Abstract
Introduction
Waterpipe smoking continues to pose significant challenges to tobacco control efforts and many adolescent waterpipe smokers experience symptoms of nicotine dependence (ND). This study examined the predictors of progression of ND symptoms in adolescent waterpipe smokers.
Methods
We assembled a cohort of Lebanese adolescents enrolled in 8th and 9th grades at baseline, and surveyed them every 6 months over the next 24 months. Progression of ND symptoms was defined as an increase over time in the number of items endorsed on the Hooked on Nicotine Checklist (HONC). Predictors included individual (e.g., psychological factors, attitudes towards waterpipe, school performance, physical activity), and socio-environmental (e.g., smoking among parents, siblings, and close friends; the café environment) attributes.
Results
Among 264 adolescent waterpipe smokers (baseline mean age=14.6 years, 50.4% females), 105 (39.7%) progressed on ND symptoms during follow up. Predictors of progression were higher baseline stress (OR=1.11, 95% CI: 1.03–1.19), and higher self-esteem (OR=1.14, 95% CI: 1.05–1.24). Reporting difficulty refraining from smoking waterpipe while in a restaurant was the strongest predictor of progression (OR=4.04, 95% CI: 1.44–11.34). Having a mother with ≥12 years of education protected against progression of ND (OR=0.46, 95% CI: 0.21–0.99).
Conclusions
A significant proportion of adolescent waterpipe smokers progressed on ND. Venue-based policies such as limiting youth access to waterpipe cafés is warranted.
Keywords: Waterpipe café, Lebanon, HONC, Progression, Nicotine Dependence
1. INTRODUCTION
Waterpipe (a.k.a. narghile, shisha, hookah) has emerged as a new component of a global tobacco epidemic, centered mainly among adolescents and young adults.1 Although waterpipe smoking commonly is perceived as a safer alternative to cigarettes,1 growing evidence shows that waterpipe smokers are exposed to significant amounts of harmful chemicals such as carbon monoxide;2 benzene;3 tobacco-specific nitrosamines;4 and nicotine, a dependence-producing stimulant drug.5, 6
The rise in waterpipe use among youth worldwide has been linked to several individual and socio-environmental factors. For example, novelty-seeking youth are commonly attracted to the glamorous design of waterpipe and the flavored tobacco (known as Maassel) commonly used in waterpipe.7 Waterpipe smoking, moreover, has unique contextual factors that shape the waterpipe experience. Smoking in groups of friends and family members and sharing the same waterpipe are salient features of waterpipe use.1 These unique factors enhance waterpipe’s appeal to young people as it provides opportunities for socialization, a source of relaxation, and an affordable and pleasurable novelty.1, 7, 8 In contrast to the stigma associated with smoking cigarettes,9, 10 waterpipe is socially acceptable in many Middle Eastern countries, and the majority of adolescents first exposure to waterpipe is at a friends’ house,7 with a family member,9 or at a waterpipe café.7 - 10 The café environment in particular represents an important environmental factor that may influence waterpipe smoking behaviors. For example, among a sample of young adults in the US (N=201, 86% 18–24 years of age), 50% reported a café as the place of first waterpipe use,11 while in a different study among US young adults (N=143, 85% 18–25 years of age) 30% reported they usually smoke it at a café.12 Attending a waterpipe café or restaurant serving a waterpipe was the strongest predictor of current (past 30 days) waterpipe use among a sample of US adolescents (N= 951, mean age= 17.6 years).13 Collectively, individual and socio-environmental factors unique to waterpipe can influence its initiation and current use.
By influencing patterns, many of these individual and socio-environmental factors can predict the appearance of ND symptoms among waterpipe smokers. Reciprocally, the appearance and severity of ND symptoms can shape some of these factors, e.g., among young people, frequent users of waterpipe – a proxy for ND – tend to smoke it in groups of friends (compared to smoking alone).12 Moreover, these unique socio-environmental factors can enhance the positive reinforcement value of waterpipe use and promote the progression of ND, and can be critical components for any efforts to reduce waterpipe smoking among youth. Therefore, examining the role of these factors in enhancing and predicting ND progression in waterpipe smokers is essential to assess the importance of these unique individual and socio-environmental factors, to inform policies and regulations specific to waterpipe, and for the design of targeted interventions.
Although waterpipe smoking is generally perceived as less addictive than cigarettes,1 there is a growing evidence from around the world that many young waterpipe smokers experience symptoms of ND, similar to cigarette smokers. Our cohort study investigating ND in adolescents (Waterpipe Dependence in Lebanese Youth “WDLY” study) indicated that 71.2% of Lebanese waterpipe smokers in our sample (mean age at baseline=14 years) compared with 75% of cigarette smokers, experience ND symptoms within a short time period after experimenting with tobacco product.14 Six other studies, outside of Lebanon (2 in the UK15, 16; 2 in Malaysia17, 18, 1 in Jordan,19 and 1 in the US20) also have assessed ND symptoms in young waterpipe smokers. One study among university students in the UK (mean age=20 years) reported that 33.3% of regular waterpipe smokers experienced cravings15, and the other study among patrons of waterpipe-serving restaurants in the UK found that 47% of the sample were dependent on waterpipe.16 In the two studies from Malaysia, both among young adults (18–30 year-olds), one reported a comparable percentages of some ND symptoms between waterpipe and cigarette smokers,17 while the other found that 12.7% of participants said they were highly dependent on waterpipe.18 The study from Jordan among college students (18–23 year-olds) reported that a third of participants were highly dependent on waterpipe,19 while the study from the US among young (18–30 year-olds) waterpipe smokers found that 48.1% of participants endorsed at least 1 symptom of ND.20 Difference across these studies in ND may be due to the use of different ND tools. Overall, however, these studies indicate that dependence among young waterpipe smokers may be a common and global phenomenon.
Limited analysis from the baseline data of the WDLY study, showed that cues such as seeing or smelling waterpipe, and the café environment triggered a craving to smoke waterpipe in adolescents.14 Using follow up data of WDLY over 24 months, we want to extend those initial observations and examine the role of individual and socio-environmental factors in predicting the progression of ND in adolescent waterpipe smokers. This study will provide the first insights into the predictors of ND progression in adolescent waterpipe smokers using longitudinal data. Findings from this longitudinal study will provide the first evidence on the role of factors unique to waterpipe in predicting ND progression in adolescents, and are instrumental for regulatory and intervention purposes. Given the globalization of the waterpipe epidemic, and the similarity of factors contributing to its worldwide spread, findings from this study can inform policies to control waterpipe in countries where waterpipe use is high among youth as in the US and elsewhere.
2. METHODS
2.1. Dataset and participants
WDLY is a longitudinal study of Lebanese adolescents recruited from 8th and 9th grades at baseline (N=498 smokers and nonsmokers, age at baseline=14 years). The main objective of the WDLY study is to describe the early symptoms and trajectories of ND symptoms among adolescent waterpipe smokers. Data on use of different tobacco products, symptoms of ND, individual and socio-environmental factors known to be associated with tobacco initiation and use behaviors or ND were collected by trained interviewers. The institutional review boards of Florida International University and the American University of Beirut approved WDLY. More details on the WDLY study have been published elsewhere.14
This study includes data collected at baseline and at 6 months follow-ups over 24 months (5 interview waves including the baseline). During this period, 49 participants were lost to follow-up due to relocation or leaving school (no evidence of differential missingness in the progression of ND between males and females). This resulted in an overall retention rate of 90.2% over 24 months. Participants were included in this analysis if they were current waterpipe smokers at baseline (smoked at least once in the past 30 days), or initiated waterpipe smoking during follow up and reported waterpipe smoking at least once in the 30 days prior to any subsequent data collection wave.
2.2. Measures
2.2.1. Individual and socio-environmental factors
Individual factors were self-reported at baseline and include age in years, gender, school performance (below, at, or above class average), weekly pocket money allowance, regular physical activity (performing physical activity at least once a week), beliefs and attitudes towards waterpipe smoking, psychological factors, and waterpipe use behaviors. Six psychological factors were assessed: stress (Cronbach’s alpha “α”=0.79), depressive symptoms (α=0.75), novelty seeking (α=0.76), impulsivity (α=0.81), self-esteem (α=0.79), and distractibility (α=0.63).21 Baseline waterpipe use frequency (less than weekly, weekly but not daily, daily), number of waterpipes (i.e., heads smoked) smoked in the past 30 days, and the usual length of a smoking session (< 30 min, 30–60 min, >60 min) were obtained.
Participants were asked about environmental exposure to waterpipe. As in a previous work on adolescents’ exposure to environmental smoking,22, 23 we inquired about waterpipe smoking among parents, siblings, and close friends. A proxy variable of exposure to waterpipe advertisements was assessed by asking participants if they had a favorite waterpipe advertisement (Yes/No).24 To assess environmental factors and cues specific to waterpipe, we used 3 items from the Syrian Center for Tobacco Studies (SCTS-28)14 that assess the effect of the café on waterpipe smoking “It would be very difficult to me to be in a restaurant, and not smoke waterpipe,” waterpipe’s sight and smell as cues for smoking “just the sight or smell of waterpipe is enough to make me want to smoke,” and usual place for smoking waterpipe “I smoke waterpipe usually with friends or in cafés/restaurants” (see Table 2). We chose these 3 items because they inquire about waterpipe characteristics and environmental cues associated with waterpipe smoking and have the potential to influence smoking behaviors and ND in adolescent waterpipe smokers.14 SCTS-28 consists of 28 items that assess subjective experience, attitudes, environmental cues, and symptoms specific to waterpipe use and dependence. SCTS-28 had a good internal consistency of 0.80 in this cohort, and a good convergent construct validity as shown by a strong correlation with the criteria of ND as measured by the WHO’s International Classification of Diseases-10th revision and scores on the Lebanon Waterpipe Dependence Scale-10J.14
Table 2.
Baseline characteristics of adolescent waterpipe smokers who did or did not subseauentlv show a progression on nicotine dependence
| Progressed on nicotine dependence
|
p-value* | ||
|---|---|---|---|
| No (n=159), n (%), mean±SD | Yes (n=105), n (%), mean±SD | ||
|
| |||
| Individual | |||
|
| |||
| Gender | 0.63 | ||
| Male | 77 (48.4) | 54 (51.4) | |
| Female | 82 (51.6) | 51 (48.6) | |
|
| |||
| Weekly allowance (LBP) | 0.85 | ||
| < 10,000 | 21 (13.2) | 12 (11.4) | |
| 10,000–20,000 | 88 (55.3) | 57 (54.3) | |
| > 20,000 | 50 (31.4) | 36 (34.3) | |
|
| |||
| Performing regular physical activity (at least once/week) | 0.69 | ||
| No | 41 (25.9) | 25 (23.8) | |
| Yes | 117 (74.1) | 80 (76.2) | |
|
| |||
| School performance | 0.62 | ||
| Below class average | 19 (11.9) | 14 (13.3) | |
| Class average | 110 (69.2) | 76 (72.4) | |
| Above class average | 30 (18.9) | 15 (14.3) | |
|
| |||
| Spiritual/religious person | 0.49 | ||
| No | 21 (13.2) | 17 (16.2) | |
| Yes | 138 (86.8) | 88 (83.8) | |
|
| |||
| Average time spend during a waterpipe smoking session (min) | 0.59 | ||
| <30 | 83 (52.2) | 54 (51.4) | |
| 30–60 | 61 (38.4) | 37 (35.2) | |
| >60 | 15 (9.4) | 14 (13.3) | |
|
| |||
| Smoking frequency in past 30 days | 0.02 | ||
| Less once a week | 91 (57.2) | 47 (44.8) | |
| At least once a week but not daily | 45 (28.3) | 47 (44.8) | |
| Daily or almost daily | 23 (14.5) | 11 (10.5) | |
|
| |||
| Number of waterpipes smoked in past 30 days | 9.5±21.9 | 7.2±8.6 | 0.06 |
|
| |||
| Waterpipe smokers look more attractive | 0.71 | ||
| Disagree/Don’t know | 121 (76.1) | 82 (78.1) | |
| Agree | 38 (23.9) | 23 (21.9) | |
|
| |||
| Waterpipe smokers have more friends | 0.53 | ||
| Disagree/Don’t know | 103 (64.8) | 64 (61.0) | |
| Agree | 56 (35.2) | 41 (39.0) | |
|
| |||
| Waterpipe smoking makes a person lose weight | 0.49 | ||
| Disagree/Don’t know | 143 (89.9) | 97 (92.4) | |
| Agree | 16 (10.1) | 8 (7.6) | |
|
| |||
| Waterpipe smoking is harmful to health | 0.02 | ||
| Disagree/Don’t know | 8 (5.0) | 0 (0.0) | |
| Agree | 151 (95.0) | 105 (100.0) | |
|
| |||
| Stress | 7.1±6.0 | 9.0±7.1 | 0.02 |
|
| |||
| Depression | 7.1±4.9 | 7.4±4.3 | 0.35 |
|
| |||
| Distractibility | 8.1±4.5 | 8.6±4.8 | 0.39 |
|
| |||
| Novelty seeking | 14.2±7.5 | 15.0±7.3 | 0.32 |
|
| |||
| Impulsivity | 10.8±6.9 | 11.8±6.8 | 0.17 |
|
| |||
| Self-esteem | 17.8±4.3 | 20.2±4.7 | 0.001 |
|
| |||
| Socio-environmental | |||
|
| |||
| School type | 0.63 | ||
| Public | 73 (45.9) | 45 (42.9) | |
| Private | 86 (54.1) | 60 (57.1) | |
|
| |||
| Father’s years of education | 0.74 | ||
| < 12 years of education/Cannot read or write | 115 (72.3) | 74 (70.5) | |
| > 12 years of education | 44 (27.7) | 31 (29.5) | |
|
| |||
| Mother’s years of education | 0.04 | ||
| < 12 years of education/Cannot read or write | 89 (56.0) | 72 (68.6) | |
| > 12 years of education | 70 (44.0) | 33 (31.4) | |
|
| |||
| Waterpipe smoking by parents | 0.94 | ||
| None/Don’t know | 72 (45.3) | 48 (45.7) | |
| At least one | 87 (54.7) | 57 (54.3) | |
|
| |||
| Waterpipe smoking by siblings | 0.27 | ||
| None/Don’t know | 76 (47.8) | 43 (41.0) | |
| At least one | 83 (52.2) | 62 (59.0) | |
|
| |||
| Waterpipe smoking by close friends | 0.02 | ||
| None | 28 (17.6) | 8 (7.6) | |
| At least one | 131 (82.4) | 97 (92.4) | |
|
| |||
| Having a favorite waterpipe ad | 0.14 | ||
| No/Don’t know | 138 (86.8) | 84 (80.0) | |
| Yes | 21 (13.2) | 21 (20.0) | |
|
| |||
| It would be very difficult to me to be in a restaurant, and not smoke waterpipe** | 0.007 | ||
| Not true | 53 (33.3) | 19 (18.1) | |
| Somewhat true | 40 (25.2) | 35 (33.3) | |
| True | 66 (41.5) | 51 (48.6) | |
|
| |||
| Just the sight or smell of waterpipe is enough to make me want to smoke** | 0.29 | ||
| Not true | 45 (28.7) | 24 (22.9) | |
| Somewhat true | 31 (19.7) | 19 (18.1) | |
| True | 81 (51.6) | 62 (59.0) | |
|
| |||
| I smoke waterpipe usually with friends or in cafes/restaurants** | 0.52 | ||
| Not true | 89 (56.0) | 54 (51.9) | |
| Somewhat true | 30 (18.9) | 21 (20.2) | |
| True | 40 (25.2) | 29 (27.9) | |
Bold indicates p<0.05;
Items 1 from the Syrian Center for Tobacco Studies (SCTS-28)
2.2.2. Outcome variable
We used the Hooked on Nicotine Checklist (HONC) as a continuous measure of ND (score range 0–10).14, 21 The HONC was administered to participants who smoked waterpipe in the 30 days prior to data collection. HONC scores were recorded for each participant at each wave (0 for waves with reports of no tobacco use). An increase over the baseline HONC score at any subsequent wave indicated a progression in the severity of ND. For participants who initiated waterpipe smoking during follow up, progression of ND was defined as a higher HONC score at a subsequent wave compared with the wave when waterpipe smoking was first reported. HONC has been validated among adolescent cigarette and smokeless tobacco users,25, 26 and among adolescent waterpipe smokers in this cohort.14 HONC has acceptable internal consistency of 0.74 and good convergent construct validity in this cohort.14
2.2.3. Statistical analysis
We compared baseline characteristics between those who progressed and those who did not. Categorical variables were compared using chi-square test, and ratio variables were compared using t-test or Mann-Whitney U test as appropriate. To model the factors predicting progression of ND symptoms (Yes=1, No=0), a generalized linear mixed model technique applying the SAS GLIMMIX procedure was used to account for clustering of participants within schools and for the repeated measures during follow up. We defined our outcome variable as binary (progressed =1, did not progress=0) rather than continuous for consistency with the literature on progression of smoking behaviors in adolescents,27–30 and for the ease of interpreting the results.
For the sample included in this study, 14 participants (5%) were missing data on the outcome of interest (progression of ND symptoms) and were excluded from the analysis.31 Covariates with p<0.30 in the bivariable analysis were included in the final multivariable model. We also controlled for cigarette use in the multivariable model.
We checked multicollinearity among predictor variables by examining the correlations among them, and by looking at the variance inflation factor (VIF). A cut-off value of VIF ≤5 was applied to rule out multicollinearity.21 Accordingly, multicollinearity was not an issue in this analysis. Independent variables with p<0.20 in the bivariable models were entered simultaneously into the multivariable model.29 Odds ratios (OR) and 95% confidence intervals (CIs) were calculated from the regression analysis. P-values of <0.05 were considered statistically significant. All analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
3. RESULTS
3.1. Sample characteristics
The analytic sample included 264 adolescents who were current waterpipe smokers at baseline or any of the 4 follow up points. This sample had a baseline mean age of 14.6 (SD=1.2) years, and 50.4% were females. During the 24 months of follow up in this study, 105 (39.7%) participants progressed on ND symptoms. Table 1 presents the proportion of participants that progressed within each period of follow-up by gender and age group. There was no significant difference (p=0.93) in baseline HONC scores between those who progressed (mean HONC score ± SD = 1.7 ± 1.7) and those who did not (2.3 ± 2.2). Figure 1 shows cumulative average HONC scores among participants in this study over the study period according to the baseline reported difficulty refraining from smoking waterpipe while in a restaurant. Those who reported difficulty refraining from smoking waterpipe while in a restaurant at baseline had higher HONC scores compared with those who reported less or no difficulty at baseline (see figure 1).
Table 1.
Proportion of participants that progressed within each follow up period by age groups and gender (N=264)
| Wave 1-Wave 2 n (%) |
Wave 2-Wave 3 n (%) |
Wave 3-Wave 4 n (%) |
Wave 4-Wave 5 n (%) |
Total n (%) |
|
|---|---|---|---|---|---|
| Age groups in years | |||||
| 12–13 (n=47) | 5 (10.6) | 19 (40.4) | 4 (8.5) | 5 (10.6) | 33 (70.2) |
| 14–15(n=164) | 22 (13.4) | 21 (12.8) | 13 (7.9) | 7 (4.3) | 63 (38.4) |
| >=16 (n=53) | 3 (5.7) | 4 (7.5) | 2 (3.8) | 0(0) | 9 (16.9) |
| Gender | |||||
| Male (n=131) | 12 (9.2) | 23 (17.6) | 9 (6.9) | 10 (7.6) | 54 (41.2) |
| Female (n=133) | 18 (13.5) | 21 (15.8) | 10 (7.5) | 2 (1.5) | 51 (38.3) |
Figure 1.
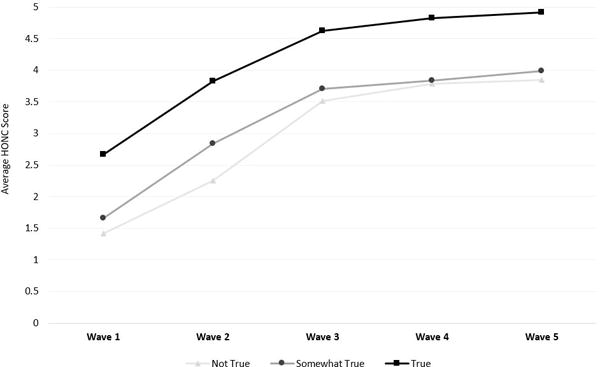
Avergae no. of nicotine dependence symptoms–measured by Hooked on Nicotine Checklist (HONC)–as predicted by baseline difficulty refraining from smoking waterpipe while in a restaurant.
3.2 Bivariable analysis
Table 2 presents participants’ individual and socio-environmental characteristics at baseline according to their ND progression status. A majority of participants smoked less than daily. A higher proportion (44.8%) of those who progressed, compared to those who did not progress (28.3%), smoked waterpipe every week (p=0.02). Concerning psychological factors, baseline stress and self-esteem scores were higher among those who progressed compared with those who did not (Table 2). In regards to socio-environmental factors, a lower proportion of participants who progressed on ND symptoms had mothers with ≥ 12 years of education, and a higher proportion of close friends who smoke waterpipe. Lastly, participants who reported difficulty refraining from smoking waterpipe while in a restaurant were more likely to progress on ND during follow up (Table 2).
3.3. Multivariable analysis
Table 3 presents results from a multilevel logistic regression analysis for factors affecting the progression on ND symptoms. Having higher baseline scores of stress, self-esteem, and reporting difficulty refraining from smoking waterpipe while in a restaurant predicted progression of ND symptoms during follow up. Having a mother with ≥ 12 years of education protected against progression of ND symptoms. These four predictors explained about 36% of the variability in progression of ND symptoms.
Table 3.
Predictors of progression of ND symptoms
| Adjusted odds ratio (95% CI) | p-value | |
|---|---|---|
|
| ||
| Mother’s years of education | ||
| < 12 years of education/Cannot read or write | Ref | 0.04 |
| ≥ 12 years of education | 0.46 (0.21–0.99) | |
|
| ||
| Stress | 1.11 (1.03–1.19) | 0.009 |
|
| ||
| Self esteem | 1.14 (1.05–1.24) | 0.003 |
|
| ||
| It would be very difficult to me to be in a restaurant, and not smoke waterpipe | ||
| Not true | Ref | 0.01 |
| Somewhat true | 4.56 (1.61–12.95) | |
| True | 4.04 (1.44–11.34) | |
4. DISCUSSION
In this longitudinal study, we examined a broad range of individual and socio-environmental predictors of a progression in ND as measured by the HONC. A mixture of individual (stress, self-esteem) and socio-environmental factors (mother’s education, waterpipe café/restaurant) predicted progression of ND symptoms in adolescent waterpipe smokers. Higher stress and self- esteem at baseline predicted progression of ND symptoms during follow up. Adolescents whose mothers have ≥12 years of education were less likely to progress on ND symptoms. A salient finding in this study is that reporting difficulty refraining from waterpipe while in a restaurant strongly predicted progression in ND symptoms in adolescent waterpipe smokers. This may underline the role of smoking cues in waterpipe-serving venues, and the important role of these venues in promoting ND. Taken together, these findings emphasize the need for a comprehensive approach that takes into account individual and socio-environmental factors to address ND in waterpipe smokers. Most importantly, venue-based policies such as limiting youth access to waterpipe cafés, and regulating the availability of waterpipes in waterpipe-serving venues can be effective interventions to curb the waterpipe epidemic among youth.
Among the conceptual models of ND, the Coping and Outcome Expectancy models provide useful insights to explain the observed association between stress with progression of ND in this study. According to the Coping model of ND, smoking is a coping mechanism adolescents use to maintain positive affects and to reduce stress in their lives.32 The Outcome Expectancy model states that an individual’s expectancies of a positive outcome associated with smoking leads to ND. Globally, youth entertain the social nature of waterpipe smoking with close friends and describe this practice as a source of relaxation.1, 7, 10 That youth may find waterpipe a way of coping with stress is plausible, given the expectation of relaxation and pleasure surrounding waterpipe use,33 which may drive continued exposure to waterpipe and progression of ND symptoms.
Interestingly, our finding that higher self-esteem predicted progression of ND symptoms in waterpipe smokers is contrary to that observed in cigarette smokers in which low self-esteem was associated with experiencing symptoms of ND.34 Generally, youth with lower self-esteem are more prone to risky behaviors, such as cigarette smoking.35 As waterpipe smoking is widely perceived as safer, less addictive than cigarettes,9, 10, 33 and is prominently social in nature,1 youth with higher self-esteem maybe more inclined to continue to engage in waterpipe than cigarette smoking. Indeed, studies in the US and elsewhere suggest that positive attitudes towards waterpipe are contributing to its spread among youth worldwide.1, 36
Findings from previous research indicate that higher educational attainment by parents protects against adolescent cigarette smoking,37 and among adolescents who do smoke, progression to ND.38 This study is the first to investigate the link between parental education and progression of ND symptoms in adolescent waterpipe smokers longitudinally. Our finding that higher maternal education protected against progression of ND symptoms in adolescents may reflect a more important role for the mother on her family members, owing to the extended time and responsibility of raising her children compared to the father in Middle Eastern societies.39, 40 In fact, waterpipe-only use or dual use of waterpipe and cigarettes by a mother was a better predictor, compared with smoking status of a father, of waterpipe smoking among adolescents in Middle Eastern societies.41 Moreover, Lebanese women with at least a secondary education are less likely to smoke compared with women with an elementary education.42 In fact, women in this study with ≥ 12 years of education were less likely to smoke waterpipe (p<0.05, data not shown), providing a role model to their children against waterpipe smoking. In addition to being well informed on smoking-related harm,43 women with higher education may have effective communication skills with their children to discourage risky behaviors such as smoking and prevent progression to more advanced stages of smoking/ND.
One of the main drivers of the global spread of waterpipe among youth is the flourishing business of waterpipe-serving establishments (known as waterpipe cafés, lounges, bars, or restaurants).1 These establishments provide an environment that facilitates social interaction and are likely to play a role in initiation and regular use of waterpipe among youth. A salient finding of this study is that adolescents who, at baseline, reported difficulty refraining from waterpipe smoking when in a restaurant were 4 times more likely, compared with those did not report difficulty, to progress on ND symptoms during follow up. Whether a dedicated waterpipe café or a restaurant serving waterpipe in addition to food,1 these venues provide environmental sensory cues that have the potential to trigger the urge to smoke waterpipe.44 As indicated above, the allure of waterpipe cafés and the social, relaxing nature of waterpipe smoking can act as positive reinforcers for nicotine self-administration. Therefore, waterpipe venues regulation (e.g., limiting underage access) can be a good start for policies aiming at reducing waterpipe use among adolescents.
This study has limitations. First, due to logistical difficulties, we relied upon adolescents to report educational attainment and smoking status of their parents instead of collecting these variables directly from the parents. This reliance on adolescents as sources may have introduced misclassification bias in parental variables. However, obtaining parental variables that influence adolescents’ smoking behaviors and ND symptoms indirectly from adolescents is a standard practice validated in national surveys such as the Global Youth Tobacco Survey administered by the World Health Organization.45 Additionally, we followed strict procedures to ensure privacy of interviews to minimize information bias. Second, we relied upon only one measure of ND symptoms (HONC) that measures the loss of autonomy. Given that ND is conceptualized as having multiple components in addition to a loss of autonomy,32 the definition of ND progression and hence the predictors of progression may differ depending on the specific tool used to evaluate ND. We chose the HONC because it is highly sensitivity to ND even with intermittent tobacco use compared with the commonly used ND diagnostic tools (i.e., ICD-10, DSM-IV), and was developed to assess the development of ND in adolescents.22 Third, it is possible that those with higher HONC scores report more difficulty refraining from smoking waterpipe while in waterpipe-serving establishments. However, there was no significant differences in baseline HONC scores between those who progressed and those who did not, and the longitudinal design allowed for investigating a temporal association between reporting difficulty refraining from smoking waterpipe while in a waterpipe-serving establishment and progression of ND.
Our findings highlight the role of individual and socio-environmental factors in the progression of ND symptoms among adolescent waterpipe smokers, and some differences from what is seen with cigarette smokers. It is important to understand ND in adolescent waterpipe smokers in order to design waterpipe specific interventions and guide policies to prevent progression of smoking and ND. This study is the first to document the salient role of exposure to environmental cues in waterpipe-serving venues in the progression of ND symptoms in adolescents. Therefore, venue-based policies such as limiting youth access to waterpipe cafés and regulating waterpipe availability in restaurants seems like a good starting point to prevent the development of ND in young waterpipe smokers.
What’s Known on This Subject
Waterpipe smoking has become a global epidemic among youth and young adults. Unique individual and socio-environmental factors contributed to the global rise of waterpipe smoking. Waterpipe smoking is addictive, and many youth experience symptoms of nicotine dependence and face difficulty quitting.
What This Study Adds
We investigated the factors associated with progression of nicotine dependence symptoms among adolescent waterpipe smokers. The waterpipe café emerged as the most important predictor of progression of nicotine dependence among adolescent waterpipe smokers.
Acknowledgments
Funding: The WDLY study is funded by grants R01DA035160 and R01TW010654 from the National Institute of Health Fogarty International Center (NIH FIC), and National Institute on Drug Abuse (NIDA) of the National Institute of Health (PI: Wasim Maziak). Dr. Eissenberg is supported, in part, by the National Institute on Drug Abuse of the National Institutes of Health under Award Number P50DA036105 and the Center for Tobacco Products of the U.S. Food and Drug Administration. The content is solely the responsibility of the authors and does not necessarily represent the views of the NIH or the FDA. Dr. Jaber was supported by the American Heart Association Tobacco Regulation and Addiction Center under National Heart, Lung, and Blood Institute of the National Institutes of Health and Center for Tobacco Products Award Number P50HL120163.
Footnotes
Contributors: Dr. Bahelah and Prof. Maziak conceptualized and designed the study, supervised data collection, performed the initial analyses, contributed to interpretation of the data, and drafted the initial manuscript, and critically revised the manuscript for important intellectual content. Drs. Ward, Ben Taleb, DiFranza, Eissenberg, and Jaber contributed to interpretation of the data, and critically revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Competing Interests: Dr. Eissenberg is a paid consultant in litigation against the tobacco industry and is named on a patent application for a device that measures the puffing behavior of electronic cigarette users. The other authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Maziak W, Taleb ZB, Bahelah R, et al. The global epidemiology of waterpipe smoking. Tob Control. 2015;24(Suppl 1):i3–i12. doi: 10.1136/tobaccocontrol-2014-051903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med. 2009;37(6):518–23. doi: 10.1016/j.amepre.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kassem NO, Kassem NO, Jackson SR, et al. Benzene uptake in Hookah smokers and nonsmokers attending Hookah social events: regulatory implications. Cancer Epidemiol Biomarkers Prev. 2014;23(12):2793–809. doi: 10.1158/1055-9965.EPI-14-0576. [DOI] [PubMed] [Google Scholar]
- 4.Al Ali R, Rastam S, Ibrahim I, et al. A comparative study of systemic carcinogen exposure in waterpipe smokers, cigarette smokers and non-smokers. Tob Control. 2015;24(2):125–7. doi: 10.1136/tobaccocontrol-2013-051206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maziak W, Rastam S, Shihadeh AL, et al. Nicotine exposure in daily waterpipe smokers and its relation to puff topography. Addict Behav. 2011;36(4):397–9. doi: 10.1016/j.addbeh.2010.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.El-Zaatari ZM, Chami HA, Zaatari GS. Health effects associated with waterpipe smoking. Tob Control. 2015;24(Suppl 1):i31–i43. doi: 10.1136/tobaccocontrol-2014-051908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Akl EA, Ward KD, Bteddini D, et al. The allure of the waterpipe: a narrative review of factors affecting the epidemic rise in waterpipe smoking among young persons globally. Tob Control. 2015;24(Suppl 1):i13–i21. doi: 10.1136/tobaccocontrol-2014-051906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gathuru IM, Tarter RE, Klein-Fedyshin M. Review of hookah tobacco smoking among college students: policy implications and research recommendations. Am J Drug Alcohol Abuse. 2015;41(4):272–80. doi: 10.3109/00952990.2015.1043738. [DOI] [PubMed] [Google Scholar]
- 9.Afifi R, Khalil J, Fouad F, et al. Social norms and attitudes linked to waterpipe use in the Eastern Mediterranean Region. Soc Sci Med. 2013;98:125–34. doi: 10.1016/j.socscimed.2013.09.007. [DOI] [PubMed] [Google Scholar]
- 10.Hammal F, Mock J, Ward KD, Eissenberg T, Maziak W. A pleasure among friends: how narghile (waterpipe) smoking differs from cigarette smoking in Syria. Tob Control. 2008;17(2):e3. doi: 10.1136/tc.2007.020529. [DOI] [PubMed] [Google Scholar]
- 11.Smith-Simone S, Maziak W, Ward KD, Eissenberg T. Waterpipe tobacco smoking: knowledge, attitudes, beliefs, and behavior in two U.S. samples. Nicotine Tob Res. 2008;10(2):393–8. doi: 10.1080/14622200701825023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ward KD, Eissenberg T, Gray JN, Srinivas V, Wilson N, Maziak W. Characteristics of U.S. waterpipe users: a preliminary report. Nicotine Tob Res. 2007;9(12):1339–46. doi: 10.1080/14622200701705019. [DOI] [PubMed] [Google Scholar]
- 13.Sterling KL, Mermelstein R. Examining hookah smoking among a cohort of adolescent ever smokers. Nicotine Tob Res. 2011;13(12):1202–9. doi: 10.1093/ntr/ntr146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bahelah R, DiFranza JR, Fouad FM, Ward KD, Eissenberg T, Maziak W. Early symptoms of nicotine dependence among adolescent waterpipe smokers. Tob Control. 2016;25(e2):e127–e134. doi: 10.1136/tobaccocontrol-2015-052809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson D, Aveyard P. Waterpipe smoking in students: prevalence, risk factors, symptoms of addiction, and smoke intake. Evidence from one British university. BMC Public Health. 2008;8:174. doi: 10.1186/1471-2458-8-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kassim S, Al-Bakri A, Al’Absi M, Croucher R. Waterpipe tobacco dependence in U.K. male adult residents: a cross-sectional study. Nicotine Tob Res. 2014;16(3):316–25. doi: 10.1093/ntr/ntt148. [DOI] [PubMed] [Google Scholar]
- 17.Baharudin MI, Al Kubaisy W, Norden N, et al. Prevalence of Nicotine Dependence Among Youth Smokers (Cigarette and Shisha) in Malaysia. GSTF Journal of Nursing and Healthcare (JNHC) 2016;3(1):39–47. [Google Scholar]
- 18.Arief M, Shankar N, Iizhar AS, et al. Determination of Awareness and Nicotine Dependency Level Among Shisha Smokers in Malaysia. IJPCR. 2016;8(6):543–547. [Google Scholar]
- 19.Primack BA, Khabour OF, Alzoubi KH, et al. The LWDS-10J: reliability and validity of the Lebanon Waterpipe Dependence Scale among university students in Jordan. Nicotine Tob Res. 2014;16(7):915–22. doi: 10.1093/ntr/ntu002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sidani JE, Shensa A, Shiffman S, Switzer GE, Primack BA. Behavioral associations with waterpipe tobacco smoking dependence among US young adults. Addiction. 2016;111(2):351–9. doi: 10.1111/add.13163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bahelah R, DiFranza JR, Ward KD, et al. Correlates of nicotine dependence among adolescent waterpipe smokers. Drug Alcohol Depend. 2016;168:230–238. doi: 10.1016/j.drugalcdep.2016.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kleinjan M, Vitaro F, Wanner B, Brug J, Van den Eijnden RJ, Engels RC. Predicting nicotine dependence profiles among adolescent smokers: the roles of personal and social-environmental factors in a longitudinal framework. BMC Public Health. 2012;12:196. doi: 10.1186/1471-2458-12-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kandel DB, Griesler PC, Hu MC. Intergenerational Patterns of Smoking and Nicotine Dependence Among US Adolescents. Am J Public Health. 2015;105(11):e63–72. doi: 10.2105/AJPH.2015.302775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Berry CC. Tobacco industry promotion of cigarettes and adolescent smoking. JAMA. 1998;279(7):511–5. doi: 10.1001/jama.279.7.511. [DOI] [PubMed] [Google Scholar]
- 25.DiFranza JR, Rigotti NA, McNeill AD, et al. Initial symptoms of nicotine dependence in adolescents. Tob Control. 2000;9:313–19. doi: 10.1136/tc.9.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DiFranza JR, Sweet M, Savageau JA, et al. The assessment of tobacco dependence in young users of smokeless tobacco. Tob Control. 2012;21:471–6. doi: 10.1136/tc.2011.043810. [DOI] [PubMed] [Google Scholar]
- 27.Kim MJ, Fleming CB, Catalano RF. Individual and Social Influences on Progression to Daily Smoking During Adolescence. Pediatrics. 2009;124(3):895–902. doi: 10.1542/peds.2008-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Audrain-McGovern J, Rodriguez D, Patel V, Faith MS, Rodgers K, Cuevas J. How do psychological factors influence adolescent smoking progression? The evidence for indirect effects through tobacco advertising receptivity. Pediatrics. 2006;117(4):1216–25. doi: 10.1542/peds.2005-0808. [DOI] [PubMed] [Google Scholar]
- 29.Jaber R, Madhivanan P, Khader Y, Mzayek F, Ward KD, Maziak W. Predictors of waterpipe smoking progression among youth in Irbid, Jordan: A longitudinal study (2008-2011) Drug Alcohol Depend. 2015;153:265–70. doi: 10.1016/j.drugalcdep.2015.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jaber R, Mzayek F, Madhivanan P, Khader Y, Maziak W. Predictors of Cigarette Smoking Progression Among a School-Based Sample of Adolescents in Irbid, Jordan: A Longitudinal Study (2008-2011) Nicotine Tob Res. 2016;18(4):403–9. doi: 10.1093/ntr/ntv100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Graham JW. Missing data analysis: making it work in the real world. Annu Rev Psychol. 2009;60:549–76. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- 32.Brandon TH, Herzog TA, Irvin JE, Gwaltney CJ. Cognitive and social learning models of drug dependence: implications for the assessment of tobacco dependence in adolescents. Addiction. 2004;99(Suppl 1):51–77. doi: 10.1111/j.1360-0443.2004.00737.x. [DOI] [PubMed] [Google Scholar]
- 33.Griffiths MA, Ford EW. Hookah smoking: behaviors and beliefs among young consumers in the United States. Soc Work Public Health. 2014;29(1):17–26. doi: 10.1080/19371918.2011.619443. [DOI] [PubMed] [Google Scholar]
- 34.Racicot S, McGrath JJ, Karp I, O’Loughlin J. Predictors of nicotine dependence symptoms among never-smoking adolescents: a longitudinal analysis from the Nicotine Dependence in Teens Study. Drug Alcohol Depend. 2013;130(1–3):38–44. doi: 10.1016/j.drugalcdep.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.O’Loughlin J, Karp I, Koulis T, Paradis G, Difranza J. Determinants of first puff and daily cigarette smoking in adolescents. Am J Epidemiol. 2009;170(5):585–97. doi: 10.1093/aje/kwp179. [DOI] [PubMed] [Google Scholar]
- 36.Sidani JE, Shensa A, Naidu MR, Yabes JG, Primack BA. Initiation, Progression, and Sustained Waterpipe Use: A Nationally Representative Longitudinal Study of U.S. Young Adults. Cancer Epidemiol Biomarkers Prev. 2017;26(5):748–755. doi: 10.1158/1055-9965.EPI-16-0687-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Reynolds B, Karraker K, Horn K, Richards JB. Delay and probability discounting as related to different stages of adolescent smoking and non-smoking. Behav Processes. 2003;64(3):333–344. doi: 10.1016/s0376-6357(03)00168-2. [DOI] [PubMed] [Google Scholar]
- 38.Kandel DB, Griesler PC, Hu MC. Intergenerational Patterns of Smoking and Nicotine Dependence Among US Adolescents. Am J Public Health. 2015;105(11):e63–72. doi: 10.2105/AJPH.2015.302775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Erbaydar T, Lawrence S, Dagli E, Hayran O, Collishaw NE. Influence of social environment in smoking among adolescents in Turkey. Eur J Public Health. 2005;15(4):404–10. doi: 10.1093/eurpub/cki040. [DOI] [PubMed] [Google Scholar]
- 40.Ny P, Plantin L, Karlsson ED, Dykes AK. Middle Eastern mothers in Sweden, their experiences of the maternal health service and their partner’s involvement. Reprod Health. 2007;24:4–9. doi: 10.1186/1742-4755-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Veeranki SP, Alzyoud S, Dierking L, et al. Associations of Adolescents’ Cigarette, Waterpipe, and Dual Tobacco Use With Parental Tobacco Use. Nicotine Tob Res. 2016;18(5):879–84. doi: 10.1093/ntr/ntv224. [DOI] [PubMed] [Google Scholar]
- 42.Afifi RA, Nakkash RT, Khawaja M. Social capital, women’s autonomy and smoking among married women in low-income urban neighborhoods of Beirut, Lebanon. Womens Health Issues. 2010;20(2):156–67. doi: 10.1016/j.whi.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 43.Maziak W, Asfar T, Mock J. Why most women in Syria do not smoke: can the passive barrier of traditions be replaced with an information-based one? Public Health. 2003;117(4):237–41. doi: 10.1016/S0033-3506(03)00070-2. [DOI] [PubMed] [Google Scholar]
- 44.Maziak W, Eissenberg T, Ward KD. Patterns of waterpipe use and dependence: implications for intervention development. Pharmacology, Biochemistry and Behavior. 2005;80:173–179. doi: 10.1016/j.pbb.2004.10.026. [DOI] [PubMed] [Google Scholar]
- 45.Global Youth Tobacco Survey (GYTS) — Overview. Available from: https://nccd.cdc.gov/GTSSDataSurveyResources/Ancillary/Documentation.aspx?SUID=1&DOCT=1 [Accessed 9/10/2017]


