Abstract
When fully implemented, the Affordable Care Act will expand the number of people with health insurance. This raises questions about the capacity of the health care workforce to meet increased demand. I used data on office-based physicians from the 2011 National Ambulatory Medical Care Survey Electronic Medical Records Supplement to summarize the percentage of physicians currently accepting any new patients. Although 96 percent of physicians accepted new patients in 2011, rates varied by payment source: 31 percent of physicians were unwilling to accept any new Medicaid patients; 17 percent would not accept new Medicare patients; and 18 percent of physicians would not accept new privately insured patients. Physicians in smaller practices and those in metropolitan areas were less likely than others to accept new Medicaid patients. Higher state Medicaid-to-Medicare fee ratios were correlated with greater acceptance of new Medicaid patients. The findings serve as a useful baseline from which to measure the anticipated impact of Affordable Care Act provisions that could boost Medicaid payment rates to primary care physicians in some states while increasing the number of people with health care coverage.
The Affordable Care Act will enable approximately twenty-four million people to purchase coverage through insurance exchanges by 2021, and millions more will be able enroll in Medicaid or the Children’s Health Insurance Program.1 Concern has been raised about the capacity of the existing health care workforce to provide care to newly insured people.2,3 Policy makers need appropriate data to evaluate this capacity at the state level both before and after policy changes. Such data have not been available to date.
This article provides a current snapshot of the availability of physician workforce capacity as measured by physicians’ willingness to accept new patients. The article also summarizes for the first time the percentage of office-based physicians accepting new patients with Medicaid for each state, and it explores correlates of physicians’ acceptance of new Medicaid patients. Determining these correlates is important, because previous reports indicate that more than onethird of US physicians do not accept any new Medicaid patients.4
Many factors unrelated to Medicaid policy levers affect the number of Medicaid patients seen by physicians who accept at least some Medicaid patients.Yet the level of Medicaid physician payment has been shown to affect a physician’s willingness to accept any Medicaid patients.5–8 Limited access to office-based physicians has in turn been shown to be one reason why Medicaid patients rely more heavily on care provided in hospital emergency and outpatient departments than do privately insured patients.9
Study Data And Methods
DATA ON ACCEPTANCE OF NEW PATIENTS
The National Ambulatory Medical Care Survey Electronic Medical Records Supplement is conducted by the Centers for Disease Control and Prevention’s National Center for Health Statistics.10 This survey supplement, conducted by mail with telephone follow-up, aims to collect information on physicians’ adoption and use of electronic health records. It is an annual, nationally representative survey of physicians, excluding radiologists, anesthesiologists, and pathologists.
The sampling frame consists of physicians in the masterfiles of the American Medical Association and the American Osteopathic Association who are licensed to practice in the United States and who are identified in the files as being engaged primarily in office-based practice. The 2011 supplement, conducted from February through June 2011, was designed to be representative by state and included questions about physicians’ acceptance of new patients.
Those who accepted new patients were questioned about which payment forms they accepted. The response rate was 64 percent. The conduct of the survey was approved by the National Center for Health Statistics research ethics review board.
ANALYSIS
The percentage of physicians accepting any new patients overall, and with particular payment sources, was estimated from 4,326 physician respondents.11 Acceptance of new patients with Medicaid was compared to acceptance of patients with other payment sources. Acceptance of new patients was also compared for physicians in primary care (general and family practice, internal medicine, and pediatrics) compared to other specialties. Finally, the acceptance rate of new Medicaid patients in each state was compared to the national average.
Analyzing the effects of changes in independent variables on changes in acceptance of new Medicaid patients can help net out the effects of correlation between included independent variables and possible confounders. Because the data currently only allow for estimates of acceptance of new Medicaid patients by state in one year, a full analysis of the relationship between policy variables and acceptance of new Medicaid patients is beyond the scope of this article.
However, given the policy importance of these data going forward, a logit model investigated the association between current acceptance rates for new Medicaid patients and basic physician characteristics and state-level variables expected to be correlated with acceptance of Medicaid patients. Physician characteristics examined included age, sex, number of physicians in the office, specialty category, whether the physician practiced within a Metropolitan Statistical Area, and whether the physician practiced in a county with at least 15 percent of the population below the federal poverty level. This last variable was measured using poverty data by county in 2008.12
State-level variables included the number of Medicaid enrollees per capita,13,14 the Medicaid capitated managed care penetration rate,15 the number of physicians per capita,16 and the Medicaid-to-Medicare fee ratio.17 The latter two variables were measured in the latest year for which data were available, which was 2009 and 2008, respectively.
Because effect size cannot be directly inferred from coefficients of logit models, marginal effects were reported. Marginal effects are calculated as the average change in the predicted probability of acceptance for a one-unit change in each independent variable, holding all other covariates at their observed values. For example, I report the difference in the percentage of physicians predicted to accept new Medicaid patients depending on whether or not a physician is in a primary care specialty.
All analyses used sample weights that yield nationally representative estimates through, for example, inflation by the reciprocals of the probabilities of selection and adjustment for nonresponse by state, Metropolitan Statistical Area status, and fifteen physician specialty groups.18 Standard errors accounted for the design of the survey (for example, allowing clustering of errors by state) using the statistical analysis software Stata, version 12. Two-tailed t-tests were used.
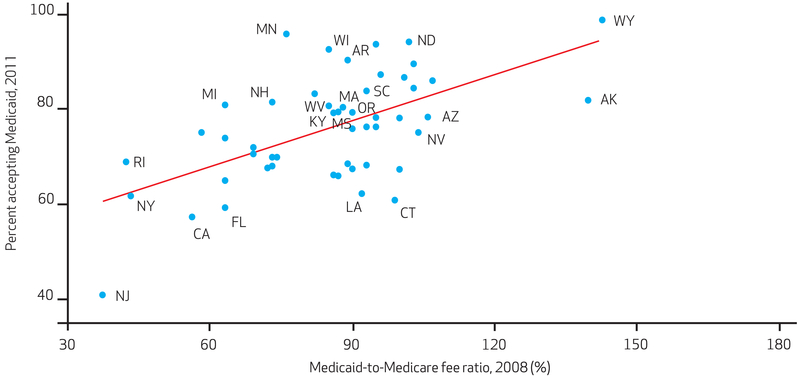
Statistical significance was assessed at p < 0.05. A scatter plot of the average percentage of physicians accepting new Medicaid patients by state and the average Medicaid-to-Medicare physician fee ratio is also provided.
LIMITATIONS
This study has several limitations. Physicians’ acceptance of new patients is a common measure of access to care. For example, the Medicare Payment Advisory Commission annually reports to Congress the percentage of physicians accepting new Medicare patients as one measure of Medicare physician payment adequacy and access to care for Medicare beneficiaries.19 The Medicaid and Children’s Health Insurance Program Payment and Access Commission also reported the percentage of physicians accepting new Medicaid patients in its first report to Congress in 2011.20
However, other measures of access are important, such as the percentage of beneficiaries with a usual source of care and the percentage who do not access care because of their inability to find a participating provider or having to wait a long time for an appointment. If these data were available by state, they might show different patterns than the data presented here. For example, if Medicaid enrollees are more geographically concentrated than other patients, less universal acceptance of Medicaid compared to other payers might not directly translate into access problems for Medicaid patients.
An additional limitation to the current work is that I was unable to include information on other determinants of physicians’ acceptance of Medicaid patients that may be important, such as administrative barriers or delays in receiving payment from Medicaid. Also, the Medicaid-to-Medicare fee ratios included in the multivariate analysis were measured in mid-2008, although the data on acceptance of new Medicaid patients were measured in early 2011. Although it may take physicians a while to respond to changes in Medicaid fees, this difference of more than two years in measurement of these two variables introduced error into the analysis.
The analysis of correlates of state acceptance rates for new Medicaid patients must also be viewed with caution because variables other than but correlated with included predictors may be the ones affecting physician acceptance of new Medicaid patients. This may be the case, although the finding regarding the Medicaid fee ratio is consistent with other work that better identifies a causal relationship between the fee ratio and acceptance of Medicaid patients.5
A final limitation of the current analysis is that the sample size was insufficient to consider acceptance rates by state for subsets of physicians, such as those in primary care.
Study Results
ACCEPTANCE OF ANY NEW PATIENTS
About 96.1 percent of office-based physicians accepted new patients in 2011 (Exhibit 1). The percentage accepting new patients was lower for those in primary care specialties (about 93.8 percent) than for others (97.6 percent).
Exhibit 1.
Percentage Of US Office-Based Physicians Accepting New Patients, By Specialty Category, 2011
| Any new patients |
Medicaid |
Medicarea |
Private insurance |
Self-pay |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| All | 96.1 | (95.0, 97.1) | 69.4 | (67.0, 71.8) | 83.0b | (81.1, 85.0) | 81.7b | (79.7, 83.7) | 91.7b | (90.2, 93.3) |
| By specialty category | ||||||||||
| Primary care | 93.8 | (91.9, 95.6) | 66.2 | (62.7. 69.7) | 71.4b | (68.2, 74.8) | 80.5b | (77.6, 83.5) | 88.2b | (85.7, 90.7) |
| Other specialties | 97.6b | (96.3, 99.0) | 71.7c | (68.4, 75.0) | 90.9b,c | (88.7, 93.2) | 82.6b | (79.9, 85.2) | 94.2b,c | (92.4, 96.1) |
SOURCE National Ambulatory Medical Care Survey Electronic Medical Records Supplement, 2011.
NOTES Excludes cases where response was blank or unknown. “Primary care” includes specialties of general and family practice, internal medicine, and pediatrics. Physicians who do not accept any new patients also do not accept new patients with Medicaid, Medicare, private insurance, or self-pay. CI is confidence interval.
The percentage of office-based physicians accepting Medicare patients is 88.3 percent (95% CI: 86.5, 90.1) if pediatricians are excluded.The percentage of primary care physicians accepting new Medicare patients is 83.2 percent (95 percent CI: 80.0, 86.4) if pediatricians are excluded.
Estimate is significantly different compared to Medicaid at the 5 percent level based on a t test.
Estimate is significantly different compared to primary care at the 5 percent level based on a t test.
ACCEPTANCE OF NEW MEDICAID PATIENTS, BY STATE
Nationally, 69.4 percent of physicians accepted new patients with Medicaid. This was lower than the percentage accepting new selfpay (91.7 percent), Medicare (83.0 percent), or privately insured patients (81.7 percent). Exhibit 2 presents state-level estimates of physician acceptance of new Medicaid patients. Although precise estimates are presented, readers should be cautious not to interpret small differences between states as differences that are statistically significant.
Exhibit 2.
Percentage Of US Office-Based Physicians Accepting New Medicaid Patients, 2011
| State | Estimate | 95% confidence interval |
|---|---|---|
| All | 69.4 | 67.0, 71.8 |
| NJ | 40.4a | 27.9, 52.9 |
| CA | 57.1 | 43.0, 71.1 |
| FL | 59.1 | 48.2, 69.9 |
| CT | 60.7 | 49.2, 72.2 |
| TN | 61.4 | 49.3, 73.5 |
| NY | 61.6 | 49.6, 73.6 |
| LA | 62.1 | 50.0, 74.2 |
| IL | 64.9 | 51.9, 77.8 |
| MD | 65.9 | 54.1, 77.7 |
| CO | 66.1 | 54.7, 77.5 |
| OK | 67.3 | 56.9, 77.8 |
| GA | 67.4 | 57.1, 77.7 |
| MO | 67.6 | 56.9, 78.2 |
| PA | 68.0 | 57.9, 78.1 |
| KS | 68.2 | 57.2, 79.2 |
| AL | 68.5 | 58.0, 79.0 |
| RI | 68.9 | 58.1, 79.7 |
| HI | 69.9 | 58.3, 81.5 |
| TX | 69.9 | 60.1, 79.8 |
| IN | 70.6 | 59.7, 81.5 |
| OH | 72.0 | 61.8, 82.2 |
| ME | 74.0 | 63.7, 84.3 |
| DC | 75.2 | 57.5, 92.9 |
| NV | 75.2 | 64.1, 86.4 |
| VA | 76.0 | 67.2, 84.8 |
| WA | 76.4 | 66.0, 86.8 |
| NC | 76.4 | 67.6, 85.2 |
| DE | 78.3 | 67.8, 88.8 |
| VT | 78.4 | 69.6, 87.3 |
| AZ | 78.5 | 68.7, 88.3 |
| KY | 79.4a | 70.6, 88.3 |
| OR | 79.5a | 69.9, 89.2 |
| MS | 79.6a | 70.4, 88.7 |
| MA | 80.6a | 71.5, 89.6 |
| WV | 80.9a | 72.4, 89.5 |
| MI | 81.1a | 70.6, 91.6 |
| NH | 81.7a | 73.4, 90.0 |
| AK | 82.1a | 73.6, 90.7 |
| UT | 83.5a | 76.0, 91.0 |
| SC | 84.1a | 71.4, 96.9 |
| ID | 84.7a | 75.5, 94.0 |
| NM | 86.3a | 79.0, 93.7 |
| NE | 87.0a | 79.4, 94.6 |
| IA | 87.6a | 80.2, 94.9 |
| MT | 89.9a | 83.3, 96.6 |
| AR | 90.7a | 84.5, 97.0 |
| WI | 93.0a | 87.5, 98.5 |
| SD | 94.1a | 88.4, 99.8 |
| ND | 94.6a | 89.1, 100.0 |
| MN | 96.3a | 92.1, 100.4 |
| WY | 99.3a | 97.9, 100.7 |
SOURCE National Ambulatory Medical Care Survey Electronic Medical Records Supplement, 2011
NOTES N = 3,979. Excludes cases where acceptance was blank or unknown
Estimate is significantly different from the national average at the 5 percent level.
The state with the lowest percentage of physicians accepting new Medicaid patients was New Jersey (about 40.4 percent). There, physicians were significantly less likely than the national average to accept new Medicaid patients. The state with the second-lowest acceptance rate for new Medicaid patients was California (57.1 percent), although the p value for the comparison of California’s rate with the national average was only 0.06.
Twenty-one states had acceptance rates for new Medicaid patients that were significantly higher than those of other states. These states included several in the Midwest and West, two states in New England (Massachusetts and New Hampshire), and five in the South (Arkansas, Kentucky, Mississippi, South Carolina, and West Virginia).
CORRELATES OF ACCEPTANCE OF NEW MEDICAID PATIENTS
Physicians in solo practice were 23.5 percentage points less likely to accept new Medicaid patients than physicians in offices with at least ten other physicians (Exhibit 3). This is a 34 percent difference relative to the average percentage of physicians accepting new Medicaid patients (69.4 percent; Exhibit 1). Primary care physicians were 7.3 percentage points (11 percent) less likely and physicians outside of Metropolitan Statistical Areas were 12.9 percentage points (19 percent) more likely, respectively, than others to accept new Medicaid patients.
Exhibit 3.
Characteristics Associated With Acceptance Of New Medicaid Patients Among US Office-Based Physicians, 2011
| Marginal effect from logit model |
|||
|---|---|---|---|
| Independent variable | Percent of sample |
Estimate | 95% CI |
| PHYSICIAN CHARACTERISTICS | |||
| Female | 27.4 | −2.0 | (−7.5, 4.8) |
| PHYSICIAN AGE (RELATIVE TO UNDER 45 YEARS OLD) | |||
| 45–54 years | 28.5 | −0.5 | (−6.6, 5.7) |
| 55–64 years | 31.9 | −2.7 | (−8.9, 3.5) |
| 65 years and older | 13.7 | −7.5 | (−16.3, 1.3) |
| NUMBER OF PHYSICIANS IN THE OFFICE(RELATIVE TO 11+ PHYSICIANS) | |||
| Solo practice | 28.0 | −23.5b | (−31.1, 15.9) |
| Two physicians | 10.1 | −21.5b | (−30.6, 12.4) |
| 3–5 physicians | 27.3 | −7.0 | (−13.8, 0.09) |
| 6–10 physicians | 18.7 | −2.7 | (−10.0, 4.2) |
| OTHER PHYSICIAN OR OFFICE CHARACTERISTICS | |||
| Primary care specialties | 41.6 | −7.3b | (−12.0, 2.7) |
| Not in a Metropolitan Statistical Area | 12.0 | 12.9b | (6.8, 19.0) |
| REGION (RELATIVE TO NORTHEAST) | |||
| Midwest | 21.2 | 8.2b | (1.8, 14.6) |
| South | 37.3 | −0.4 | (−8.4, 7.5) |
| West | 20.3 | 0.3 | (−11.4,11.9) |
| POVERTY STATUS | |||
| At least 15% of the 2008 population in poverty in the county where the practice is located | 28.5 | 8.4b | (2.4, 14.5) |
| Marginal effect from logit model |
|||
|---|---|---|---|
| State-level variables | Mean | Estimate | 95% CI |
| Medicaid-to-Medicare fee ratio (2008)a | 74.2 | 0.4b | (0.2, 0.5) |
| Physicians per 10 million population (2009) | 8.6 | 0.8 | (−0.9, 2.5) |
| Medicaid enrollees per 100,000 population (2010) | 1.7 | 4.2 | (−1.4, 9.8) |
| Managed care (other than primary care case management)penetration (2010, per 100) | 0.5 | 1.8 | (−5.4, 9.0) |
SOURCE National Ambulatory Medical Care Survey Electronic Medical Records Supplement, 2011.
NOTES N = 3,979. Excludes cases where acceptance was blank or unknown. Also excludes Tennessee because of missing data on the Medicaid-to-Medicare fee ratio. “Primary care” includes specialties of general and family practice, internal medicine, and pediatrics. CI is confidence interval.
Based on the logit parameter estimates, an increase in the fee ratio from 74.2 to 100.0 would be expected to increase acceptance of new Medicaid patients from 70.0 percent (95% CI: 67.7, 72.2) to 78.6 percent (95% CI: 75.4, 81.7), a difference of 8.6 percentage points (95% CI: 5.2, 12.0, p < 0.001).
Significant at the 5 percent level based on a t test.
Physicians in the Midwest were 8.2 percentage points (12 percent) more likely than those in the Northeast to accept new Medicaid patients. Not surprisingly, physicians practicing in counties where at least 15 percent of the population was under the federal poverty level were more likely—by about 8.4 percentage points (12 percent)—than others to accept new Medicaid patients.
Controlling for other factors, acceptance of new Medicaid patients across states was not significantly associated with the percent of Medicaid enrollees in the state, the percentage of the Medicaid population in capitated managed care plans, or the number of physicians per capita in the state. However, acceptance rates of new Medicaid patients were higher in states with higher Medicaid-to-Medicare fee-for-service fee ratios. On average, a ten-percentage-point increase in the fee ratio raised the acceptance of new Medicaid patients by four percentage points.
Using the logit parameter estimates, raising Medicaid fees to Medicare levels for all physicians, a 25.8-percentage-point increase in fees relative to the current average ratio of 74.2, would be predicted to be associated with an increase in the acceptance rate of new Medicaid patients from an average of 70.0 percent across physicians to an average of 78.6 percent—a difference of 8.6 percentage points (12 percent) (p < 0.001). This 78.6 percent predicted acceptance rate for new Medicaid patients is much closer than 70.0 percent to the current acceptance rates for new privately insured (81.7 percent) and Medicare (83.1 percent) patients. Exhibit 4 also plots the data on acceptance of new Medicaid patients and the Medicaid-to-Medicare fee ratio by state.
Exhibit 4. Percentage Of US Office-Based Physicians Accepting New Medicaid Patients In 2011 And The Medicaid-To-Medicare Fee Ratio.
sources National Ambulatory Medical Care Survey Electronic Medical Records Supplement, 2011; and Note 17 in text. NOTES The line pictured is from an ordinary least squares regression of the percentage of US office-based physicians accepting new patients, by state, on the fee ratio. Data points represent all fifty states and Washington, D.C., but only selected points are labeled.
Although not reported, the analysis in Exhibit 3 was also run considering only physicians in primary care. Results were similar to those for all physicians. For example, an increase in the Medicaid-to-Medicare fee ratio for primary care to 100 was predicted to increase acceptance of new Medicaid patients among primary care physicians from 64.7 percent to 71.7 percent—a difference of 7.0 percentage points (11 percent) (p = 0.06).
Although also not reported, interactions introduced one by one between the fee ratio and the indicator for having a high poverty rate in the county, the state Medicaid managed care penetration rate, and the indicator for being outside of a Metropolitan Statistical Area were not significant in either the model for all physicians or the one for physicians in primary care only.
Discussion
About 96 percent of office-based physicians accepted new patients in 2011, although the percentage was lower for primary care physicians than for other specialties. The percentage of physicians accepting new patients with Medicaid was lower than the percentage accepting new self-pay, Medicare, or privately insured patients. Physicians in smaller practices and those practicing in Metropolitan Statistical Areas were less likely than others to accept new Medicaid patients.
Acceptance rates for new Medicaid patients varied greatly across states. Physicians in New Jersey were the least likely to accept new Medicaid patients. Also, the acceptance rate for new Medicaid patients was positively associated with the average Medicaid-to-Medicare fee ratio in a state.
If Affordable Care Act provisions are implemented as planned, Medicaid payment rates for primary care services provided by primary care physicians will increase to 100 percent of Medicare rates in 2013 and 2014. This will greatly affect Medicaid payment rates in some states, including New Jersey and California, where the 2008 ratios were 37 percent and 56 percent respectively (and 41 percent and 47 percent, respectively, for primary care).17
Prior evidence suggests that physicians’ acceptance of Medicaid patients will increase as Medicaid payment rates increase.5 Evidence also suggests that this may increase the number of times that a Medicaid patient sees a physician and decrease reliance on hospitals for outpatient care.9
However, several questions remain. The fact that the planned increases are temporary could mitigate their impact. Also, evidence of the relationship between Medicaid physician fees and physicians’ participation in Medicaid relied on past changes in state fee ratios that were mostly smaller than the increase that is expected to occur in 2013 for some states. It is difficult to predict physicians’ responses to increases in fee ratios of a magnitude that has rarely occurred in the past. Finally, the number of people with health care coverage through Medicaid and the exchanges is expected to increase at the same time as Medicaid payment rates for primary care physicians are expected to increase in some states. This raises a question about the capacity of the health care workforce to meet this increased demand. The data in this article provide an important baseline available to use in monitoring this question.
Acknowledgments
The findings and conclusions in this article are those of the author and do not necessarily represent the views of the Centers for Disease Control and Prevention or the Office of the National Coordinator for Health Information Technology (ONC).The author thanks the ONC for funding the survey supplement; Jane Sisk, Susan Schappert, and Chun-Ju Hsiao for help with the data; and Clarice Brown, Jennifer Madans, Genevieve M. Kenney, and other participants in the conference “Measuring Primary Care Access” at the University of Pennsylvania, April 13, 2012, for helpful comments on a previous draft.
ABOUT THE AUTHOR: SANDRA L. DECKER

Sandra L. Decker is an economist at the National Center for Health Statistics.
In this month’s Health Affairs, Sandra Decker reports on her analysis of national survey data to determine what percentage of physicians in 2011 were accepting any new patients, including those on Medicaid. The survey data show that 31 percent of physicians were unwilling to accept any new Medicaid patients, versus 17 percent who would not accept new Medicare patients and 18 percent of physicians who would not accept new privately insured patients. Fees may be a major contributor to the differential. Decker says that the state-by-state findings “serve as a useful baseline” from which to measure how raising Medicaid rates in some states will affect the willingness of primary care physicians to take on new Medicaid patients.
Decker is an economist at the National Center for Health Statistics. Previously, she worked as an analyst at the International Longevity Center–USA; was on the faculty of the School of Public Service at New York University; served as a research economist at the National Bureau of Economic Research; and had work funded by the National Institute on Aging, the Robert Wood Johnson Foundation, and the Commonwealth Fund. Most of her research focuses on causal connections between state Medicaid eligibility or provider reimbursement rules on the one hand and insurance status, use of health care services, and health outcomes for vulnerable populations on the other. She holds a doctorate in economics from Harvard University.
NOTES
- 1.Congressional Budget Office. CBO’s analysis of the major health care legislation enacted in March 2010. Washington (DC): CBO; 2011. March 30. [Google Scholar]
- 2.Goodson JD. Patient Protection and Affordable Care Act: promise and peril for primary care. Ann Int Med. 2010;152(11):742–4. [DOI] [PubMed] [Google Scholar]
- 3.Ku L, Jones K, Shin P, Bruen B, Hayes K. The states’ next challenge— securing primary care for expanded Medicaid populations. N Engl J Med. 2011;364(6):493–5. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. QuickStats: percentage of office-based physicians accepting new patients, by type of payment accepted—United States, 1999–2000 and 2008–2009. MMWR Morb Mortal Wkly Rep. 2011;60(27):928. [Google Scholar]
- 5.Decker SL. The effect of physician reimbursement levels on the primary care of Medicaid patients. Review Econ Househ. 2011;5(1):95–112. [Google Scholar]
- 6.Showalter MH. Physicians’ cost shifting behavior: Medicaid versus other patients. Contemporary Econ Pol. 1997;15(2):74–84. [Google Scholar]
- 7.Cohen JW. Medicaid physician fees and use of physician and hospital services. Inquiry. 1993;30:281–92. [PubMed] [Google Scholar]
- 8.Sloan F, Mitchell J, Cromwell J. Physician participation in state Medicaid programs. J Hum Resour. 1978;13:211–45. [PubMed] [Google Scholar]
- 9.Decker SL. Medicaid physician fees and ambulatory care of Medicaid patients. Inquiry. 2009;46(3): 291–304. [DOI] [PubMed] [Google Scholar]
- 10.National Center for Health Statistics. National Ambulatory Medical Care Survey: Electronic Medical Records Supplement 2011 [Internet]. Hyattsville (MD): NCHS; [cited 2011. October 25]. Available from: from: http://www.cdc.gov/nchs/data/ahcd/2011_EMR_Survey.pdf [Google Scholar]
- 11.Information was presented for physicians who responded to each particular question, yielding a sample that was 1 percent, 8 percent, 6 percent, 4 percent, and 4 percent, respectively, less than 4,326 because of item nonresponse for any new patients and patients with payment sources of Medicaid, Medicare, private insurance, and self-pay, respectively.
- 12.Resources Health and Administration Services. Area Resource File— 2009/2010. Rockville (MD): HRSA; 2009. [Google Scholar]
- 13.Kaiser Commission on Medicaid and the Uninsured. Medicaid enrollment: December 2010 data snapshot [Internet]. Washington (DC): The Commission; 2011 Dec [cited 2012. July 3]. (Medicaid Facts). Available from: http://www.kff.org/medicaid/upload/8050-04.pdf [Google Scholar]
- 14.Census Bureau. Resident population data [Internet]. Washington (DC): The Bureau; [cited 2012. July 3]. Available from: http://2010.census.gov/2010census/data/apportionment-pop-text.php [Google Scholar]
- 15.Kaiser Commission on Medicaid and the Uninsured. A profile of Medicaid managed care programs in 2010: findings from a 50-state survey. Washington (DC): The Commission; 2011. Sep. [Google Scholar]
- 16.American Medical Association. Physician characteristics and distribution in the U.S., 2011 [Internet].Chicago (IL): AMA; 2011. [cited 2012 July 3]. Available for purchase from: http://amascb.pdn.ipublishcentral.com/product/physiciancharacteristics-distribution-in-us-2011 [Google Scholar]
- 17.Zuckerman S, Williams AF, Stockley KE. Trends in Medicaid physician fees, 2003–2008. Health Aff (Millwood). 2009;28(3):w510–9. DOI: 10.1377/hlthaff.28.3.w510. [DOI] [PubMed] [Google Scholar]
- 18.Goldberg EJ, Shimizu IM. Specifications for state level estimates for 2010 EMR Mail Survey. Hyattsville (MD): National Center for Health Statistics; 2011. September 29. Unpublished document. [Google Scholar]
- 19.Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy. Washington (DC): MedPAC: 2012. March. [Google Scholar]
- 20.Medicaid and CHIP Payment and Access Commission. Report to Congress on Medicaid and CHIP. Washington (DC): MACPAC;2010. Mar. [Google Scholar]