Abstract
Aims
Recently, the clinical importance of total antioxidant capacity (TAC) and its protective role against several chronic diseases like cardiovascular disease, osteoporosis and several types of cancers has been reported. However, its association with cardio-metabolic risk factors among patients candidate for coronary artery bypass graft surgery (CABG) has not been evaluated yet. CABG is associated with increased oxidative stress and free radicals; so, the current study was aimed to evaluate the potential association of TAC with cardiovascular risk factors among patients candidate for CABG.
Methods and materials
In the current cross-sectional study, 454 patients aged 35–80 years as candidates of CABG and hospitalized in Tehran Heart Center were enrolled. Anthropometric and demographic characteristics were obtained from all participants. Total dietary antioxidant capacity (TAC) was calculated according to the findings of semi-quantitative food-frequency questionnaire (FFQ). Biochemical parameters including serum lipids, albumin, creatinine, HbA1C, C-reactive protein (CRP), lipoprotein (a), creatinine, blood urea nitrogen (BUN) and serum vitamin D concentrations were also assessed by commercial laboratory methods.
Results
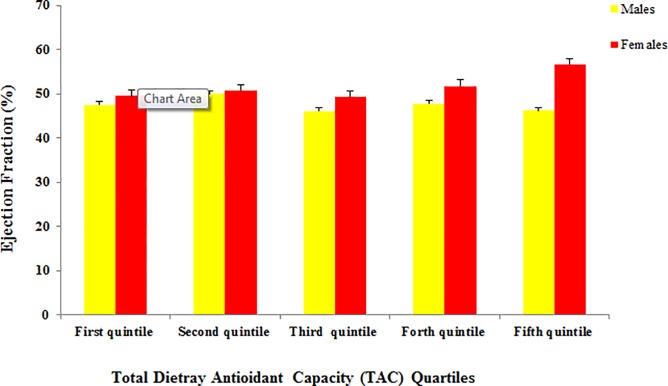
Male patients in the top quintiles of TAC had significantly lower prevalence of hypertension (35.1% vs 45.9%). Moreover, male patients at fifth quintile of TAC were 2% more serum vitamin D concentrations, 3% lower serum cholesterol concentrations compared with lowest quintile. Top quintiles of TAC make patients more likely to have low hematocrit and high serum albumin concentrations compared with lowest quintiles (P < 0.05). However, in female participants, only serum creatinine concentration was in negative association with TAC. In comparison of clinical parameters, females in the fifth quintile of TAC had 9% higher EF compared with patients in the first quintile (P = 0.021).
Conclusion
To our findings, higher dietary antioxidant capacity was associated with lower prevalence of hypertension, lower hematocrit, total cholesterol and higher albumin and vitamin D concentrations. Therefore, high dietary TAC could be considered as a potent protective tool against cardio-metabolic risk factors in patients CABG candidate for especially in male patients.
Introduction
Coronary artery bypass grafting surgery (CABG), as a category of coronary revascularization, is one of the most frequent procedures performed and annually about 50000 open-heart surgeries are performed in Iran, 50–60% of which is allocated to CABG [1]. The CABG was first introduced in the 1960s with the aim of offering symptomatic relief, improved quality of life, and increased life expectancy in patients with coronary artery disease (CAD) [2–3]. The surgery major indicators are over 50% left main coronary artery stenosis or over 70% stenosis of the proximal left anterior descending (LAD) and proximal circumflex arteries [4]. According to the world health organization report, cardiovascular diseases (CVDs) are the number one cause of death globally: more people die annually from CVDs than from any other cause. An estimated 17.7 million people died from CVDs in 2015, representing 31% of all global deaths. Of these deaths, an estimated 7.4 million were due to coronary heart disease and 6.7 million were due to stroke [5]. In Iran, also CAD is a major cause of mortality and morbidity and accounts for nearly 50 percent of all deaths per year [6].
It is well known that oxidative stress is involved in the pathogenesis and development of coronary artery disease and atherosclerosis; increased serum free radicals include reactive intermediates of oxygen—reactive oxygen species metabolism (ROMs), such as superoxide radicals (O2-·) hydroperoxyl (HO2·) and hydroxyl (OH·) and hydrogen peroxide (H2O2) are associated with the extent and severity of CAD and the occurrence of different atherogenic risk factors [7–9]. Most importantly, patients candidate for CABG have increased markers of oxidative stress [10] and the CABG process by itself, triggers the oxidative stress status even during and after surgery [11]; in the study by Cavalca et al increased oxidative stress regarding an impairment in the arginine/nitric oxide pathway and reduced antioxidant level has been reported in candidates of CABG [12–13].
The role of nutritional behaviors and dietary intakes in prevention of CVD or its progression has been studied before; numerous studies suggested the role of healthy dietary choices and improved life style with higher physical activity level [14] and higher intakes of healthy food choices including fruits and vegetables and dietary antioxidants in prevention and treatment of cardiovascular events [15]; moreover, there are multiple studies have investigated the role of single anti-oxidant nutrients as a supplement [16, 17] in improving the cardiovascular disease severity and attenuating the CABG consequences.
Dietary total antioxidant capacity (TAC) reflects all of the antioxidant compounds present in food and the interactions between those compounds [18]. The total antioxidant capacity of diet is inversely associated with cardiovascular diseases [19], heart failure [20] myocardial infarction [21] stroke [22]. However, as mentioned above, studying the potential antioxidant capacity of diet in the pre-CABG patients could be considered as a useful preventive tool to assess the possible need to antioxidants. Moreover, while vitamin D is classically well-known for its classic role in bone homeostasis, recent studies have identified new roles for it. The antioxidant activity of vitamin D has been proved by Wiseman in 1993 while indicating its role in prevention of lipid peroxidation in the cell membrane [23]. Moreover, it has been identified that vitamin D deficinecy is a powerful contributor of cardiovascular deaths; In a cohort study of 3258 participants, death from cardiovascular disease in patients with severe and moderate vitamin D deficiency was 1.8 to 2.5 times more prevalent compared with patients with mild or no vitamin D deficiency [24].
Therefore in the current study we aimed to evaluate the total dietary anti-oxidant capacity and its association with metabolic risk factors of CVD and serum vitamin D concentrations in patients candidate of CABG.
Materials and methods
Subjects
The study protocol has been reported elsewhere [25]; participants in the current cross-sectional study were recruited for Tehran Heart Center-Coronary Outcome Measurement (THC-COM) study and were candidates for isolated CABG with cardiopulmonary bypass. Participants in this study were patients admitted to the cardiothoracic ward for CABG surgery at a large heart center in this time period. The sample size calculation has been explained before [26]; briefly, the sample size was calculated using the formula for comparing two proportions: n = [(Zα/2 + Zβ)2 × {(p1 (1-p1) + (p2 (1-p2))}]/ (p1—p2)2 where p1 is the proportion of the women with low quality Mediterranean regimen (0.3), p2 is the proportion of the men with low quality Mediterranean regimen (0.25), α error = 0.05, and power = 80% (1-β). Accordingly, a 125-subject sample size was determined for the study (125 in each group). We also assumed 20% loss (125 + 25) and as men with CAD are twice as women (150 + 300), the final sample size of 450 was considered for the study [26–28]. Reasons for drop-out or exclusion were incomplete dietary questionnaires (n = 1), and incomplete demographic questionnaires (n = 5). Finally, 454 patients aged 35–80 years completed the study. The details of study procedure and biochemical assays have been provided elsewhere [26]. The study was approved by the ethics committee of Tehran Heart Center, Tehran University of Medical Sciences, Research Undersecretary of Tabriz University of Medical Sciences, and written informed consent was obtained from all of the participants.
Clinical assessment of patients
Clinical assessment and pre-operative cardiac status was also measured by several variables including: left ventricular ejection- fraction, number of diseased vessels, New York Heart Association (NYHA) functional class and the European system for cardiac operative risk evaluation (EuroSCORE) [29]. EuroSCORE is a simple, additive risk model of perioperative mortality and as a useful predictor of the long term hazard of cardiovascular events leading to death or morbidity after cardiac surgery [30]. It is calculated according to the standard additive methods and was assessed as a continuous variable [31]. NYHA functional classification provides a simple way of classifying the extent of heart failure. It places patients in one of four categories based on how much they are limited during physical activity; Class I denotes normal activity and class IV indicates there are problems such as dyspnea even at rest [32].
Anthropometric assessments
Anthropometric variables including weight and height were measured and body mass index (BMI) was calculated. Weight was measured while subjects wearing light clothes [33].
Dietary assessments and calculation of total antioxidant capacity
Total antioxidant capacity of diet (TAC) was calculated based on a 138-item semi-quantitative food frequency questionnaire (FFQ) consisting of a list of foods with standard serving sizes commonly consumed by Iranians. Participants were asked to report how often they consumed each of the food items listed as the number of times per day, per week, per month or per year during the previous year. The reported frequency for each food item was then converted to a daily intake. Portion sizes of consumed foods were converted to grams by using household measures [34]. The questionnaire was previously validated for healthy Iranian population [35]. TAC was calculated using Trolox equivalent according to previous database of the common foods antioxidant capacity estimated by Oxygen Radical Absorbance Capacity (ORAC) assay [36, 37]. The ORAC assay measures the inhibition of peroxyl radical–induced oxidation by the test sample and is expressed as μmol-Trolox equivalent (TE)/100g; Trolox is a potent antioxidant derived from vitamin E [37]. The total antioxidant capacity of diet was calculated by multiplying the average frequency of consumption of each food by ORAC content (μmol TE/100 g) of age-specific portion sizes. Overall, in the 138-item food-frequency questionnaire there were 100 items with ORAC values. Total antioxidant capacity of diet was adjusted for total energy intake with the residual method [38].
Statistics
Analysis of data was performed by SPSS software (statistical package for social analysis, version 18, SPSS Inc., Chicago, IL, USA). The normality of data was tested by Kolmogorov-Smirnov test. The comparison of discrete and continuous variables between different quartiles of TAC score was performed by Chi- square test and analysis of variance (ANOVA) respectively. Odds ratios and 95% confidence intervals for the association between different TAC quintiles and clinical parameters were estimated using multivariate multinomial logistic regression models adjusting for confounders including age, BMI, educational attainment and presence of diabetes and myocardial infarction. All data are expressed as means ± SD or number and percent. A two-sided P value less than 0.05 was considered significant.
Results
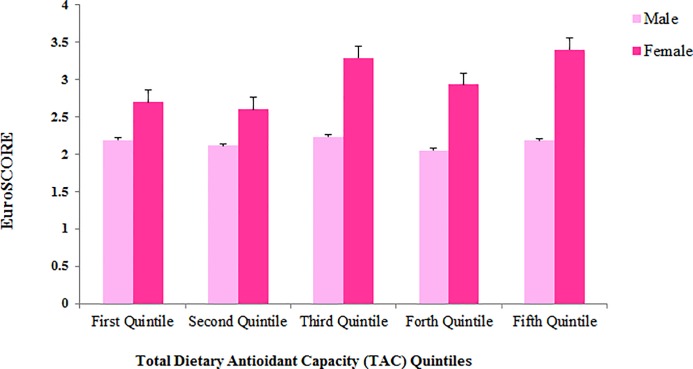
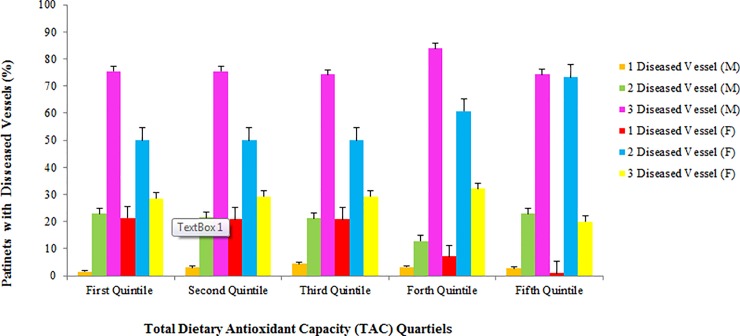
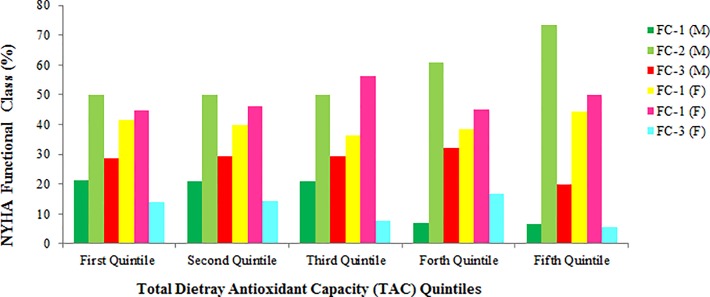
Table 1 presents the baseline characteristics of male participants in different TAC quintiles. Male patients in the first quintile of TAC had significantly higher prevalence of hypertension compared with other quintiles. Other parameters including age, BMI, presence of MI, diabetes, smoking and hyperlipidemia were not significantly different between patients’ in different TAC quintiles. Moreover, in females (Table 2), none of these parameters were different (P > 0.05). As shown in Table 3, male patients in second and fifth quintile of TAC had 2–3% higher amounts of serum vitamin D compared with first quintile (P <0.05). Moreover, male patients in the second, third, fourth and fifth quintiles, had approximately 10–17% lower hematocrit concentrations compared with first quintile and being in top quintiles of TAC was associated with higher serum albumin concentrations. In female participants (Table 4), however, only serum creatinine concentration was in negative association with TAC. In comparison of clinical parameters in study participants in a gender separated analysis (Figs 1–4), female in the fifth quintile of TAC had 9% higher left ventricular ejection-fraction compared with patients in the first quintile (P = 0.021).
Table 1. Baseline characteristics of male patients candidate for CABG according to TAC quintiles.
| Quintiles of TAC score | ||||||
|---|---|---|---|---|---|---|
| Variable | 1st quintiles | 2nd quintiles | 3rd quintiles | 4th quintiles | 5th quintiles | P value |
| N = 61 | N = 66 | N = 66 | N = 62 | N = 74 | ||
| Age (y) | 60.02±10.51 | 59.88 ±10.07 | 57.68±8.61 | 57.42±9.37 | 58.50±8.56 | 0.38 |
| BMI (kg/m2) | 25.84±3.52 | 27.17±2.96 | 26.89±3.69 | 26.36±3.52 | 26.86±3.75 | 0.22 |
| Diabetic [n (%)] | 20 (32.8) | 19 (28.8) | 25 (37.9) | 23 (37.1) | 22 (29.7) | 0.95 |
| Smokers [n (%)] | 25 (41) | 26 (39.4) | 36 (54.5) | 33 (53.2) | 33 (44.6) | 0.32 |
| Hyperlipidemia [n (%)] | 42 (68.9) | 41 (62.1) | 46 (69.7) | 39 (62.9) | 46 (62.2) | 0.5 |
| Hypertension [n (%)] | 28 (45.9) | 33 (50) | 25 (37.9) | 17 (27.4) | 26 (35.1) | 0.023 |
| MI [n (%)] | 31 (51.7) | 31 (47) | 35 (53.8) | 38 (61.3) | 45 (60.8) | 0.09 |
BMI, body mass index; MI, myocardial Infarction; P value for discrete variables based on Chi-Square Test and for continuous variables based on ANOVA. Discrete and continuous variables data are presented as number (percent) and mean (SD). High educational attainment was defined as educational level more than 12 years.
Table 2. Baseline characteristics of female patients candidate for CABG according to TAC quintiles.
| Quintiles of TAC score | ||||||
|---|---|---|---|---|---|---|
| Variable | 1st quintiles | 2nd quintiles | 3rd quintiles | 4th quintiles | 5th quintiles | P value |
| N = 28 | N = 24 | N = 24 | N = 28 | N = 15 | ||
| Age (y) | 61.79± 8.35 | 57.33 ±6.68 | 59.21± 6.11 | 58.57 ± 6.81 | 60.60± 9.55 | 0.25 |
| BMI (kg/m2) | 28.89± 5.38 | 31.30± 4.33 | 28.77 ±4.39 | 29.62± 4.79 | 28.57±3.78 | 0.27 |
| Diabetic [n (%)] | 19 (67.9) | 18 (75) | 16 (66.7) | 19 (67.9) | 8 (53.3) | 0.37 |
| Smokers [n (%)] | 1 (3.6) | 0 | 0 | 2 (7.1) | 0 | 0.81 |
| Hyperlipidemia [n (%)] | 25 (89.3) | 23 (95.8) | 21 (87.5) | 23 (82.1) | 14 (93.3) | 0.61 |
| Hypertension [n (%)] | 18 (64.3) | 16 (66.7) | 20 (83.3) | 21 (75) | 10 (66.7) | 0.48 |
| MI [n (%)] | 8 (28.6) | 11 (45.8) | 13 (54.2) | 10 (35.7) | 3 (20) | 0.71 |
BMI, body mass index; MI, myocardial Infarction; P value for discrete variables based on Chi-Square Test and for continuous variables based on ANOVA. Discrete and continuous variables data are presented as number (percent) and mean (SD). High educational attainment was defined as educational level more than 12 years.
Table 3. Odd’s ratio (OR) and confidence interval (CI) for the association between TAC and biochemical variables in male patients candidate for CABG.
| Quintile of TAC score | |||||
|---|---|---|---|---|---|
| Variable | 1st quintile | 2nd quintile | 3rd quintile | 4th quintile | 5th quintile |
| N = 61 | N = 66 | N = 66 | N = 62 | N = 74 | |
| Serum vitamin D (ng/ml) | 1 (Ref.) | 1.03 (1.02–1.07) | 1.02 (0.99–1.05) | 0.99 (0.96–1.03) | 1.02 (0.98–1.05) |
| HbA1C (%) | 1 (Ref.) | 1.08 (0.87–1.35) | 1.01 (0.81–1.27) | 1.12 (0.90–1.39) | 1.06 (0.86–1.32) |
| TC (mg/dl) | 1 (Ref.) | 0.98 (0.95–1.02) | 1.02 (0.98–1.06) | 0.98 (0.95–1.09) | 0.97 (0.94–1.003) |
| TG (mg/dl) | 1 (Ref.) | 1.00 (0.99–1.002) | 0.99 (0.98–1.002) | 1.01 (0.99–1.01) | 1.01 0.99–1.009) |
| LDL (mg/dl) | 1 (Ref.) | 1.02 (0.98–1.05) | 0.98 (0.94–1.02) | 1.01 (0.97–1.04) | 1.02 (0.99–1.06) |
| HDL (mg/dl) | 1 (Ref.) | 1.01 (0.95–1.07) | 0.97 (0.92–1.044) | 1.02 (0.96–1.08) | 1.04 (0.98–1.10) |
| HCT (%) | 1 (Ref.) | 0.90 (0.82–0.99) | 0.86 (0.78–0.95) | 0.83 (0.75–0.93) | 0.89 (0.81–0.99) |
| Albumin (g/dL) | 1 (Ref.) | 2.94 (0.87–9.92) | 2.55 (0.75–8.68) | 3.43 (0.95–12.32) | 4.18 (1.27–13.77) |
| Creatinine (mg/dL) | 1 (Ref.) | 0.84 (0.15–4.69) | 0.86 (0.15–4.96) | 0.27 (0.04–1.9) | 1.03 (0.19–5.52) |
| BUN (mg/dL) | 1 (Ref.) | 0.98 (0.95–1.02) | 0.97 (0.93–1.01) | 0.99 (0.96–1.03) | 0.98 (0.95–1.02) |
| Lipoprotein (a) (mg/dL) | 1 (Ref.) | 0.99 (0.98–1.02) | 1.001 (0.98–1.02) | 1.01 (0.98–1.02) | 0.99 (0.98–1.01) |
| CRP (mg/dL) | 1 (Ref.) | 1.02 (0.99–1.13) | 0.92 (0.80–1.06) | 1.01 (0.89–1.12) | 1.02 (0.92–1.12) |
CI, confidence interval; TAC, total dietary antioxidant capacity; Hb, hemoglobin; TC, total cholesterol; TG, triglyceride; LDL, low density lipoprotein cholesterol; HDL, high density lipoprotein cholesterol; HCT, hematocrit; BUN, blood urea nitrogen; Lp, lipoprotein; CRP, C-reactive protein. The multivariate multinomial logistic regression was used for estimation of ORs and confidence interval (CI) with adjustment for the confounding effects of age, gender, BMI and presence of diabetes and myocardial infarction. Bold digits indicate statistically significant values as P < 0.05.
Table 4. Odd’s ratio (OR) and confidence interval (CI) for the association between TAC and biochemical variables in female patients candidate for CABG.
| Quartiles of TAC score | |||||
|---|---|---|---|---|---|
| Variable | 1st quartile | 2nd quartile | 3rd quartile | 4th quartile | 5th quintile |
| N = 24 | N = 24 | N = 28 | N = 15 | N = 74 | |
| Vitamin D (ng/ml) | 1 (Ref.) | 0.94 (0.90–0.99) | 0.99 (0.95–1.04) | 0.99 (0.95–1.04) | 0.94 (0.89–0.99) |
| HbA1C (%) | 1 (Ref.) | 1.17 (0.76–1.81) | 0.93 (0.59–1.43) | 0.97(0.64–1.47) | 0.80 (0.48–1.34) |
| TC (mg/dl) | 1 (Ref.) | 1.37 (0.84–2.24) | 1.31 (0.79–2.15) | 1.35 (0.83–2.21) | 1.31 (0.78–2.21) |
| TG (mg/dl) | 1 (Ref.) | 0.93 (0.85–1.03) | 0.95 (0.85–1.05) | 0.94 (0.85–1.03) | 0.94 (0.85–1.05) |
| LDL (mg/dl) | 1 (Ref.) | 0.71 (0.45–1.68) | 0.75 (0.45–1.24) | 0.73 (0.45–1.20) | 0.75 (0.44–1.26) |
| HDL (mg/dl) | 1 (Ref.) | 0.71 (0.44–1.61) | 0.80 (0.48–1.31) | 0.75 (0.46–1.23) | 0.73 (0.44–1.26) |
| HCT (%) | 1 (Ref.) | 1.11 (0.89–1.40) | 1.01 (0.81–1.24) | 1 (0.80–1.25) | 1.05 (0.82–1.35) |
| Albumin (g/dL) | 1 (Ref.) | 3.85 (0.45–33.20) | 0.2 (0.02–1.55) | 0.83 (0.13–5.53) | 1.27 (0.12–12.16) |
| Creatinine (mg/dL) | 1 (Ref.) | 0.22(0.002–20.82) | 0.01 (0–1.99) | 0.58 (0.01–32.15) | 0.02 (0–3.58) |
| BUN (mg/dL) | 1 (Ref.) | 1.07 (0.99–1.15) | 1.07 (0.98–1.15) | 1.03 (0.95–1.03) | 1.01 (0.92–1.10) |
| Lp (a) (mg/dL) | 1 (Ref.) | 1.01 (0.98–1.03) | 0.99 (0.96–1.07) | 1.01(0.99–1.03) | 1.02 (0.99–1.04) |
| CRP (mg/dL) | 1 (Ref.) | 1.02 (0.86–1.2) | 1.11 (0.94–1.31) | 0.84 (0.63–1.12) | 0.84 (0.55–1.28) |
CI, confidence interval; TAC, total dietary antioxidant capacity; Hb, hemoglobin; TC, total cholesterol; TG, triglyceride; LDL, low density lipoprotein cholesterol; HDL, high density lipoprotein cholesterol; HCT, hematocrit; BUN, blood urea nitrogen; Lp, lipoprotein; CRP, C-reactive protein. The multivariate multinomial logistic regression was used for estimation of ORs and confidence interval (CI) with adjustment for the confounding effects of age, gender, BMI and presence of diabetes and myocardial infarction. Bold digits indicate statistically significant values as P < 0.05.
Fig 1. European system for cardiac operative risk evaluation (EuroSCORE) in patients according to TAC quintiles; no significant difference was observed.
Fig 4. Number of diseased vessels in patients according to TAC quintiles; no significant difference between different quintiles of TAC has been observed.
Fig 2. New York Heart Association (NYHA) functional class in patients according to TAC quartiles; no significant difference between different quintiles of TAC has been observed.
Fig 3. Left ventricular ejection-fraction in patients according to TAC quartiles; female in the fifth quintile of TAC had 9% higher EF compared with patients in the first quintile (P = 0.021).
Discussion
According to the results of the current work, high total antioxidant capacity of the diet was associated with the lower prevalence of hypertension, lower hematocrit and higher serum albumin concentrations in male candidate for CABG. Moreover, higher serum vitamin D was also accompanied with higher TAC in males which was a novel finding by itself. In females, however, only lower serum creatinine was associated with high TAC values.
In recent years, there are emerging evidences supporting the role of oxidative stress in the pathogenesis of hypertension [39–41]. Numerous studies even demonstrated that hypertension is the result of increase reactive oxygen species (ROS) [42–44] and antioxidant therapy relieves hypertension in animal or human models. It has been proposed that several possible underlying mechanisms of the role of oxidative stress in the pathophysiology of hypertension are increased reactive aldehyde, methylglyoxal, disrupted vascular calcium channels, enzymes, [45] oxidation of low-density lipoproteins, primarily by oxygen-free radicals [46], reduced bioactivity of NO and the activation of NAD(P)H oxidase in long term development of hypertension [47]. Several studies also have reported the negative association between dietary antioxidants intakes and development of hypertension; in the study by Kumar et al dietary antioxidant vitamin intake in hypertensive individuals were lower than normotensive individuals [48]. In another study by Rodriguez-Iturbe et al [49] antioxidant-enriched diet reduced the renal interstitial inflammation and improved hypertension in spontaneously hypertensive rats. In the current study, for the first time, we revealed the possible protective role of total dietary antioxidant capacity as a global measure of antioxidant potential of diet against hypertension. Numerous previous studies have revealed that elevated hematocrit concentration is a well-known risk factor of cardiovascular disease [50, 51]; these associations were gender-specific with more pronunciation in men possibly because of higher blood hematocrit concentrations in men; however several other studies also revealed the higher risk of CVD in women by elevated hematocrit concentrations [52]. Increased hematocrit concentrations is involved in increased CVD risk via: increased blood viscosity and raising peripheral resistance, reducing blood flow and perfusion [53], activation of platelets by releasing adenosine diphosphate (ADP) [54] and increased oxidative stress and lipid peroxidation by accumulated iron [55]. In our study, higher TAC of diet was associated with lower hematocrit concentrations; a valuable finding confirming the possible protective role of dietary antioxidants in reducing HCT and reducing the risk of CVD.
The direct association between higher serum albumin concentrations and high total dietary antioxidant capacity is also an evidence of the protective role of dietary antioxidants against CVD risk factors; in has been clarified that reduced serum albumin concentration is a known risk factor of cardiovascular events [56] and measuring its concentration could be a valuable diagnostic marker in the risk prediction of CVD [57]. Reduced serum albumin concentrations is associated with increased mortality from CVD, stroke and chronic heart disease [58]. Albumin has major antioxidant capabilities; it is a major antioxidant in plasma, accounting for 70% of free radical-trapping activity of serum due to its thiol group and high plasma concentration [59]. In addition, the ligand-binding ability of albumin contributes to its antioxidant ability because it limits the oxidation of LDL from copper or hydroxyl radical production from iron reaction with hydroperoxide [60]. It has been reported that increased serum albumin per unit is associated with a 12% reduced risk of CVD incidence over a three-year period [61]. Our study demonstrated that increased dietary antioxidant capacity increases serum albumin concentrations in men confirming its antioxidant capabilities. Another finding of the current study was increased serum vitamin D concentration in parallel of increased TAC. Vitamin D exerts its antioxidant actions by reduced peroxidation of lipids, suppression of nicotine amide adenine dinucleotide phosphate enzyme expression and inhibition of the AGEs accumulation in the cardiac vessels [62, 63]. Moreover, vitamin D reduces impairment in endothelial tissue after hydrogen superoxide induced stress and prevents ROS production by inhibiting MEKs/ERKs/SIRT-1 axis switching [64, 65]. Vitamin D exerts its cardio-protective effects via anti-oxidant and anti-inflammatory roles which have been clarified previously [66].
In addition, in men also high TAC scores were associated with lower TC concentrations. Dietary and supplementary antioxidant therapy is associated with lipid and cholesterol lowering effects as indicated in numerous previous studies [67, 68]. However, our study revealed an inverse association between dietary antioxidant capacity and TC as a major CVD risk factor.
Several limitations of the current study should also be addressed; the self-reported dietary information, not measuring indices of central adiposity were potential limitations of the current study. The study’s relatively large sample size and inclusion of multiple confounders in the statistical model are potent strengths of the current study. Moreover, this is the first study evaluated the association between TAC and CVD risk factors in patients candidate for CABG.
Conclusion
In conclusion, our study, for the first time revealed that total dietary antioxidant capacity as a global measure of dietary antioxidant has a potential association with the major cardiovascular risk factors including HCT, TC, albumin and serum vitamin D in patients’ candidate for CABG. These associations were gender-specific with more pronunciation in men. CABG role as a trigger of oxidative stress and increased free radicals has been reported before, so, the findings of the current study has a major beneficial applications in advising these patients to increase their dietary antioxidant capability to reduce the CVD risk factors.
Supporting information
(SAV)
Acknowledgments
The authors appreciate the cooperation of the patients in the current work.
Abbreviations
- TAC
total dietary antioxidant capacity
- ANOVA
analysis of variance
- CAD
coronary artery disease
- CVD
cardiovascular disease
- HDL
high density lipoprotein cholesterol
- LDL
low density lipoprotein cholesterol
- TC
total cholesterol
- LP
lipoprotein
- CABG
coronary artery bypass grafting surgery
- CRP
C-reactive protein
Data Availability
The raw data and other materials in the current study are available as supporting files for all of the researchers throughout the world for scientific use with kind full permission.
Funding Statement
This research received a grant from the research undersecretary of Tabriz University of Medical Sciences, Tabriz, Iran.
References
- 1.Islamic Republic News Agency (IRNA). 50 thousand heart surgeries performed annually in the country. Available from: http://www.irna.ir/fa/News/80650875/. 2016.
- 2.Konstantinov IE. The first coronary artery bypass operation and forgotten pioneers. Ann Thorac Surg 1997. 64(5): 1522–3. 10.1016/S0003-4975(97)00928-4 [DOI] [PubMed] [Google Scholar]
- 3.Veterans Administration Coronary Artery Bypass Surgery Cooperative Study Group. Eleven-year survival in the Veterans Administration randomized trial of coronary bypass surgery for stable angina. N Engl J Med. 1984; 311(21): 1333–9. 10.1056/NEJM198411223112102 [DOI] [PubMed] [Google Scholar]
- 4.Shahani R. Coronary Artery Bypass Grafting. 2017; Available from: https://emedicine.medscape.com/article/1893992-overview.
- 5.World Health Organization (WHO). Cardiovascular Disease (CVDs) 2017; Available from: http://www.who.int/mediacentre/factsheets/fs317/en/.
- 6.Hatmi ZN, Tahvildari S, Motlag AG, Kashani AS. Prevalence of coronary artery disease risk factors in Iran: a population based survey. BMC Cardiovas Disord.2007; 7: 32–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vassalle C, Botto N, Andreassi MG, Biagini B. Evidence for enhanced 8-isoprostane plasma levels, as index of oxidative stress in vivo, in patients with coronary artery disease. Coron Artery Dis 2003; 14(3): 213–8. 10.1097/01.mca.0000063504.13456.c3 [DOI] [PubMed] [Google Scholar]
- 8.Cohen MV. Free radicals in ischemic and reperfusion myocardial injury: is this the time for clinical trials? Ann Intern Med 1989; 111(11): 918–31. [DOI] [PubMed] [Google Scholar]
- 9.Heinecke JW. Is the emperor wearing clothes? Clinical trials of vitamin E and the LDL oxidation hypothesis. Arterioscler Thromb Vasc Bio 2001; 21(8): 1261–4. [DOI] [PubMed] [Google Scholar]
- 10.D'souza AB, Vishwanath P, D'souza V. Oxidative injury and antioxidants in coronary artery bypass graft surgery: Off-pump CABG significantly reduces oxidative stress. Clinica Chimica Acta 2007; 375(1–2): 147–152. [DOI] [PubMed] [Google Scholar]
- 11.Dias AE, Melnikov P, Zélia L, Consolo Z. Oxidative stress in coronary artery bypass surgery. Braz J Cardiovasc Surg 2015; 30(4): 417–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavalca V, Tremoli E, Porro B, Veglia F, Myasoedova V, Squellerio I, et al. Oxidative stress and nitric oxide pathway in adult patients who are candidates for cardiac surgery: patterns and differences. Interact Cardiovasc Thorac Surg 2013; 17(6): 923–930. 10.1093/icvts/ivt386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Plicner D, Stoliński J, Wąsowicz M, Gawęda B, Hymczak H, Kapelak B, et al. Preoperative values of inflammatory markers predict clinical outcomes in patients after CABG, regardless of the use of cardiopulmonary bypass. Indian Heart Journa 2016; 68 (S3): S10–S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lichtenstein AH, Appel LJ, Brands M, Carnethon M, Daniels S, Franch HA, et al. Diet and lifestyle recommendations revision 2006 A scientific statement from the American Heart Association nutrition committee. Circulation 2006; 114(1): 82–96. 10.1161/CIRCULATIONAHA.106.176158 [DOI] [PubMed] [Google Scholar]
- 15.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Aros F, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. New Engl J Med 2013; 368 (14): 1279–1290. 10.1056/NEJMoa1200303 [DOI] [PubMed] [Google Scholar]
- 16.Shaikh AK, Suryakar A. Oxidative stress and antioxidant status before and after supplementation of A-Z anti-oxidant tablets in coronary artery disease. Biomedical Research 2009; 20(2): 136–140. [Google Scholar]
- 17.Stanger O, Aigner I, Schimetta W, Wonisch W. Antioxidant supplementation attenuates oxidative stress in patients undergoing coronary artery bypass graft surgery. Tohoku J Exp Med. 2014; 232(2): 145–54. [DOI] [PubMed] [Google Scholar]
- 18.Rautiainen S, Serafini M, Morgenstern R, Prior RL, Wolk A. The validity and reproducibility of food-frequency questionnaire-based total antioxidant capacity estimates in Swedish women. Am J Clin Nutr 2008; 87: 1247–1253. 10.1093/ajcn/87.5.1247 [DOI] [PubMed] [Google Scholar]
- 19.Zujko ME, Witkowska AM, Waśkiewicz A, Piotrowski W, Terlikowska KM. Dietary antioxidant capacity of the patients with cardiovascular disease in a cross-sectional study. Nutrition Journal 2015; 14:26: 26–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rautiainen S, Levitan EB, Orsini N, Åkesson A, Morgenstern R, Mittleman MA, et al. Total antioxidant capacity from diet and risk of myocardial infarction: a prospective cohort of women. Am J Med 2012; 125(10): 974–80. 10.1016/j.amjmed.2012.03.008 [DOI] [PubMed] [Google Scholar]
- 21.Rautiainen S, Levitan EB, Mittleman MA, Alicja Wolk A, MedScib D. Total antioxidant capacity of diet and risk of heart failure: A population-based prospective cohort of women. Am J Med 2013; 126: 494–500. 10.1016/j.amjmed.2013.01.006 [DOI] [PubMed] [Google Scholar]
- 22.Rautiainen S, Larsson S, Virtamo J, Wolk A. Total antioxidant capacity of diet and risk of stroke: a population-based prospective cohort of women. Stroke 2012; 43: 335–340. 10.1161/STROKEAHA.111.635557 [DOI] [PubMed] [Google Scholar]
- 23.Wiseman H. Vitamin D is a membrane antioxidant Ability to inhibit iron-dependent lipid peroxidation in liposomes compared to cholesterol, ergosterol and tamoxifen and relevance to anticancer action. FEBS Lett. 1993; 326: 285–8. [DOI] [PubMed] [Google Scholar]
- 24.Murr C, Pilz S, Grammer TB, Kleber ME, Meinitzer A, Boehm BO. Vitamin D deficiency parallels inflammation and immune activation, the Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Clin Chem Lab Med 2012; 50(12): 2205–2212. 10.1515/cclm-2012-0157 [DOI] [PubMed] [Google Scholar]
- 25.Farhangi MA, Najafi M. Dietary inflammatory index: a potent association with cardiovascular risk factors among patients candidate for coronary artery bypass grafting (CABG) surgery. Nutrition Journal 2018; 17: 20–30. 10.1186/s12937-018-0325-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Najafi M, Sheikhvatan M. Gender differences in coronary artery disease: correlational study on dietary pattern and known cardiovascular risk factors. Int Cardiovasc Res J. 2013; 7(4): 124–129. [PMC free article] [PubMed] [Google Scholar]
- 27.Farhangi MA, Ataie-Jafari A, Najafi M, Foroushani GS, Tehrani MM, Jahangiry L. Gender differences in major dietary patterns and their relationship with cardio-metabolic risk factors in a year before coronary artery bypass grafting (CABG) surgery period. Arch Iran Med. 2016; 19(7): 470–479. [PubMed] [Google Scholar]
- 28.Farhangi MA, Najafi M, Jafarabadi MA, Jahangiry L. Mediterranean dietary quality index and dietary phytochemical index among patients candidate for coronary artery bypass grafting (CABG) surgery. BMC Cardiovascular Disorders 2017; 17: 114–122. 10.1186/s12872-017-0544-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Maria R, Mazzoni M, Parolini M, Gregori D, Bortone F, Arena V, et al. Predictive value of EuroSCORE on long term outcome in cardiac surgery patients: a single institution study. Heart 2005; 91: 779–784. 10.1136/hrt.2004.037135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maria RD, Mazzoni M, Parolini M, Gregori D, Bortone F, Arena V, et al. Predictive value of EuroSCORE on long term outcome in cardiac surgery patients: a single institution study. Heart 2005; 91(6(6): 779–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nashef SAM, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardio-Thoracic Surg 1999; 16 9–13. [DOI] [PubMed] [Google Scholar]
- 32.Association., T.C.C.o.t.N.Y.H., Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9 ed 1994, Boston: Little, Brown & Co. [Google Scholar]
- 33.Mirinazhad MM, Farhangi MA, Jahangiri L, Yaghoubi A. Serum adiponectin concentrations in relation to lipid proffle, anthropometric variables and insulin resistance in patients with metabolic syndrome. Malay J Nutr 2014; 20(3): 283–289. [Google Scholar]
- 34.Ghaffarpour M, Houshiar-Rad A, Kianfar H, The manual for household measures, cooking yields factors and edible portion of foods (In Persian). 1999, Tehran, Iran: Keshaverzi Press. [Google Scholar]
- 35.Esmaillzadeh A, Mirmiran P, Azizi F. Whole-grain intake and the prevalence of hypertriglyceridemic waist phenotype in Tehranian adults. Am J Clin Nutr 2005; 81: 55–63. 10.1093/ajcn/81.1.55 [DOI] [PubMed] [Google Scholar]
- 36.Wu X, Beecher GR, Holden JM. Lipophilic and hydrophilic antioxidant capacities of common foods in the United States. J Agric Food Chem 2004; 52:: 4026–4037. 10.1021/jf049696w [DOI] [PubMed] [Google Scholar]
- 37.Sanchez-Moreno C, Cao G, Ou B, Prior RL. Anthocyanin and proanthocyanidin content in selected white and red wines. Oxygen radical absorbance capacity comparison with nontraditional wines obtained from highbush blueberry. J Agric Food Chem 2003; 51: 4889–4896. 10.1021/jf030081t [DOI] [PubMed] [Google Scholar]
- 38.Willett WC, Nutritional Epidemiology. 2nd ed ed. 1998, New York: Oxford University Press. [Google Scholar]
- 39.Berry C, Brosnan MJ, Fennell J, Hamilton CA, Dominiczak AF. Oxidative stress and vascular damage in hypertension. Curr Opin Nephrol Hypertens. 2001; 10: 247–255. [DOI] [PubMed] [Google Scholar]
- 40.Dhalla NS, Temsah RM, Netticadan T. Role of oxidative stress in cardiovascular diseases. J Hypertens. 2000; 18: 655–673. [DOI] [PubMed] [Google Scholar]
- 41.Schnackenberg CG. Physiological and pathophysiological roles of oxygen radicals in the renal microvasculature. Am J Physiol (Regulatory Physiol) 2002; 282: R335–R342. [DOI] [PubMed] [Google Scholar]
- 42.Barton CH, Ni Z, Vaziri ND. Enhanced nitric oxide inactivation in aortic coarctation-induced hypertension. Kidney Int. 2001; 60: 1083–1087. 10.1046/j.1523-1755.2001.0600031083.x [DOI] [PubMed] [Google Scholar]
- 43.Makino A, Skelton MM, Zou AP, Roman RJ, Cowley AW Jr. Increased renal medullary oxidative stress produces hypertension. Hypertension 2002; 39: 667–672. [DOI] [PubMed] [Google Scholar]
- 44.Zhou XJ, Vaziri ND, Wang XQ, Silva FG, Laszik Z. Nitric oxide synthase expression in hypertension induced by inhibition of glutathione synthase. J Pharmacol Exp Ther. 2002; 300: 762–767. [DOI] [PubMed] [Google Scholar]
- 45.Tripathi JS, Byadgi PS, Narasimha MK. The role of psychological factors in aetiopathogenesis and management of obesity related disease. J Appl Pharm Sci. 2011; 1(5): 32–34. [Google Scholar]
- 46.Witztum JL, Steinberg D. The oxidative modification hypothesis of atherosclerosis: does it hold for humans? Trends Cardiovasc Med. 2001. 11(3–4): 93–102. [DOI] [PubMed] [Google Scholar]
- 47.Förstermann U. Nitric oxide and oxidative stress in vascular disease. Pflugers Arch. 2010. 459(6): 923–39. 10.1007/s00424-010-0808-2 [DOI] [PubMed] [Google Scholar]
- 48.Kumar A. Correlation between anthropometric measurement, lipid profile, dietary vitamins, serum antioxidants, lipoprotein (a) and lipid peroxides in known cases of 345 elderly hypertensive South Asian aged 56–64 y-A hospital based study. Asian Pac J Trop Biomed 2014; 4(Suppl 1): S189–S197. doi: 10.12980/APJTB.4.2014D153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rodriguez-Iturbe B, Zhan CD, Quiroz Y, Sindhu PK, Vaziri ND. Antioxidant-rich diet relieves hypertension and reduces renal immune infiltration in spontaneously hypertensive rats. Hypertension. 2003; 41: 341–346. [DOI] [PubMed] [Google Scholar]
- 50.Carter C, McGee D, Reed D, Yano K, Stemmermann G. Hematocrit and the risk of coronary heart disease: the Honolulu Heart Program. Am Heart J. 1983; 105: 674–679. [DOI] [PubMed] [Google Scholar]
- 51.Campbell MJ, Elwood PC, Mackean J, Waters WE. Mortality, haemoglobin level and haematocrit in women. J Chronic Dis 1985; 38: 881–889. [DOI] [PubMed] [Google Scholar]
- 52.Gagnon DR, Zhang TJ, Brand FN, Kannel WB. Hematocrit and the risk of cardiovascular disease—the Framingham study: a 34-year follow-up. Am Heart J. 1994. 127(3): 674–82. [DOI] [PubMed] [Google Scholar]
- 53.Burch GE, DePasquale NP. Hematocrit, viscosity and coronary blood flow. Dis Chest. 1965. 48(3): 225–32. [DOI] [PubMed] [Google Scholar]
- 54.Lowe GD, Forbes CD. Platelet aggregation, haematocrit, and fibrinogen. Lancet. 1985. 16(1(8425)): 395–6. [DOI] [PubMed] [Google Scholar]
- 55.Salonen JT, Nyyssönen K, Korpela H, Tuomilehto J, Seppänen R, Salonen R. High stored iron levels are associated with excess risk of myocardial infarction in eastern Finnish men. Circulation 1992. 86(3): 803–11. [DOI] [PubMed] [Google Scholar]
- 56.Shaper AG, Wannamethee SG, Whincup PH. Serum albumin and risk of stroke, coronary heart disease, and mortality: the role of cigarette smoking. J Clin Epidemiol. 2004; 57(2): 195–202. 10.1016/j.jclinepi.2003.07.001 [DOI] [PubMed] [Google Scholar]
- 57.Chien SC, Chen CY, Lin CF, Yeh HI. Critical appraisal of the role of serum albumin in cardiovascular disease. Biomark Res. 2017; 5: 31–41. 10.1186/s40364-017-0111-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kuller LH, Eichner JE, Orchard TJ, Grandits GA, McCallum L, Tracy RP. The relation between serum albumin levels and risk of coronary heart disease in the multiple risk factor intervention trial. Am J Epidemiol 1991; 134(11): 1266–1277. [DOI] [PubMed] [Google Scholar]
- 59.Roche M, Rondeau P, Singh NR, Tarnus E, Bourdon E. The antioxidant properties of serum albumin. FEBS. Lett 2008;; 582: 1783–1787. 10.1016/j.febslet.2008.04.057 [DOI] [PubMed] [Google Scholar]
- 60.Bar-Or D, Rael LT, Lau EP, Rao NK, Thomas GW, Winkler JV. An analog of the human albumin N-terminus (Asp-Ala-His-Lys) prevents formation of copper-induced reactive oxygen species. Biochem. Biophys. Res. Commun. 2001; 284: 856–862. 10.1006/bbrc.2001.5042 [DOI] [PubMed] [Google Scholar]
- 61.Schalk BW, Visser M, Bremmer MA, Penninx BW, Bouter LM, Deeg DJ. Change of serum albumin and risk of cardiovascular disease and all-cause mortality: Longitudinal Aging Study Amsterdam. Am J Epidemiol. 2006; 164: 969–977. 10.1093/aje/kwj312 [DOI] [PubMed] [Google Scholar]
- 62.Tarcin O, Yavuz DG, Ozben B, Telli A, Ogunc AV, Yuksel M. Effect of vitamin D deficiency and replacement on endothelial function in asymptomatic subjects. J Clin Endocrinol Metab 2009; 94: 4023–30. 10.1210/jc.2008-1212 [DOI] [PubMed] [Google Scholar]
- 63.Hirata M, Serizawa K, Aizawa K, Yogo K, Tashiro Y, Takeda S. 22-Oxacalcitriol prevents progression of endothelial dysfunction through antioxidative effects in rats with type 2 diabetes and early-stage nephropathy. Nephrol Dial Transplant. 2013; 28: 1166–74. 10.1093/ndt/gfs536 [DOI] [PubMed] [Google Scholar]
- 64.Polidoro L, Properzi G, Marampon F, Gravina GL, Festuccia C, Di Cesare E. Vitamin D protects human endothelial cells from H(2)O(2) oxidant injury through the Mek/Erk- Sirt1 axis activation. J Cardiovasc Transl Res 2013; 6: 221–31. 10.1007/s12265-012-9436-x [DOI] [PubMed] [Google Scholar]
- 65.Uberti F, Lattuada D, Morsanuto V, Nava U, Bolis G, Vacca G. Vitamin D protects human endothelial cells from oxidative stress through the autophagic and survival pathways. J Clin Endocrinol Metab 2014; 99: 1367–74. 10.1210/jc.2013-2103 [DOI] [PubMed] [Google Scholar]
- 66.Farhangi MA, Nameni G, Hajiluian G, Mesgari-Abbasi M. Cardiac tissue oxidative stress and inflammation after vitamin D administrations in high fat- diet induced obese rats. BMC Cardiovasc Disord. 2017; 17:: 161–171. 10.1186/s12872-017-0597-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Amom Z, Zakaria Z, Mohamed J, Azlan A, Bahari H, Baharuldin MTH, et al. Lipid lowering effect of antioxidant alpha-lipoic acid in experimental atherosclerosis. J Clin Biochem Nutr. 2008. 43(2): 88–94. 10.3164/jcbn.2008051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Crawford RS, Kirk EA, Rosenfeld ME, LeBoeuf RC, Chait A. Dietary antioxidants inhibit development of fatty streak lesions in the LDL receptor–deficient mouse. Arterioscler Thromb Vasc Biol. 1998; 18: 1506–1513. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
The raw data and other materials in the current study are available as supporting files for all of the researchers throughout the world for scientific use with kind full permission.