Abstract
Introduction
Although a handful of studies have examined mortality among caregivers of persons with Alzheimer's disease or a related dementia (ADRD), the proportion of caregivers who die before their cognitively impaired care recipients remains unknown.
Methods
We conducted descriptive and survival analyses on up to 17 years of data from the nationally representative Health and Retirement Study to evaluate the proportion of spouse caregivers who died before their care recipients.
Results
Eighteen percent of spouse ADRD caregivers died before their care recipients, and spouse caregivers had a significantly lower risk of mortality than their husbands or wives with ADRD.
Discussion
Although a large majority of spouse ADRD caregivers will likely not die before their cognitively impaired husband or wife, those persons with ADRD who survive longer than their caregivers are worthy of future inquiry given their potential risk for negative health outcomes.
Keywords: Alzheimer’s disease, Dementia, Mortality, Caregiver, Timing
1. Introduction
There is a well-established scientific literature that documents the adverse health implications of family care for persons with Alzheimer's disease or related dementias (ADRDs). The accumulation of emotional, social, and physical stressors of ADRD caregiving has led several investigators to examine if family caregivers are at risk for expedited mortality when compared to non-ADRD caregivers or noncaregivers. Among caregivers of persons who were hospitalized, those who helped persons with ADRD were more likely to die over the course of a year than non-ADRD caregivers [1]. Available syntheses of population-based studies, however, suggest mixed overall effects of caregiving status on mortality [2]. In brief, the available findings imply that caregiving itself is not associated with an increased risk of death. Rather, an individual's appraisals of the stress and strain of care responsibilities moderate the effect of caregiving on mortality [3].
To our knowledge, no study has examined the number of ADRD caregivers who die before a care recipient with dementia. This is a potentially important concern from a public health perspective; the absence of a family caregiver likely complicates the management of ADRD and is linked to adverse outcomes such as nursing home admission [4]. This analysis thus sought to generate empirical evidence to determine the proportion of dementia caregivers who die before their care recipients.
2. Dementia caregiver mortality using the Health and Retirement Study
We used nationally representative longitudinal data from the Health and Retirement Study (HRS) to compare the risk of mortality between persons with ADRD and their spouse caregiver. The HRS attempts to follow up all respondents until death and collects detailed sociodemographic, physical, mental, and cognitive health data on a respondent and their spouse [5].
Using the HRS, we identified individuals with ADRD and their spouse (i.e., dyads). An individual was classified as having ADRDs if they ever reported having memory problems, Alzheimer's disease, dementia, or had a RAND HRS dementia probability weight of >0.50 [6], [7]. We then identified dyads in which the person with ADRD, or their proxy, reported receiving help from their spouse for any of the following functional tasks: help to cross a room, dress, bathe, eat, get into and out of bed, use the toilet, prepare meals, grocery shop, make telephone calls, or take medications. We limited our analysis to dyads in which a person with ADRD was observed not needing functional help from a spouse in a prior interview but then receiving spousal functional support in a subsequent interview. The point of needing functional assistance, regardless of ADRD status at the time, served as the first year (i.e., baseline) of the person with ADRD receiving caregiving.
We excluded individuals with ADRD who were never married or that had multiple marriages, dyads where both individuals had ADRDs, dyads where the cognitively intact spouse did not provide functional support for the person with ADRD, dyads where both the person with ADRD and the spouse provided functional support for each other, dyads where both the person with ADRD and their spouse were not living in the community at baseline, and dyads with any missing data on control variables (described below). Finally, owing to the inconsistent wording of cognitive questions in earlier HRS waves, we limited our analysis to HRS years 1998–2014.
We conducted two sets of analyses to ascertain whether spouse caregivers experience a greater risk of mortality than persons with ADRD. First, we counted the number of dyads in which the spouse caregiver died before the person with ADRD, the number of dyads in which the spouse caregiver died after the person with ADRD, and the number of dyads in which no mortality event had yet to be observed. Among the dyads that experienced a mortality event, we tested the equality of the proportion of dyads in which the caregiver died before the person with ADRD to the proportion of dyads in which the person with ADRD died before the spouse caregiver. We also estimated a logistic regression model in which we compared the demographic characteristics of caregivers (age at baseline, gender, race, years of education, region of residence, number of chronic conditions, self-reported health status, and number of children) who died before (coded 1) or after the person with ADRD (coded 0).
Second, we generated survival curves for spouse caregivers and persons with ADRD using the Kaplan-Meier method and we compared their curves using the log-rank test. We also estimated a Cox proportional hazards model that included an indicator for if the person was a spouse caregiver or person with ADRD and controlled for both the caregiver's and ADRD person's age at baseline, gender, race, years of education, region of residence, number of chronic conditions, self-reported health status, and number of children. Standard errors were clustered at the dyad level, and all analyses were conducted in Stata, version 14.2 (Stata, College Station, TX).
3. Comparison of mortality among persons with dementia and their spousal caregiver
We identified 4725 individuals in the HRS that met our definition of ADRDs. Following the exclusion criteria, our analytic sample consisted of 926 individuals (463 persons with ADRD and 463 spouse caregivers) or 463 dyads. The mean age of persons with ADRD was 74.30 (SD 8.78) years and 38% were female. Spouse caregivers had a mean age of 71.77 (SD 8.72) years and 62% were female (Table 1).
Table 1.
Sample characteristics at baseline (N = 463 dyads)
| Variable | Spouse caregiver | Person with Alzheimer's disease or a related dementia (ADRD) |
|---|---|---|
| Mean age (SD) | 71.77 (8.72) | 74.30 (8.78) |
| Female, n (%) | 285 (62) | 177 (38) |
| Mean number of comorbidities (SD) | 1.83 (1.22) | 2.56 (1.53) |
| Mean years of education (SD) | 12.40 (3.08) | 11.72 (3.56) |
| Mean number of children (SD) | 3.26 (2.07) | |
| Race, n (%) | ||
| Caucasian | 406 (87) | 399 (86) |
| African American | 45 (10) | 48 (10) |
| Other | 12 (3) | 16 (4) |
| Self-reported health, n (%) | ||
| Excellent | 53 (11.45) | 17 (3.67) |
| Very good | 151 (32.61) | 117 (25.27) |
| Good | 151 (32.61) | 141 (30.45) |
| Fair | 86 (18.57) | 143 (30.89) |
| Poor | 22 (4.75) | 143 (30.89) |
| Region of residence, n (%) | ||
| Northeast | 71 (15.33) | |
| Midwest | 122 (26.35) | |
| South | 191 (41.25) | |
| West | 77 (16.63) | |
| Other | 2 (0.43) | |
Median length of follow-up was 6.21 years, and 483 total deaths were observed in the sample. In 18% (n = 83) of the dyads, the spouse caregiver died before the person with ADRD, in 57% (n = 265) of the dyads the person with ADRD died before the spouse caregiver, in 0.43% (n = 2) of the dyads both the person with ADRD and spouse caregiver died on the same day, and in 24% (n = 113) of dyads both the person with ADRD and spouse caregiver were still alive at the last HRS interview.
Among the dyads that experienced a mortality event (n = 348), there were significantly fewer dyads in which the caregiver died before the person with ADRD (P < .001). In the logistic regression model comparing the characteristics of caregivers who died before (n = 83) or after the person with ADRD (n = 265), only caregiver gender was associated with mortality (Table 2). Specifically, female caregivers compared with male caregivers (odds ratio 0.26, 95% CI: 0.15, 0.46) were significantly less likely to die before the person with ADRD than after the person with ADRD.
Table 2.
Odds of spouse caregiver dying before person with Alzheimer's disease or a related dementia (ADRD)
| Variable | Odds ratio | 95% Confidence interval | P-value |
|---|---|---|---|
| Baseline age | 1.03 | 1.00, 1.07 | 0.058 |
| Gender (ref: Female) | 0.26 | 0.15, 0.46 | 0.000 |
| Number of comorbidities | 1.23 | 0.98, 1.56 | 0.074 |
| Years of education | 0.95 | 0.88, 1.00 | 0.267 |
| Number of children | 0.91 | 0.79, 1.05 | 0.226 |
| Race (ref: Caucasian) | |||
| African American | 1.86 | 0.79, 4.36 | 0.157 |
| Other | 2.20 | 0.35, 13.00 | 0.400 |
| Self-reported health (ref: Excellent) | |||
| Very good | 1.19 | 0.39, 3.50 | 0.761 |
| Good | 2.00 | 0.68, 5.83 | 0.206 |
| Fair | 2.56 | 0.83, 7.90 | 0.103 |
| Poor | 4.00 | 0.97, 16.4 | 0.054 |
| Region of residence (ref: Northeast) | |||
| Midwest | 1.24 | 0.49, 3.10 | 0.654 |
| South | 1.48 | 0.61, 3.63 | 0.388 |
| West | 2.00 | 0.72, 5.54 | 0.182 |
| Other | 1.39 | 0.05, 41.2 | 0.850 |
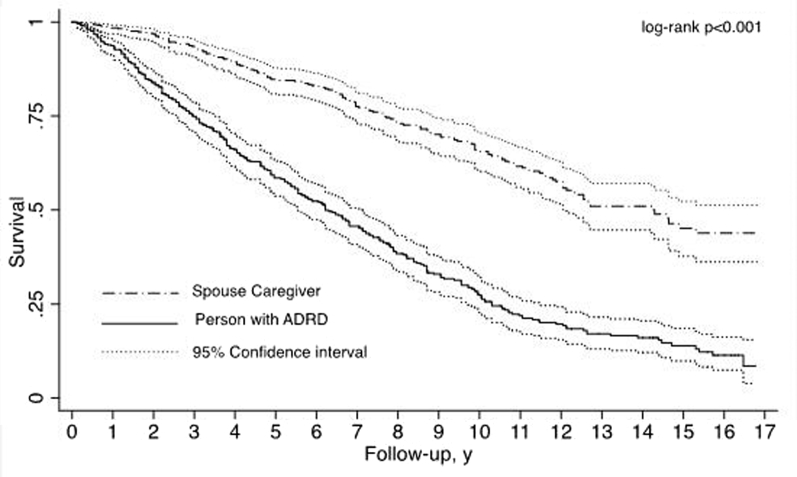
Spousal caregivers had significantly longer survival compared to the person with ADRD (Fig. 1; log-rank P < .001). In the Cox proportional hazard model, being a spouse caregiver was associated with a significantly lower risk of death (hazard ratio 0.63, 95% CI: 0.51, 0.78). Factors independent of caregiving status associated with a greater risk of death for both the spouse caregiver and person with ADRD included older age at baseline, being male, more years of education, having chronic conditions, and self-reported health as fair or poor compared to excellent.
Fig. 1.
Kaplan-Meier survival curves for spouse caregivers and persons with ADRD–current version. Abbreviation: ADRD, Alzheimer's disease or a related dementia.
4. Implications of dementia caregivers dying before care recipients with dementia
The findings demonstrate that a large majority of spouses caring for a partner with ADRD will outlive their cognitively impaired husband or wife. The notion that most ADRD caregivers die before their care recipients is easily dismissed given that the largest proportion of family caregivers of persons with ADRD are adult daughters [8], [9]. The inherent differences in age between adult child caregivers and their care recipients make it unlikely that a large percentage of caregivers die before the person with ADRD. However, a considerable percentage of ADRD caregivers are spouses, and because of the large body of research documenting the various health implications of dementia caregiving, it is necessary to examine the prevalence and timing of mortality among persons with ADRD and their spousal caregivers.
It is also important to note that a small proportion of ADRD caregivers do pass away before their care recipients, and the care recipients in this situation warrant future inquiry. In particular, care recipients with ADRD who are bereaved may experience particular hardships in the form of disruptions to at-home care routines and help. Additional research that describes this subpopulation of people with ADRD (e.g., racial and ethnic background) and the health ramifications of caregiver loss for these individuals would yield important insights. Subsequent work could then develop and evaluate interventions to address the needs and safety concerns for these individuals and identify effective models of support (“gatekeeper” approaches, assistive technologies, etc.) [10].
This study has several limitations. The HRS only includes detailed mortality data on spouse caregivers and limited mortality data on other caregivers (e.g., adult children). We excluded individuals who never married or were married multiple times from our analysis, and this may limit the generalizability of our findings. Although the HRS is nationally representative, our analytic sample was predominantly Caucasian, which fails to capture the diversity of the US and the aging population. Our method of classifying individuals with dementia was dependent on individuals self-reporting (or a proxy) having memory impairment, Alzheimer's disease, dementia, or having a validated RAND HRS dementia probability weight of >0.50. This approach does not provide a detailed diagnostic classification of cause of dementia. The average caregiver and care recipient in our sample obtained over 11 years of education. Years of education was positively associated with mortality, which is contrary to expectation. This result may be a reflection of variation within those who are highly educated and not be true of the general population.
The findings emphasize that for a sizable proportion of persons with ADRD, their spousal caregivers do not die before them. The long-term trajectory of ADRD family caregiving, often lasting to the end of life (and beyond) of care recipients, has led to some scholars to consider it a “career” highlighted by key transitions (onset, institutionalization, bereavement). The caregiving career demands a longitudinal perspective when both describing and intervening upon [11], [12]. However, the nearly 1 in 5 persons with ADRD whose spouse did die before them represent an important subpopulation that heretofore has received little scientific attention. Future descriptive and clinical research that considers the health ramifications of outliving a family caregiver, subgroups at risk for this scenario, and effective interventions to support and sustain persons with ADRD living alone or without an available caregiver would advance the field of dementia care services and supports.
Research in Context.
-
1.
Systematic review: Available syntheses of population-based studies suggest mixed overall effects of caregiving status on mortality. To our knowledge, no study has examined the number of caregivers who die before a care recipient with Alzheimer’s disease and related dementia (ADRD). This analysis sought to generate empirical evidence to determine the proportion of dementia spousal caregivers who die before their care recipients.
-
2.
Interpretation: Less than one in five spousal caregivers died before their partner with dementia.
-
3.
Future directions: The findings emphasize that for a sizable proportion of persons with ADRD, their spousal caregivers do not die before them. However, future research that considers the health ramifications of outliving a family caregiver, subgroups at risk for this scenario, and effective interventions to support persons with ADRD living alone is needed.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
The authors have declared that no conflict of interest exists.
Appendix.
Appendix Table 1.
Proportional hazard model for risk of death
| Variable | Hazard ratio (95% Confidence interval) |
|---|---|
| Spouse caregiver | 0.63 (0.51, 0.78) |
| Baseline age | 1.08 (1.06, 1.10) |
| Female | 0.63 (0.52, 0.78) |
| Number of comorbidities | 1.23 (1.15, 1.31) |
| Years of education | 1.04 (1.01, 1.07) |
| Number of children | 0.98 (0.93, 1.04) |
| Race (ref = Caucasian) | |
| African American | 0.84 (0.61, 1.15) |
| Other | 0.73 (0.31, 1.70) |
| Self-reported health (ref = excellent) | |
| Very good | 1.45 (0.70, 3.00) |
| Good | 2.00 (0.99, 4.01) |
| Fair | 2.40 (1.19, 4.82) |
| Poor | 5.65 (2.74, 11.67) |
| Residence region (ref = Northeast) | |
| Midwest | 1.19 (0.90, 1.58) |
| South | 1.13 (0.87, 1.48) |
| West | 1.30 (0.94, 1.79) |
| Other | 1.55 (0.69, 3.50) |
Appendix Table 2.
Sample characteristics at baseline of dyads where spouse caregiver dies before person with Alzheimer's disease or a related dementia (ADRD) (n = 83 dyads)
| Variable | Spouse caregiver | Person with ADRD |
|---|---|---|
| Mean age (SD) | 75.41 (7.78) | 75.93 (7.41) |
| Female, n (%) | 29 (34.94) | 54 (65.06) |
| Mean number of comorbidities (SD) | 2.28 (1.25) | 2.18 (1.30) |
| Mean years of education (SD) | 11.83 (3.52) | 11.78 (3.74) |
| Mean number of children (SD) | 2.87 (1.91) | |
| Race, n (%) | ||
| Caucasian | 71 (85.54) | 72 (86.75) |
| African American | 10 (12.05) | 10 (12.05) |
| Other | 2 (2.41) | 1 (1.20) |
| Self-reported health, n (%) | ||
| Excellent | 5 (6.02) | 3 (3.61) |
| Very good | 15 (18.07) | 8 (9.64) |
| Good | 29 (34.94) | 24 (28.92) |
| Fair | 25 (30.12) | 27 (32.53) |
| Poor | 9 (10.84) | 21 (25.30) |
| Region of residence, n (%) | ||
| Northeast | 9 (10.84) | |
| Midwest | 22 (26.51) | |
| South | 36 (43.37) | |
| West | 16 (19.28) | |
| Other | 0 (0.00) | |
References
- 1.Christakis N.A., Allison P.D. Mortality after the hospitalizaion of a spouse. N Engl J Med. 2006;354:719–730. doi: 10.1056/NEJMsa050196. [DOI] [PubMed] [Google Scholar]
- 2.Roth D.L., Fredman L., Haley W.E. Informal caregiving and its impact on health: a reappraisal from population-based studies. Gerontologist. 2015;55:309–319. doi: 10.1093/geront/gnu177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perkins M., Howard V.J., Wadley V.G., Crowe M., Safford M.M., Haley W.E. Caregiving strain and all-cause mortality: evidence from the REGARDS Study. J Gerontol B Psychol Sci Soc Sci. 2013;68:504–512. doi: 10.1093/geronb/gbs084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaugler J.E., Duval S., Anderson K.A., Kane R.L. Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Juster F.T., Suzman R. An overview of the Health and Retirement Study. J Hum Resour. 1995;30:S7–S56. [Google Scholar]
- 6.Kelley A.S., McGarry K., Gorges R., Skinner J.S. The burden of health care costs for patients with dementia in the last 5 years of life. Ann Intern Med. 2015;163:729–736. doi: 10.7326/M15-0381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hurd M.D., Martorell P., Delavande A., Mullen K.J., Langa K.M. Monetary costs of dementia in the United States. N Engl J Med. 2013;368:1326–1334. doi: 10.1056/NEJMsa1204629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Friedman E.M., Shih R.A., Langa K.M., Hurd M.D. US prevalence and predictors of informal caregiving for dementia. Health Aff. 2015;34:1637–1641. doi: 10.1377/hlthaff.2015.0510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kasper J.D., Freedman V.A., Spillman B.C., Wolff J.L. The disproportionate impact of dementia on family and unpaid caregiving to older adults. Health Aff. 2015;34:1642–1649. doi: 10.1377/hlthaff.2015.0536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gould E. National Research Summit on Care, Services, and Supports for Persons with Dementia and their Caregivers; October 17, 2017. 2017. Living alone with dementia: Identification, unmet needs, and safety concerns. Bethesda, MD. [Google Scholar]
- 11.Aneshensel C.S., Pearlin L.I., Mullan J.T., Zarit S.H., Whitlatch C.J. Academic Press; San Diego: 1995. Profiles in caregiving: The unexpected career. [Google Scholar]
- 12.Gaugler J.E., Kane R.L., Kane R.A., Newcomer R. The longitudinal effects of early behavior problems in the dementia caregiving career. Psychol Aging. 2005;20:100–116. doi: 10.1037/0882-7974.20.1.100. [DOI] [PubMed] [Google Scholar]