Abstract
Introduction:
Hyperparathyroidism significantly decreases quality of life, yet elderly patients are underdiagnosed and undertreated even though parathyroidectomy offers definitive cure with minimal morbidity. The purpose of this study is to determine why older patients with hyperparathyroidism are not appropriately diagnosed and referred for parathyroidectomy.
Methods:
We reviewed charts for a random sample of 25 patients aged 75 and older who had hyperparathyroidism and were referred for surgical evaluation, and 25 who were not referred. Two reviewers independently evaluated medical records to identify reasons for delayed diagnosis of hyperparathyroidism and reasons for nonreferral for parathyroidectomy.
Results:
The median age of our cohort was 84 (80-96) years, 90% were women, 60% were white, and median follow-up was 5.5 (1-17) years. In 58% of all patients, an elevated serum calcium was not acknowledged. Even when calcium and parathyroid hormone levels were both elevated, the diagnosis was missed in 28% of patients, and 16% with clear symptoms of hyperparathyroidism remained undiagnosed. For 42% of patients, a nonsurgeon informed them that surgery offered no benefit. Surgery was also rejected as a treatment for 36% of patients despite the development of new symptoms or rising calcium.
Conclusions:
Substantial gaps exist in processes for diagnosis and referral of patients with hyperparathyroidism that lead to underdiagnosis and undertreatment. To improve rates of diagnosis and treatment, strategies are needed to educate nonsurgeons and patients about the benefits of surgery and to modify care processes to more efficiently diagnose and refer patients.
Keywords: Hyperparathyroidism, underdiagnosis, elderly, parathyroidectomy
Background
Primary hyperparathyroidism is thought to be the most common cause of hypercalcemia, affecting approximately 2 million Americans.1,2 The incidence of hyperparathyroidism increases with age from 12 to 24 per 100 000 in patients less than 50 years old to 95 to 196 per 100 000 in patients aged 70 to 79 years.1 Failure to diagnose and treat hyperparathyroidism increases the risk of osteoporosis and fractures, leads to kidney stones and renal failure, and can greatly impair quality of life.3,4 Parathyroidectomy is the only definitive treatment for hyperparathyroidism and can restore bone health, reduce the odds of renal failure or kidney stones, and dramatically improve quality of life.3–5 Surgical treatment of hyperparathyroidism is more cost-effective than observation or medical therapy because the procedure has minimal morbidity and offers substantial benefit by reducing or eliminating the harmful effects of the disease.6–8 Unfortunately, our group and others have found that older patients are significantly less likely to be diagnosed and treated for hyperparathyroidism than younger patients.1,9–11
Although hyperparathyroidism is underdiagnosed and undertreated in the elderly, the reasons for these deficiencies have not been identified. This represents a critical barrier to the design of effective interventions because it is not clear what the intervention content should be and how implementation should be designed. Several potential explanations for why older patients with hyperparathyroidism are underdiagnosed or underreferred have been proposed.9–12 The most common presentation of hyperparathyroidism is an abnormal calcium on routine laboratory evaluation, and this could easily be missed or attributed to other causes. The diagnosis of hyperparathyroidism requires the ability to interpret the relationship between calcium and parathyroid hormone (PTH) levels, and this can be a complex calculation that requires expert assistance. In addition, nonsurgeons may overestimate the risks of surgery or underestimate the benefits to patients, which could decrease rates of referral.
The purpose of this study is to better understand why hyperparathyroidism is underdiagnosed and undertreated by (1) exploring the reasons why elderly patients with hypercalcemia are not evaluated for hyperparathyroidism and (2) evaluating why elderly patients are not being referred to surgeons to discuss treatment. We hypothesized that (1) patients are not diagnosed because abnormal lab results are missed, or a diagnosis of primary hyperparathyroidism is not considered when patients present with hypercalcemia, and (2) patients are not referred for discussion of parathyroidectomy because nonsurgeons underestimate the benefits or overestimate the risks of surgery.
Methods
Patient population
We used administrative data from the electronic medical record system at the University of Alabama at Birmingham (UAB), a tertiary referral center, from 2011 to 2015. Institutional review board approval was obtained for data collection and analysis. We developed our study cohort by first identifying 10 432 patients with hypercalcemia (defined as serum calcium >10.5 mg/dL) at UAB. From that cohort, we found 1825 patients with hypercalcemia who also had an elevated PTH. We divided the cohort into patients who were eventually referred to a surgeon and those who were never referred and then randomly selected 25 charts for patients aged 75 years or older from each group. Patients were classified as “referred to surgeon” if any note from a surgeon who performs parathyroidectomy was found in the medical record after the initial abnormal calcium was identified.
Data collection and analysis
The 2 reviewers (A.D., a medical student, and B.B., an undergraduate student) received thorough education on workup and diagnosis of hyperparathyroidism from a fellowship trained endocrine surgeon (C.J.B.) prior to the beginning of data collection. Competence and ability to adequately collect information from the chart were confirmed and periodically reassessed to ensure quality and accuracy of data collection. For each chart, the 2 reviewers analyzed clinic notes, diagnostic data, and communications within the medical record beginning at the first elevated calcium for each patient to create a chronological narrative description of the decisions and events related to the diagnosis and treatment of hyperparathyroidism.
Although all the patients in our cohort were eventually diagnosed with hyperparathyroidism and half were referred for treatment, we wanted to investigate whether there were missed opportunities for earlier diagnosis and treatment that could potentially improve outcomes for patients. To do this, each narrative was constructed using a template established prior to data collection that contained a list of actions or decisions (shown in Tables 2 and 3) that could have led to earlier diagnosis of hyperparathyroidism (missed opportunities for diagnosis) or earlier surgical referral (missed opportunities for surgical referral). The different events that were recorded were defined as follows:
Table 2.
Frequency of missed opportunities for diagnosis of hyperparathyroidism.
| Event | Overall (N = 50) | Not referred (N = 25) | Referred (N = 25) | P value |
|---|---|---|---|---|
| Elevated calcium not acknowledged | 29 (58%) | 17 (68%) | 12 (48%) | .15 |
| New doctor misses Abnormal calcium | 8 (16%) | 5 (20%) | 3 (12%) | .44 |
| Abnormal calcium noted but not evaluated | 6 (12%) | 2 (8%) | 4 (16%) | .38 |
| Inadequate workup | 15 (30%) | 8 (32%) | 7 (28%) | .76 |
| Parathyroid hormone high but no diagnosis | 14 (28%) | 11 (44%) | 3 (12%) | .14 |
| Evaluation of hypercalcemia planned but not done | 4 (8%) | 3 (12%) | 1 (4%) | .29 |
| Hypercalcemia attributed to other cause | 22 (44%) | 11 (44%) | 11 (44%) | 1 |
| Symptoms of hyperparathyroidism present but diagnosis not considered | 8 (16%) | 4 (16%) | 4 (16%) | 1 |
Table 3.
Frequency of missed opportunities for referral to a surgeon to discuss treatment.
| Event | Overall (N = 50) | Not referred (N = 25) | Referred (N = 25) | P value |
|---|---|---|---|---|
| Physician mentions no benefit to surgery | 21 (42%) | 11 (44%) | 10 (40%) | .77 |
| Decision for medical management | 11 (22%) | 7 (28%) | 4 (16%) | .3 |
| Decision to observe | 13 (26%) | 6 (24%) | 7 (28%) | .75 |
| Concerns over age | 7 (14%) | 5 (20%) | 2 (8%) | .22 |
| Concerns over comorbidity | 10 (20%) | 7 (28%) | 3 (12%) | .15 |
| “Mild or asymptomatic” disease | 7 (14%) | 3 (12%) | 4 (16%) | .68 |
| “Mild or stable hypercalcemia” | 7 (14%) | 4 (16%) | 3 (12%) | .68 |
| NIH criteria mentioned | 2 (4%) | 1 (4%) | 1 (4%) | 1 |
| Surgery not mentioned as treatment option | 10 (40%) | |||
| Patient chooses not to see surgeon | 4 (16%) | |||
| Health change does not prompt reconsideration of treatment | 18 (36%) | 10 (40%) | 8 (32%) | .56 |
| Surgeon feels patient would not benefit from surgery | 3 (12%) | |||
| Concern about surgical risk | 0 | |||
| Concern about age | 1 (4%) | |||
| Concern about comorbidity | 3 (12%) | |||
| Mild symptoms only | 0 | |||
| Mild hypercalcemia | 0 | |||
| Parathyroid hormone not high enough | 1 (4%) | |||
| NIH criteria | 1 (4%) |
Abbreviation: NIH, National Institutes of Health.
Elevated calcium not acknowledged. If the patient had hypercalcemia on any lab work performed, but there was no mention of the abnormal result in any clinic notes or communications with the patient.
New doctor misses abnormal calcium. If the patient’s care was transferred to a new physician after having hypercalcemia on recent lab work, but the new physician does not acknowledge that abnormality.
Abnormal calcium noted but not evaluated. If hypercalcemia is acknowledged in a clinic note or communication with the patient, but no workup of the abnormality is planned or performed.
PTH high but no diagnosis. If the patient had hypercalcemia and an elevated PTH on further workup, but no diagnosis of hyperparathyroidism is mentioned in the note or communicated to the patient.
Evaluation of hypercalcemia planned but not done. If the physician discussed a plan for further workup of the patient’s hypercalcemia, but nothing was performed.
Hypercalcemia attributed to other cause. If the patient’s hypercalcemia was attributed to another cause without any further workup.
Symptoms of hyperparathyroidism but no diagnosis. If the patient had hypercalcemia along with symptoms that can be attributed to hyperparathyroidism, but no consideration of hyperparathyroidism is mentioned.
Physician mentions no benefit to surgery. If the physician states that the patient would not benefit from surgery. For each occurrence, it was documented whether the physician listed a reason that the patient would not benefit from surgery. In addition, it was also documented whether the physician chose to pursue observation or medical management.
Surgery not mentioned as a treatment option. If the physician diagnoses the patient with hyperparathyroidism but makes no mention of surgery as a treatment option.
Patient chooses not to see surgeon. If it is noted that the patient has decided not to see a surgeon or pursue surgical management.
Health change does not prompt reconsideration of treatment. If the patient was diagnosed with hyperparathyroidism and was currently being observed or managed medically and then develops any complications attributable to hyperparathyroidism and there is no reconsideration of surgical treatment.
Surgeon feels patient would not benefit from surgery. If the patient is referred to a surgeon and the surgeon decides that the patient would not be a surgical candidate.
It is important to note that patients may fall into one or more of the categories noted above if decisions in management change over time. For example, a physician may have initially decided to only observe a patient diagnosed with hyperparathyroidism and then later chose to start medical therapy.
To guarantee the quality of data collection, the 2 reviewers analyzed the first 5 charts together at the same computer to ensure consistency of approach and narrative construction. Both reviewers then analyzed the next 5 charts at separate computers and compared narrative descriptions. Conflicts over data collected were resolved by consensus in meetings with another author (C.J.B.). The remaining 40 charts were reviewed in a series, with each reviewer analyzing 4 separate charts separately and then analyzing and comparing a fifth chart together to make sure that data were being collected consistently by both reviewers. The coding template was revised to include new information after the initial 5 charts were analyzed and was revised iteratively throughout the process of data collection until thematic saturation was achieved. The frequency of the different events resulting in underdiagnosis and underreferral was categorized into 2 ways. First, the total number of distinct clinical encounters where a specific event occurred was determined for each patient over the time followed at UAB. To calculate this number, we counted the total number of visits that occurred from the time of the initial event until it was corrected. For example, if hypercalcemia was attributed to a cause other than hyperparathyroidism during a visit with the primary care physician, then each visit after that was counted as a distinct clinical encounter until the physician acknowledged that the high calcium was due to hyperparathyroidism. Second, we determined how many patients experienced each cause of underdiagnosis or undertreatment.
Statistical analysis
Categorical variables were compared using the likelihood ratio χ2, and continuous variables were compared using the Wilcoxon rank sum test. All analyses were done with Stata (StataCorp 2017; Stata Statistical Software: Release 15; StataCorp LLC, College Station, TX, USA).
Results
Patient characteristics
The median age of our cohort was 84 (80-96) years, 90% were women, and 60% were white (Table 1). The uneven sex distribution of our cohort is expected as the prevalence of hyperparathyroidism is significantly higher in women (estimated to be as much as 5-fold higher in patients 80 years or older).1,2 Most of the patients had Medicare (60%), whereas 40% had commercial/private insurance. The median number of comorbidities was 2 (range 0-10) and the median duration of follow-up for the cohort was 5.5 years (range 1-13). Next, we compared the characteristics of patients who were referred to a surgeon and those who were not referred. Age, index calcium, index PTH level, race, comorbidities, and follow-up time were similar between the group that was referred to a surgeon and the group that was not referred. There was a higher percentage of women in the group that was not referred to surgery (92%) compared with 68% in the group that was referred to surgery (P = .03; Table 1).
Table 1.
Patient demographics for the entire cohort and comparison of patients referred to surgeons vs not referred.
| Demographic | Overall (N = 50) | Not referred to surgeon (N = 25) | Referred to surgeon (N = 25) | P value |
|---|---|---|---|---|
| Age, y | 84 (80–96) | 84 (80–96) | 82 (80-90) | .1 |
| Index calcium, mg/dL | 10.9 (10.6–12.7) | 10.8 (10.6–11.8) | 10.9 (10.6-12.7) | .98 |
| Index parathyroid hormone level, pg/mL | 132.8 (70–595) | 155 (75–525) | 126 (70-595) | .37 |
| Gender | .03 | |||
| Male | 10 (20%) | 2 (8%) | 8 (32%) | |
| Female | 40 (80%) | 23 (92%) | 17 (68%) | |
| Race/ethnicity | .25 | |||
| African American | 20 (40%) | 12 (48%) | 8 (32%) | |
| White | 30 (60%) | 13 (52%) | 17 (68%) | |
| No. of Elixhauser comorbidities | .76 | |||
| 0 | 17 (34%) | 10 (40%) | 7 (28%) | |
| 1 | 8 (16%) | 3 (12%) | 5 (20%) | |
| 2 | 4 (8%) | 2 (8%) | 2 (8%) | |
| 3 | 7 (14%) | 3 (12%) | 4 (16%) | |
| 4+ | 14 (28%) | 7 (28%) | 7 (28%) | |
| Kidney stones | 2 (4%) | 1 (4%) | 1 (4%) | 1 |
| Fractures | 2 (4%) | 1 (4%) | 1(4%) | 1 |
| Osteoporosis | 10 (20%) | 5 (20%) | 5 (20%) | 1 |
| Follow-up, y | 5.5 (1–17) | 6 (1–17) | 5 (1–13) | .39 |
| Time interval from first hypercalcemia to seeing a surgeon, mo | 41 (0–123) | |||
Values represent either number and % or median and range.
Reasons for delay in diagnosis of hyperparathyroidism
All 50 patients in the cohort were eventually diagnosed with hyperparathyroidism by a physician. About 58% of all patients had at least an elevated calcium that was not commented on in the medical record and was not further evaluated at the following visits (Table 2). These patients had 257 visits with their physicians after the initial high calcium in which there was no evidence that hypercalcemia was recognized for that further workup was planned. When hypercalcemia was noted, it was attributed to other causes in 44% of patients. These other causes included calcium supplementation (18% of patients), diuretic use (12%), dehydration (10%), cancer (2%), renal dysfunction (10%), and vitamin D deficiency (16%). In addition, 28% of patients had both an elevated calcium and PTH, yet were not immediately diagnosed with hyperparathyroidism. Also, 16% of patients had symptoms and sequelae which may be attributable to hyperparathyroidism (fractures, kidney stones, or osteoporosis) along with hypercalcemia, yet the diagnosis was still missed.
Hypercalcemia was often evaluated with a workup that was inadequate to make a correct diagnosis, as 30% of patients had their serum calcium rechecked without ordering a PTH and/or vitamin D level. This led to 24 separate clinic appointments where there was insufficient information to make a diagnosis of hyperparathyroidism. Additional reasons for delays in diagnosis included failure of a new physician to recognize a prior episode of hypercalcemia following transfer of care (16% of patients), hypercalcemia being noted but not further evaluated (12%), or the workup of hypercalcemia being planned but never completed (8%). We compared the frequency of missed opportunities for diagnosis between the group that was referred and the group that was not referred and found that there were no significant differences (Table 2).
Reasons for delay in referral to surgeon for parathyroidectomy
For 42% of patients, a nonsurgeon documented at least one discussion suggesting that surgery would not be beneficial (Table 3). Reasons given for not pursuing surgical treatment included patient age (14%), concerns over comorbidities (20%), belief that the patient has “mild/asymptomatic disease” (14%), or “mild/stable” hypercalcemia (14%). In addition, the physician mentioned National Institutes of Health (NIH) consensus criteria as a reason for nonoperative management in 4% of cases. Among these patients, the decision for medical management with calcium-reducing agents was made for 22% of patients and the decision to observe and monitor calcium levels was made for 26% patients. Even after patients develop worsening symptoms of hyperparathyroidism (new fractures or kidney stones, worsening osteoporosis, or a rise in serum calcium greater than 1 mg/dL), physicians frequently fail to reconsider the benefits of surgical referral. One-third of the patients (36%) experienced one of these changes in disease progression, but their physicians did not reconsider the choice of nonsurgical management. Furthermore, for the group that was not referred to a surgeon, surgery was never mentioned as a treatment option for 40% of patients. We also found that there was no significant difference in the frequency of individual missed opportunities for referral to a surgeon between the group that was referred and the group that was not referred (Table 3).
The median time interval from the first elevated serum calcium to the patient being seen by a surgeon was 41 months. Patients who were not referred to a surgeon for parathyroidectomy have had their disease untreated for a median of 6 (1-17) years. Of the 25 patients who were referred to a surgeon, only 1 patient did not follow-up and 4 stated that they did not want to have surgery. Among the referral group, only 3 (12%) were deemed not surgical candidates by a surgeon due to comorbidities (3 patients) or age (1 patient).
Discussion
Our article represents an important contribution to the literature on hyperparathyroidism because it outlines the key reasons for underdiagnosis and undertreatment among older patients. Understanding the barriers to diagnosis and surgical referral is a necessary step toward designing interventions to ensure that older patients are treated in a timely fashion that optimizes quality of life by minimizing exposure to disease-related morbidity. We found that hypercalcemia on routine laboratory evaluation (the most common presentation of hyperparathyroidism) is frequently overlooked, inadequately evaluated, and often attributed to causes other than hyperparathyroidism. We also demonstrated that older patients are not being referred to surgeons because primary care providers and other nonsurgeons believe that patients will not benefit from surgery and overestimate the risks related to age and other comorbidities. Physicians also frequently fail to reconsider their initial decision about treatment even when a patient’s clinical status worsens as a result of untreated hyperparathyroidism. The end result is significant delays in diagnosis and treatment, with a median time of nearly 4 years from first elevated serum calcium to being seen by a surgeon for those who underwent surgery. Notably, the rates of missed opportunities for diagnosis and referral are similar between older patients who eventually reach a surgeon and those who do not. This finding suggests that the primary driver of diagnosis and referral is not patient characteristics but is due to poor systems of care related to identifying and treating patients in a timely fashion.
The failure of care systems to diagnose and treat hyperparathyroidism can potentially have a large impact on older patients. Untreated hyperparathyroidism increases the risk of multiple adverse outcomes including fractures (75% increase), cardiovascular disease (2.5-fold), kidney stones (5-fold), renal failure (14-fold), and mortality (40% increase).13 Surgical treatment of hyperparathyroidism substantially improves quality of life and is more cost-effective than medical management.5,14 Fractures can result in permanent mobility impairments, nursing home dependence, and death. Kidney stones can cause intense pain and may lead to sepsis, delirium, and loss of renal function with a need for dialysis. These complications could be greatly reduced by early diagnosis and treatment of hyperparathyroidism.
Our study expands on previous work that establishes the prevalence of underdiagnosis and undertreatment of hyperparathyroidism. Our most recent study used administrative data from the UAB to determine the prevalence of undiagnosed and untreated hyperparathyroidism.9 In this group of 10 432 patients with hypercalcemia, only 31% had PTH evaluated and only 22% of the patients with classic hyperparathyroidism were referred to surgeons to discuss treatment.9 During that study, we found that older patients aged 75 years and older had a decreased chance of being referred for surgery.9 Press et al10 reviewed medical records from the Cleveland Clinic and estimated that 43% of patients with hypercalcemia were likely to have hyperparathyroidism, yet only 24% had a PTH evaluated and only 1.3% received a diagnosis of hyperparathyroidism. Recent work by Sharata et al12 surveyed primary care providers and found that the majority are not familiar with criteria for surgical intervention and that only 37% are familiar with a focused parathyroidectomy as a treatment option. This further illustrates the need for intervention at the health care provider level to better prepare physicians and health systems to care for patients with hyperparathyroidism. Wu et al11 used administrative data from Kaiser Permanente in California to examine the use of parathyroidectomy in an elderly population and determined that the likelihood of undergoing parathyroidectomy decreases with age when adjusting for other patient factors. This study highlights the difficulties faced by the elderly population when it comes to treatment of hyperparathyroidism. Our work adds to these studies by identifying the specific barriers that must be overcome to enhance rates of diagnosis and treatment.
Although our project is designed to elucidate potential barriers to diagnosis and treatment of hyperparathyroidism, there are several limitations that should be acknowledged. First, the sample of 50 patients from our institution may not be broadly representative of all patients with hyperparathyroidism and their evaluation in other health systems. However, the project was designed to be an initial exploration of barriers that could guide subsequent work, and the reasons for underdiagnosis and underreferral are fairly comprehensive and have reasonable face validity. Second, all information about care processes and decisions was obtained from electronic medical records and lack of mention in the chart does not necessarily imply lack of thought by the physician. Clinical documentation does provide a useful surrogate, however, and we took care to look for any orders or messages between providers that would indicate awareness of potential hyperparathyroidism and plans for workup or treatment that were not written in progress notes. We also identified multiple quotations from the medical record that are consistent with our hypotheses and highlighted these as part of the project (Table 4).
Table 4.
Select representative quotations from the medical record.
| Category | Quote |
|---|---|
| Elevated calcium not acknowledged | “all tests look good.” (calcium was 10.8); “shows no electrolyte abnormalities” (calcium was 11.7 mg/dL) |
| Parathyroid hormone high but no diagnosis | “Her PTH level was 168 and her vitamin D level was 49. We will make no changes” |
| Elevated Ca or PTH attributed to other cause | |
| Lab error | “I don’t trust our calcium levels right now at UAB and have been meeting with the lab. Ill follow up, thanks” |
| Cancer | “Monitor calcium and PTH to see if they normalize with chemoradiation” |
| Renal dysfunction | “Mild hypercalcemia in the setting of renal dysfunction. Because it is very mild I would elect to observe this for now, though there is some chance it could indicate systemic abnormalities” |
| Doctor feels patient would not benefit from surgery | |
| Decision for medical management | “will monitor hyperparathyroidism for now. Surgery does not seem to be an ideal option for now, bone protection with osteoporosis treatment. Follow calcium levels” |
| Decision for observation | “calcium 10.9 with elevated PTH, likely primary hyperparathyroidism. With the patient’s age and comorbidities I don’t feel that we need to pursue further evaluation” |
| Concern for surgical risk | “It is reasonable to treat her hypercalcemia medically with cinacalcet to prevent kidney stones and bone loss, especially since she is prone to dehydration given her poor PO intake. She is not a good surgical candidate given her advanced age and multiple comorbidities” |
| Concern for old age | “I did discuss with her daughter that the impaired renal function was technically an indication for parathyroid surgery . . . I did not feel compelled at her age to necessarily suggest that at this point” |
| Concern for comorbidities | “Based on her advanced dementia, surgical therapy for this would be unwise” |
| Change in health status does not prompt reconsideration of surgical treatment with patient | “interestingly she has many calcium oxalate crystals in her urine” but did not reconsider management plan |
The next step toward intervention design is to validate our findings from the medical record using qualitative techniques such as semi-structured interviews or focus groups with primary care providers and patients. Qualitative methods will allow us to further explore potential barriers and facilitators to diagnosis. A mixed-methods approach that combines our current quantitative work with qualitative data will allow us to formulate a robust model for designing interventions that increase rates of diagnosis and referral.
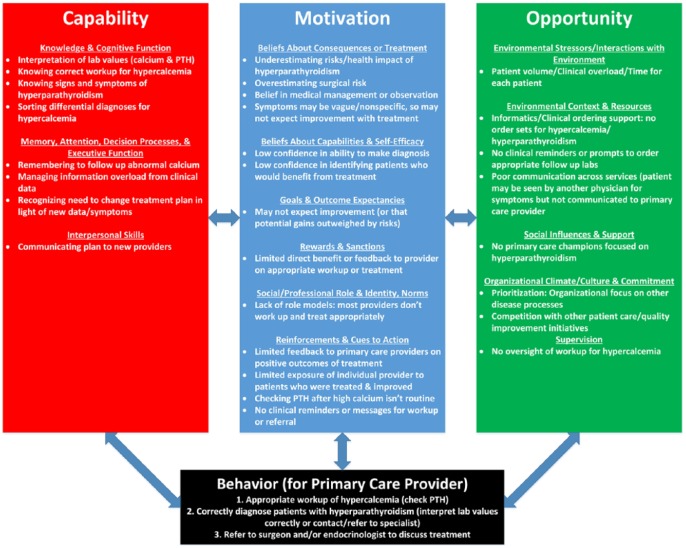
We have combined our current work with existing literature and conversations with expert endocrine surgeons to develop a conceptual model that will facilitate intervention design. Our approach is based on the Capability, Opportunity, Motivation, and Behavior model (COM-B), which was developed for design, evaluation, and implementation of clinical interventions.15 The model, shown in Figure 1, assesses how capability, opportunity, and motivation of providers can interact to affect behavior (diagnosis and treatment of hyperparathyroidism). The model allows us to categorize how physician knowledge and decision making interact with treatment risks/benefits and environmental factors that affect the desired behavior. The domains of the COM-B model can be used to guide questions for interviews and assist with coding and interpretation of the data. In addition, each content domain of the model can be paired with a behavior change technique when designing a clinical intervention. This ensures that intervention design is systematic and optimizes the chances of successful implementation.
Figure 1.
Conceptual model for understanding the reasons for delay in diagnosis or referral for hyperparathyroidism by primary care providers.
Improvements in the process of care for hyperparathyroidism will require both system-level changes and stakeholder engagement. Efforts to educate primary care providers on detecting primary hyperparathyroidism will likely be necessary to increase the likelihood of timely diagnosis. In addition, delivering accurate information about the benefits and safety of parathyroidectomy may increase provider motivation to refer patients for surgery. Similarly, educating patients about hyperparathyroidism can help them make informed decisions about treatment. Furthermore, system-level interventions to automate the detection of hypercalcemia and evaluation of PTH along with prompts to discuss treatment with a surgeon can increase opportunity and improve the efficiency of diagnosis treatment.
In conclusion, older patients with hyperparathyroidism are often undiagnosed and untreated because physicians miss hypercalcemia on routine labs, do not consider the diagnosis, and fail to make the appropriate referral for treatment. Although not all older patients with hyperparathyroidism will ultimately undergo parathyroidectomy, it is important that they have the opportunity to discuss surgery with an expert who can offer a reasonable estimation of risks and benefits. Ultimately, an endocrine surgeon is the best person to have this conversation with the patient as the surgeon has the greatest understanding of operative risks and has the most experience with the benefits related to surgery. Recent changes to treatment guidelines reflect a recognition of this fact and encourage all patients to at least have an expert discussion about potential benefits and risks of treatment.8 Interventions to accelerate diagnosis and referral of hyperparathyroidism can potentially improve quality of life and reduce overall health care costs by reducing the risk of complications from the disease. Our project is a useful step toward this goal.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number TL1TR001418 for A.D. and by an AHRQ K12–mentored career development award (HS023009-03) for C.J.B. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All authors made substantial contributions to study conception and design, interpretation of data, drafting and revising the article, and approval of the final draft. AD, BB, and RX were responsible for data collection. CJB was primarily responsible for analysis.
References
- 1. Yeh MW, Ituarte PH, Zhou HC, et al. Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab. 2013;98:1122–1129. doi: 10.1210/jc.2012-4022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fraser WD. Hyperparathyroidism. Lancet. 2009;374:145–158. doi: 10.1016/S0140-6736(09)60507-9. [DOI] [PubMed] [Google Scholar]
- 3. Madkhali T, Alhefdhi A, Chen H, Elfenbein D. Primary hyperparathyroidism. Ulus Cerrahi Derg. 2016;32:58–66. doi: 10.5152/UCD.2015.3032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Coker LH, Rorie K, Cantley L, et al. Primary hyperparathyroidism, cognition, and health-related quality of life. Ann Surg. 2005;242:642–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brito K, Edirimanne S, Eslick GD. The extent of improvement of health-related quality of life as assessed by the SF36 and Paseika scales after parathyroidectomy in patients with primary hyperparathyroidism—a systematic review and meta-analysis. Int J Surg. 2015;13:245–249. doi: 10.1016/j.ijsu.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 6. Aliabadi-Wahle S, Kelly TL, Rozenfeld Y, et al. Treatment strategies for primary hyperparathyroidism: what is the cost? Am Surg. 2014;80:1146–1151. [PubMed] [Google Scholar]
- 7. Stechman MJ, Weisters M, Gleeson FV, Sadler GP, Mihai R. Parathyroidectomy is safe and improves symptoms in elderly patients with primary hyperparathyroidism (PHPT). Clin Endocrinol (Oxf). 2009;71:787–791. doi: 10.1111/j.1365-2265.2009.03540.x. [DOI] [PubMed] [Google Scholar]
- 8. Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons Guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. 2016;151:959–968. doi: 10.1001/jamasurg.2016.2310. [DOI] [PubMed] [Google Scholar]
- 9. Balentine CJ, Xie R, Kirklin JK, Chen H. Failure to diagnose hyperparathyroidism in 10,432 patients with hypercalcemia: opportunities for system-level intervention to increase surgical referrals and cure. Ann Surg. 2017;266:632–640. doi: 10.1097/SLA.0000000000002370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Press DM, Siperstein AE, Berber E, et al. The prevalence of undiagnosed and unrecognized primary hyperparathyroidism: a population-based analysis from the electronic medical record. Surgery. 2013;154:1232–1237, discussion 1237–1238. [DOI] [PubMed] [Google Scholar]
- 11. Wu B, Haigh PI, Hwang R, et al. Underutilization of parathyroidectomy in elderly patients with primary hyperparathyroidism. J Clin Endocrinol Metab. 2010;95:4324–4330. doi: 10.1210/jc.2009-2819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sharata A, Kelly TL, Rozenfeld Y, et al. Management of primary hyperparathyroidism: can we do better? Am Surg. 2017;83:64–70. [PubMed] [Google Scholar]
- 13. Yu N, Donnan PT, Leese GP. A record linkage study of outcomes in patients with mild primary hyperparathyroidism: the Parathyroid Epidemiology and Audit Research Study (PEARS). Clin Endocrinol (Oxf). 2011;75:169–176. doi: 10.1111/j.1365-2265.2010.03958.x. [DOI] [PubMed] [Google Scholar]
- 14. Zanocco KA, Wu JX, Yeh MW. Parathyroidectomy for asymptomatic primary hyperparathyroidism: a revised cost-effectiveness analysis incorporating fracture risk reduction. Surgery. 2017;161:16–24. doi: 10.1016/j.surg.2016.06.062. [DOI] [PubMed] [Google Scholar]
- 15. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]