secondary hospitals. This may be because the stewardship programs/policies, support staff, etc. were different between tertiary and secondary hospitals.
Regarding clean surgery, only the antibiotic prophylaxis rate in public tertiary hospitals was below the national maximum limit of 30%. In secondary hospitals, the antibiotic prophylaxis rate was very high and the reasonable use rate was unacceptable. Compared with other countries, the rate of reasonable antibiotic use in secondary hospitals in China remains relatively high. An international survey of antimicrobial prophylaxis in surgery found that 26.1% of patients did not adhere to the proper duration of medication administration and 27.2% did not follow the proper medication course [28]. In a survey conducted in Italy from 2009 to 2012, the preoperative antibiotic prophylaxis was appropriate in 18.1% of cases, and the appropriateness of timing of the prophylactic antibiotic administration was observed in 53.4% of procedures [29]. A study conducted in China in 2013 found that the antibiotic prophylaxis rate in Class I incision surgery decreased from 77.38% to 46.60% [30], but it was still very high.
There are many reasons for antibiotics abuse [31–35]. One is the cause of the patient, who may view antibiotics as a panacea, and therefore demand them even when they are unwarranted, or they may demand intravenous over oral therapies, perceiving them to be more efficacious. The other is the supply side; physicians may overprescribe antibiotics because they lack professional knowledge about proper antibiotic usage, or simply because they believe that is what patient wants. This study aimed to explore how antibiotics were used in secondary and tertiary hospitals after the implementation of the Action Initiative.
There are several limitations in this study. First, this research was conducted in one city in China: Xi’an; therefore, the results may not reflect the antibiotic use in hospitals throughout the nation. However, in this pilot study, we used a multistratified grouping random sampling method to reveal the antimicrobial drug use between different levels and different types of hospitals. Second, we did not investigate the characteristics of the medical staff in research hospitals, such as education level, work experience, salary and so on. Finally, the current study revealed the use of antibiotics among outpatients, emergency patients, and inpatients, but we did not analyze the rational use rate of antibiotics by analyzing each prescription. However, we compared the difference between our study results and the national standards, which were designed by policy-makers who considered the rational use of antibiotics before formulating the standards.
Conclusions
In this study, we found substantial antibiotic overuse in Chinese hospitals. To counter the current situation of antibiotic misuse, policy-makers should continue to improve the administration of antimicrobial use in hospitals. Strict norms are also needed to regulate the prescribing behavior of physicians. At the same time, training of medical professionals and interventions for physicians should be conducted to fundamentally reduce the irrational use of antibiotics, especially in secondary hospitals.
Supporting information
General characteristics of hospitals.
(ZIP)
The antibacterial drug sales in different level of hospitals.
(ZIP)
The indicators of drug prescribing in different level of hospitals.
(ZIP)
Acknowledgments
We thank all of the hospitals involved in the study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was financially supported by the National Natural Science Foundation of China (grant number 71603199 to KY), the Central University Basic Research Fund (2015qngz05 to YF), and the “Young Talent Support Plan” of Xi’an Jiaotong University to YF. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hiltunen T, Virta M, Laine AL. Antibiotic resistance in the wild: an eco-evolutionary perspective. Philosophical Transactions of the Royal Society of London, 2017, 372(1712): 20160039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baur D, Gladstone BP, Burkert F, Carrara E, Foschi F, Döbele S, et al. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis. Lancet Infectious Diseases, 2017, 17(9): 990–1001. 10.1016/S1473-3099(17)30325-0 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Antimicrobial resistance: global report on surveillance. Australasian Medical Journal, 2014, 7(4): 237. [Google Scholar]
- 4.Full text: G20 Leaders’ Communique, Hangzhou Summit. http://www.china.org.cn/world/2016-09/06/content_39245577.htm (accessed 25 May 2018).
- 5.Cosgrove SE, Carmeli Y. The impact of antimicrobial resistance on health and economic outcomes. Clinical Infectious Diseases, 2003, 36: 1433–1437. 10.1086/375081 [DOI] [PubMed] [Google Scholar]
- 6.Naylor NR, Silva S, Kulasabanathan K, Atun R, Zhu N, Knight GM, et al. Methods for estimating the burden of antimicrobial resistance: a systematic literature review protocol. BMC Systematic Reviews, 2016, 5(1): 187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United State. 2013. https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf (accessed 11 February 2018)
- 8.Yezli S, Li H. Antibiotic resistance amongst healthcare-associated pathogens in China. International Journal of Antimicrobial Agents, 2012, 40(5): 389–97. 10.1016/j.ijantimicag.2012.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paterson DL, Van DD. China’s antibiotic resistance problems. Lancet Infectious Diseases, 2017, 17(4): 351–352. 10.1016/S1473-3099(17)30053-1 [DOI] [PubMed] [Google Scholar]
- 10.Fridkin SK, Cleveland AA, See I, Lynfield R. Emerging Infections Program as Surveillance for Antimicrobial Drug Resistance. Emerging Infectious Diseases, 2015, 21(9):1578–81. 10.3201/eid2109.150512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Costelloe C, Metcalfe C, Lovering A, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. British Medical Journal, 2010, 340: c2096. [DOI] [PubMed] [Google Scholar]
- 12.Arason VA, Sigurdsson JA, Erlendsdottir H, Kristinsson KG. The role of antimicrobial use in the epidemiology of resistant pneumococci: a 10-year follow up. Microbial Drug Resistance, 2006, 12(3): 169–176. 10.1089/mdr.2006.12.169 (accessed 11 February 2018) [DOI] [PubMed] [Google Scholar]
- 13.Fang Yu. China should curb non-prescription use of antibiotics in the community. British Medical Journal, 2014, 348: g4233. [DOI] [PubMed] [Google Scholar]
- 14.Wang J, Wang P, Wang X, Zheng Y, Xiao Y. Use and prescription of antibiotics in primary health care settings in China. JAMAInternal Medicine, 2014, 174(12): 1914–1920. [DOI] [PubMed] [Google Scholar]
- 15.Ma X, Xie J, Yang Y, Guo F, Gao Z, Shao H, et al. Antimicrobial stewardship of Chinese ministry of health reduces multidrug-resistant organism isolates in critically ill patients: a pre-post study from a single center. BMC Infectious Diseases, 2016, 16(1): 704 10.1186/s12879-016-2051-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dong L, Yan H, Wang D. Drug prescribing indicators in village health clinics across 10 provinces of Western China. Family Practice, 2011, 28(1): 63–67. 10.1093/fampra/cmq077 [DOI] [PubMed] [Google Scholar]
- 17.Xiao Y, Li L. Legislation of clinical antibiotic use in China. Lancet Infectious Diseases, 2013, 13(3): 189–191. 10.1016/S1473-3099(13)70011-2 [DOI] [PubMed] [Google Scholar]
- 18.Bao L, Peng R, Wang Y, Ma R, Ren X, Meng W, et al. Significant reduction of antibiotic consumption and patients’ costs after an Action Plan in China, 2010–2014. PloS ONE, 2015, 10(3): e0118868 10.1371/journal.pone.0118868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The Statistical Yearbook in Xi’an in 2016. http://tjj.xa.gov.cn/ptl/def/def/2016/zk/indexch.htm (accessed 25 May 2018).
- 20.Ghei P. How to investigate drug use in health facilities Selected drug use indicators: WHO Publications, Geneva, 87 pp. 1993. Health Policy, 1995, 34(1): 73–71. [Google Scholar]
- 21.Ministry of Health of the People’s Republic of China. Regulations for Clinical Application of Antibacterial Agents. Beijing, 2012:4.
- 22.World Health Organization. The Anatomical Therapeutic Chemical Classification System with Defined Daily Doses (ATC/DDD). Oslo, Norway: WHO; 2006. http://www.who.int/classifications/atcddd/en/(accessed 11 February 2018)
- 23.National Health and Family Planning Commission of the People’s Republic of China. Guiding Principles of Clinical Application of Antibacterials. Beijing, 2015:7.
- 24.Xiao Y, Zhang J, Zheng B, Zhao L, Li S, Li L. Changes in Chinese Policies to Promote the Rational Use of Antibiotics. PLoS Medicine, 2013, 10(11): e1001556 10.1371/journal.pmed.1001556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shi W, Wang L, Zhao Z, Yue X. Analysis on the progression of the special rectification on antibacterials using in tertiary hospital of Bejing from 2011 to 2013 [in Chinese]. Clinical Medication Journal, 2014, 12(5): 21–26. [Google Scholar]
- 26.Mao X, Ye Q, Han J, Zhou Y. Antibiotics usage in outpatient department after new antibiotic policy [in Chinese]. Chinese Journal of Nosocomiology, 2013, 23(15): 3739–3741. [Google Scholar]
- 27.Alexiou VG, Ierodiakonou V, Peppas G, Falagas ME. Antimicrobial prophylaxis in surgery: an international survey. Surgical Infections, 2010, 11(4): 343–348. 10.1089/sur.2009.023 [DOI] [PubMed] [Google Scholar]
- 28.Gutema G, Håkonsen H, Engidawork E, Toverud EL. Multiple challenges of antibiotic use in a large hospital in Ethiopia—a ward-specific study showing high rates of hospital-acquired infections and ineffective prophylaxis. BMC Health Services Research, 2018, 18(1):326 10.1186/s12913-018-3107-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Francesco N, Maria TI, Gabriella DG, Angelillo IF. Evaluation of the appropriate perioperative antibiotic prophylaxis in Italy. PLoS ONE, 2013, 8(11): e79532 10.1371/journal.pone.0079532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ran SP, Jia LP, Ying GU, Liu XB. Intervention in perioperative antimicrobial prophylaxis in clean incision operation [in Chinese]. Chinese Journal of Infection Control, 2016, 15(5): 330–333. [Google Scholar]
- 31.Cars H, Hakansson A. To prescribe—or not to prescribe—antibiotics: district physicians’ habits vary greatly, and are difficult to change. Scandinavian Journal of Primary Health Care, 1995, 13 (1): 3–7. [DOI] [PubMed] [Google Scholar]
- 32.Dar-Odeh NS, Abu-Hammad OA, Al-Omiri MK, Khraisat AS, Shehabi AA. Antibiotic prescribing practices by dentists: a review. Therapeutics and Clinic Risk Management, 2010, 6: 301–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bennett D, Hung CL, Lauderdale TL. Health Care Competition and Antibiotic Use in Taiwan. Journal of Industrial Economics, 2015, 63(2):371–393. [Google Scholar]
- 34.Yao K, Yang Y. Streptococcus pneumoniae diseases in Chinese children: past, present and future. Vaccine, 2008, 26 (35): 4425–4433. 10.1016/j.vaccine.2008.06.052 [DOI] [PubMed] [Google Scholar]
- 35.Currie J, Lin W, Zhang W. Patient knowledge and antibiotic abuse: Evidence from an audit study in China. Journal of Health Economics, 2011, 30(5): 933 10.1016/j.jhealeco.2011.05.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
General characteristics of hospitals.
(ZIP)
The antibacterial drug sales in different level of hospitals.
(ZIP)
The indicators of drug prescribing in different level of hospitals.
(ZIP)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.