Abstract
A one-year-old baby girl with one-month history of recurrent pus fluid exuding from her left preauricular sinus orifice, who failed multiple courses of surgical drainage of the abscess and persistent debridement for the wound, presented with MRSA infection. The patient was treated with linezolid for three days. Her pain and paresthesia resolved, and C-reactive protein decreased to normal.
Keywords: Preauricularsinus, Surgery, Overuse antibiotics, Methicillin-resistant staphylococcus aureus, Cellulitis
1. Case report
The patient, a 1 year old female, was admitted to the hospital for repeated discharge from a left preauricular sinus for one month. Slight swelling appeared in the left preauricular area around a hole at the root of the helix, through which discharge exuded out, accompanied by pain and fever. The wound had been treated with open drainage, repeated debridement and dressing exchange in the local hospital of her hometown. Due to her recurrent symptoms and poor condition control, the patient was referred to our hospital.
Physical examination showed a small hole in front of the left ear (Fig. 1) with no abnormal exudate. Body temperature was 36.3 °C. After appropriate preoperative evaluation, a fistulectomy was performed under general anesthesia at 9 a.m. on the second day in the hospital. At 4 p.m. on the operation day, body temperature rose to 40.1 °C and the left frontotemporal and mandibular area became red and swollen, spreading across the chin to the contralateral side (Fig. 2).
Fig. 1.
There was a small orifice in front of her left ear.
Fig. 2.
The left frontotemporal and lower jaw became red and swollen, spreading from submentum to opposite side cheek.
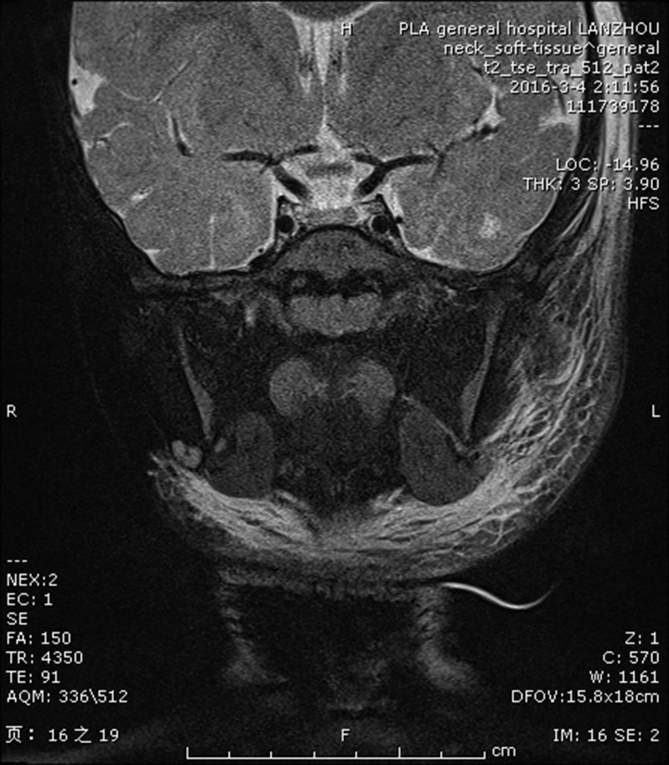
Laboratory tests showed increased c-reactive protein levels to 130.25 mg/L. Routine blood tests indicated infection, with white blood cell count at 17.96 * 109/L, neutrophils at 16.03 * 109/L and neutrophilic granulocytes at 89.3%. At the same time, magnetic resonance imaging showed soft tissue swelling in the neck and interstitial exudation spreading to the left frontotemporal area, eyelid, maxillofacial area, both sides of the nasal root and nasal ridge, mandibular angle and thyroid area (Fig. 3).
Fig. 3.
Cervical soft tissue swelling and interstitial exudation spreading to the left frontotemporal, eyelid, maxillofacial region, bilateral root of nose, nasal dorsum, angle of mandible to thyroid region.
Enlarged lymph nodes were seen in the interstitial space between the peripharyngeal space and bilateral carotid arteries. The cause for increased body temperature was determined to be bacterial infection, and aztreonam was immediately started as an anti-infection treatment. On the second day after surgery, upon dressing exchange, a large amount of purulent secretion was drained from the wound with worse swelling. Exudate specimens were taken for bacterial culture, which came back 3 days later as positive for methoxicillin resistant staphylococcus aureus (MRSA+), indicating cellulitis caused by MRSA infection.
Based on bacterial culture and sensitivity results, linezolid was used as the antibacterial agent instead of aztreonam on the 4th day after surgery. During the following period, body temperature was constantly monitored for physical cooling and other treatments, with the wound cleaned daily using hydrogen peroxide and sodium chloride. A drainage strip was kept in the incision.
On the 6th day after operation, the patient's body temperature was down to 36.9 °C, while swelling of the left frontotemporal area subsided. As daily debridement and antibiotic therapy continued, pain significantly reduced. Laboratory tests now showed c-reactive protein at 4.1 mg/L, with white blood cell count at 10.63 × 109/L and neutrophils at 2.83 × 109/L. One month later, color ultrasound continued to show cervical lymph nodes enlargement, but no other abnormalities. No recurrence was observed in 20 months of follow-up. Detailed review of medication usage history reviewed that the child had been taking Cefixime and other cephalosporin antibiotics repeatedly without prescription.
2. Discussion
Preauricular fistula, also called congenital ear fistula, usually presents with a small opening at the root of helix (Gan et al., 2013). Preauricular fistula is usually asymptomatic and does not require treatment (Gur et al., 1998). Patients with fistula infection must be treated with systemic antibiotics. Once infection occurs, the likelihood of acute deterioration is high. Improper treatment of patients with fistula infection can lead to repeated infection and may lead to severe postoperative scar formation (Tan et al., 2005).The most common pathogens that cause infection are staphylococcus aureus and streptococcus viridans, pseudomonas aeruginosa, peptostreptococcus, clostridium perfringens and fragile bacillus. While proteus, streptococcus and digestive bacteria genera are rarely involved (Xiao et al., 2010; Scheinfeld et al., 2004).
MRSA is resistant to all β-lactam antibiotics and kills about 20,000 people a year in the United States. Although there have been few reports of preauricular fistula infection by MRSA, there has been an increase of MRSA infection in soft tissues in the ear, nose and throat area (Bothwell et al., 2007; Thirumazhisi, 2014). This case is the first case of a preauricular fistula complicated with MRSA infection.
In this case, there is evidence of irregular use of multiple cephalosporin antibiotics and combined use of multiple antibiotics. The operation may be one of the causes for the outbreak of the drug-resistant bacteria, which led to the occurrence of cellulitis. In addition to the use of sensitive antibiotics, repeated dressings exchanges combined with cleaning using hydrogen peroxide and normal saline, as well as other comprehensive treatments also produced significant effects.
3. Conclusion
Once preauricular sinus infection occurs repeatedly, the possibility of acute exacerbation is high, and the fistula should be surgically removed (Scheinfeld et al., 2004). If the patient develops an abscess, open drainage should be considered, with specimens sent for bacteria culture. Patients with recurrent infection and abscess formation should be treated with open drainage, rather than antibiotics without the guidance by a physician.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.joto.2018.07.002.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- Bothwell N.E., Shvidler J., Cable B.B. Acute rise in methicillin-resistant Staphylococcus aureus infections in a coastal community. Otolaryngol. Head Neck Surg. 2007;137 doi: 10.1016/j.otohns.2007.09.013. 942e946. [DOI] [PubMed] [Google Scholar]
- Gan E.C., Anicete R., Tan H.K., Balakrishnan A. Preauricular sinuses in the pediatric population: techniques and recurrence rates. Int. J. Pediatr. Otorhinolaryngol. 2013;77(3):372–378. doi: 10.1016/j.ijporl.2012.11.029. [DOI] [PubMed] [Google Scholar]
- Gur E., Yeung A., Al-Azzawi M., Thomson H. The excised preauricular sinus in 14 years of experience: is there a problem? Plast. Reconstr. Surg. 1998;102(5):1405–1408. doi: 10.1097/00006534-199810000-00012. [DOI] [PubMed] [Google Scholar]
- Scheinfeld N.S., Silverberg N.B., Weinberg J.M., Nozad V. The preauricular sinus: a review of its clinical presentation, treatment, and associations. Pediatr. Dermatol. 2004;21(3):191–196. doi: 10.1111/j.0736-8046.2004.21301.x. [DOI] [PubMed] [Google Scholar]
- Tan T., Constantinides H., Mitchell T.E. The preauricular sinus: a review of its aetiology, clinical presentation and management. Int. J. Pediatr. Otorhinolaryngol. 2005;69(11):1469–1474. doi: 10.1016/j.ijporl.2005.07.008. [DOI] [PubMed] [Google Scholar]
- Thirumazhisi S.S. Rising methicillin-resistant Staphylococcus aureus infections in ear, nose, and throat diseases. Case Rep Otolaryngol. 2014;2014 doi: 10.1155/2014/253945. 253945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Y.H., Fang H., Jin W. Chinese Health Economics; 2010. An Investigation into Socio-economic Impact of Adverse Drug Reactions of Antibacterial Agent Irrational Use. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.