Abstract
BACKGROUND CONTEXT:
With the changing landscape of health care, outpatient spine surgery is being more commonly performed to reduce cost and to improve efficiency. Anterior cervical discectomy and fusion (ACDF) is one of the most common spine surgeries performed and demand is expected to increase with an aging population.
PURPOSE:
The objective of this study was to determine the nationwide trends and relative complication rates associated with outpatient ACDF.
STUDY DESIGN/SETTING:
This is a large-scale retrospective case control study.
PATIENT SAMPLE:
The patient sample included Humana-insured patients who underwent one- to two-level ACDF as either outpatients or inpatients from 2011 to 2016
OUTCOME MEASURES:
The outcome measures included incidence and the adjusted odds ratio (OR) of postoperative medical and surgical complications within 1 year of the index surgery.
MATERIALS AND METHODS:
A retrospective review was performed of the PearlDiver Humana insurance records database to identify patients undergoing one- to two-level ACDF (Current Procedural Terminology [CPT]-22551 and International Classification of Diseases [ICD]-9-816.2) as either outpatients or inpatients from 2011 to 2016. The incidence of perioperative medical and surgical complications was determined by querying for relevant ICD and CPT codes. Multivariate logistic regression adjusting for age, gender, and Charlson Comorbidity Index was used to calculate ORs of complications among outpatients relative to inpatients undergoing ACDF.
RESULTS:
Cohorts of 1,215 patients who underwent outpatient ACDF and 10,964 patients who underwent inpatient ACDF were identified. The median age was in the 65–69 age group for both cohorts. The annual relative incidence of outpatient ACDF increased from 0.11 in 2011 to 0.22 in 2016 (R2=0.82, p=.04). Adjusting for age, gender, and comorbidities, patients undergoing outpatient ACDF were more likely to undergo revision surgery for posterior fusion at both 6 months (OR 1.58, confidence interval [CI] 1.27–1.96, p<.001) and 1 year (OR 1.79, CI 1.51–2.13, p<.001) postoperatively. Outpatient ACDF was also associated with a higher likelihood of revision anterior fusion at 1 year postoperatively (OR 1.46, CI 1.26–1.70, p<.001). Among medical complications, postoperative acute renal failure was more frequently associated with outpatient ACDF than inpatient ACDF (OR 1.25, CI 1.06–1.49, p=.010). Adjusted rates of all other queried surgical and medical complications were comparable.
CONCLUSIONS:
Outpatient ACDF is increasing in frequency nationwide over the past several years. Nationwide data demonstrate a greater risk of perioperative surgical complications, including revision anterior and posterior fusion, as well as a higher risk of postoperative acute renal failure. Candidates for outpatient ACDF should be counseled and carefully selected to reduce these risks.
Keywords: Ambulatory, Anterior cervical discectomy fusion, Complications, Outpatient, Outpatient spine surgery, Reoperation, Revision surgery
Introduction
With the rising cost of health care in the United States, interest has developed in outpatient spine surgery as a mechanism for cost reduction on a population level [1]. This proposed strategy involves transitioning traditionally inpatient procedures to an ambulatory setting in appropriately selected patients to avoid costs associated with a standard postoperative hospital stay. Anterior cervical discectomy and fusion (ACDF), which has seen a significant decrease in hospital length of stay and complication rates, has become an increasingly attractive option to be performed on an outpatient basis [2]. At present, length of stay following ACDF averages under 2 days nationwide, with greater than 80% of patients being discharged within that time frame [3,4]. To this end, multiple studies published in recent years have demonstrated that ACDF is increasingly performed as an outpatient procedure with discharge within ≤24 hours [2,5–11].
Despite its potential for cost savings and perceived safety, outpatient ACDF is still relatively uncommon, with evidence on safety and outcomes limited to a few reports. Reports of outpatient ACDF date back to 2005 and were primarily in the form of case series from single, high-volume institutions [2,7,9,12,13]. These studies reported successful outcomes but are limited by comparatively small samples sizes, short-term follow-up and outcome measures, and significant practitioner and patient selection bias. More recently, data derived from multi-institutional database sources have emerged, including analysis of the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database [6,8,14] and other regional surgical registry databases [15]. These data consistently suggest that outpatient ACDF is associated with equivalent or favorable short-term complication and hospital readmission rates, with significantly lower payor costs when compared with traditional inpatient ACDF [16]. Typically, patients undergoing outpatient ACDF are ideal surgical candidates with little to no medical comorbidities, thereby reducing the perioperative risk of the surgery in the outpatient setting.
The purpose of the present study was to use a large multi-institutional insurance record database to investigate national trends in outpatient one- to two-level ACDF and to determine the frequency and risk of perioperative medical and long-term surgical complications requiring reoperation relative to inpatient ACDF. Our initial hypothesis was that the incidence of outpatient ACDF has increased over the past several years and that the perioperative complication rate of outpatient and inpatient ACDFs would be comparable.
Materials and methods
A retrospective review of the PearlDiver Patient Record Database (Colorado Springs, CO, USA) was conducted. This commercially available database consists of 20 million patient records from the Humana (Louisville, KY, USA) nationwide health insurance provider. Clinical diagnoses can be queried by using patient billing codes, including those classified by the International Classification of Diseases (ICD) and Current Procedural Terminology (CPT).
Patients undergoing ACDF were identified by querying for patients undergoing one- to two-level ACDF (CPT-22551 and ICD-9-816.2) as either outpatients or inpatients using service location modifiers “21” (inpatient) and “22” (outpatient), respectively. The service location modifier 22 represents discharge occurring from either a hospital or ambulatory surgery setting without an associated inpatient hospital admission and absolute length of stay less than 24 hours. Patient records were available for cases performed from 2011 to 2016, and the demographic data for aggregate records included the patient age (reported as 5-year ranges), gender, geographic location, year of procedure, and Charlson Comorbidity Index (CCI). The CCI is a well-validated prospective tool to determine 1-year mortality based on 22 medical conditions [17]. Inferential statistics comparing the baseline age, gender, and regional distributions of the outpatient and inpatient cohorts was performed using chi-square analysis. A two-tailed Student t test was used to compare the baseline CCI of the two cohorts. A linear regression model was used to determine the R2 coefficient to ascertain the trends for the annual incidence of procedures across the study period. Statistical significance was defined as p<.05.
The aforementioned cohorts were queried to identify patients who had a series of postoperative surgical and medical complications based on CPT and International Classification of Diseases, Ninth Revision (ICD-9), codes, respectively. Surgical complications (Table 1) included hardware removal, surgical site infection (requiring irrigation and debridement, explantation of prosthesis, or evacuation), conversion to posterior fusion, revision or extension of anterior fusion, decompressive laminectomy, dural tear, and neurologic deficit at both 6 months and 1 year following the primary index ACDF. Medical complication categories (Supplementary Table S1) included deep vein thrombosis and pulmonary embolism within 60 days; pneumonia, acute renal failure, and respiratory failure within 14 days; and acute myocardial infarction and cerebrovascular accident within 30 days. Using the PearlDiver statistical analysis package, multivariate logistic regression with patient age, gender, and CCI as covariates was performed to calculate adjusted odds ratios (ORs) for each complication category, with outpatient ACDF treated as the exposed group.
Table 1.
List of queried surgical complications following anterior cervical discectomy and fusion*
| Complication category | Code | Code description |
|---|---|---|
| Removal of hardware | CPT-22855 | Removal of anterior instrumentation |
| I&D, explantation, or evacuation | CPT-22010 | Incision and drainage, open, of deep abscess (subfascial), posterior spine; cervical, thoracic, or cervicothoracic |
| CPT-22830 | Exploration of spinal fusion | |
| CPT-63265 | Laminectomy for excision or evacuation of intraspinal lesion other than neoplasm, extradural; cervical | |
| Posterior fusion | CPT-22600 | Arthrodesis, posterior or posterolateral technique, single level; cervical below C2 segment |
| CPT-22614 | Arthrodesis, posterior or posterolateral technique, single level; thoracic (with lateral transverse technique, when performed) | |
| CPT-22842 | Posterior segmental instrumentation (eg, pedicle fixation, dual rods with multiple hooks and sublaminar wires); three to six vertebral segments (list separately in addition to code for primary procedure) | |
| Anterior revision or extension | CPT-22551 | Arthrodesis, anterior interbody, including disc space preparation, discectomy, osteophytectomy, and decompression of spinal cord and nerve roots; cervical below C2 |
| CPT-22552 | Arthrodesis, anterior interbody, including disc space preparation, discectomy, osteophytectomy, and decompression of spinal cord or nerve roots; cervical below C2, each additional interspace | |
| CPT-22554 | Arthrodesis, anterior interbody technique, including minimal discectomy to prepare interspace (other than for decompression); cervical below C2 | |
| Decompressive laminectomy | CPT-63045 | Laminectomy, facetectomy, and foraminotomy (unilateral or bilateral with decompression of spinal cord, cauda equina, and nerve roots [eg, spinal or lateral recess stenosis]), single vertebral segment; cervical |
| CPT-63048 | Laminectomy, facetectomy, and foraminotomy (unilateral or bilateral with decompression of spinal cord, cauda equina, and nerve roots [eg, spinal or lateral recess stenosis]), single vertebral segment; each additional segment, cervical, thoracic, or lumbar | |
| Dural tear | CPT-63707 | Repair of dural or cerebrospinal fluid leak, not requiring laminectomy |
| CPT-63709 | Repair of dural or cerebrospinal fluid leak or pseudomeningocele, with laminectomy | |
| CPT-63710 | Dural graft, spinal | |
| Neurologic deficit | ICD-9-344† | Other paralytic syndromes |
I&D, irrigation and debridement; ICD, International Classification of Diseases; CPT, Current Procedural Terminology.
Excludes cases with concomitant codes for I&D and explantation of prosthesis.
Includes all ICD subcodes.
Results
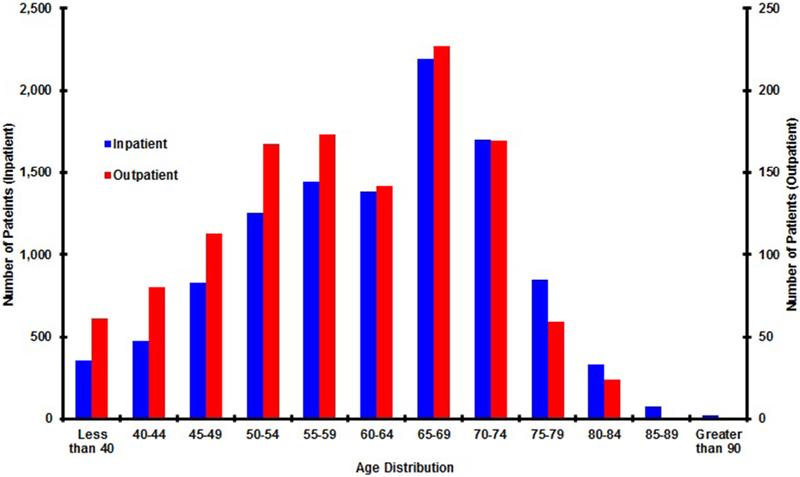
A total of 1,215 patients who underwent outpatient one- to two-level ACDF and 10,964 patients who underwent inpatient one- to two-level ACDF were identified in the Humana database from 2011 to 2016 (Table 2). Across the study period, the overall incidence of outpatient ACDF was 2.8 cases per 100,000 Humana-insured patients compared with 25.8 per 100,000 Humana-insured patients for inpatient ACDF. The age distribution was younger for outpatient undergoing outpatient ACDF when compared with inpatients (p<.001) (Figure). For both cohorts, the median age was in the 65–69 age group, and the mode age group was 60–64. The relative ratio of outpatient to inpatient ACDF decreased with increased patient age (R2=0.93, p<.001). Women comprised 50.5% of outpatient ACDF and 52.0% of inpatient ACDF patients identified (p=.132). The incidence of outpatient ACDF was not equivalent between geographic regions (p<.001), with the Midwest region having the highest incidence of outpatient ACDF (5.0 cases per 100,000). The mean CCIs of outpatients and inpatients undergoing ACDF were 1.74±2.55 and 2.81±3.19, respectively (p<.001). The annual relative incidence of outpatient ACDF increased from 0.11 in 2011 to 0.22 in 2016 (R2=0.82, p=.04).
Table 2.
Age, gender, regional, and annual case volume distribution of study cohorts†
| Outpatient ACDF (N=1,215) |
Inpatient ACDF (N=10,964) |
Relative ratio of outpatient ACDF |
|||
|---|---|---|---|---|---|
| n | Incidence (per 100,000)* |
n | Incidence (per 100,000)* |
||
| Age | |||||
| Less than 40 | 61 | 0.2 | 355 | 3.0 | 0.17 |
| 40–44 | 80 | 1.8 | 475 | 20.1 | 0.17 |
| 45–49 | 113 | 2.8 | 825 | 28.7 | 0.14 |
| 50–54 | 167 | 3.2 | 1,255 | 36.0 | 0.13 |
| 55–59 | 173 | 4.3 | 1,446 | 37.3 | 0.12 |
| 60–64 | 142 | 4.3 | 1,382 | 34.2 | 0.10 |
| 65–69 | 227 | 1.0 | 2,188 | 16.1 | 0.10 |
| 70–74 | 169 | 1.9 | 1,698 | 14.2 | 0.10 |
| 75–79 | 59 | 1.9 | 844 | 9.4 | 0.07 |
| 80–84 | 24 | 1.0 | 329 | 5.4 | 0.07 |
| 85–89 | 0 | 0 | 73 | 3.1 | 0 |
| 90+ | 0 | 0 | 22 | 0.5 | 0 |
| Gender | |||||
| Male | 601 | 1.4 | 5,265 | 12.0 | 0.11 |
| Female | 614 | 1.9 | 5,699 | 17.7 | 0.11 |
| Geographic region | |||||
| Midwest | 264 | 5.0 | 2,182 | 41.5 | 0.12 |
| Northeast | 16 | 0.1 | 188 | 1.0 | 0.09 |
| South | 856 | 2.1 | 7,608 | 18.6 | 0.11 |
| West | 79 | 0.8 | 986 | 9.5 | 0.08 |
| Case year | |||||
| 2011 | 168 | 2.6 | 1,523 | 23.3 | 0.11 |
| 2012 | 207 | 2.8 | 1,966 | 27.3 | 0.11 |
| 2013 | 276 | 3.4 | 2,347 | 29.7 | 0.12 |
| 2014 | 338 | 3.4 | 2,727 | 28.3 | 0.12 |
| 2015 | 235 | 2.0 | 2,348 | 20.5 | 0.10 |
| 2016 | 12 | N/A | 54 | N/A | 0.22 |
N/A, not applicable; ACDF, anterior cervical discectomy and fusion.
Incidence per 100,000 Humana-insured patients.
N/A where complete incidence data not available for 2016 calendar year at the time of query.
Figure.
Age distributions of Humana-insured patients undergoing anterior cervical discectomy and fusion as either an outpatient (red) or inpatient (blue). The age distributions between the two groups are statistically comparable. For both cohorts, the median age was in the 65–69 age group and the mode age group was 60–64.
Among surgical complications, the most common complications requiring reoperation at 1 year were conversion to posterior fusion (5.51% outpatient, 4.11% inpatient), revision or extension of anterior fusion (3.95% outpatient, 3.11% inpatient), and decompressive laminectomy (3.54% outpatient, 3.66% inpatient) (Table 3). All other surgical complications occurred in fewer than 1% of patients undergoing ACDF in the outpatient and inpatient settings. When adjusting for patient age, gender, and CCI, patients undergoing outpatient ACDF had a greater likelihood of posterior fusion (OR 1.79, CI 1.51–2.13, p<.001) and anterior revision or extension (OR 1.46, CI 1.26–1.70, p<.001) at 1 year; outpatient ACDF was also associated with an increased likelihood of posterior fusion (OR 1.58, CI 1.27–1.96, p<.001) at 6 months. Among postoperative medical complications queried, acute renal failure within 14 days (OR 1.25, CI 1.06–1.49, p=.010) was more frequently associated with outpatient ACDF. The incidence of all other queried postoperative complications was comparable between the two cohorts (Table 3).
Table 3.
Frequency and adjusted OR of surgical and medical complications following outpatient ACDF
| Outpatient ACDF (N=1,215) |
Inpatient ACDF (N=10,964) |
Adjusted OR (for outpatient ACDF)† |
p-Value | ||||
|---|---|---|---|---|---|---|---|
| n | Frequency (%) |
n | Frequency (%) |
||||
| Surgical complications | |||||||
| Removal of hardware (at 6 mo) | * | * | 56 | 0.51 | |||
| Removal of hardware (at 1 y) | * | * | 74 | 0.67 | |||
| I&D, exploration, or evacuation (at 6 mo) | * | * | 63 | 0.57 | |||
| I&D, exploration, or evacuation (at 1 y) | * | * | 84 | 0.77 | |||
| Posterior fusion (at 6 mo) | 40 | 3.29 | 287 | 2.62 | 1.58 (1.27–1.96) | <.001 | |
| Posterior fusion (at 1 y) | 67 | 5.51 | 451 | 4.11 | 1.79 (1.51–2.13) | <.001 | |
| Anterior revision or extension (at 6 mo) | 33 | 2.72 | 290 | 2.65 | 1.03 (0.85–1.23) | .784 | |
| Anterior revision or extension (at 1 y) | 48 | 3.95 | 341 | 3.11 | 1.46(1.26–1.70) | <.001 | |
| Decompressive laminectomy (at 6 mo) | 26 | 2.14 | 264 | 2.41 | 1.10(0.83–1.44) | .508 | |
| Decompressive laminectomy (at 1 y) | 43 | 3.54 | 401 | 3.66 | 1.22(0.98–1.52) | .071 | |
| Dural tear (at 6 mo) | * | * | 11 | 0.10 | |||
| Dural tear (at 1 y) | * | * | 21 | 0.19 | |||
| Neurologic injury | * | * | 178 | 1.62 | |||
| Medical complications | |||||||
| DVT | * | * | 65 | 0.59 | |||
| PE | * | * | 85 | 0.78 | |||
| Pneumonia | * | * | * | * | |||
| Acute renal failure | 15 | 1.23 | 164 | 1.50 | 1.25 (1.06–1.49) | .010 | |
| Respiratory failure | 16 | 1.32 | 313 | 2.85 | 1.01 (0.84–1.22) | .883 | |
| MI | * | * | 60 | 0.55 | |||
| Cerebrovascular accident | 12 | 0.99 | 132 | 1.20 | 0.94(0.76–1.18) | .608 | |
OR, odds ratio; ACDF, anterior cervical discectomy and fusion; I&D, irrigation and debridement; DVT, deep vein thrombosis; PE, pulmonary embolism; MI, myocardial infarction.
Indicates complications where <11 cases were reported, corresponding to a frequency of <0.9%; OR cannot be defined for these instances.
Adjusted OR derived from multivariate logistic regression with patient age, gender, and Charlson Comorbidity Index used as covariates.
Discussion
Anterior cervical discectomy and fusion has increased significantly in volume over the past several decades as a popular and successful surgical management option for various cervical pathologies, including cervical radiculopathy and cervical spondylotic myelopathy [18]. With the increasing emphasis on value-based care and cost efficiency in orthopedics, surgeons and health-care administrators are showing increasing interest in outpatient spine surgery as a possible strategy for minimizing costs and the burden associated with lengthy postoperative hospital courses and increasing satisfaction in an appropriately selected patient population. Because of its relatively recent emergence in the orthopedic literature, information on national trends and complication rates in outpatient ACDF is limited, and its feasibility in the community outside of high-volume centers is poorly understood [2,7,9,19]. Much of the current scientific literature regarding outpatient ACDF is composed of smaller studies. Because the incidence of ACDF-associated complications is low, the generalizability of these smaller studies is limited. To our knowledge, the present study reports the largest cohort of patients across multiple institutions evaluating the trends and postoperative complications associated with ACDF performed in the outpatient setting.
Demographically, we found the age distribution of Humana-insured patients undergoing outpatient ACDF to be younger when compared with that of the inpatient comparison cohort. The result that outpatient ACDF patients were younger than their inpatient counterparts is not unexpected, given that age is a known independent risk factor for perioperative complications in spine surgery [20]. The present study also found that the relative incidence of outpatient ACDF varied by geographic region, with the incidence significantly higher in the South and Midwest regions than in the Northeast and West regions. We anticipate that this marked regional difference will narrow with gradual adoption of outpatient spine surgery as a practice more pervasively across the United States.
We also found that the incidence of outpatient ACDF cases performed has increased over the study period, with a twofold increase in relative frequency from 2007 to 2016. The earliest published case series on outpatient ACDF dates back to 2005, wherein Stieber et al. reported one- to two-level ACDF with plate fixation in a series of 30 patients at an ambulatory surgery center [2]. Stieber et al. reported a lower complication rate compared with controls, which they attributed to the inherent selection bias of their outpatient cohort. Subsequently, multiple case series have been reported on ACDF with ≤24 hours of postoperative stay with equivalent or favorable outcomes and short-term complication profiles [2,7,9,10,19,21]. More recently, multi-institutional data from statewide registries and the NSQIP database have shown similar results of outpatient ACDF as non-inferior to inpatient ACDF in carefully selected patient populations.
The present study also found that after adjusting for baseline demographics and comorbidities, ACDF performed in the outpatient setting was associated with higher odds of (1) anterior revision or extension of fusion (OR 1.46 at 1 year); (2) conversion to posterior fusion (OR 1.58 at 6 months, OR 1.79 at 1 year); and (3) acute renal failure within 14 days (OR 1.25). This finding disproved our initial hypothesis that complication rates would be equivalent between the two cohorts. To our knowledge, this is the first report of higher postoperative complication rates in the outpatient ACDF literature. Given the careful selection of patients as candidates for outpatient ACDF who are presumably healthier and more functional at baseline, the increased incidence of surgical complications is a concerning finding. To date, the outpatient spine surgery literature has primarily focused on short-term outcomes and readmission rates. These early reports have demonstrated equivalent or lower rates of 30-day readmission, early reoperation, postoperative anemia, and transfusion, durotomy, nerve injury, respiratory compromise, transient dysphagia, and mortality [2,6,8–10,22]. This equivalency has also held true in recent independently published propensity-adjusted analyses using the NSQIP database by both Khanna et al. [6] and Fu et al. [8].
From these data, the underlying cause of the association between outpatient ACDF and the elevated risk of revision surgery is not readily apparent. We surmise that this finding may be due to higher rates of postoperative pseudarthrosis necessitating repeat instrumentation and revision fusion, although the likely etiology that would explain this difference between outpatients and inpatients is uncertain [23–25]. With greater emphasis to efficiency and the time demands of a high surgical volume at a busy ambulatory surgery center, rigorous attention may not be paid to the finer points of the ACDF procedure, such as complete discectomy and decompression, adequate end plate preparation, and proper instrumentation and fusion techniques. Another potential factor driving this observed difference may be due to external pressures in the ambulatory surgery center setting, wherein shorter operative times and a more maximized use of scheduled operating room time are incentivized because of financial incentives and staff leaving early. In addition, newer standalone ACDF systems allow for significantly reduced surgical times as compared with traditional plate and screw systems, despite reductions in biomechanical stiffness, which may lead to an increased risk of pseudarthrosis [26,27]. Adjacent segment disease may also contribute to these higher rates of revision surgery, which is a well-known long-term complication of the ACDF procedure. Again, it is unclear precisely why revision surgery caused by adjacent segment disease would occur more commonly in the outpatient setting. Although the present study design exclusively analyzed one- to two-level fusions in both cohorts, it is conceivable that surgeons elected to perform one- to two-level fusions on an outpatient basis in patients who may have milder disease involving a third adjacent segment. Here, the surgeon may be more comfortable doing a three-level ACDF in the inpatient setting, whereas he or she may be more comfortable taking the one- to two-level ACDF in the ambulatory setting. This finding may explain the increased rate of revision anterior fusion among outpatients observed in the present study.
With regard to medical complications, the slightly higher propensity-adjusted OR of acute renal failure (OR 1.25) may be secondary to inadequate postoperative hydration secondary to early discharge from the monitored hospital setting. Inpatients are more likely to undergo postoperative intravenous fluid resuscitation and laboratory monitoring, which may ameliorate this risk to some extent. We note that the rates of acute renal failure found in the present study are similar to rates reported for other ambulatory orthopedic surgical procedures, suggesting that these observed differences may not be specific to ACDF in particular [28]. Given the small difference in absolute risk between the two cohorts, it is also possible that this finding may be statistically but not clinically significant. We also note that there was no significant difference in the incidence of postoperative hematoma or respiratory failure from airway compromise. These are important postoperative complications following ACDF that may potential affect the surgeon’s decision on outpatient discharge versus postoperative hospital stay.
We also acknowledge the possibility that provider selection may account for the higher complication rates observed in the present study, wherein individual high-volume centers and NSQIP-participating sites that have reported equivalent outcomes may be better equipped to perform ACDF on an outpatient basis than the non-selected population of providers that is represented by the Humana database. Further study through prospective, large-scale clinical trials is warranted before ubiquitous adoption of outpatient spine surgery as a standard of care in the appropriate patient population. As reported by a recently published Delphi protocol expert panel [5], consensus practice guidelines and evidence-based protocols are lacking and will be paramount to establishing ambulatory spine surgery as the standard of care in the appropriate provider and patient population. Widespread implementation of safe and efficient patient selection and perioperative decision making for outpatient spine surgery is expected to help achieve significant cost savings for the healthcare system [16].
Although the findings in the present study are unique, such a study design has several limitations. First, the PearlDiver database has limited granularity and provides aggregate rather than individual patient data for privacy concerns. Because the database is searched by CPT and ICD codes, the available data on baseline health characteristics and complications are less comprehensive than are available through conventional chart review. Although this limitation is partially mitigated by multivariate logistic regression controlling for CCI, this database design remains susceptible to source data biases and errors from miscoding. Second, this design also limits analysis of early complications, including emergency department presentations, hospitalizations, and readmission for postoperative anemia or pain control, which cannot be adequately captured using CPT and ICD codes. These events could significantly countermand cost savings associated with early discharge. Here, the use of billing service location modifiers as the primary query agent predisposes our data to ambiguity, wherein it is conceivable that, because of variations or errors in coding practices, patients who undergo “outpatient” ACDF at an ambulatory surgery center may be subsequently admitted to a hospital building under a separate inpatient encounter. Finally, the database provides no information on functional or patient-reported outcomes, which was beyond the scope and intent of the study but should be incorporated to determine the relative effectiveness of outpatient ACDF.
Conclusions
The present study found that outpatient ACDF is increasing in frequency nationwide, likely because of changes in health-care delivery and greater attention to cost reduction and improved efficiency. Data collected from a national private insurance database demonstrate a greater risk of perioperative surgical complications, including revision anterior and posterior fusion, as well as a higher risk of postoperative acute renal failure. Candidates for outpatient ACDF should be counseled and carefully selected to reduce these risks. Surgeons and health-care systems that wish to implement outpatient spine surgery should consider complication rates and adapt rigorous and comprehensive clinical pathways to carefully select and treat patients.
Supplementary Material
Acknowledgment
The authors thank the UCLA Statistical Consulting Group through the Institute for Digital Research and Education for assistance with the statistical analysis.
Footnotes
FDA device/drug status: Not applicable.
Author disclosures: AA: Nothing to disclose. CW: Nothing to disclose. HYP: Nothing to disclose. GWB: Nothing to disclose. ZB: Consulting: Xenco Medical (B), AO Spine (B), outside the submitted work. JCW: Royalties: Aesculap (B), Biomet (G), Amedica (C), Seaspine (D), Synthes (C); Stock Ownership: Fziomed (<1%); Private Investments: Promethean Spine (1 share, 1%, $10,000 investment, less than 1% of entity), Paradigm Spine (<1% of entity), Benevenue (<1% of entity), NexGen (<1% of entity), Vertiflex (<1% of entity), Electrocore (<1% of entity), Surgitech (<1% of entity), Expanding Orthopaedics (<1% of entity), Osprey (<1% of entity), Bone Biologics (<1% of entity), Curative Biosciences (<1% of entity), PearlDiver (<1% of entity); Board of Directors: North American Spine Society (non-financial, reimbursement for travel for board meetings, courses, etc.), North American Spine Foundation (non-financial), Cervical Spine Research Society (non-financial, reimbursement for travel for board meetings), AO Spine and AO Foundation (both, E, honorariums for board position); Fellowship Support: AO Foundation (E, Paid directly to institution); outside the submitted work. ANS: Royalties: Seaspine (C); Research Support (Investigator Salary, Staff and Materials) (D, Paid directly to institution), outside the submitted work. DYP: Consulting: Nuvasive (B), Globus (B), Depuy Synthes (A); outside the submitted work.
The disclosure key can be found on the Table of Contents and at www.TheSpineJournalOnline.com.
Supplementary material
Supplementary material related to this article can be found at https://doi.org/10.1016/j.spinee.2017.11.012.
References
- [1].McClelland S, Oren JH, Protopsaltis TS, Passias PG. Outpatient anterior cervical discectomy and fusion: a meta-analysis. J Clin Neurosci 2016;34:166–8. [DOI] [PubMed] [Google Scholar]
- [2].Stieber JR, Brown K, Donald GD, Cohen JD. Anterior cervical decompression and fusion with plate fixation as an outpatient procedure. Spine J 2005;5:503–7. [DOI] [PubMed] [Google Scholar]
- [3].Basques BA, Bohl DD, Golinvaux NS, Gruskay JA, Grauer JN. Preoperative factors affecting length of stay after elective anterior cervical discectomy and fusion with and without corpectomy. Spine 2014;39:939–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gruskay JA, Fu M, Basques B, Bohl DD, Buerba R, Webb ML, et al. Factors affecting length of stay and complications following elective anterior cervical discectomy and fusion. J Spinal Disord Tech 2014;29:1. [DOI] [PubMed] [Google Scholar]
- [5].Mohandas A, Summa C, Worthington WB, Lerner J, Foley KT, Bohinski RJ, et al. Best practices for outpatient anterior cervical surgery: results from a Delphi panel. Spine 2017;42:E648–59. [DOI] [PubMed] [Google Scholar]
- [6].Khanna R, Kim RB, Lam SK, Cybulski GR, Smith ZA, Dahdaleh NS. Comparing short-term complications of inpatient versus outpatient single-level anterior cervical discectomy and fusion: an analysis of 6940 patients using the ACS-NSQIP database. Clin Spine Surg 2017;doi:10.1097/BSD.0000000000000499. [DOI] [PubMed] [Google Scholar]
- [7].Erickson M, Fites BS, Thieken MT, McGee AW. Outpatient anterior cervical discectomy and fusion. Am J Orthop (Belle Mead NJ) 2007;36:429–32. [PubMed] [Google Scholar]
- [8].Fu MC, Gruskay JA, Samuel AM, Sheha ED, Derman PB, Iyer S, et al. Outpatient anterior cervical discectomy and fusion is associated with fewer short-term complications in one-and two-level cases: a propensity-adjusted analysis. Spine 2016;42:1044–9. [DOI] [PubMed] [Google Scholar]
- [9].Villavicencio AT, Pushchak E, Burneikiene S, Thramann JJ. The safety of instrumented outpatient anterior cervical discectomy and fusion. Spine J 2007;7:148–53. [DOI] [PubMed] [Google Scholar]
- [10].Tally WC, Tarabadkar S, Kovalenko BV. Safety and feasibility of outpatient ACDF in an ambulatory setting: a retrospective chart review. Int J Spine Surg 2013;7:e84–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Chin KR, Pencle FJR, Seale JA, Pencle FK. Clinical outcomes of outpatient cervical total disc replacement compared with outpatient anterior cervical discectomy and fusion. Spine 2017;42:E567–74. [DOI] [PubMed] [Google Scholar]
- [12].Lied B, Rønning PA, Halvorsen CM, Ekseth K, Helseth E. Outpatient anterior cervical discectomy and fusion for cervical disk disease: a prospective consecutive series of 96 patients. Acta Neurol Scand 2013;127:31–7. [DOI] [PubMed] [Google Scholar]
- [13].Ban D, Liu Y, Cao T, Feng S. Safety of outpatient anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur J Med Res 2016;21:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Somani S, Di Capua J, Kim JS, Kothari P, Lee NJ, Leven DM, et al. Comparing national inpatient sample and National Surgical Quality Improvement Program: an independent risk factor analysis for risk stratification in anterior cervical discectomy and fusion. Spine 2017;42:565–72. [DOI] [PubMed] [Google Scholar]
- [15].McClelland S, Passias PG, Errico TJ, Bess RS, Protopsaltis TS. Outpatient anterior cervical discectomy and fusion: an analysis of readmissions from the New Jersey State Ambulatory Services Database. Int J Spine Surg 2017;11:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Purger DA, Pendharkar AV, Ho AL, Sussman ES, Yang L, Desai M, et al. Outpatient vs inpatient anterior cervical discectomy and fusion: a population-level analysis of outcomes and cost. Neurosurgery 2017;doi:10.1093/neuros/nyx215. [DOI] [PubMed] [Google Scholar]
- [17].Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373–83. [DOI] [PubMed] [Google Scholar]
- [18].Passias PG, Marascalchi BJ, Boniello AJ, Yang S, Bianco K, Jalai CM, et al. Cervical spondylotic myelopathy: National trends in the treatment and peri-operative outcomes over 10 years. J Clin Neurosci 2017;42:75–80. [DOI] [PubMed] [Google Scholar]
- [19].Liu JT, Briner RP, Friedman JA. Comparison of inpatient vs. outpatient anterior cervical discectomy and fusion: a retrospective case series. BMC Surg 2009;9:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Buerba RA, Giles E, Webb ML, Fu MC, Gvozdyev B, Grauer JN. Increased risk of complications after anterior cervical discectomy and fusion in the elderly. Spine 2014;39:2062–9. [DOI] [PubMed] [Google Scholar]
- [21].Trahan J, Abramova MV, Richter EO, Steck JC. Feasibility of anterior cervical discectomy and fusion as an outpatient procedure. World Neurosurg 2011;75:145–8 [discussion 43-4]. [DOI] [PubMed] [Google Scholar]
- [22].McGirt MJ, Godil SS, Asher AL, Parker SL, Devin CJ. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus 2015;39:E9. [DOI] [PubMed] [Google Scholar]
- [23].Lee D-H, Cho JH, Hwang CJ, Lee CS, Cho SK, Kim C, et al. What is the fate of pseudarthrosis detected 1 year after anterior cervical discectomy and fusion? Spine 2017;doi:10.1097/BRS.0000000000002077. [DOI] [PubMed] [Google Scholar]
- [24].van Eck CF, Regan C, Donaldson WF, Kang JD, Lee JY. The revision rate and occurrence of adjacent segment disease after anterior cervical discectomy and fusion. Spine 2014;39:2143–7. [DOI] [PubMed] [Google Scholar]
- [25].Elder BD, Sankey EW, Theodros D, Bydon M, Rory Goodwin C, Lo S-F, et al. Successful anterior fusion following posterior cervical fusion for revision of anterior cervical discectomy and fusion pseudarthrosis. J Clin Neurosci 2016;24:57–62. [DOI] [PubMed] [Google Scholar]
- [26].Scholz M, Schleicher P, Pabst S, Kandziora F. A zero-profile anchored spacer in multilevel cervical anterior interbody fusion: biomechanical comparison to established fixation techniques. Spine 2015;40:E375–80. [DOI] [PubMed] [Google Scholar]
- [27].Shimamoto N, Cunningham BW, Dmitriev AE, Minami A, McAfee PC. Biomechanical evaluation of stand-alone interbody fusion cages in the cervical spine. Spine 2001;26:E432–6. [DOI] [PubMed] [Google Scholar]
- [28].Noureldin M, Habermann EB, Ubl DS, Kakar S. Unplanned readmissions following outpatient hand and elbow surgery. J Bone Jt Surg 2017;99:541–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.