Abstract
By 2015, diabetes has affected more than 415 million people over the world. It is anticipated that 640 million adults will suffer from diabetes in 2040. The elongation of the life expectancy, as the result of better general health care, extends also the time when diabetic complications may develop together with other senility-specific problems. The Giant Geriatric Syndromes (Geriatric Giants) have been qualified by the original Nascher’s criteria defined more than 100 years ago, but they are becoming more and more relevant in connection with the aging of societies. The criteria comprise the older age, commonness of the health problem, multifactorial etiology, functional or cognitive impairment, worsened outcome, and increased morbidity and mortality. We described the impact of diabetes on Geriatric Giants including cognitive dysfunction, depression, malnutrition, incontinence, falls and fractures, chronic pain, and the loss of senses. The association of diabetes with Geriatric Giants reveals as a vicious circle with the background of neurovascular complications. However, diabetes influence on the incidence of cancer in elderly was also discussed, since neoplastic diseases associate with Geriatric Giants, for example, chronic pain and depression. The knowledge about these aspects of functional decline in geriatric population is crucial to improve patient care.
Keywords: diabetes complications, elderly, hypoglycemia, fall and fractures, dementia and depression, cancer, malnutrition, incontinence, geriatric syndromes, Geriatric Giants
Introduction
The diabetes prevalence is rapidly increasing as a civilization disease, which results from improper nutritional habits, low physical activity, and obesity, however, triggered on the background of some genetic predispositions. According to the statistics of American Diabetes Association (ADA) from 2012, 29.1 million Americans (9.3% population) have suffered from diabetes, including 8.1 million of undiagnosed patients. The prevalence of diabetes in senior Americans, age 65 and older, remains high at the level of 25.9%, what equals to 11.8 million elderly people, comprising diagnosed and undiagnosed cases. The International Diabetes Federation informs that the diabetes affects 415 million adults by 2015, but by 2040, this will rise to approximately 640 million over the world (International Diabetes Federation, 2017; National Diabetes Statistics Report, 2017).
The diabetes in elderly patients concerns almost type 2 diabetes; only 5% to 10% of people with diabetes have the type 1 of the disease (Caspersen, Thomas, Boseman, Beckles, & Albright, 2012). The diabetic patients in Europe count about 60 million people. Annual diabetes mortality equals 3.4 million people, and almost 80% of these deaths occur in low and middle income countries, with more than half of those concerning age over 70 years (“Data and Statistics,” 2018).
Despite this tremendous statistics, a lot of studies on diabetes treatment exclude patients older than 65 years. Practically, all of them disregard patients older than 75 years and only a small fraction targets elderly people (Avorn, 1995; Lakey et al., 2013; Piątkiewicz et al., 2014). There are stipulations driven by demographic changes to remove the upper age limit for clinical trials, from 65 years to no restrictions (Shenoy & Harugeri, 2015). This is particularly desirable, as the elderly with diabetes are especially burdened, which deteriorates their prognosis and consumes a lot of health care resources.
The specific impact of diabetes on deterioration of Geriatric Giants should be widely known to provide adequate interventions and support more comprehensive prevention in the long-term perspectives.
Methodology of Evidence Collection and Assessment
This literature review was based on the key concept: diabetes—impaired functioning of elderly. The relevant issues were basically searched in PubMed and GoogleScolar after a preliminary search with Google engine, for the combination of main terms: diabetes/diabetic AND elderly/geriatrics/complications /hypoglycemia/hyperglycemia/ cancer/depression/dementia/pain/fractures/ frailty/falls risk/ sarcopenia/ urinary/incontinence/ vision loss/gait instability/ dizziness/complication /geriatric/giants. Where it was relevant, the study group size and age structure were specified for better assessment of the quality and meaning of the results.
Difficulties With Glycemia Control Increase With Age
The quality of glucose control during the younger age projects on older age and determines farther extent of neurovascular complications. The diabetes history varies among elderly, including those with long-term cases, early onset disease, or recently diagnosed but lasting a long time. The prevention of the diabetes complications comprises past treatment quality and current metabolic alignment. This may swing between hyperglycemia and hypoglycemia incidents. According to the recommendation of Polish Diabetes Association (PTD), ADA therapeutic targets vary depending on clinical status and compliance, the actual presence of macroangiopathic damages, the diabetes duration time, and life expectancy (ADA, 2017; Diabetology, 2018).
The glycemia self-management becomes really troublesome with decline of cognitive function and memory loss. Type 2 diabetes is an established risk factor for dementia, and the prevalence of those two diseases increases with age. Although the association between diabetes and vascular dementia is demonstrated and strengthened in the studies with phosphodiesterase 3 (PDE-3) inhibitor on animal model, the links of diabetes and neurodegenerative diseases are also supposed, particularly in the case of tau-pathology (Kwon et al., 2015; Sutherland, Lim, Srikanth, & Bruce, 2017). It has been found in the study including 8,888 participants aged 50+, Health and Retirement Study, that high glycosylated hemoglobin (HbA1c) was associated with a 10% faster rate of memory decline (β = −0.04 per decade; 95% confidence interval [CI] = [−0.06, −0.01]). It has been also reported that higher HbA1c was associated with memory decline (β = −0.05 per decade; 95% CI = [−0.08, −0.03]) in patients with HbA1c < 6.5% (threshold for diabetes), although, yet, not meeting the criteria for diabetes (Marden, Mayeda, Tchetgen Tchetgen, Kawachi, & Glymour, 2017).
However, according to recommendations cited above, the cognitive impairment or coexisting diseases allow to loosen the HbA1c criteria with the upper limit of 8.0% or even higher (8.5%). It is especially valid if end-stage chronic diseases coexist and when the benefits of strict glycemic control do not extend the life expectancy or are directly opposed by the increased risk of hypoglycemia.
Besides long-term hyperglycemia, the short incidents of severe hypoglycemia are causative factors for cardiovascular events and neurological damages, including death. This is more common in type 1 diabetes, although their occurrence in type 2 diabetes is also serious (McCoy et al., 2012).
The prevention of recurrent hypoglycemia becomes a priority in elderly. Hypoglycemia incidence in patients with long-term diabetes increases and it is strongly associated with glucose-level variability (Weinstock et al., 2013). A case control study including 18 diabetes centers in the T1D Exchange Clinic Network with participants 60 years or older with type 1 diabetes for longer than 20 years reveals such a dependence. Case subjects (n = 101) with at least one severe hypoglycemic event in the prior 12 months have greater glucose variability (p = .008) and experienced glucose levels lower than 60 mg/dL for longer than 20 min on 46% of days compared with 33% of days in control subjects which had no hypoglycemia in the prior 3 years (p = .1). The unawareness of hypoglycemia was observed more frequently in the case subjects. Only the 11% of case subjects, compared with 43% of controls, reported progenitor symptoms of the low glucose level. Moreover, the case subjects revealed worse cognitive status than controls (Weinstock et al., 2015).
Furthermore, significantly increased risk of nocturnal hypoglycemia was observed in the elderly with a newly diagnosed type 2 diabetes. The older patients had lower glucose concentrations from 2:00 a.m. to 7:00 a.m., compared with the younger controls. Surprisingly, in the older patient group, a potential risk of hypoglycemia after continuous subcutaneous insulin infusion therapy, especially during 11:00 p.m. to 4:00 a.m. and 4:00 a.m. to 6:00 a.m., has revealed in the males subgroup (F. Li et al., 2017).
Comprehensive geriatric assessment should be performed to determine safe therapeutic goals, especially in case of patients with cognitive impairment for whom self-management becomes difficult or impossible.
Diabetic Complications as a Trigger for Giant Geriatric Syndromes (Geriatric Giant)
The recognition of Geriatric Giant makes geriatric medicine far more comprehensive than usual internal medicine of the adults, embracing the connection of health status and overall functionality of older patients burdened with comorbidities and dependent on others. The term, which is 104 years old, becomes more and more current with the aging of societies. The health problem to qualify as a Geriatric Giant has to meet recognized criteria originally described by Nascher (“Geriatrics: The Diseases of Old Age and Their Treatment,” 1914).
It includes the age and the commonness of the considered health problem, multifactorial etiology, functional or cognitive impairment, worse outcome, and increased morbidity and mortality. The diabetes inevitably contributes to meet those criteria. The dysregulation of glycemia translates into neuropathy at the sensory, autonomic, and motor nerves level.
Macroangiopathy affects cardiovascular, central, and peripheral nervous system and vasculatory of extremities. In patients with diabetes, incidence of cardiovascular disease is from two- to eightfold higher compared with the general population, and it is the leading cause of death (Bohn et al., 2016). Microangiopathy reveals especially in kidney and retina, but vascular complications affect also other organs (see below). Diabetes boosts progression of the decline of cognitive functions and drastically increases the risk of stroke, which abruptly deteriorates functionality (Groeneveld, Kappelle, & Biessels, 2015).
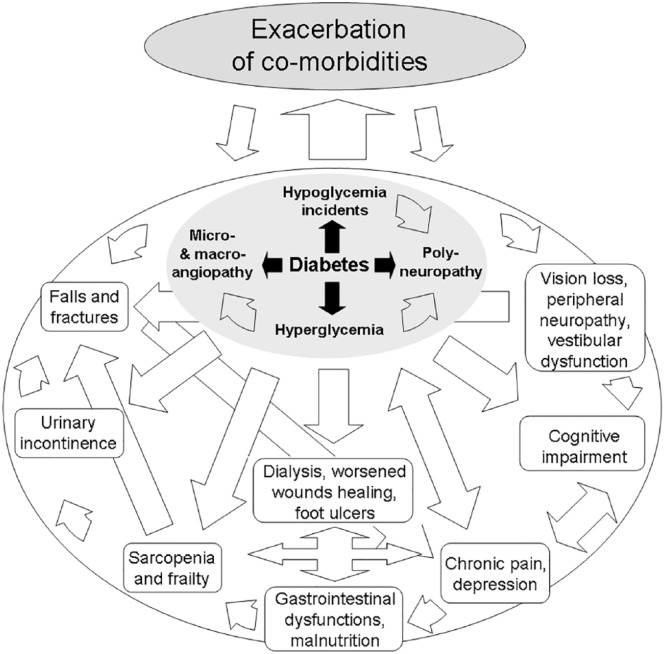
It was also found that diabetes moderately increases the risk of such geriatric syndromes as falls or delirium, with an average odds ratio [OR] of 2.0 for two comorbidities (Vetrano et al., 2016). The bidirectional relationships between diabetic complications, difficulties with glycemia control, and comorbidities exacerbate geriatric problems by the mechanism of vicious cycles (Figure 1).
Figure 1.
The complex relations between geriatric syndromes, diabetes complications, and comorbidities.
Note. The position on the diagram does not prejudge the importance of the health problems mutually dependent on each other.
The Impact of Diabetes on Health and Functionality – Wider Than is Usually Thought: Gastrointestinal Complications and Malnutrition
It is commonly known that diabetes affects kidneys and increases the risk of death from cardiovascular reasons (Subramanian et al., 2017); however, the disease also deteriorates function of other organs. Gastrointestinal disorders exacerbated by diabetes include oral candidiasis, gastroparesis, nonalcoholic fatty liver disease, gastroesophageal reflux, dysphagia, and chronic diarrhea. Symptoms of gastroparesis include early satiety, postprandial fullness, nausea, vomiting of undigested food, bloating, and abdominal pain (Martinez, Jaimes-Aveldañez, Hernández-Pérez, Arenas, & Miguel, 2013; Tau & Arevalo Santana, 2017).
Small intestinal and colorectal dysfunctions are common in patients with long diabetes history. Constipation altering with painless diarrhea or even fecal incontinence, especially in patients with diabetic enteropathy, particularly deteriorates quality of life (Krishnan, 2013).
It should be highlighted that decline of the secretory function of pancreas comprises insufficiency of not only endocrine excretion of insulin but also exocrine dysfunction, especially in type 2 diabetes with poor glycemic control (Terzin et al., 2014).
All of above mechanisms contribute to digestive inefficiency and undernourishment in elderly. The protein-energy malnutrition exacerbating with diabetes impairs the immunity, which, for example, increases susceptibility to Mycobacterium tuberculosis, especially in resource-poor communities (Menon et al., 2016).
The nutritional studies have shown that a third of diabetic patients admitted at Spanish hospitals were malnourished, and malnutrition in diabetic patients causes longer hospitalizations in comparison with those at no nutritional risk (Miguel et al., 2015).
Diabetes, Sarcopenia, Frailty and Falls, Polypharmacy and Delirium, Wound and Fractures Healing, Peri- and Postoperative Risk, and Glycemic Control
Malnutrition leads to the loss of muscle mass and the loss of muscle strength and function, which characterizes sarcopenia (Vellas et al., 2018). It is interesting that sarcopenia associates with diabetes with the extent depending on diabetes type, suggesting autoimmune background of muscles loss in diabetes.
The higher prevalence of sarcopenia has been observed in LADA (Latent Autoimmune Diabetes in Adults) (35.0%) than in type 2 diabetes (13.3%) or control subjects (9.8%) in the study including LADA (N = 20), type 2 diabetes (N = 208), and control subjects (N = 41).
In a multivariate model including age and body mass index, LADA was more strongly associated with sarcopenia (OR = 9.57, 95% CI = [1.86, 49.27]), than type 2 diabetes, associated with moderate risk (OR = 2.99, 95% CI = [0.83, 10.80]) (Bouchi et al., 2017).
Sarcopenia contributes to frailty syndrome defined by the three conditions met from five, comprising weakness, slowness, low level of physical activity, exhaustion, and weight loss, according to original Fried criteria (Fried et al., 2001).
Diabetes was associated with increased risk of frailty with factors of 1.36 (95% CI = [1.18, 1.56]) and 1.56 (95% CI = [1.32, 1.85]) for prevalence and incidence, respectively, compared with non-diabetic controls in the large study including a baseline total of 10,039 subjects with a mean age of 70.51 (±7.82) and 6,293 older adults followed up at 12 months (Chhetri, Zheng, Xu, Ma, & Chan, 2017).
Decrease of the muscles mass and their complex function results in the posture imbalance, increased risk of falls, and life threatening fractures. In one study comprising 139 elderly (88 ± 7 years, range = 70-105 years), 49 participants experienced a fall over the follow-up period (M = 299 days). The incidence rate for the participants with and without diabetes mellitus was 78% and 30%, respectively (p < .001), with adjusted hazard ratio = 4.03 (95% CI = [1.96, 8.28]) (Maurer, Burcham, & Cheng, 2005). The multimorbidity, exacerbated with diabetes, results in polypharmacy, for example, benzodiazepines and “Z-drugs” abuse, and increases risk of delirium and recurrent falls (Richardson, Bennett, & Kenny, 2014).
The increased risk of falls in diabetes raises the rate of hip fractures, which drastically restrains precedent functionality and worsen prognosis. The elevated risk of low energy fractures results from the impact of diabetes on bone metabolism, however, in the manner depending on the type of diabetes. Impaired anabolism and decreased mineral density is observed in type 1 diabetes due to the lack of insulin. In case of the type 2 diabetes, the bone turnover is affected by insulin resistance and may have an impact on bone quality (Tonks, White, Center, Samocha-Bonet, & Greenfield, 2017).
The changed bone mineral turnover in diabetic kidney disease, concomitant parathyroidism, or adynamic bone disease, either in type 1 or type 2 diabetes, are also crucial determinants of increased bone fragility (Miller, 2014).
Furthermore, it was demonstrated that besides hyperglycemia, elevated tumor necrosis factor alpha (TNF-α) impairs healing of the fracture in diabetic patients, suggesting inflammatory background (Lim et al., 2017). The orthopedic surgery has also worse prognosis in the case of diabetes (Reátegui et al., 2017).
The proper glycemic control in perioperative period is the most important mean to reduce postoperative complications (Carpintero, 2014). It has been proved that only comprehensive and full care of elderly diabetic patients after hip fractures, combined with home glycemic control, can reduce the number of complications. The study reported the beneficial effect of lowering HbA1c level on the recovery process and the avoidance of adverse events (Reátegui et al., 2017).
Poor glycemic control is the cause of poor wound healing and infectious complications. It affects not only the wound itself but causes systemic effects. In addition, elderly people often have coexisting diseases and malnutrition with protein deficiency, which further aggravates prognosis (Carpintero, 2014).
Furthermore, the onset time of diabetes, level of glycated hemoglobin, smoking, peripheral neuropathy, peripheral vascular disease, limitation of mobility in joints, and trauma had a significant association with occurrence of diabetic foot and also worse healing. It has been shown that diabetic foot ulcers were more frequent in elderly males, and it is the serious cause of functional disablity (Nongmaithem et al., 2016).
Diabetes Associates With Depression Which Leads to Deteriorate Psychosocial Functioning
The type 1 and type 2 diabetes are associated with higher risk of depression, but on the other side, depression predisposes to type 2 diabetes. Diabetes and depression coincide around 2 times often than it would be predicted by chance alone (Holt, De Groot, & Golden, 2014).
These relationships are not fully understood. The depression influences the glycemic control, deteriorates nutritional habits, and causes overfeeding or, on the contrary, malnutrition. It leads to nonadherence to medication. Diabetes deteriorates health status and, in consequence, induces depression. Some data suggest that there is no direct association between glycated hemoglobin level, glycemic control, and depression (Asuzu, Walker, Williams, & Egede, 2017). Authors have supposed that the depressive symptoms or fatalism is directly related to the higher diabetes distress. These aspects are crucial for elderly patients, burdened with many risk factors of depression, including loneliness, low economic status, the end of professional life, and dependence from others.
Chronic Neuropathic Pain
The chronic neuropathic pain, which not treated properly, may associate with depression development. It was found that painful diabetic polyneuropathy was a greater determinant of depression than other diabetes-related complications and comorbidities (D’Amato et al., 2016). In the single-center study including 4,283 patients with diabetes, 65 years and older with mean age 73 ± 6 years, significant relationships were found between depression severity and chronic diabetic complications including retinopathy, symptoms related to peripheral polyneuropathy, autonomic neuropathy, and end-stage renal disease requiring dialysis, and quantified by the Patient Health Questionnaire–9 (PHQ-9) into three severity categories (Ishizawa et al., 2016).
Impact of Diabetes on Cancers in Elderly
The cancer diseases are distinctively inscribed in the epidemiology of older age. They often develop insidiously and are advanced in stage when newly diagnosed. Although the issue deserves a separate paper, we must mention about the impact of diabetes on cancer incidence and progression, which definitely affects functionality, relates to chronic pain and depression, and aggravates outcome.
The observed diabetes–cancer association is dependent on cancer type. Increased risk of twofold or higher has been shown for liver, pancreas, and endometrium cancers in case of type 2 diabetes. The moderate risk of 1.2- to 1.5-fold was observed for colon or rectum, breast, and bladder cancers, but no risk associated with diabetes has been found for lung cancer (Giovannucci et al., 2010).
More recent studies on a large cohort of 771,000 have shown that type 2 diabetes was associated with 26% increased risk of death from any cancer in Asian population. However, no significant association of diabetes has been found with the risk of death from leukemia and cancers of the bladder, cervix, esophagus, stomach, and lung (Chen et al., 2017).
On the contrary, it is known that diabetes is inversely correlated with and seems to protect against prostate cancer (Bansal, Bhansali, Kapil, Undela, & Tiwari, 2012).
It also should be emphasized that the use of antidiabetic drug as metformin can reduce the cancer risk. In the case of other glucose lowering drugs, data are conflicting; the diabetes–cancer link is confounded by many factors including diet, obesity, smoking, or physical activity (Shlomai, Neel, LeRoith, & Gallagher, 2016).
Diabetes Influence on Urinary Tract Problems Reduces Quality of Life
The urinary tract infections, as well as pneumonias, are often geriatric problems, which substantially decrease a life quality and predispose to other geriatric syndromes, including falls, mood disorders, and even delirium (Magny et al., 2018).
The urinary incontinence is one of the most troublesome problem, often leading to social withdrawal. The diabetes at all, together with hypertension, has revealed to be the main risk factor of urge urinary incontinence among women in the cohort study including 719 adult women aged 18 or older with prevalence of urinary incontinence of 50.3% (Demir, Sen, Irer, Bozkurt, & Esen, 2017). The study comprises the wide range of age; however, the elderly seems to contribute independent risk.
Furthermore, it has been demonstrated, in the study including 871 subjects with mean age 85.5 ± 5.2 years, all males, that urinary incontinence is a independent risk factor for recurrent falls (OR = 2.37, 95% CI = [1.45, 3.82], p < .001) (Hung et al., 2017).
The increased risk of urinary tract infection is one of the causes of urinary incontinence, but surprisingly, the disease prevalence in diabetic population was similar to that in patients without diabetes. It did not concern, however, the asymptomatic bacteriuria, the frequency of which was 2 to 3 times higher in diabetic patients (De Lastours & Foxman, 2014; Moore, Jackson, Boyko, Scholes, & Fihn, 2008).
An exception must be noted for genitourinary tract infections associated with use of sodium-glucose cotransporter-2 inhibitors (SGLT-2), which increase urinary glucose concentration. In this case, only prevalence of genital infections (not urinary tract infections) has been clearly increased and associated with poor glycemic control, although most of them were mild and easy to treat (Rizzi & Trevisan, 2016).
The diabetic cystopathy, usually developing in middle-aged or elderly patients with long-term diabetes, that poorly controlled glycemia is another complication from urinary tract (Golbidi & Laher, 2010). It comprises impairment of bladder sensation and contraction, increase in bladder capacity, and postvoiding volume. The pathophysiology of this disorder is multifactorial with involved polyneuropathy, accompanied by myogenic and urothelial changes (Powell, 2014).
The proper management of urinary tract disorders including overactive bladder, nocturia, urinary incontinence, and urinary tract infections may be preventive for falls and serious injuries (Soliman, Meyer, & Baum, 2016).
Furthermore, the diabetic kidney disease is a key microangiopathic complication, which drastically impairs functionality when it shifts to end-stage renal disease requiring renal replacement therapy. The burdensome disorder dramatically changes the course of life; imposes many psychosocial consequences including significantly increased prevalence of depression, than is 3 to 4 times higher compared to general population; and also leads to dementia (Shirazian et al., 2017).
The Vision Loss in the Crossway of Geriatric Syndromes
The essential imprint of diabetes is diabetic retinopathy, which often coincides with cataract related to older age, additionally triggered by diabetes. The cataract and diabetic retinopathy are considered as two major causes of the blindness in some areas of the world (Rabiu, Al Bdour, Abu Ameerh, & Jadoon, 2015).
However, other studies with 3,877 (98%) people out of the 3,885 eligible, examined, have shown that the main causes of the blindness and serious visual impairment were the untreated cataract (58.2%), glaucoma (10.9%), and other posterior segment injuries (10.9%). Diabetes affects more than half of diabetic population by various forms of retinopathy and causes vision loss threatening damages in 14.6% of the population (Zatic et al., 2014). The meta-analysis of eight studies involving 20,837 subjects has shown that the risk of cataract in type 2 diabetes was increased in comparison with non-diabetic subjects (OR = 1.97, 95% CI = [1.45, 2.67], p < .001) (L. Li, Wan, & Zhao, 2014). This is basically obvious, that the visual impairment deprives of crucial cognitive function, worsens the quality of life, increases risk of falls and fractures, restricts social contacts, deteriorates self-management, and limits adherence to medication.
Posture Instability Due to Vestibular Dysfunction
Although sensory neuropathy is the main factor of posture instability in diabetes and diabetic retinopathy is mainly responsible for increased risk of falls in diabetes, the diabetes complications may involve other senses including internal ear, leading to vestibular dysfunction (D’Silva, Lin, Staecker, Whitney, & Kluding, 2015) as well as hearing impairment (Ren et al., 2018).
However, relationship between vertigo, dizziness, and diabetes is not clear and multifactorial. It may simply involve dehydration and orthostatic hypotonia preceded by hyperglicemia. On the contrary, hypoglycemia associates with equilibrium disturbances and falls, when glucose supply for the brain decreases. Impaired glucose level associated with electrolyte imbalance and heart arrhythmias can cause dizziness or even syncope. The higher prevalence of benign paroxysmal positional vertigo was observed in diabetic patients; however, it was supposed to be related with hypertension on diabetic background, rather than diabetes itself (D’Silva et al., 2016). The atherosclerosis triggered by diabetes impairs microcirculation, which may affect equilibrium organ and perturb its function. According to the authors of available literature review, which included 14 studies comprising total of the 1,364 patients, it appears plausible to hypothesize a direct link between chronic metabolic imbalance and peripheral vestibular organ dysfunction (Gioacchini et al., 2018). This specificity of elderly, especially burdened with diabetes, should be widely known for health care professionals in hospitals, nursing homes, and caregivers dealing with community dwelling older people.
Summary
Mutual relationships between glycemic imbalance, diabetic complications, comorbidities and Geriatric Giant, deteriorate health status and functionality of elderly patients. The comprehensive knowledge about the influence of diabetes on Geriatric Giant is necessary to provide required healthcare at various levels of health care system. It comprises of comprehensive interventions, efficient encourage to early prevention, what also spares health care resources in long-term perspectives.The national prevention programs should disseminate the knowledge about specific problems of elderly patients with diabetes, emphasizing Geriatric Giants. However, the long-term educational programs should be addressed to younger population, stressing the necessity of change of sitting style–life and inappropriate diet. In the light of meta-analysis comprising 63 studies, the lifestyle modification appears an effective way to reduce the risk of diabetes even with a small weight reduction (Galaviz et al., 2018).
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- American Diabetes Association. (2017). Promoting health and reducing disparities in populations. Diabetes Care, 40(Suppl. 1), S6-S10. doi: 10.2337/dc17-s004 [DOI] [PubMed] [Google Scholar]
- Asuzu C. C., Walker R. J., Williams J. S., Egede L. E. (2017). Pathways for the relationship between diabetes distress, depression, fatalism and glycemic control in adults with type 2 diabetes. Journal of Diabetes and Its Complications, 31, 169-174. doi: 10.1016/j.jdiacomp.2016.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avorn J. (1995). Essay: Medication use and the elderly: Current status and opportunities. Health Affairs, 14, 276-286. doi: 10.1377/hlthaff.14.1.276 [DOI] [PubMed] [Google Scholar]
- Bansal D., Bhansali A., Kapil G., Undela K., Tiwari P. (2012). Type 2 diabetes and risk of prostate cancer: A meta-analysis of observational studies. Prostate Cancer and Prostatic Diseases, 16, 151-158. doi: 10.1038/pcan.2012.40 [DOI] [PubMed] [Google Scholar]
- Bohn B., Schöfl C., Zimmer V., Hummel M., Heise N., Holl R. W. (2016). Achievement of treatment goals for secondary prevention of myocardial infarction or stroke in 29,325 patients with type 2 diabetes: A German/Austrian DPV-multicenter analysis. Cardiovascular Diabetology, 15(1), Article 72. doi: 10.1186/s12933-016-0391-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouchi R., Fukuda T., Takeuchi T., Nakano Y., Murakami M., Minami I., . . . Ogawa Y. (2017). Association of sarcopenia with both latent autoimmune diabetes in adults and type 2 diabetes: A cross-sectional study. Journal of Diabetes and Its Complications, 31, 992-996. doi: 10.1016/j.jdiacomp.2017.02.021 [DOI] [PubMed] [Google Scholar]
- Carpintero P. (2014). Complications of hip fractures: A review. World Journal of Orthopedics, 5, 402-411. doi: 10.5312/wjo.v5.i4.402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspersen C. J., Thomas G. D., Boseman L. A., Beckles G. L., Albright A. L. (2012). Aging, Diabetes, and the Public Health System in the United States. American Journal of Public Health, 102, 1482-1497. doi: 10.2105/ajph.2011.300616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Wu F., Saito E., Lin Y., Song M., Luu H. N., . . . Potter J. D. (2017). Association between type 2 diabetes and risk of cancer mortality: A pooled analysis of over 771,000 individuals in the Asia Cohort Consortium. Diabetologia, 60, 1022-1032. doi: 10.1007/s00125-017-4229-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chhetri J. K., Zheng Z., Xu X., Ma C., Chan P. (2017). The prevalence and incidence of frailty in Pre-diabetic and diabetic community-dwelling older population: Results from Beijing longitudinal study of aging II (BLSA-II). BMC Geriatrics, 17(1), Article 47. doi: 10.1186/s12877-017-0439-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amato C., Morganti R., Greco C., Di Gennaro F., Cacciotti L., Longo S., . . . Spallone V. (2016). Diabetic peripheral neuropathic pain is a stronger predictor of depression than other diabetic complications and comorbidities. Diabetes and Vascular Disease Research, 13, 418-428. doi: 10.1177/1479164116653240 [DOI] [PubMed] [Google Scholar]
- Data and statistics. (2018, July 18). Retrieved from http://www.euro.who.int/en/health-topics/noncommunicable-diseases/diabetes/data-and-statistics
- De Lastours V., Foxman B. (2014). Urinary tract infection in diabetes: Epidemiologic considerations. Current Infectious Disease Reports, 16(1), Article 389. doi: 10.1007/s11908-013-0389-2 [DOI] [PubMed] [Google Scholar]
- Demir O., Sen V., Irer B., Bozkurt O., Esen A. (2017). Prevalence and possible risk factors for urinary incontinence: A cohort study in the city of Izmir. Urologia Internationalis, 99, 84-90. doi: 10.1159/000466705 [DOI] [PubMed] [Google Scholar]
- Diabetology C. (2018). 2018 Guidelines on the management of diabetic patients. A Position of Diabetes Poland. Clinical Diabetology, 7, 1-90. doi: 10.5603/dk.2018.0001 [DOI] [Google Scholar]
- D’Silva L. J., Lin J., Staecker H., Whitney S. L., Kluding P. M. (2015). Impact of diabetic complications on balance and falls: Contribution of the vestibular system. Physical Therapy, 96, 400-409. doi: 10.2522/ptj.20140604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Silva L. J., Staecker H., Lin J., Sykes K. J., Phadnis M. A., McMahon T. M., . . . Kluding P. M. (2016). Retrospective data suggests that the higher prevalence of benign paroxysmal positional vertigo in individuals with type 2 diabetes is mediated by hypertension. Journal of Vestibular Research, 25, 233-239. doi: 10.3233/ves-150563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried L. P., Tangen C. M., Walston J., Newman A. B., Hirsch C., Gottdiener J., . . . McBurnie M. A. (2001). Frailty in Older Adults: Evidence for a Phenotype. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 56(3), M146-M157. doi: 10.1093/gerona/56.3.m146 [DOI] [PubMed] [Google Scholar]
- Galaviz K. I., Weber M. B., Straus A., Haw J. S., Narayan K. V., Ali M. K. (2018). Global diabetes prevention interventions: A systematic review and network meta-analysis of the real-world impact on incidence, weight, and glucose. Diabetes Care, 41, 1526-1534. doi: 10.2337/dc17-2222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geriatrics: The diseases of old age and their treatment. (1914). Journal of the American Medical Association, LXIII(1), Article 53. doi: 10.1001/jama.1914.02570010055026 [DOI] [Google Scholar]
- Gioacchini F. M., Albera R., Re M., Scarpa A., Cassandro C., Cassandro E. (2018). Hyperglycemia and diabetes mellitus are related to vestibular organs dysfunction: Truth or suggestion? A literature review. Acta Diabetologica. Advance online publication. doi: 10.1007/s00592-018-1183-2 [DOI] [PubMed] [Google Scholar]
- Giovannucci E., Harlan D. M., Archer M. C., Bergenstal R. M., Gapstur S. M., Habel L. A., . . . Yee D. (2010). Diabetes and cancer: A consensus report. Diabetes Care, 33, 1674-1685. doi: 10.2337/dc10-0666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golbidi S., Laher I. (2010). Bladder dysfunction in diabetes mellitus. Frontiers in Pharmacology, 1, 136. doi: 10.3389/fphar.2010.00136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groeneveld O. N., Kappelle L. J., Biessels G. J. (2015). Potentials of incretin-based therapies in dementia and stroke in type 2 diabetes mellitus. Journal of Diabetes Investigation, 7, 5-16. doi: 10.1111/jdi.12420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt R. I., De Groot M., Golden S. H. (2014). Diabetes and depression. Current Diabetes Reports, 14(6), Article 491. doi: 10.1007/s11892-014-0491-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung C., Wang C., Tang T., Chen L., Peng L., Hsiao F., Chen L. (2017). Recurrent falls and its risk factors among older men living in the veterans retirement communities: A cross-sectional study. Archives of Gerontology and Geriatrics, 70, 214-218. doi: 10.1016/j.archger.2017.02.001 [DOI] [PubMed] [Google Scholar]
- International Diabetes Federation. (2017). IDF diabetes atlas (8th ed.). Retrieved from http://diabetesatlas.org/resources/2017-atlas.html
- Ishizawa K., Babazono T., Horiba Y., Nakajima J., Takasaki K., Miura J., . . .Uchigata Y. (2016). The relationship between depressive symptoms and diabetic complications in elderly patients with diabetes: Analysis using the Diabetes Study from the Center of Tokyo Women’s Medical University (DIACET). Journal of Diabetes and Its Complications, 30, 597-602. doi: 10.1016/j.jdiacomp.2016.02.004 [DOI] [PubMed] [Google Scholar]
- Krishnan B. (2013). Gastrointestinal complications of diabetes mellitus. World Journal of Diabetes, 4(3), 51-63. doi: 10.4239/wjd.v4.i3.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kwon K. J., Lee E. J., Kim M. K., Kim S. Y., Kim J. N., Kim J. O., . . . Han S. (2015). Diabetes augments cognitive dysfunction in chronic cerebral hypoperfusion by increasing neuronal cell death: Implication of cilostazol for diabetes mellitus-induced dementia. Neurobiology of Disease, 73, 12-23. doi: 10.1016/j.nbd.2014.08.034 [DOI] [PubMed] [Google Scholar]
- Lakey W., Barnard K., Batch B., Chiswell K., Tasneem A., Green J. (2013). Are current clinical trials in diabetes addressing important issues in diabetes care? Diabetologia, 56, 1226-1235. doi: 10.1007/s00125-013-2890-4 [DOI] [PubMed] [Google Scholar]
- Li F., Liu B., Zhu H., Li T., Zhang W., Su X., . . . Ma J. (2017). Continuous glucose monitoring in newly diagnosed type 2 diabetes patients reveals a potential risk of hypoglycemia in older men. Journal of Diabetes Research, 2017, Article 2740372. doi: 10.1155/2017/2740372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L., Wan X., Zhao G. (2014). Meta-analysis of the risk of cataract in type 2 diabetes. BMC Ophthalmology, 14(1), Article 94. doi: 10.1186/1471-2415-14-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim J. C., Ko K. I., Mattos M., Fang M., Zhang C., Feinberg D., . . . Graves D. T. (2017). TNFα contributes to diabetes impaired angiogenesis in fracture healing. Bone, 99, 26-38. doi: 10.1016/j.bone.2017.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magny E., Le Petitcorps H., Pociumban M., Bouksani-Kacher Z., Pautas É., Belmin J., . . . Lafuente-Lafuente C. (2018). Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: A prospective case series. PLoS ONE, 13(2), e0193034. doi: 10.1371/journal.pone.0193034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marden J. R., Mayeda E. R., Tchetgen Tchetgen E. J., Kawachi I., Glymour M. M. (2017). High hemoglobin A1c and diabetes predict memory decline in the health and retirement study. Alzheimer Disease & Associated Disorders, 31, 48-54. doi: 10.1097/wad.0000000000000182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez R. F., Jaimes-Aveldañez A., Hernández-Pérez F., Arenas R., Miguel G. F. (2013). Oral Candida spp carriers: Its prevalence in patients with type 2 Diabetes Mellitus. Anais Brasileiros De Dermatologia, 88, 222-225. doi: 10.1590/s0365-05962013000200006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurer M. S., Burcham J., Cheng H. (2005). Diabetes mellitus is associated with an increased risk of falls in elderly residents of a long-term Care facility. The Journals of Gerontology, Series A: Biological Sciences & Medical Sciences, 60, 1157-1162.doi: 10.1093/gerona/60.9.1157 [DOI] [PubMed] [Google Scholar]
- McCoy R. G., Van Houten H. K., Ziegenfuss J. Y., Shah N. D., Wermers R. A., Smith S. A. (2012). Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care, 35, 1897-1901. doi: 10.2337/dc11-2054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon S., Rossi R., Nshimyumukiza L., Wusiman A., Zdraveska N., Eldin M. S. (2016). Convergence of a diabetes mellitus, protein energy malnutrition, and TB epidemic: The neglected elderly population. BMC Infectious Diseases, 16(1), Article 361. doi: 10.1186/s12879-016-1718-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miguel L., Julia A. H., Mercè P., Abelardo G. L., Krysmaru A., Sebastián C. (2015). Prevalence of hospital malnutrition in patients with diabetes mellitus: A sub-analysis of the PREDyCES study. SM Journal of Public Health & Epidemiology, 1, Article 1018. [Google Scholar]
- Miller P. D. (2014). Chronic kidney disease and osteoporosis: Evaluation and management. Bonekey Reports, 3, Article 542. doi: 10.1038/bonekey.2014.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore E. E., Jackson S. L., Boyko E. J., Scholes D., Fihn S. D. (2008). Urinary incontinence and urinary tract infection. Obstetrics & Gynecology, 111(2, Part 1), 317-323. doi: 10.1097/aog.0b013e318160d64a [DOI] [PubMed] [Google Scholar]
- National Diabetes Statistics Report. (2017). Estimates of Diabetes and Its Burden in the United States. Retrieved from http://www.diabetes.org/assets/pdfs/basics/cdc-statistics-report-2017.pdf
- Nongmaithem M., Bawa A. P., Pithwa A., Bhatia S., Singh G., Gooptu S. (2016). A study of risk factors and foot care behavior among diabetics. Journal of Family Medicine and Primary Care, 5, 399-403. doi: 10.4103/2249-4863.192340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piątkiewicz P., Buraczewska-Leszczyńska B., Kuczerowski R., Bernat-Karpińska M., Rabijewski M., . . . Kowrach M. (2014). Ciężka hipoglikemia u pacjentów w starszym wieku z cukrzycą typu 2 oraz towarzyszącymi chorobami układu krążenia [Severe hypoglycaemia in elderly patients with type 2 diabetes and accompanying cardiovascular diseases]. Kardiologia Polska. doi: 10.5603/kp.a2016.0043 [DOI] [PubMed] [Google Scholar]
- Powell C. R. (2014). Is the diabetic bladder a neurogenic bladder? Evidence from the literature. Current Bladder Dysfunction Reports, 9, 261-267. doi: 10.1007/s11884-014-0255-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabiu M. M., Al Bdour M. D., Abu Ameerh M. A., Jadoon M. Z. (2015). Prevalence of blindness and diabetic retinopathy in Northern Jordan. European Journal of Ophthalmology, 25, 320-327. doi: 10.5301/ejo.5000557 [DOI] [PubMed] [Google Scholar]
- Reátegui D., Tornero E., Popescu D., Sastre S., Camafort M., Gines G., . . . Lozano L. (2017). Postoperative hyperglycaemia control reduces postoperative complications in patients subject to total knee arthroplasty. The Knee, 24, 128-136. doi: 10.1016/j.knee.2016.09.011 [DOI] [PubMed] [Google Scholar]
- Ren J., Ma F., Zhou Y., Xu A., Zhang J., Ma R., Xiao X. (2018). Hearing impairment in type 2 diabetics and patients with early diabetic nephropathy. Journal of Diabetes and Its Complications, 32, 575-579. doi: 10.1016/j.jdiacomp.2018.03.014 [DOI] [PubMed] [Google Scholar]
- Richardson K., Bennett K., Kenny R. A. (2014). Polypharmacy including falls risk-increasing medications and subsequent falls in community-dwelling middle-aged and older adults. Age and Ageing, 44, 90-96. doi: 10.1093/ageing/afu141 [DOI] [PubMed] [Google Scholar]
- Rizzi M., Trevisan R. (2016). Genitourinary infections in diabetic patients in the new era of diabetes therapy with sodium-glucose cotransporter-2 inhibitors. Nutrition, Metabolism and Cardiovascular Diseases, 26, 963-970. doi: 10.1016/j.numecd.2016.07.006 [DOI] [PubMed] [Google Scholar]
- Shenoy P., Harugeri A. (2015). Elderly patients’ participation in clinical trials. Perspectives in Clinical Research, 6, 184-189. doi: 10.4103/2229-3485.167099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirazian S., Grant C. D., Aina O., Mattana J., Khorassani F., Ricardo A. C. (2017). Depression in chronic kidney disease and end-stage renal disease: Similarities and differences in diagnosis, epidemiology, and management. Kidney International Reports, 2, 94-107. doi: 10.1016/j.ekir.2016.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shlomai G., Neel B., LeRoith D., Gallagher E. J. (2016). Type 2 diabetes mellitus and cancer: The role of pharmacotherapy. Journal of Clinical Oncology, 34, 4261-4269. doi: 10.1200/jco.2016.67.4044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soliman Y., Meyer R., Baum N. (2016). Falls in the elderly secondary to urinary symptoms. Reviews in Urology, 18, 28-32. [PMC free article] [PubMed] [Google Scholar]
- Subramanian L., Quinn M., Zhao J., Lachance L., Zee J., Tentori F. (2017). Coping with kidney disease—Qualitative findings from the Empowering Patients on Choices for Renal Replacement Therapy (EPOCH-RRT) study. BMC Nephrology, 18(1), Article 119. doi: 10.1186/s12882-017-0542-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland G. T., Lim J., Srikanth V., Bruce D. G. (2017). Epidemiological approaches to understanding the link between type 2 diabetes and dementia. Journal of Alzheimer’s Disease, 59, 393-403. doi: 10.3233/jad-161194 [DOI] [PubMed] [Google Scholar]
- Tau J. A., Arevalo Santana L. F. (2017). Esophageal disease in diabetes mellitus. In Sellin J. (Ed.), Managing gastrointestinal complications of diabetes (pp. 15-24). doi: 10.1007/978-3-319-48662-8_2 [DOI] [Google Scholar]
- Terzin V., Várkonyi T., Szabolcs A., Lengyel C., Takács T., Zsóri G., . . . Czakó L. (2014). Prevalence of exocrine pancreatic insufficiency in type 2 diabetes mellitus with poor glycemic control. Pancreatology, 14, 356-360. doi: 10.1016/j.pan.2014.07.004 [DOI] [PubMed] [Google Scholar]
- Tonks K. T., White C. P., Center J. R., Samocha-Bonet D., Greenfield J. R. (2017). Bone turnover is suppressed in insulin resistance, independent of adiposity. The Journal of Clinical Endocrinology & Metabolism, 102, 1112-1121. doi: 10.1210/jc.2016-3282 [DOI] [PubMed] [Google Scholar]
- Vellas B., Fielding R. A., Bens C., Bernabei R., Cawthon P. M., Cederholm T. (2018). Implications of ICD-10 for sarcopenia clinical practice and clinical trials: Report by the international conference on Frailty and Sarcopenia Research Task Force. Journal of Frailty and Aging, 7(1), 2-9. doi: 10.14283/jfa.2017.30 [DOI] [PubMed] [Google Scholar]
- Vetrano D. L., Foebel A. D., Marengoni A., Brandi V., Collamati A., Heckman G. A., . . . Onder G. (2016). Chronic diseases and geriatric syndromes: The different weight of comorbidity. European Journal of Internal Medicine, 27, 62-67. doi: 10.1016/j.ejim.2015.10.025 [DOI] [PubMed] [Google Scholar]
- Weinstock R. S., DuBose S. N., Bergenstal R. M., Chaytor N. S., Peterson C., Olson B. A., . . .Hirsch I. B. (2015). Risk factors associated with severe hypoglycemia in older adults with type 1 diabetes. Diabetes Care, 39, 603-610. doi: 10.2337/dc15-1426 [DOI] [PubMed] [Google Scholar]
- Weinstock R. S., Xing D., Maahs D. M., Michels A., Rickels M. R., Peters A. L. (2013). Severe hypoglycemia and diabetic ketoacidosis in adults with type 1 diabetes: Results from the T1D exchange clinic registry. The Journal of Clinical Endocrinology & Metabolism, 98, 3411-3419. doi: 10.1210/jc.2013-1589 [DOI] [PubMed] [Google Scholar]
- Zatic T., Bendelic E., Paduca A., Rabiu M., Corduneanu A., Garaba A., . . . Zamă-Mardari I. (2014). Rapid assessment of avoidable blindness and diabetic retinopathy in Republic of Moldova. British Journal of Ophthalmology, 99, 832-836. doi: 10.1136/bjophthalmol-2014-305824 [DOI] [PubMed] [Google Scholar]