Abstract
To evaluate the efficacy of a health-promotion intervention in increasing self-reported physical activity among university students in Sub-Saharan Africa. Randomly selected second-year students at a university in South Africa were randomized to an intervention based on social cognitive theory: health-promotion, targeting physical activity and fruit, vegetable, and fat consumption; or HIV risk-reduction, targeting sexual-risk behaviors. Participants completed assessments via audio computer-assisted self-interviewing pre-intervention and 6 and 12 months post-intervention. 176 were randomized with 171 (97.2 %) retained 12 months post-intervention. Generalized-estimating-equations analyses indicated that the health-promotion-intervention participants were more likely to meet physical-activity guidelines than were control participants, post-intervention, adjusting for pre-intervention physical activity (odds ratio [OR] = 3.35; 95% CI: 1.33-8.41). Health-promotion participants reported a greater number of days they did vigorous-intensity (risk ratio [RR] = 2.01; 95% CI: 1.43-2.83) and moderate-intensity (RR = 1.40; 95% CI: 1.01-1.95) aerobic activity, but not strength-building activity (RR = 1.37; 95% CI: 0.091-2.07). The intervention reduced self-reported servings of fried foods (mean difference = −0.31; 95% CI: −0.60, −0.02). The findings suggest that theory-based, contextually appropriate interventions may increase physical activity among university students in Sub-Saharan Africa.
Keywords: Randomized controlled trial, physical activity, health-promotion intervention, 5-a-Day diet, Social cognitive theory, Sub-Saharan Africa, University students
Over the past 30 years, the prevalence of non-communicable diseases (NCDs) has been rising worldwide, and now NCDs are the world’s leading killers, causing more deaths than all other causes combined 1. Nearly 75% of the world’s 38 million NCDs-related deaths during 2012 occurred in low-and-middle-income countries. Each year 8 million people below the age of 60 years in low-and-middle income countries die from preventable NCDs, including cardiovascular diseases, hypertension, cancer, and diabetes. The risk of these diseases is associated with certain behaviors, including physical inactivity and inadequate fruit-and-vegetable consumption.
There is growing recognition of the impact of NCDs on morbidity and mortality in South Africa.2-4 NCD behavioral risk factors, particularly physical inactivity, are prevalent in South Africa. For instance, a national survey found that 46.6% of female and 31.3% of male black South Africans 15 to 24 years of age engaged in insufficient physical activity 5. Another national survey found that 42.4% of female and 34.4% of male black pubic high school students engaged in insufficient physical activity 6.
Few physical-activity interventions have been rigorously evaluated with South Africans 7-12. Most physical-activity interventions have been developed, implemented, and evaluated in developed countries 10, 11. Two recent randomized controlled trials (RCTs) of health-promotion interventions in South Africa, one on young adolescents 13 and one on men 14, 15, found significant increases in physical activity.
Students encounter challenges during the transition from high school to university, a transition that provides freedom from parental supervision, often accompanied by changes in behavior, including decreased physical activity 16. Based on a review of the scientific literature 17, guidelines for physical activity 18 were developed that recommended a combination of aerobic activity and strength-building activity because evidence linked both types of physical activity to reduced risk of NCDs and all-cause mortality. Here we report a RCT testing the efficacy of an intervention to increase adherence to those physical-activity guidelines and other healthful behaviors among university students in South Africa. The intervention was developed based on behavior-change theories 19, 20, integrated with extensive formative research, including focus groups 21 and surveys 22-25 with the target population.
We hypothesized that the health-promotion intervention would increase self-reported adherence to physical-activity guidelines during a 12-month post-intervention period compared with an attention-matched control group. Secondary outcomes included fruit-and-vegetable consumption and fried food intake.
Methods
The Institutional Review Board of the University of Pennsylvania and the Ethics Committee of the University of Fort Hare approved the study. The study was conducted at a university located in a rural area in Eastern Cape Province, South Africa. In November 2008, toward the end of the academic year, the university’s administration provided a list with names, gender, nationality, and contact details of all first-year students. Using computer-generated random number sequences, from the 1,469 first-year students, we randomly selected and invited to participate 244 such that the sample would include equal numbers of male and female and South African and non-South African students. Those who were 18 to 24 years of age and who did not plan to leave the university within the following 12 months were eligible.
Eligible students were invited to participate in “Wake-up!,” a health-promotion project. As compensation, the students were offered a t-shirt with the study logo, a certificate of completion, and a grocery-shop voucher of R120 at post-intervention assessment; a portfolio with the study logo and a grocery-shop voucher of R60 at the 6-month follow-up; and a backpack with the study logo and a grocery-shop voucher of R100 at the 12-month follow-up. At the time of informed consent, R1 was worth about $0.10 US dollars.
All participants gave written informed consent before enrollment. After returning to the university in January 2009 for their second academic year, eligible students were invited to attend the baseline data collection. Those who completed the baseline assessment were invited to attend a separate session at which computer-generated random number sequences were used to randomize them to the health-promotion or attention-matched control intervention. A biostatistician conducted the computer-generated random assignments; the principal investigator, Dr. Heeren, implemented the assignments. South African and non-South African and male as well as female students were randomly assigned separately to ensure that nationality and gender were balanced across the interventions.
Intervention Methods
Each intervention consisted of 8, 45-minute modules, with 2 modules implemented during each of 4 weekly sessions. Each intervention was highly structured and involved interactive exercises, games, brainstorming, role-playing, videos, and group discussions implemented in mixed-gender groups of 7 to 11 participants (mean group size = 8.8) led by co-facilitator pairs using standardized intervention manuals.
The health-promotion intervention was designed to increase knowledge, attitudes, self-efficacy, and skills to prevent NCDs by increasing physical activities, choosing healthy diets, and limiting alcohol use. Formative research was conducted and all activities were pilot tested to ensure the appropriateness of the intervention and to determine whether the games, videos and exercise aids, such as pedometers and rubber bands for strength building, would be accepted by the population 21.
Table 1 presents the outline of the health-promotion intervention. In a health-assessment activity, participants recorded their health-related behaviors to understand how and where they could make changes to reduce their risk for NCDs. Participants learned and practiced different types of physical activity: (a) aerobic, defined as activity that increases the ability of the heart, lungs and systems of blood vessels to supply oxygen and nutrients to the body to move further, and longer, with less effort (b) strength building, defined as activity that builds muscle; and (c) flexibility increasing, defined as activity that increases the ability to move around easily and safely through a range of motion.
Table 1.
Outline of the Wake-up Health-Promotion intervention
| Module | Title | Components |
|---|---|---|
| 1 | Getting to know you-me and my life | Introduction of program |
| Established group rules | ||
| Introduce “Wake Up” theme | ||
| Identify participants’ short and long-term life goals, obstacles to goals and their solutions. | ||
| 2 | Nutrition: You are what you eat | Life on Campus |
| Health Risk Assessment | ||
| Eating better 5-a-Day Diet |
||
| 3 | Nutrition: Planning & Budget | Eating healthy: Barriers & Solution |
| Introduction to Time | ||
| Cooking Healthy on Campus | ||
| 4 | Exercise: You are what you do | Assessment Physical Activity |
| Video on Physical Activity | ||
| Physical Activity Fitness | ||
| Benefits of Exercising | ||
| Attitudes about Exercise | ||
| 5 | Exercise: Planning & Budget | Aerobic Workout |
| Exercising on Campus | ||
| 6 | Alcohol: You are what you do | Alcohol Intake Assessment |
| The Health Risks of Alcohol Limiting Alcohol Intake |
||
| 7 | Staying committed to your health | Personal Health Goals |
| Barriers & Solutions | ||
| Peer and partner pressure | ||
| Rugby Review Activity | ||
| 8 | Review and closing Review | Closing activity-Letter to Self |
| Commitment to healthy life style | ||
| Closing ceremony | ||
Consistent with physical-activity guidelines, we encouraged participants to engage in a combination of aerobic and strength-building exercises each week: (1) at least 30 minutes of moderate-intensity aerobic activity on 5 days or at least 20 minutes of vigorous-intensity aerobic activity on 4 days and (2) strength-building activity on at least 2 days 18. During the intervention, participants exercised to upbeat South African music. Because self-efficacy is confidence in the ability to perform a behavior despite obstacles, an important element of the intervention was brainstorming to identify the participants’ barriers to exercising, commonly including lack of motivation, interest, time, and physical ability, and concrete ways they could surmount them.
Other activities covered the 5-a-Day recommendation, defined as consuming 5 to 9 servings of fruits and vegetables daily, and the “South African Food Pyramid” and addressed barriers to healthful eating that focus groups identified, including cost, taste and availability of fresh produce, and strategies for overcoming them. Participants learned ways to prepare healthy meals, avoiding excess fat and fatty sauces, and to improve their own cooking recipes and to avoid frying and to substitute healthful for unhealthful food choices. A closing ceremony was conducted during which the participants received certificates of completion.
The attention-matched control intervention, focused on HIV risk-reduction, had the same number of sessions as the health-promotion intervention and was designed to control for “Hawthorne effects” to reduce the likelihood that the health-promotion intervention’s effects could be attributed to its nonspecific features, including group interaction, and special attention 26. As reported elsewhere, it was designed to reduce unprotected sexual intercourse and multiple sexual partnerships 27.
The co-facilitators were 16 graduate students at the university (6 women and 10 men) 24 to 49 years of age (mean = 27.6; SD = 5.6) who had previously worked as HIV peer educators. We randomized them to a 5-day training to implement 1 of the 2 interventions, thereby randomizing facilitators’ characteristics across interventions. During the training, the trainers modeled the intervention activities and the facilitators practiced implementing them, received feedback, and created common responses to potential issues that might arise during implementation. The importance of fidelity to the intervention and protecting participants’ confidentiality was emphasized.
Data Collection and Measures
The participants completed confidential surveys pre-intervention and 6 and 12 months post-intervention via audio computer assisted self-interviewing (ACASI). Physical activity was assessed with 3 open-ended items the Centers for Disease Control and Prevention 28 developed: On how many of the past 7 days, did you exercise or participate in physical activity for at least 20 minutes that made you sweat and breathe hard, such as jogging, aerobic, soccer or similar physical activities? On how many of the past 7 days, did you exercise or participate in physical activity for at least 30 minutes that did not make you sweat or breathe heard, such as walking or anything else that caused small increases in breathing or heart rate? On how many of the past 7 days, did you do push-ups or sit-ups?’ The primary outcome was a binary variable, used in previous research 13, 15, 29, indicating whether the participant met the physical-activity guideline. Participants were defined as meeting the guideline if they engaged in strength-building activity on at least 2 days and engaged in either 20 minutes of vigorous activity on at least 4 days or 30 minutes of moderate activity on at least 5 days 18.
A 7-item food frequency questionnaire developed by the National Cancer Institute to evaluate 5-a-Day studies was used to measure fruit-and-vegetable consumption over the past 30 days 30. The items concerned 100% orange or grapefruit juice, other 100% juices, fruit, green salad, fried potatoes, other potatoes and other vegetables (e.g. In the past month [30 days], about how often did you drink 100% orange juice or grapefruit juice? with eight categories from did not drink 100% orange or grapefruit juice in the past month to five or more times per day). Total consumption was computed by summing individual item scores 31. A binary outcome, used in previous research 13, 29, was calculated indicating whether the participant met the 5-a-Day guideline of eating at least 5 servings of fruit and vegetables daily in the past 30 days.
To facilitate the participants’ ability to recall their behavior, they were asked to report their behaviors during a brief period (i.e., past 3 months, 30 days or 7 days). The dates comprising the period were written on a whiteboard. Additionally, they were given calendars where they could highlight the periods of concern. The importance of responding honestly was stressed, informing them that their responses would be used to create programs for other students like themselves and such programs would be effective and accurate only if the participants answered the questions honestly. The peer co-facilitators were not involved in data collection, and data collectors were blinded to participants’ intervention.
Sample Size and Statistical Analyses
Sample size and power for this trial, based on the HIV/STI risk-reduction intervention, are described elsewhere 27. Chi-square and t-tests were used to identify variables that predicted attrition. The efficacy for the health-promotion intervention was tested using logistic, Poisson, or linear generalized estimating equations (GEE) regression models32 depending on the type of outcome variable (binary, count, or continuous, respectively). The models included baseline measure of the criterion, intervention, time (two categories representing 6- and 12-month follow-up), gender, age group (coded 18 to 20 years and 21 to 24 years), nationality (South African vs. non-South African), and the Intervention-Condition x Nationality interaction. An exchangeable working correlation matrix was specified in the estimation of the model parameters and robust sandwich estimators of the standard errors were used.
We report odds ratios (OR) for binary outcomes, meeting physical-activity and 5-a-Day diet guidelines, risk ratios (RR) for counts, number of days of vigorous-intensity and moderate-intensity aerobic activity and strength-building activity, and mean differences for all other behaviors, which were linear outcomes, and corresponding 95% confidence intervals. We report Cohen’s d, an effect size estimate in standard deviation units 33 calculated using the Cox method for odds ratios 34 and the Z-test statistic and N from the GEE analysis for continuous and count variables. Analyses were performed using an intent-to-treat mode with participants analyzed based on their intervention assignment regardless of the number of intervention or data-collection sessions attended. All analyses were completed using SAS V9.3.
Results
Figure 1 shows the flow of participants through the trial. Of the 1469 first-year students attending the university, 244 were randomly selected and 240 were eligible. Of these, 201 completed the baseline assessment, and 176 (73.3%) were randomized. Among the eligible students, only 64 (53.3%) South Africans compared with 112 (93.3%) non-South Africans were randomized (χ2 = 49.09, N = 176, p = .0001). The percentage of eligible women and men randomized did not differ significantly.
Figure 1:
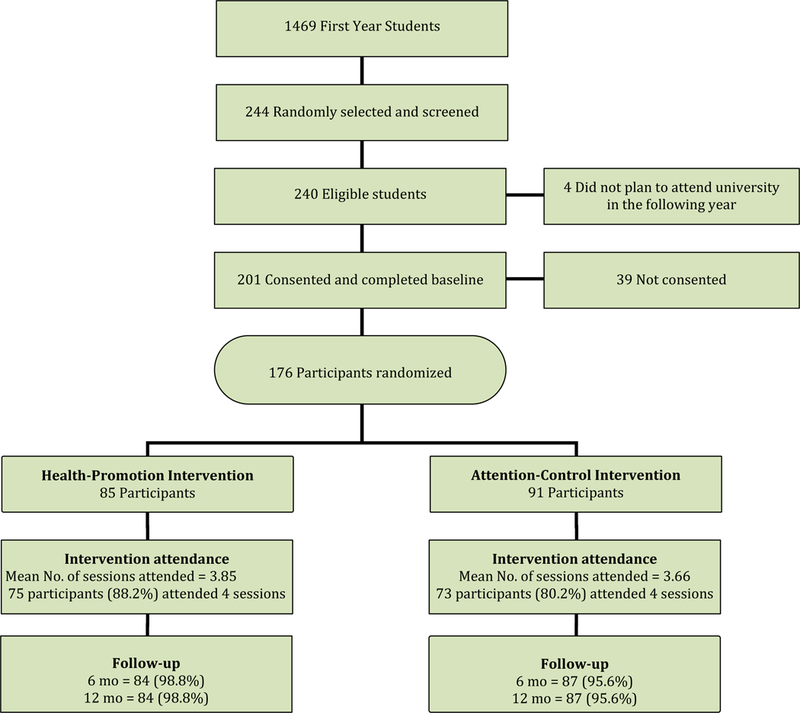
Flow of participants through the trial.
Table 2 summarizes the characteristics of the participants at baseline by intervention. Participants were 18 to 25 years of age (mean = 20.8) and 53.4% were women. Most (86.4%) participants lived on campus. About 36.4% were South Africans, 58.0% were Zimbabweans, and 5.7% were from other African countries. About 35.8% reported having problems with alcohol on the CAGE, and 4% reported using dagga (marijuana) in the past 30 days.
Table 2.
Sociodemographic characteristics and self-reported behaviors of participating students at baseline, by intervention condition, Alice, South Africa, 2009.
|
Characteristic |
HIV Control Intervention (N1=91) |
Health Intervention (N2=85) |
Total (N=176) |
|---|---|---|---|
| No. (%) Female | 47 (51.7%) | 47 (55.3%) | 94 (53.4%) |
| Mean Age (SD), years | 20.8 (1.52) | 20.9 (1.46) | 20.8 (1.49) |
| No. (%) Nationality | |||
| South Africa | 34 (37.4)% | 30 (35.3%) | 64 (36.4%) |
| Zimbabwe | 49 (53.8%) | 53 (62.4%) | 102 (58.0%) |
| Other | 8 (8.8%) | 2 (2.4%) | 10 (5.7%) |
| No. (%) Lives on campus/hostel | 76 (83.5%) | 76 (89.4%) | 152 (86.4%) |
| No. (%) Lives with steady partner | 7 (7.7%) | 6 (7.1%) | 13 (7.4%) |
| No. (%) Mother completed high school | 40 (47.6%) | 35 (44.3%) | 75 (46.01%) |
| No. (%) Father completed high school | 38 (59.4%) | 43 (59.7%) | 81(59.6%) |
| No. (%) Attends church at least weekly | 63 (69.2%) | 65 (76.5%) | 128 (72.7%) |
| No. (%) Alcohol dependent (CAGE GE 2) | 35 (38.5%) | 28 (32.9%) | 63 (35.8%) |
| No. (%) Dagga past 30 days | 3 (3.3%) | 4 (4.7%) | 7 (4.0%) |
Attendance at all intervention and data-collection sessions was excellent. A total of 173 (98.3%) attended Intervention Session 1, and 156 (88.6%), 161 (91.5%), and 170 (96.6%) attended Sessions 2-4, respectively. The number of sessions attended did not differ by any of the variables in Table 1, with the exception of nationality. South Africans (mean = 3.41) attended fewer intervention sessions than did Non-South Africans (mean = 3.95), F (1, 174) =33.83, p < .0001. A total of 173 (98.3%) attended at least 1 of the 2 follow-up data-collection sessions, 171 (97.2%) attended the 6-month and 171 (97.2%) attended the 12-month follow-up. Attending a follow-up was unrelated to the variables in Table 1 or the behavioral outcomes, with one exception. The more days on which the participants used marijuana in the past 30 days, the less likely they were to attend a follow-up session, OR = 0.64, 95% CI: 0.47-0.88.
Effects on Outcome Variables
Table 3 presents the descriptive statistics for the health behaviors by intervention and assessment. Table 4 presents the estimated intervention effects unadjusted and adjusted for baseline prevalence. Only 18% of the participants met the guidelines for both aerobic and strength-building physical activity at baseline; irrespective of intervention arm, the percentage reporting adherence to the guidelines increased significantly at 6 (27%; p = .008) and 12 months post-intervention (27%; p = .016), compared with pre-intervention. As hypothesized, the health-promotion intervention significantly affected the primary outcome, increasing self-reported adherence to the physical-activity guidelines, compared with the attention-matched control intervention, adjusting for pre-intervention adherence to physical-activity guidelines. The intervention also significantly increased the self-reported number of reported days the participants engaged in vigorous- and moderate-intensity aerobic activity compared with the control intervention. However, it did not significantly increase strength-building activity compared with the control intervention.
Table 3.
Health Behaviors by Intervention Condition and Assessment Period, University Health Promotion Program, Alice, South Africa 2008-2010.
| Variable | Baseline | 6-Month | 12-Month |
|---|---|---|---|
| No. (%) meeting physical activity guideline in past 7 days | |||
| Health Intervention | 14 (16.47) | 26 (30.95) | 28 (33.33) |
| HIV/STD Intervention | 17 (18.68) | 21 (24.14) | 19 (21.84) |
| P value | .255 | .048 | |
| Mean (SE) days intensive cardiovascular physical activity in past 7 days | |||
| Health Intervention | 1.21 (0.19) | 2.58 (0.25) | 2.51 (0.25) |
| HIV/STD Intervention | 1.63 (0.20) | 2.02 (0.20) | 2.06 (0.22) |
| P value | .026 | .033 | |
| Mean (SE) days moderate cardiovascular physical activity in past 7 days | |||
| Health Intervention | 3.31 (0.31) | 3.32 (0.28) | 3.44 (0.28) |
| HIV/STD Intervention | 2.63 (0.27) | 2.98 (0.26) | 2.49 (0.25) |
| P value | .658 | .036 | |
| Mean (SE) days strength-building physical activity in past 7 days | |||
| Health Intervention | 1.26 (0.21) | 1.87 (0.24) | 2.15 (0.26) |
| HIV/STD Intervention | 1.29 (0.17) | 1.76 (0.21) | 1.53 (0.20) |
| P value | .751 | .052 | |
| No. (%) 5-a-Day fruit and vegetables in the past 30 days | |||
| Health Intervention | 25 (29.41) | 20 (23.81) | 17 (20.48) |
| HIV/STD Intervention | 17 (19.10) | 11 (12.64) | 10 (11.49) |
| P value | .152 | .287 | |
| Mean (SE) servings of fruit per day in the past 30 days | |||
| Health Intervention | 2.22 (0.24) | 1.97 (0.23) | 1.88 (0.26) |
| HIV/STD Intervention | 1.75 (0.24) | 1.47 (0.18) | 1.31 (0.16) |
| P value | .194 | .179 | |
| Mean (SE) servings of vegetables per day in the past 30 days | |||
| Health Intervention | 1.41 (0.14) | 1.13 (0.13) | 1.59 (0.25) |
| HIV/STD Intervention | 1.13 (0.10) | 1.11 (0.13) | 1.07 (0.13) |
| P value | .823 | .092 | |
| Mean (SE) servings of fried food per day in the past 30 days | |||
| Health Intervention | 0.49 (0.09) | 0.33 (0.05) | 0.42 (0.06) |
| HIV/STD Intervention | 0.51 (0.08) | 0.52 (0.10) | 0.45 (0.07) |
| P value | .093 | .811 | |
Table 4.
GEE Empirical Significance Tests and Effect Size Estimates for the Intervention Effect Averaged Over the 6- and 12-month Follow-up Assessments Unadjusted for Baseline Prevalence and Adjusted for Baseline Prevalence, Alice, South Africa 2008-2010
| Unadjusted for Baseline | Adjusted for Baseline | |||||
|---|---|---|---|---|---|---|
| Outcome | Estimate (95% CI) | Cohen’s d | p value | Estimate (95% CI) | Cohen’s d | p value |
| Met physical activity guideline | 2.82 (1.12, 7.11) | 0.63 | .028 | 3.35 (1.33, 8.41) | 0.73 | 0.010 |
| Days vigorous aerobic activity | 1.66 (1.11, 2.50) | 0.38 | .014 | 2.01 (1.43, 2.83) | 0.64 | <0.001 |
| Days moderate aerobic activity | 1.59 (1.13, 2.23) | 0.41 | .008 | 1.40 (1.01, 1.95) | 0.31 | 0.044 |
| Days strength-building activity | 1.52 (0.97, 2.37) | 0.28 | .067 | 1.37 (0.91, 2.07) | 0.23 | 0.128 |
| Met 5-a-Day guideline | 1.34 (0.53, 3.38) | 0.18 | .540 | 0.98 (0.35, 2.73) | −0.01 | 0.966 |
| Servings of fruit per day | 0.04 (−0.66, 0.75) | 0.02 | .905 | −0.16 (−0.81, 0.48) | 0.07 | 0.622 |
| Servings of vegetables per day | 0.05 (−0.52, 0.63) | 0.03 | .853 | −0.06 (−0.64, 0.52) | 0.03 | 0.836 |
| Servings of fried food per day | −0.32 (−0.61, −0.04) | 0.34 | .027 | −0.31 (−0.60, −0.02) | 0.32 | 0.037 |
Note. Estimate = Odds ratio (Health intervention versus HIV/STD control) for binary outcome variables meeting physical activity and 5-a-Day diet guideline; estimate = risk ratio (Health intervention versus HIV/STD control) for count variables number of days of vigorous aerobic activity, moderate aerobic activity, and strength-building activity; estimate = mean difference (Health intervention - HIV/STD control) for continuous outcomes on other health behaviors. Cohen’s d =is an effect size estimate in standard deviation units calculated using the Cox method for odds ratios and the Z test statistic and N from the GEE analysis for continuous and count variables. Physical activity is in the past 7 days. Diet is in the past 30 days.
Although the health-promotion intervention did not increase adherence to the 5-a-Day guideline or servings of fruits or vegetables, it decreased the self-reported number of servings of fried food compared with the control intervention. There was a significant Nationality x Intervention interaction on vigorous aerobic activity, Z = 2.91, p = .004. The health-promotion intervention caused a greater increase in vigorous aerobic activity among South Africans, RR = 2.08, 95% CI, 1.48-2.93, p < .001, than among non-South Africans, RR = 1.07, 95% CI, 0.84, 1.37, p = .594. The only other significant Nationality x Intervention interaction was in the unadjusted-for-baseline analysis of servings of fried food, Z = 2.01, p = .044. The health-promotion intervention caused a greater decrease in servings of fried foods among South Africans, mean difference = −0.32, 95% CI, −0.61, −0.04, p = .026, than among non-South Africans, mean difference = 0.01, 95% CI, −0.15, 0.18, p = .864.
Discussion
As hypothesized, the health-promotion intervention increased self-reported adherence to physical-activity guidelines, the primary outcome, compared with the attention-matched control group, adjusting for baseline adherence. Only 18% of the participants at baseline met the physical-activity guidelines, which recommend a combination of aerobic and strength-building activity each week: strength-building on at least 2 days and either vigorous-intensity aerobic activity for at least 20 min on at least 4 days or moderate-intensity aerobic activity for at least 30 min on at least 5 days. Analyses also revealed that the intervention increased the self-reported number of days on which the students engaged in vigorous- and moderate-intensity aerobic activity, as compared with the control group, though it did not significantly increase strength-building activity.
Although there are growing calls for physical-activity interventions to reduce health risks 35, 36, few RCTs have tested the effects of such interventions in sub-Saharan Africa, particularly among university students. One study, using a quasi-experimental pre-post design, found that South African university women in a 10-week aerobic exercise program had improved BMI, waist and hip circumference, and blood pressure immediately post-intervention compared with pre-intervention, but did not examine longer-term outcomes. Two RCTs with South Africans found that interventions improved physical activity during a 12-month post-intervention period, but one was with young adolescents 13 and the other was with adult men 15. Other studies testing physical-activity interventions with South Africans have not employed RCT designs37 or have had brief follow-up periods 38. Thus, this study, consistent with epidemiological studies highlights the low levels of physical activity among young South African adults, and shows for the first time that a theory-based and contextually appropriate health-promotion intervention can be effective in increasing self-reported adherence to physical-activity guidelines among sub-Saharan university students.
The intervention employed in this study, developed based on behavior-change theories integrated with qualitative research on the target population, can be disseminated to universities in sub-Saharan Africa to address the low levels of physical activity among students. Employing a peer educator model makes the intervention cost-effective compared with the alternative of employing professionals as facilitators; moreover, peer educators may be better able to establish rapport with fellow students and to motivate them to attend the multiple intervention sessions. A RCT comparing peer educators and professionals who facilitated HIV risk-reduction or health-promotion interventions found that the adolescent participants randomized to the peer-educator conditions liked the interventions more and the facilitators more than did those randomized to professionals 39.
The strengths and limitations of this research should be considered in evaluating the findings. The strengths include the use of behavior-change theories, the use of extensive qualitative research to tailor the theories to the population, the pilot testing of the interventions, the use of a RCT, the dose-equivalent control group, and the high attendance at intervention sessions and retention at data-collection sessions. A limitation of the intervention is that, although it increased self-reported physical activity, it did not increase adherence to the 5-a-Day diet, a surprising finding in light of the extensive intervention content focused on fruit-and-vegetable consumption. On the other hand, the intervention did reduce self-reported fried food consumption. It may be that increasing students’ fruit-and-vegetable consumption is especially difficult in this rural university setting. Perhaps more structural interventions, changing the food choices available to students, are needed. Future research must address this issue.
Although we planned to have a sample that was one-half South African and one-half non-South African, we did not reach this goal. We do not know why the enrollment rate was lower among South Africans. Additional research must identify strategies to encourage South African students to participate, particularly since they appeared to benefit from the health-promotion intervention at least as much as did the non-South African students. Another limitation of the study is the use of self-reports of behavior. Although using ACASI may have reduced the impact of social desirability response bias,40 future research should employ objective measures of physical activity to confirm the present findings. Although we randomly selected students from the university, the university itself was not randomly selected; accordingly, whether the findings generalize to students at other universities in South Africa is unknown.
In conclusion, the findings support the view that health-promotion interventions based on social cognitive theory and the theory of planned behavior when integrated with formative research with the target population can be efficacious in increasing self-reported adherence to physical-activity guidelines among university students in South Africa. These findings are consistent with accumulating evidence on the utility in sub-Saharan Africa of cognitive-behavioral theories developed in the West. By implementing theory-based physical-activity interventions, it may be possible to reduce the burden of NCDs tied to physical inactivity, a burden that is growing in South Africa and other sub-Saharan African countries.
References
- 1.World Health Organization. Global status report on noncommunicable diseases 2014. Geneva: World Health Organization; 2014. [DOI] [PubMed] [Google Scholar]
- 2.Mayosi BM, Lawn JE, van Niekerk A, et al. Health in South Africa: changes and challenges since 2009. Lancet. 2012;380(9858):2029–2043. [DOI] [PubMed] [Google Scholar]
- 3.Joubert J, Norman R, Lambert EV, et al. Estimating the burden of disease attributable to physical inactivity in South Africa in 2000. S Afr Med J 2007:725–731. [PubMed] [Google Scholar]
- 4.Schneider M, Norman R, Steyn N, et al. Estimating the burden of disease attributable to low fruit and vegetable intake in South Africa in 2000. S Afr Med J 2007:717–723. [PubMed] [Google Scholar]
- 5.Peer N, Bradshaw D, Laubscher R, et al. Urban-rural and gender differences in tobacco and alcohol use, diet and physical activity among young black South Africans between 1998 and 2003. Global Health Action. 2013;6:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amosun SL, Reddy PS, Kambaran N, et al. Are students in public high schools in South Africa physically active? Outcome of the 1st South African National Youth Risk Behaviour Survey. Canadian Journal of Public Health. 2007;98(4):254–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.George ES, Kolt GS, Duncan MJ, et al. A review of the effectiveness of physical activity interventions for adult males. Sports Med. 2012;42(4):281–300. [DOI] [PubMed] [Google Scholar]
- 8.Foster C, Hillsdon M, Thorogood M, et al. Interventions for promoting physical activity. Cochrane Database Syst Rev. 2013(1):1–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hillsdon M, Foster C, Thorogood M. Interventions for promoting physical activity. Cochrane Database of Systematic Reviews. 2005(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Richards J, Hillsdon M, Thorogood M, et al. Face-to-face interventions for promoting physical activity. Cochrane Database of Systematic Reviews. 2013(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waters LA, Galichet B, Owen N, et al. Who participates in physical activity intervention trials? J Phys Act Health. 2011;8(1):85–103. [DOI] [PubMed] [Google Scholar]
- 12.King K, Meader N, Wright K, et al. Characteristics of Interventions Targeting Multiple Lifestyle Risk Behaviours in Adult Populations: A Systematic Scoping Review. Plos One. 2015;10(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jemmott JB 3rd, Jemmott LS, O’Leary A, et al. Cognitive-behavioural health-promotion intervention increases fruit and vegetable consumption and physical activity among South African adolescents: a cluster-randomised controlled trial. Psychol Health. 2011;26(2):167–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jemmott JB 3rd, Stephens-Shields A, O’Leary A, et al. Mediation of effects of a theory-based intervention on self-reported physical activity in South African men. Prev Med. 2015;72:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jemmott JB 3rd, Jemmott LS, Ngwane Z, et al. Theory-based behavioral intervention increases physical activity in South African men: a cluster-randomized controlled trial. Prev Med. 2014;64:114–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edmonds MJ, Ferreira KJ, Nikiforuk EA, et al. Body weight and percent body fat increase during the transition from high school to university in females. J Am Diet Assoc. 2008;108(6):1033–1037. [DOI] [PubMed] [Google Scholar]
- 17.Physical Activity Guidelines Advisory Committee Physical activity guidelines advisory commitee report. Washington, DC: U. S. Department of Health and Human Service; 2008. [Google Scholar]
- 18.Department of Health and Human Services. 2008. physical activity guidelines for Americans Available: http://www.health.gov/PAGuidelines/pdf/paguide.pdf. [Google Scholar]
- 19.Ajzen I The theory of planned behavior. Organ Behav Hum Dec. 1991;50(2):179–211. [Google Scholar]
- 20.Bandura A Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986. [Google Scholar]
- 21.Batidzirai JM, Heeren GA, Marange CS, et al. Wake-Up. A Health Promotion Project for Sub-Saharan University Students: Results of Focus Group Sessions. Mediterranean Journal of Social Sciences. 2014;5(7):346–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Heeren GA, Jemmott JB 3rd, Mandeya A, et al. Theory-based predictors of condom use among university students in the United States and South Africa. AIDS Education and Prevention. 2007;19(1):1–12. [DOI] [PubMed] [Google Scholar]
- 23.Heeren GA, Jemmott JB 3rd, Mandeya A, et al. Sub-Saharan African university students’ beliefs about condoms, condom-use intention, and subsequent condom use: a prospective study. AIDS Behav. 2009;13(2):268–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heeren GA, Jemmott JB 3rd, Mandeya A, et al. Sexual attitudes and behaviour of university students at a rural South African University: Results of a Pilot Survey. Journal Of Human Behavior In The Social Environment. 2012;22(8):1021–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heeren GA, Mandeya A, Marange CS, et al. Health promotion project for university students at a South African university: results of a pilot survey. Journal of Human Behavior in the Social Environment. 2013;23(8):967–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cook T, Campbell D. Quasi-experimentation: design and analysis for field settings. Chicago: Houghton Mifflin; 1979. [Google Scholar]
- 27.Heeren GA, Jemmott JB 3rd, Ngwane Z, et al. A randomized controlled pilot study of an HIV risk-reduction intervention for sub-Saharan African university students. AIDS Behav. 2013;17(3):1105–1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention. 2001. national school-based youth risk behavior survey. Public-use data documentation. Available: ftp.cdc.gov/pub/data/yrbs/2001/YRBS_2001_National_User_Guide.pdf Accessed August 2003. [Google Scholar]
- 29.El-Bassel N, Jemmott JB 3rd, Landis JR, et al. Intervention to Influence Behaviors Linked to Risk of Chronic Diseases: A Multisite Randomized Controlled Trial With African-American HIV-Serodiscordant Heterosexual Couples. Arch Intern Med. 2011;171(8):728–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thompson FE, Byers T. Dietary assessment resource manual. J Nutr. 1994;124(11 Suppl):2245S–2317S. [DOI] [PubMed] [Google Scholar]
- 31.Campbell MK, Demark-Wahnefried W, Symons M, et al. Fruit and vegetable consumption and prevention of cancer: the Black Churches United for Better Health project. Am J Public Health. 1999;89(9):1390–1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. New York: John Wiley & Sons; 2004. [Google Scholar]
- 33.Cohen J Statistical power analysis for the behavioral sciences. Hillsdale: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 34.Sanchez-Meca J, Marin-Martinez F, Chacon-Moscoso S. Effect-size indices for dichotomized outcomes in meta-analysis. Psychol Methods. 2003;8(4):448–467. [DOI] [PubMed] [Google Scholar]
- 35.Muzigaba M, Kolbe-Alexander TL, Wong F. The perceived role and influencers of physical activity among pregnant women from low socioeconomic status communities in South Africa. J Phys Act Health. 2014;11(7):1276–1283. [DOI] [PubMed] [Google Scholar]
- 36.Mokabane NN, Mashao MM, van Staden M, et al. Low levels of physical activity in female adolescents cause overweight and obesity: are our schools failing our children? S Afr Med J. 2014;104(10):665–667. [DOI] [PubMed] [Google Scholar]
- 37.Pienaar AE, Salome Kruger H, Steyn HS, et al. Change over three years in adolescents’ physical activity levels and patterns after a physical activity intervention: play study. J Sports Med Phys Fitness. 2012;52(3):300–310. [PubMed] [Google Scholar]
- 38.Edries N, Jelsma J, Maart S . The impact of an employee wellness programme in clothing/textile manufacturing companies: a randomised controlled trial. BMC Public Health. 2013;13:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jemmott JB 3rd, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: a randomized controlled trial. JAMA. 1998;279(19):1529–1536. [DOI] [PubMed] [Google Scholar]
- 40.Langhaug LF, Sherr L, Cowan FM. How to improve the validity of sexual behaviour reporting: systematic review of questionnaire delivery modes in developing countries. Tropical Med & Int Health. 2010;15(3):362–381. [DOI] [PMC free article] [PubMed] [Google Scholar]


