Abstract
Background:
Opioid agonist therapies (OAT) in Ukraine were first introduced in 2004 not as addiction treatment, but for HIV prevention. Numerous obstacles have thwarted OAT scale-up, including individual constraints and structural barriers.
Methods:
A cross-sectional survey of 1613 opioid dependent people who inject drugs (PWID) were recruited in 2014-2015 using stratified sampling in Kyiv, Odesa, Mykolayiv, Dnipro and Lviv. Analysis was restricted to a subset of 811 PWID who never received OAT. Barriers to OAT were assessed based on reasons why study participants were reluctant to enroll into OAT. A Rasch model from the Item Response Theory was applied to 24 potential barriers, used to score their severity and estimate a latent composite measure for each person’s willingness and ability to participate in OAT.
Results:
The Rasch model confirmed the cumulative nature of barriers with concerns over treatment efficacy, safety and tolerability being more prevalent than barriers related to logistical constraints, opportunity costs and social stigma. If barriers related to treatment perception and logistics were eliminated, the average barrier number would decrease from 10 to 2.2. Participants were more likely to have a higher resistance to OAT entry if they experienced fewer overdoses, did not attain higher education, were not previously incarcerated and if their peers did not have a higher level of resistance to OAT.
Conclusions:
Understanding the interdependence of various barriers and attitudes toward OAT can improve the rate of OAT expansion and ameliorate entry into substance abuse treatment programs in Ukraine.
Keywords: Addiction, opioid agonist treatment, people who inject drugs, opioid substitution treatment, Barriers to entry
1. Introduction
Ukraine, a country of 45.5 million people, has the highest HIV prevalence in Europe and is located within Eastern Europe, a region where HIV incidence and mortality continue to increase in the setting of suboptimal HIV prevention and treatment (State Statistics Service of Ukraine, 2017; Joint United Nations Programme on HIV/AIDS (UNAIDS), 2016a; Joint United Nations Programme on HIV/AIDS (UNAIDS), 2016b). Previous research based on mathematical modeling has found opioid agonist therapies (OAT) to be the most cost-effective strategy to reduce new HIV infections in Ukraine, while the combination of OAT scale-up and expansion of antiretroviral therapy coverage (ART) is the most effective strategy to reduce new HIV infections (Alistar et al., 2011). Adult HIV prevalence in Ukraine is 1.2% with more than 16,000 new infections occurring annually (UNAIDS, 2016). Ukraine’s HIV epidemic has been fueled by injection drug use, which increased in the 1990s following the dissolution of the Soviet Union (DeBell and Carter, 2005). It is estimated that close to 1% of Ukraine’s adult population injects drugs (Degenhardt et al., 2014). Among PWID, HIV prevalence is estimated to be 21.3%-41.8% (Balakirieva et al., 2014; Mathers et al., 2008; Ministry of Health et al., 2013). Opioid agonist therapies were first introduced in Ukraine with buprenorphine (BMT) in 2004 (Bruce et al., 2007), and followed by methadone maintenance treatment (MMT) in 2008 (Schaub et al., 2010) in order to stem the opioid epidemic and reduce HIV incidence (Altice et al., 2010). Importantly, however, OAT is also one of the most effective treatments for opioid use disorders that is safe, tolerable and improves a number of health, social and legal outcomes like reduction or elimination of illicit drug use, reduced crime and incarceration, increased social stability and employment and better engagement in care (Altice et al., 2010).
Despite its many documented benefits, OAT scale-up efforts have been thwarted by numerous individual and structural factors such that 8,512 of the estimated 325,000 (172,000-590,000) PWID in Ukraine, most of whom injected opioids, enrolled in OAT treatment in 2015 (Alliance for Public Health, 2016; Berleva and Sazonova, 2017). In Eastern Europe and Central Asia, treatment for opioid use disorders has been influenced more by both patient and physician predispositions and prejudices rather than by scientific evidence. The attitudes toward treatment for opioid use disorder among patients and medical staff have been reinforced by the culture within Narcology, a medical subfield of psychiatry established in the Soviet Union, which favored abstinence-based strategies over more evidence-based pharmacological treatment (Torrens et al., 2013). Qualitative studies of PWID in Ukraine suggest that individual-level barriers, including stigma, perceived ineffectiveness of treatment, fear of law enforcement coupled with other structural barriers such as administrative regulations and lengthy waiting times to enter OAT have contributed to individuals’ unwillingness to enter treatment (Bojko et al., 2016; Kutsa et al., 2016; Mazhnaya et al., 2016). Attitudes and beliefs regarding treatment have been shown to be predictive of treatment entry in both community and prison settings (Rozanova et al., 2017; Schwartz et al., 2011). Absent in previous analyses is a quantitative assessment to determine which type of barriers most frequently hinder an individual’s ability to enter OAT. A greater understanding of the interdependence of barriers can allow the policy makers to prioritize strategies that can reduce and eliminate some, if not all, of the barriers to OAT entry and improve the rate of OAT expansion. In this study, we use a Rasch model from Item Response Theory (IRT) to score the various barriers related to OAT entry and assess individual willingness and ability to participate in OAT in five cities in Ukraine.
2. Data description
From January 2014 to March 2015, self-administered surveys assessing barriers and facilitators to OAT were conducted in five large cities: Kyiv (Kiev), Odesa (Odessa), Mykolayiv (Nikolaev), Dnipro (Dnepropetrovsk), and Lviv, and stratified into three groups of PWID: 1) currently on OAT; 2) previously on OAT; and 3) never on OAT. The eligibility criteria included age (≥18 years) and meeting ICD-10 criteria for opioid dependence. Study participants who were currently or previously on OAT were randomly selected from client lists obtained from OAT sites in each city. Respondent driven sampling (RDS) was used primarily to recruit clients who were never on OAT, but also included some clients who were prescribed either BMT or MMT. RDS seeds were selected based on criteria that included residential location, age, injection duration and sex. Participants were paid 100 UAH (~US$4-10) for completing the survey, and earned 20 UAH (~US$l-2) for up to 3 recruited PWID peers (Salganik and Heckathom, 2004). Of the 1613 participants, we excluded responders who had previously enrolled into OAT, leaving the final sample of 811 individuals. The study was approved by institutional review boards at Yale University and the Gromashevskiy Institute at the National Academy of Medical Sciences.
3. Methodology
The list of barriers to OAT was derived from multiple focus group discussions that included 199 PWID from five cities in Ukraine in 2013. Findings from these focus groups have been published previously (Bojko et al., 2015; Bojko, 2016; Mazhnaya, 2016), but were used to develop an expansive list of barriers to OAT that was ultimately included in a structured survey on which our analysis is based. Table 1 provides the complete list of reasons individuals gave for not wanting to participate in OAT. OAT entry barriers were measured as dichotomous variables taking a value of 1 if a particular reason was selected and 0 otherwise. The barriers cover the following thematic areas: 1) Treatment concerns related to safety, tolerability and efficacy; 2) Perception of treatment appropriateness; 3) Program-level barriers that include perceived difficulty of gaining entry into the program, costs and logistical issues; 4) Stigma and social resentment, including disapproval from family and friends, police harassment and poor conduct of clinical staff.
Table 1.
Prevalence and Severity of Barriers to OST Entry among PWID in Ukraine (N=811)
| Barrier to Entry into OAT | Group | Prevalence (%) | Severity ( β ) Coefficient | Severity 95% CI | Average Resistance ( θ ) within Barrier Group |
|---|---|---|---|---|---|
| 1. OAT replaces one addiction for another | T | 64.48 | −0.33 | [−0.46, −0.26] | 0.542 |
| 2. OAT is bad for health | T | 63.65 | −0.30 | [−0.44, −0.24] | 0.569 |
| 3. OAT has bad side effects | T | 60.19 | −0.18 | [−0.32, −0.13] | 0.605 |
| 4. OAT is ineffective in treating addiction | T | 59.24 | −0.15 | [−0.28, −0.08] | 0.575 |
| 5. Patient not ready to start treatment | I | 57.21 | −0.09 | [−0.21, −0.02] | 0.617 |
| 6. Negative reputation of OAT | T | 53.75 | 0.01 | [−0.11, 0.07] | 0.652 |
| 7. Desire to avoid registration with narcology center | P | 50.06 | 0.11 | [−0.01, 0.18] | 0.648 |
| 8. Fear of OAT treatment | T | 48.63 | 0.15 | [0.02, 0.21] | 0.695 |
| 9. Inability to detox from OAT | T | 47.2 | 0.19 | [0.06, 0.24] | 0.709 |
| 10. Family disapproves of OAT | S | 46.72 | 0.20 | [0.09, 0.28] | 0.715 |
| 11. Reluctance to travel daily to the treatment center | P | 46.13 | 0.22 | [0.10, 0.28] | 0.743 |
| 12. Patient thinks can stop substance use without OAT | T | 45.17 | 0.24 | [0.12, 0.30] | 0.682 |
| 13. Travel restrictions associated with OAT enrollment | P | 41.6 | 0.33 | [0.22, 0.41] | 0.775 |
| 14. Perceived difficult to gain entry into treatment | P | 40.05 | 0.37 | [0.26, 0.45] | 0.745 |
| 15. Time constraints due to employment | P | 40.05 | 0.37 | [0.27, 0.46] | 0.798 |
| 16. Rigidity of the OAT program | P | 37.07 | 0.45 | [0.34, 0.52] | 0.836 |
| 17. Too young to start treatment | I | 32.06 | 0.58 | [0.47, 0.67] | 0.850 |
| 18. Inability to combine OAT with other treatments | T | 30.75 | 0.62 | [0.51, 0.71] | 0.894 |
| 19. Excessive travel time to OAT | P | 28.61 | 0.68 | [0.57, 0.77] | 0.901 |
| 20. Stigma from neighbors and/or friends | S | 26.58 | 0.74 | [0.62, 0.82] | 0.943 |
| 21. Insufficient duration of injection history | I | 25.98 | 0.75 | [0.65, 0.85] | 0.888 |
| 22. Fear of police harassment | S | 25.63 | 0.76 | [0.65, 0.86] | 0.924 |
| 23. Too costly to gain entry into treatment | P | 25.15 | 0.78 | [0.66, 0.87] | 0.872 |
| 24. Negative staff attitudes toward patients | S/P | 23.72 | 0.82 | [0.71, 0.92] | 0.960 |
Legend: Barrier Classes: T -Treatment concerns regarding safety, efficacy, tolerability; I- Treatment viewed as inappropriate; P - Program Entry and logistic barriers, S - Stigma and social resentment.
The total number of barriers listed may not provide a valid measure of the individual’s ability to access OAT because not all items are created equal and the problem of measurement scale implies that respondents may not be comparable on the basis of the number of barriers encountered. The measure of each individual’s ability to access OAT cannot be done directly, as true “ability” to access OAT is a latent trait, which by itself does not have a well-defined scale that can render individuals comparable to one another. Item Response Theory (IRT) provides a powerful conceptual and methodological framework to derive such a scale that could measure an individual’s ability based on the barriers to OAT that each person lists in the survey. In addition, one of the main advantages of using IRT is that each individual is scored based on the basis of the types of barriers selected without disclosing the total score, such that the final measurement does not depend on the overall survey instruments, but only on the distribution of responses (Bortolotti et al., 2013). Another major advantage of IRT is that the method permits one to draw comparisons of ability (to enter OAT) for different populations provided that the survey instrument is based on a common list of items (Hambleton, 1991).
We apply the IRT to model the distribution of barriers in order to rank the different barriers to OAT and to estimate the relative ability of each respondent to access OAT based on the barriers selected. Applying the one parameter model, which is also known as the Rasch in psychometric research (Baker, 2004), we estimate the log odds ratio of having a particular barrier and not having that particular barrier to be equal to the difference in the difficulty of the barrier and the respondent’s (latent) ability. In the context of OAT, the difficulty of each barrier is referred to as the parameter of severity (Cappelleri, 2014; Fusco, 2008), while the latent ability measure, in the context of OAT is referred to as the parameter of resistance to OAT participation. The parameter of severity βj reflects how prevalent the barrier is in the population. The higher the parameter of severity, the less frequently the barrier is experienced by the population and the more the model considers it to be severe (Fusco, 2008). The higher the resistance parameter, θ, the higher the probability that the individual experiences multiple barriers restricting his or her willingness to participate in treatment and/or barriers that are particularly severe (Fusco, 2008). The technical details of the model are contained the on-line supplemental Appendix1. To verify the validity of the model’s assumptions, we performed multiple additional analyses, including sensitivity analyses based on fitting a zero-inflated mixture Rasch Model to account for a larger number of individuals with no barriers, the description of which is also contained in the on-line supplemental Appendix1. As a final component of the analysis, we assessed independent correlates associated with the latent measure of individuals’ resistance to OAT entry. The correlates were based on self-report and included sex, number of injection days in the past month, number of lifetime overdoses, previous incarceration, educational attainment (3 categories: less than High School, High School, Some College or more). We estimated an auto-regression model, which included an additional parameter measuring an average correlation of ability within each individual’s coupon-recruitment network (Drukker, 2013; Heckathorn, 2011; LeSage, 2009). All analyses were performed in Stata version 14 (StataCorp, 2015).
4. Results
Table 1 contains a summary of the sample frequencies of various barriers to OAT entry. The most prevalent barriers were related to negative attitudes and perceptions about OAT. Over 60% of the sample indicated a strong dislike of either buprenorphine or methadone, viewing it as replacement of one addiction for another (64.5%), detrimental for health (63.7%), causing negative side effects (60.1%) and not being an effective treatment (59.2%). On the opposite end of the prevalence spectrum were barriers related to social stigma: less than a third of the respondents indicated negative staff attitudes toward patients (23.7%) and fear of police harassment (25.6%) among barriers to OAT entry. Other program level and personal barriers such as financial costs associated with entry (25.1%) and insufficient duration of injection history (25.9%) were also among the barriers that were less prevalent.
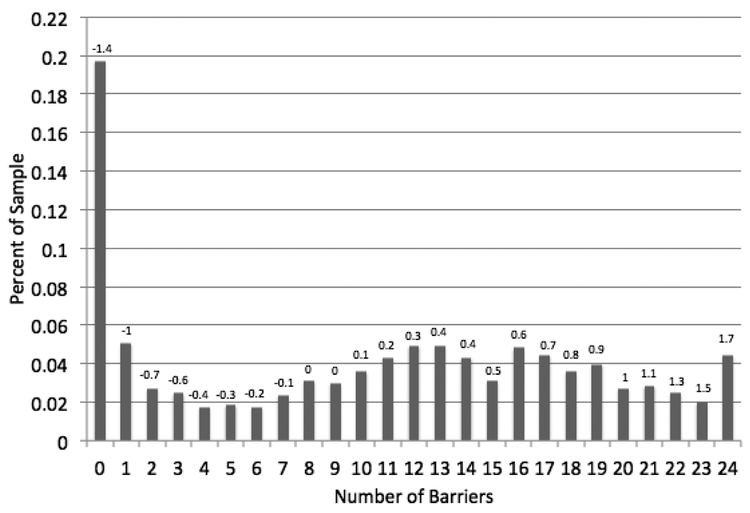
The Rasch model measures the extent to which all of the barriers are cumulative and form a hierarchical relationship. Table 1 contains the results from the Rasch model estimates for each of the barriers to entry. The severity parameter is negatively correlated with each barrier’s prevalence rate and ranges from −0.33 to 0.82. According to the modeling assumption, the higher the prevalence of the barrier the lower the relative severity of the barrier. The magnitude of the severity parameter is inversely related to the average measure of resistance among patients who reported experiencing a particular barrier (Columns 2-3, Table 1). More intuitively, this means that if a patient encounters a more severe barrier to OAT entry, s/he is more likely to encounter a barrier that is less severe. For example, the higher average resistance parameter indicates that the individuals who select less prevalent barriers, such as “negative staff attitudes toward patients,” are more likely to select other barriers with lower severity (e.g., “OAT replaces one addiction for another”). The resistance parameter has a range of −1.45 to 1.87, with the average centered at 0. Fig 1 displays the distribution of the resistance parameter associated with the total raw score of indicated barriers, as well as the range of the resistance parameter displayed above the graphical bars.
Figure 1.
Distribution of the Number of Barriers among PWID in Ukraine (N=811). The scale of resistance parameter θ is listed above the bars
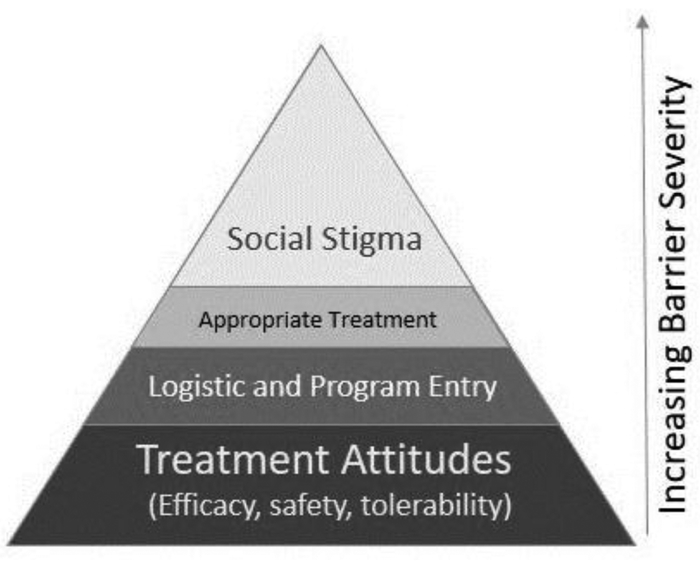
Calculating the average of the resistance parameter across four thematic categories (Category 1: Treatment concerns about safety, tolerability and efficacy; Category 2: Appropriateness of Treatment; Category 3: Program level barriers related to perceived difficulty of gaining entry into the program, costs and logistical issues; Category 4: Stigma and Social resentment); we find that many of the barriers are interconnected and the categories align in a hierarchical pattern (Fig 2). The respondents who indicated at least one barrier related to Social Stigma have the highest average resistance of 0.62. Patients indicated at least one barrier related to perception of OAT as inappropriate, having an average resistance of 0.57. Individuals who indicated at least one logistical and program-level barrier have an average resistance to entry of 0.51; and those patients who indicated concerns about OAT’s efficacy, safety and tolerability, have an average resistance parameter 0.40.
Figure 2.
Cumulative Effects of OAT Entry Barriers as Identified by Item Response Theory
The average latent measure of resistance to OAT entry varied by city. The lowest levels of unwillingness to initiate OAT were observed in Kyiv and Lviv. In Kyiv and Lviv, the average resistance parameter was −0.22 and −0.16, corresponding to approximately eight barriers being selected by an average respondent. In Dnipro and Mykolayiv the average resistance to OAT entry was equal to 0.11 and 0.13, respectively, corresponding to an average of 11 barriers that were selected. In Odesa, the average resistance parameter was 0.18 corresponding to approximately 12 barriers which were selected by respondents on average.
As a counterfactual experiment, if all the barriers related to perception of safety, tolerability and efficacy were eliminated, the average number of barriers named by participants in all cities would fall from 10 to 5.5. Under this scenario, the estimated resistance parameter would be expected to decline by 0.48 points per person on average if the severity parameters are held constant. If the barriers related to logistic and program entry were eliminated, the average number of barriers listed by participants would fall to 7.7 from 10, and the resistance parameter would be expected to decline 0.29 points on average per person. If barriers related to perceptions about appropriateness were no longer present, the average number of barriers would decline from 10 to 9, coinciding with 0.13-point decline in resistance parameter, while if barriers related to social stigma were eliminated, the average number of barriers would also fall from 10 to 9. This scenario would be associated with a 0.14 decline in the average resistance per person. Notably, if category 1 (perceptions of efficacy, safety) and category 3 barriers (logistic issues) were eliminated, the average barrier score would decline from 10 to 2.2 barriers and the resistance parameter would decline 0.80 points on average per person assuming that severity parameters do not change.
Participants were more likely to have a higher resistance to OAT entry if they experienced fewer overdoses, did not have prior history of incarceration and if they were embedded into the network of peers with higher level of resistance to OAT. In addition, PWID with higher levels of education (some college or more) had lower resistance to OAT on average relative to PWID with lower levels of education. Other factors such as sex, years of injection and monthly frequency of injection were not significantly correlated on average with the outcome measuring the individual’s resistance to OAT (Table 2).
Table 2.
Determinants of Individual’s Resistance (or Unwillingness) to Enroll into OAT based on Network Auto-Regressive Linear Model (N=811)
| Covariate | Beta Coefficient | 95% CI | P-value |
|---|---|---|---|
| Years of Injection | 0.001 | [−0.02, 0.001] | 0.69 |
| Gender | |||
| Male | Referent | ||
| Female | −0.03 | [−0.18, 0.13] | 0.75 |
| Education | |||
| Incomplete High School | −0.07 | [−0.25, 0.10] | 0.41 |
| High School Graduate | Referent | ||
| Some College or more | −0.22 | [−0.45, 0.002] | 0.05 |
| Injection Days (last 30 days) | −0.01 | [−0.02, 0.01] | 0.13 |
| Number of Overdoses (Lifetime) | −0.01 | [−0.02, −0.002] | 0.01 |
| Ever Incarcerated | −0.04 | [−0.07, −0.005] | 0.02 |
| Peer Resistance/Unwillingness | 0.08 | [0.01, 0.14] | 0.02 |
| Constant | 0.28 | [−0.06, 0.61] | 0.11 |
5. Discussion
The study uses a new method to enhance our understanding of the interdependence of the barriers to OAT among PWID who have never previously received OAT – the largest population of PWID in Ukraine. Given the low OAT coverage in Ukraine, the overwhelming majority of PWID who have never accessed it constitute ideal candidates that need to be targeted in order to curtail the HIV and opioid epidemic. While buprenorphine and methadone provide the best evidence for treating opioid use disorder and have been available for several decades, OAT is relatively new in Ukraine and its expansion has been impeded by a number of structural, social and personal barriers (Bojko, 2016).
The barriers that appear to have a lower relative prevalence are interlinked with other barriers that are more widespread. PWID who indicate resistance to OAT entry have on average approximately 13 barriers that they report as preventing their entry. At the top of the barrier distribution, 20% of respondents indicated that they have an average of 18 of 24 potential barriers, while at the lower end of the barrier distribution 20% indicate that they do not have any barriers to OAT entry and are willing to participate. In the hierarchy of barriers, we found that the perceptions about efficacy, safety and its (negative) impact on health cluster toward the bottom, as they tend to be more widespread and are associated with lower average level of resistance of OAT entry, followed by barriers related to logistical and program-level issues, perception of inappropriateness of treatment and lastly, social stigma. Development of programs and interventions that address the issues stemming from multiple barriers concomitantly is more likely to yield successful outcomes for program participation. More importantly, however, is addressing the barriers serially by dealing first with issues that are more prevalent such as perceptions about efficacy and safety prior to a less prevalent issues such as social stigma. This approach is more likely to increase the effectiveness of barrier reduction on OAT participation.
The results based on counterfactual analysis suggest that the largest declines in the average resistance parameter would be achieved by eliminating barrier perceptions of safety, tolerability and efficacy, while lower relative declines would be observed if elimination commenced with barriers related to social stigma and medication tolerance. The persistence of negative attitudes stemming from misinformation and prejudices will need to be tackled by a combination of social marketing campaigns, as well as development of healthcare decision aids. The public health marketing campaign is likely to be effective at dissemination of information, including within social networks, and among family and friends. Because negative attitudes and behaviors are reinforced through social interactions, using injection networks to harness positive change may be a crucial strategy. Studies of peer-driven interventions have documented the benefits of HIV prevention and treatment in PWID (Broadhead et al., 2012; Broadhead et al., 2002; Broadhead et al., 1998; Ostertag et al., 2006). In this study, we find that the highest correlate of the overall unwillingness to enter OAT is the reluctance and inability of each person’s peer, as measured through the recruitment chains. While the correlation is likely due to the shared environment rather than a contagion of attitudes, changes in the individual’s perception and negative attitudes toward OAT will need to transpire socially within the large group of PWID. Peer driven interventions have been shown to be effective in increasing adherence to HIV treatment (Broadhead et al., 2002), and reduction of HIV risk behaviors (Broadhead et al., 1998), and can be used to bolster OAT program entry and treatment initiation.
In addition, we find that the respondents who experienced a large number of overdoses have lower resistance to OAT entry, and may be easier to persuade than respondents who have never experienced overdose. This is likely explained by the higher perceived risk from injecting opioids and recognition that OAT reduces injection and overdose risk. Framing of OAT programs in terms of harm reduction benefit, especially for the prevention of fatal overdose, may help to draw respondents who have higher levels of loss aversion, the psychological tendency to avoid losses (Kahneman and Tversky, 1984), but the strategy would have a limited effect on those PWID who never experience an overdose, which, in the case of our RDS sample, was half of the respondents. Social marketing campaigns aimed at achieving public health goals have been effective in improving diet, increasing exercise and leading the reduction in alcohol and tobacco in the United States and Europe (Gordon, 2006; Helming and Thaler, 2010), and have the potential to reduce the negative perception bias toward OAT.
The effort to combat myths and misinformation, especially regarding the detrimental effects, safety and efficacy can be bolstered by implementing shared decision-making aids, which provides accurate information through an interaction tool that incorporates the best evidence aligned with patient preferences that allow patients and clinicians to better communicate (Elwyn et al., 2006). As such, patients can explore all the advantages and disadvantages of treatment and help the patients to reach an optimal decision. The decision aids can also eliminate misinformation, alleviating concerns about health detriments and side effects, and personal beliefs about safety and efficacy. Consequently, patients can become more motivated to adopt safer practices and adhere to the treatment regime and attain better health outcomes (King, 2005; Mondloch et al., 2001). Previous research has shown that knowledge gains by patients lead to more confidence in decisions, more active patient involvement, and, in many situations, informed patients select more suitable treatment options (Stacey et al., 2014).
Addressing organizational barriers and logistical impediments is also important for making OAT programs more accessible. Long waiting lists, delayed entry, travel restrictions, economic costs and time commitment are likely to turn away patients from treatment prior to initiating treatment. The NIATx (Network for the Improvement of Addiction Treatment) treatment improvement model for behavioral health uses short change projects to influence organizational change and is now underway throughout Ukraine. This evidence-based implementation strategy improves treatment outcomes by reducing system-level inefficiencies that cause delays in treatment entry and increases retention by improving quality care. Programs adopting the NIATx framework team-up with expert consultants to develop strategies and implement changes geared toward reducing waiting times, increasing treatment retention and reducing attrition by tackling various organizational impediments (Campbell et al., 2009; Capoccia et al., 2007; Fitzgerald and McCarty, 2009; Hoffman et al., 2008; Madden, 2018; McCarty and Chandler, 2009; McCarty et al., 2009; McCarty et al., 2007).
As of March 2016, the Ukrainian Ministry of Health adopted an amendment under Order 200, which expanded OAT access by allowing PWID to obtain OAT in pharmacies and forego the “official” registration as a drug user, provided the patient could afford the out of pocket expenses. Under this new legal rule, physicians are allowed to prescribe buprenorphine to patients directly. This change is likely to reduce the logistical barriers for many potential participants. In addition, the expansion of OAT through pharmacy prescriptions is more likely to be convenient and less stigmatizing, and may reduce incidence of police harassment, likely further reducing the overall unwillingness and inability to participate in OAT (Kutsa, 2016). The change, however, is also associated with higher out of pocket expenses, which many PWID may not be able to afford. In addition, unless other barriers related to psychological perceptions are addressed as well, removing logistical barriers is unlikely to lead to dramatic increases in OAT participation. Through counterfactual analysis, we found that elimination of the logistical barriers would hypothetically result in the decline of an overall barrier score from 10 to approximately 7.7, leaving in place many other barriers to OAT entry. While OAT expansion is underway through OAT prescriptions, including in newly developed private clinics, the risk of medical diversion may evolve as a new concern since the past highly regulated and supervised OAT programs had little diversion. Data from elsewhere that expanded OAT to pharmacies and primary care providers did identify this as a major issue (Bachireddy et al., 2015). The greater flexibility resulting in higher number and greater heterogeneity of patients being treated, however, may offset the risks of medical diversion, as expansion of formal treatment programs is likely to complement the growth in OAT prescription programs. Implementing the needed changes to overcome existing balances would not be without challenges. For example, the most prevalent barriers, such as negative perceptions and attitudes to OAT, might be addressed through harm reduction NGOs involved in outreach work within peer networks and have the potential to effectively disseminate information to PWID. On a larger scale, social marketing that may come from government or private/public partnerships might provide the best strategy for structuring and disseminating this information nationally. In the case of logistical constraints, governmental organizations would need to revisit OAT treatment guidelines (e.g., Order 200) to remove ramaining legal impediments to treatment. Alternatively, NIATx projects could be successful if done with public/private partnerships or by community NGOs that work with PWID and have alliances with OAT treatment providers.
Despite the new findings presented, the study is not without limitations. First, the small sample size, ranging from 128-200 in each city could bias our estimates due to the presence of selection bias inherent in the RDS. Our sample consists of participants from urban areas in Ukraine and may not describe the experience of the residents of rural areas or smaller cities. In addition, our survey measures the scale and scope of personal and structural barriers as perceived by the respondents at one point in time and may be subject to cognitive biases, including omission bias, availability cascade and focusing effect. We cannot rule out that the barriers are not the root “cause” of non-participation in OAT, but rather the “effect” of the latent unwillingness to enroll into OAT. The cross-sectional study design does not provide a glimpse into the belief formation and learning processes, yielding little insight into whether the perceptions are amendable to change over time. Finally, one of the assumptions used in scoring the items is that barriers that are less prevalent are severe may not hold true. In reality, the barriers are likely to reflect disparate problems that may not conceptually align into a unified dimension, even though the principle component analysis seems to suggest otherwise. The advantage of applying a Rasch model is that it helps to develop a scale for the latent ability and willingness to participate in OAT derived from types of barriers selected.
6. Conclusions
The personal attitudes and beliefs coupled with programmatic and structural barriers indicate a need for a review of existing practices, development of novel interventions and expansion of an outreach marketing campaign that can counter the prejudices and misinformation associated with OAT in Ukraine. Addressing the barriers serially by prioritizing issues related to perceptions about efficacy and safety and logistical concerns is likely to increase the effectiveness of barrier reduction in OAT participation.
While the new policy changes in Order 200, such as making buprenorphine available through prescriptions is likely to reduce logistical barriers, improving patients’ awareness and understanding of OAT benefits through targeted education and expansion of decision aids may bolster the participation in OAT across Ukraine. The analysis of barriers to OAT entry will help to inform amendments to existing policy guidelines and procedures and will enable Ukraine to meet its goal of continuing to expand the coverage of OAT treatment, while curtailing the spread of infectious diseases among PWID in Ukraine.
Supplementary Material
Highlights.
Barriers to opioid agonist treatment entry tend to be cumulative and interrelated
Concerns over tolerability, safety + efficacy comprise the most prevalent barriers
Social stigma is the least prevalent, but likely to coincide with other barriers
Resistance to treatment is related to education, incarceration and overdose history
Analysis of barrier interlinkage can improve the rate of treatment expansion
Acknowledgments
The authors would like to acknowledge the National Institute on Drug Abuse for funding for research (FLA: R01DA029910, R01 DA033679) and career development (FLA: K24 DA017072, AZ: K01DA037826) and the Global Health Equity Scholars Program funded by the Fogarty International Center and the National Institute of Allergy and Infectious Diseases (AM: Research Training Grant R25 TW009338). The funding sources had no role in the collection of data, statistical analysis or the manuscript writing.
Footnotes
Author Disclosures
Role of the Funding Source
Nothing declared
Conflict of Interest
No conflicts declared
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
References
- Alistar SS, Owens DK, Brandeau ML, 2011. Effectiveness and cost effectiveness of expanding harm reduction and antiretroviral therapy in a mixed HIV epidemic: A modeling analysis for Ukraine. PLoS Med 8, e1000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alliance for Public Health, 2016. Annual Report 2015. Kiev, Ukraine, http://aph.org.ua/wp-content/uploads/2016/07/ar2015_en.pdf. [Google Scholar]
- Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH, 2010. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. Lancet 376, 59–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachireddy C, Weisberg DF, Altice FL, 2015. Balancing access and safety in prescribing opioid agonist therapy to prevent HIV transmission. Addiction 110, 1869–1871. [DOI] [PubMed] [Google Scholar]
- Baker F, Ho-Kim S, 2004. Item Response Theory: Parameter Estimation Techniques. CRC Press, New York. [Google Scholar]
- Balakirieva O, Bondar T, Loktieva I, Sazonova Y, Sereda Y, 2014. Summary of the analytical report: Monitoring the behavior and HIV-infection prevalence among people who inject drugs as a component of the HIV second generation surveillance International HIV/AIDS Alliance, Kiev. [Google Scholar]
- Berleva G, Sazonova Y, 2017. Estimation of the Size of Populations Most-at-Risk for HIV Infection in Ukraine 2017. IFC Alliance for Public Health in Ukraine, Kiev. [Google Scholar]
- Bojko MJ, Mazhnaya A, Makarenko I, Marcus R, Dvoriak S, Islam Z, Altice FL, 2015. “Bureaucracy and Beliefs”: Assessing the barriers to accessing opioid substitution therapy by people who inject drugs in Ukraine . Drugs Educ. Prev. Pol 22, 255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojko MJ, Mazhnaya A, Marcus R, Makarenko I, Islam Z, Filippovych S, Dvoriak S, Altice FL, 2016. The future of opioid agonist therapies in Ukraine: A qualitative assessment of multilevel barriers and ways forward to promote retention in treatment. J. Subst. Abuse Treat 66, 37–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bortolotti SLV, Tezza R, de Andrade DF, Bornia AC, Farias de Sousa Junior A, 2013. Relevance and advantages of using the item response theory. Qual. Quant 47, 2341–2360. [Google Scholar]
- Broadhead RS, Borch C, Hulst YV, Gauchat G, Tehrani S, Stringer KL, Heckathorn DD, Altice FL, 2012. Relying on injection drug users to access and adhere to HIV therapeutics: Bittersweet lessons using respondent-driven sampling and a peer-driven intervention. J. Drug Issues 127–146. [Google Scholar]
- Broadhead RS, Heckathorn DD, Altice FL, van Hulst Y, Carbone M, Friedland GH, O’Connor PG, Selwyn PA, 2002. Increasing drug users’ adherence to HIV treatment: Results of a peer-driven intervention feasibility study. Soc. Sci. Med 55, 235–246. [DOI] [PubMed] [Google Scholar]
- Broadhead RS, Heckathorn DD, Weakliem DL, Anthony DL, Madray H, Mills RJ, Hughes J, 1998. Harnessing peer networks as an instrument for AIDS prevention: Results from a peer-driven intervention. Pub. Health Rep 113, 42–57. [PMC free article] [PubMed] [Google Scholar]
- Bruce RD, Dvoryak S, Sylla L, Altice FL, 2007. HIV treatment access and scale-up for delivery of opiate substitution therapy with buprenorphine for IDUs in Ukraine--programme description and policy implications. Int. J. Drug Pol 18, 326–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell BK, Fuller BE, Lee ES, Tillotson C, Woelfel T, Jenkins L, Robinson J, Booth RE, McCarty D, 2009. Facilitating outpatient treatment entry following detoxification for injection drug use: A multisite test of three interventions. Psychol. Addict. Behav 23, 260–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capoccia VA, Cotter F, Gustafson DH, Cassidy EF, Ford JH 2nd, Madden L, Owens BH, Farnum SO, McCarty D, Molfenter T, 2007. Making “stone soup”: Improvements in clinic access and retention in addiction treatment. J.t Comm.J. Qual. Patient Saf 33, 95–103. [DOI] [PubMed] [Google Scholar]
- Cappelleri J, Lundy JJ, Hays RD, 2014. Overview of Classical Test Theory and Item Response Theory for quantitative assessment of items in developing patient-reported outcome measures. Clin. Ther 36, 648–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBell D, Carter R, 2005. Impact of transition on public health in Ukraine: Case study of the HIV/AIDS epidemic. BMJ 331, 216–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Mathers B, Wirtz A, Wolfe D, Kamarulzaman A, Carrieri M, Strathdee S, Malinowska-Sempruch K, Kazatchkine M, Beyrer C, 2014. What has been achieved in HIV prevention, treatment and care for people who inject drugs, 2010-2012? A review of the six highest burden countries. Int. J. Drug Pol 25, 53–60. [DOI] [PubMed] [Google Scholar]
- Drukker D, Prucha I, Raciborski R, 2013. Maximum Likelihood and generalized spatial two stage least squares estimators for spatial autoregressive model with spatial autorefressive disturbances. Stata J 13, 221–241. [Google Scholar]
- Elwyn G, O’Connor A, Stacey D, Volk R, Edwards A, Coulter A, Thomson R, Barratt A, Barry M, Bernstein S, Butow P, Clarke A, Entwistle V, Feldman-Stewart D, Holmes-Rovner M, Llewellyn-Thomas H, Moumjid N, Mulley A, Ruland C, Sepucha K, Sykes A, Whelan T, International Patient Decision Aids Standards Collaboration, 2006. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ 333, 417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald JP, McCarty D, 2009. Understanding attitudes towards use of medication in substance abuse treatment: A multilevel approach. Psychol. Serv 6, 74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusco A, Dickes P, 2008. The Rasch model and multidimensional poverty measurement In: Kakwani N,S,J (Ed.), Quantitative approaches to multidimensional poverty measurement. Palgrave Macmillan, New York: pp. 49–62. [Google Scholar]
- Gordon R, McDermott L, Stead M, Angus K 2006. The effectiveness of social marketing interventions for health improvement: What’s the evidence? J. R. Institute Public Health 120, 1133–1139. [DOI] [PubMed] [Google Scholar]
- Hambleton RK, Swaminathan H, Rogers HJ 1991. Fundamentals of Item Response Theory. Sage Publications, Inc., Newbury Park, CA. [Google Scholar]
- Heckathorn D, 2011. Snowball versus Respondent Driven Sampling. Sociol. Methodol 41, 355–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helming B, Thaler J, 2010. On the effectiveness of social marketing – what do we really know? J. Nonprofit Public Sector Market. 22, 264–287. [Google Scholar]
- Hoffman KA, Ford JH 2nd, Choi D, Gustafson DH, McCarty D, 2008. Replication and sustainability of improved access and retention within the Network for the Improvement of Addiction Treatment. Drug Alcohol Depend 98, 63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS), 2016a. Global AIDS Update 2016. Geneva, Switzerland: Pp. Accessed on May 28, 2016 at: http://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS), 2016b. Prevention Gap Report. Geneva, Switzerland: pp. Accessed on July 14, 2016 at: http://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf. [Google Scholar]
- Kahneman D, Tversky A 1984. Choices, values, and frames. Am. Psychol 39, 341–350. [Google Scholar]
- King M, Nazareth I, Lampe F, Bower P, Chandler M, Morou M, Sibbald B, Lai R, 2005. Impact of participant and physician intervention preferences on randomized trials: A systematic review. JAMA 293, 1089–1099. [DOI] [PubMed] [Google Scholar]
- Kutsa O, Marcus R, Bojko M, Zelenev A, Mazhnaya A, Dvoriak S, Filippovych S, Altice FL, 2016. Factors associated with physical and sexual violence by police among people who inject drugs in Ukraine: Implications for retention on opioid agonist therapy. J. Int. Aids Soc 19, 20897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeSage J, Pace RK, 2009. Introduction to Spatial Econometrics. CRC Press/Taylor and Francis Group, LLC, Boca Raton, FL. [Google Scholar]
- Madden L, Farnum S, Eggert K, Quanbeck AR, Freeman R, Ball SA, Schottenfeld RS, Shi JM, Savage ME, Barry DT, 2018. An investigation of an open-access model for scaling up methadone maintenance treatment. Addiction. [Epub ahed of print]. [DOI] [PubMed] [Google Scholar]
- Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, Wodak A, Panda S, Tyndall M, Toufik A, Mattick RP, Reference Group to the UN on HIV and Injecting Drug Use, 2008. Global epidemiology of injecting drug use and HIV among people who inject drugs: A systematic review. Lancet 372, 1733–1745. [DOI] [PubMed] [Google Scholar]
- Mazhnaya A, Bojko MJ, Marcus R, Filippovych S, Islam Z, Dvoriak S, Altice FL, 2016. In their own voices: Breaking the vicious cycle of addiction, treatment and criminal justice among people who inject drugs in Ukraine. Drugs 23, 163–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty D, Chandler RK, 2009. Understanding the importance of organizational and system variables on addiction treatment services within criminal justice settings. Drug Alcohol Depend 103 Suppl 1, S91–S93. [DOI] [PubMed] [Google Scholar]
- McCarty D, Gustafson D, Capoccia VA, Cotter F, 2009. Improving care for the treatment of alcohol and drug disorders. J. Behav. Health Serv. Res 36, 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarty D, Gustafson DH, Wisdom JP, Ford J, Choi D, Molfenter T, Capoccia V, Cotter F, 2007. The Network for the Improvement of Addiction Treatment (NIATx): Enhancing access and retention. Drug Alcohol Depend 88, 138–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Health, Ukranian Center for Disease Control and The National Institute of Epidemiology in the Ukranian Academic of Sciences, 2013. HIV Infection in Ukraine: Informational Bulletin Ukrainian Center for Socially Dangerous Disease Control of the Ministry of Health of Ukraine, L.V. Gromashevsky Institute of Epidemiology and Infectious Diseases of the Academy of Medical Sciences of Ukraine, Kiev, Ukraine. [Google Scholar]
- Mondloch M, Cole D, Frank J, 2001. Does how you do depend on how you think you’ll do? A systematic review of the evidence for a relation between patients’ recovery expectations and health outcomes. Can. Med. Assoc. J 165, 174–179. [PMC free article] [PubMed] [Google Scholar]
- Ostertag S, Wright BRE, Broadhead RS, Altice FL, 2006. Trust and other characteristics associated with health care utilization by injection drug users. J. Drug Issues 36, 953–974. [Google Scholar]
- Rozanova J, Marcus R, Taxman FS, Bojko MJ, Madden L, Farnum SO, Mazhnaya A, Dvoriak S, Altice FL, 2017. Why people who inject drugs voluntarily transition off methadone in Ukraine. Qual. Health Res 27, 2057 – 2070. [DOI] [PubMed] [Google Scholar]
- Salganik MJ, Heckathorn DD, 2004. Sampling and estimation in hidden populations using respondent-driven sampling. Sociol. Methodol 34, 193–239. [Google Scholar]
- Schaub M, Chtenguelov V, Subata E, Weiler G, Uchtenhagen A, 2010. Feasibility of buprenorphine and methadone maintenance programmes among users of home made opioids in Ukraine. Int. J. Drug Policy 21, 229–233. [DOI] [PubMed] [Google Scholar]
- Schwartz R, Kelly S, O’Grady K, Mitchell S, Brown B, 2011. Antecedents and correlates of methadone treatment entry: A comparison of out-of-treatment and in-treatment cohorts. Drug Alcohol Depend 115, 23–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey D, Legare F, Col NF, Bennett CL, Barry MJ, Eden KB, Holmes-Rovner M, Llewellyn-Thomas H, Lyddiatt A, Thomson R, Trevena L, Wu JH, 2014. Decision aids for people facing health treatment or screening decisions. Cochrane Database Systematic Review 4, CD001431. doi: 10.1002/14651858.CD001431.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp, 2015. Stata: Release 14 Statistical Software. StataCorp LP, College Station, TX. [Google Scholar]
- State Statistics Service of Ukraine, 2017. Population and migration: Demographic and social statistics. Kiev, Ukraine. [Google Scholar]
- Torrens M, Fonseca F, Castillo C, Domingo-Salvany A, 2013. Methadone maintenance treatment in Spain: the success of a harm reduction approach. WHO Bulletin 91, 136–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS, 2016. Prevention Gap Report. UNAIDS; Geneva: http://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.