Highlights
-
•
An epidemiological model of causal pathways in the syndemic of diabetes and depression is presented.
-
•
Depression and diabetes are clustering in the adult Brazilian population partly due to shared social and behavioural causes.
-
•
There is an interaction between depression and diabetes in their association with disability.
-
•
There is a differential susceptibility to the effect of obesity on diabetes across levels of education and depression.
The comorbidity of depression and diabetes
The first studies observing a higher prevalence of depression among diabetes patients compared to the healthy population i.e., clustering of the two disorders, were published more than 30 years ago (Anderson, Freedland, Clouse, & Lustman, 2001). Most studies are from high income countries but reviews indicate that the same clustering exist in LMIC (Leone et al., 2012, Lloyd et al., 2012, Mendenhall et al., 2014). Depression is however found to be clustering with many other age-related chronic disorders (Huang, Dong, Lu, Yue, & Liu, 2010). The observed comorbidity between depression and diabetes has, independently of whatever causal mechanisms are involved, implications for clinical practice and health care delivery (Petrak, Baumesiter, Skinner, Brown, & Holt, 2015).
There are three causal potential mechanisms that all might contribute to the observed clustering: Depression and diabetes may share common causes, diabetes may increase the risk of depression, and the reverse causation may also exist. The first mechanism is well supported by existing evidence: age, short education, long term stress, physical inactivity and obesity are all factors that increase the risk of both depression and type-2 diabetes (Tabak, Akbaraly, Batty, & Kivimäki, 2014). Many cross-sectional studies have in search for a causal relationship between the disorders adjusted for these potential confounders and have still found higher prevalence of depression among diabetics, while the association between depression and pre-diabetes is found to be weaker after adjustment (Kan et al., 2013). Many studies have indicated that dysregulation of the HPA-axis and innate immunity and inflammation is involved in the aetiology of both type 2 diabetes and depression (Joseph and Golden, 2017, Moulton et al., 2015) and mediate the effect on both conditions of adverse social conditions and behaviours. Some studies have with a longitudinal design looked at the timing of incident cases and the results have indicated that diagnosed type 2 diabetes might increase risk of diabetes and vice versa (Eaton, 2002, Oladeji and Gureje, 2013). It is however unclear to what extent this is due to residual confounding of the shared causes, different induction time of the shared causes, or due to some of the biological mechanisms mentioned above (Tabak et al. 2014). It is however clear that the experience of a chronic disorder like diabetes might increase the risk of depression, and depression has a negative influence on self-care and treatment adherence among diabetics (Ciechanowski et al., 2000, Petrak et al., 2015, Pirraglia and Gupta, 2007). That means implicitly that depression and diabetes might interact in their effects on disease course and consequences (Petrak, Röhrig, & Ismail, 2018). A few studies have made a more formal interaction analysis on the effect on mortality (Black et al., 2003, Naicker et al., 2017) and disability (Egede, 2004).
Syndemic theory
The concept of “syndemics” (i.e., synergistic epidemics) was introduced by medical anthropologist Merrill Singer in the 1990s as a way to bring new perspectives and insights for public health and clinical practice by focusing explicitly on the interaction between co-existing disorders in specific communities and with biological, behavioural and social factors that influence the occurrence and consequences of the diseases (Singer, 1996). “A syndemic is a set of intertwined and mutually enhancing epidemics involving disease interactions at the biological level that develop and are sustained in a community/population because of harmful social conditions and injurious social connections.” (Singer & Clair, 2003).
The original definitions of syndemics was not very specific in terms of the quantitative empirical criteria. Recent reviews (Tsai and Burns, 2015, Tsai and Venkataramani, 2016, Tsai et al., 2017) has pointed out that many studies aiming to demonstrate interactions between diseases and conditions have applied a “sum-score” approach that might illustrate that effects are adding up, but fail to analyse whether they interact in the sense that the effect of one condition is influenced by the existence of another (Tsai, 2018).
We have interpreted the syndemic theory as a theory about how clustering and interaction between two or more diseases has both social causes and consequences. The interaction between diseases means that one disease influences the course and consequences of another disease. Clustering of disease will often be caused by clustering of specific causes. That clustering might be generated by shared more upstream fundamental individual or contextual causes that generate a differential exposure to the specific causes. The specific causes might then also interact with each other generating a differential susceptibility across levels of the fundamental cause.
In the case of a diabetes/depression syndemic previous studies have, as mentioned above, indicated that depression might influence both the occurrence and the consequences of diabetes and might also modify the effect of obesity on diabetes (Tsenkova & Karlamangla, 2016). The effect of social conditions might be mediated through specific causes such as obesity and the effect of obesity might be modified by social conditions. That combination of differential exposure (mediation) and differential susceptibility (interaction) has been raised as a more general and policy relevant mechanism in the pathways generating social disparities in health (Diderichsen, Hallqvist, & Whitehead, 2018).
Most of the empirical studies applying the concept of syndemics have dealt with communicable comorbidities where biological interaction is more obvious (Singer, Bulled, Ostrach, & Mendenhall, 2017). Some pathogens like HIV disrupt the function of the immune system in ways that increases the susceptibility for the infection with other pathogens such as tuberculosis. Other examples are the potential syndemics of Arbovirus infections in Latin America (Singer, 2016) and the interaction where influenza virus makes the lungs more susceptible to pneumococcus infection (McCullers, 2006). For most non-communicable diseases, the biological interactions may be less clear as mentioned above, but the diabetes/depression comorbidity has recently been studied as a case of non-communicable syndemics of growing relevance in many both high- and low-income populations. Mendenhall has with ethnographic methodology analysed the complex dynamics of violence, immigration, depression, diabetes, and abuse (VIDDA) among first- and second-generation Mexican immigrant women in Chicago (Mendenhall, 2012, Mendenhall, 2016, Mendenhall et al., 2017, Weaver and Mendenhall, 2014). She describes vividly how the social stress of poverty drives violence and obesity and how depression and diabetes in synergy frames the daily burden of illness.
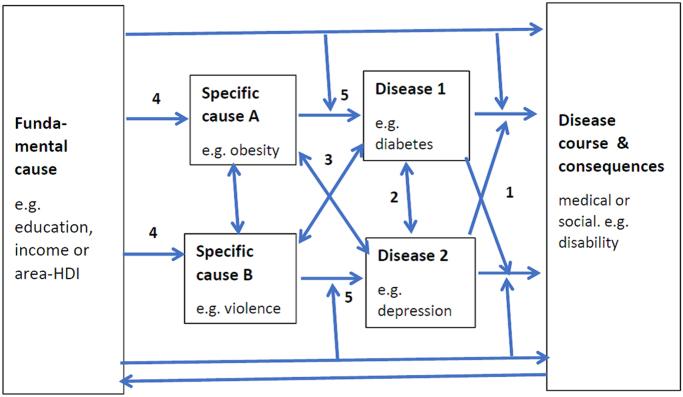
Fig. 1 presents a model that outlines five major mechanisms driving the syndemics, who can be analysed with epidemiological methods.
Fig. 1.
A model of the main causal relationships of syndemics.
The model has five elements [1–5] referring to numbers in Fig. 1: A basic element of syndemics is the interaction between diseases i.e., that one disease modifies the course as well as the medical and social consequences of the other (see [1] in Fig. 1). The health impact on a specific population of this interaction depends on how frequent the co-existence of the two diseases is – with no co-occurrence there will be no interaction. Clustering of two disorders can in principle be generated by four different mechanisms [2–5]: One disease may influence the occurrence of the other disease – bi-directional causality [2] – e.g. diabetes may raise the risk of depression and vice versa. The two diseases may also share a specific cause [3] e.g., stress, or share an individual or contextual fundamental cause (Link & Phelan, 1995) such as socioeconomic position or community resources, whose effect is mediated through specific cause(s) [4]. Since specific causes may interact with other causes associated with the fundamental cause there might be a differential susceptibility across levels of the fundamental cause to the effect of the mediating cause(s) [5]. The effect of obesity on diabetes might for example be stronger among people living under the economic stress of poverty. There might finally be a feed-back where disease consequences have socioeconomic implications.
In this paper we make an epidemiological analysis on a large sample of the Brazilian population of the five main mechanistic elements outlined above. It is interesting to study this syndemic in a Brazilian context where large social inequalities and high poverty rates are driving both violence, obesity, depression and diabetes. Epidemiological studies of large heterogenous populations might “dilute” some of the intensity found in the anthropological studies on selected communities mentioned above, but if the syndemic processes are found even in large heterogenous populations it will emphasize their public health relevance. We shall therefore in this paper examine the five key mechanisms of syndemics illustrated in Fig. 1:
-
•
The interaction between the two disorders in their association with disability and to what extent the consequences of diseases are modified by the fundamental causes [1].
-
•
The clustering of prevalent diabetes and depression [2 in Fig. 1], and to what extent it is generated by specific causes such as obesity and violence [3], or more fundamental causes here exemplified by individual education, income or state level social development [4].
-
•
The differential susceptibility across levels of education, income and state-level development to obesity and violence in their relation with diabetes and depression [5].
The Brazilian context
Brazil is a very heterogenous country with large inequalities. Economic inequalities and poverty rates have been reduced remarkably during the period 1995–2015, but are now increasing again from a level already among the 10 most unequal countries in the world. Brazil has a relatively young population, but the growing burden of diabetes (in terms of Disability Adjusted Life Years – DALY per 100,000) is 24% higher than in the EU and 23% lower than in the US (Global Burden of Disease GBD, 2018). The epidemiology of depression is more uncertain but the GBD estimates indicate the same level as in Europe. Brazil is suffering from a triple health burden with a burden from communicable diseases still approximately 3 times higher than in US and EU and from violence that is 20 (twenty) times higher than EU and four times higher than US. The burden from non-communicable disease is 20% lower than Europe and US, but adjusted for the younger age structure of the Brazilian population the burden is actually higher. The prevalence of both diabetes and depression show steep social gradients in Brazil as elsewhere (Iser et al., 2015, Malta et al., 2016), and it is in Brazil, like other middle-income countries particularly pronounced among women (Wang, Stronks, & Arah, 2014). These conditions are driving a social determination of syndemics both among communicable and non-communicable diseases, and a study of syndemics where comorbidity is analysed in a social context might provide insights of high relevance for Brazilian public health policies.
Material and method
The analysis is based on the latest Brazilian National Health Survey PNS 2013 (Szwarcwald, Malta, Pereira, Vieira, & Conde, 2014), which has already been used in studies of the prevalence of diabetes, depression and multimorbidity (Barros et al., 2017, Malta et al., 2016, Rzewuska et al., 2017). It is a cross-sectional household survey designed with a three-stage random sampling procedure. The census tracts are the primary units, the households are the second-stage units, and one resident per household aged 18 years or older is the third-stage units. The sample includes 81,357 households. 8.1% did not want to participate or could not be contacted. Interviews on health issues were carried out with 60,202 individuals. The survey was approved by the Comissão Nacional de Ética em Pesquisa (CONEP – National Commission of Ethics in Research - no. 328,159). PNS 2013 is thus a survey with sufficient size for the often very power-demanding interaction analyses, but it is cross-sectional which limits any attempt to draw causal inferences.
The two disorders analyzed are prevalent cases of self-reported diabetes and depressive symptoms. The first is based on an affirmative answer to the question “Has a doctor ever told you that you have diabetes?” The second is based on the PHQ-9 scale with a sum-score ranging from 0 to 27. Having moderate or severe depressive symptoms (“Depression”) is defined as scoring 10 or higher (Kroenke, Spitzer, & Williams, 2001). The measure of disability is based on questions raised for each of 13 different chronic disorders: to what degree the disease or its complications limit daily activities including work. Those who answer “moderate, serious or very serious” to at least one of these questions are classified as having disability i.e. limiting activities due to illness. “Short education” is defined as those who have basic school or less. “Low income” is defined as a monthly income below BRL 800 (=USD 212 in 2013).
For a syndemics analysis it would be ideal to have contextual data on local community level, but that is not available in this dataset. As a contextual measure of socioeconomic development, we have used the Human Development Index (HDI) of the 27 Brazilian states. It is a composite index including measures of education, income and longevity. The HDI of Brazil has according to UNDP increased 24% since 1990, but there are still large inequalities between states. In 2010 HDI varied from 0.631 in Alagoas in the North East region - similar to Honduras, to 0.824 in the District Federal - similar to Argentina (Atlas Brazil, 2013). The median HDI in 2010 for the PNS population is 0.734, and “Low HDI” is here defined as those living in a state below that level.
Both depression and diabetes have complex causal networks with several interacting component causes. We have chosen two causes, highlighted in the ethnographic syndemic-research, with well documented effects on one or both disorders: obesity and violence. Height and weight is measured at the interview and obesity is defined as BMI ≥ 30. Exposure to violence is measured as the affirmative answer to whether the interviewee during the previous 12 months has been a victim to violence.
The outcomes analyzed in terms of prevalent disease or disability is binary. Logistic regression is then often used, but we have used Generalized Linear models with binomial distribution in IBM SPSS, v25 for regression analysis. Associations are thus measured in absolute terms as risk-difference (RD) in percentage units of prevalence. We have chosen this measure of associations since it is more policy relevant and adequate for estimating interaction. When interaction as here is understood as conditional causation in a sufficient-component causal framework the relevant empirical criteria is departure from additivity of effects (Rothman, Greenland, and Walker, 1980). The size of interactions between two exposures are estimated as the difference in disease prevalence between those exposed to both compared to those exposed to none, minus the sum of the effects of single exposures. Some confounders are included in the regression model as indicated under the tables, but several other potential confounders are not included since they are not collected in the survey. We have applied weights to adjust for sampling stratification and differential non-response in the survey (Szwarcwald et al., 2014).
Results
Prevalence rates for diseases and covariates as well as the absolute unweighted numbers of participants in the survey are shown in Table 1. In the sample 6.2% reported to be diagnosed with diabetes while 7.9% has moderate to severe depressive symptoms. 20.8% are obese and 5.4% have been exposed to violence the previous 12 months.
Table 1.
Study population: prevalence of outcomes and covariates. Proportions in % weighted, N’s unweighted. Brazil PNS 2013.
|
With diabetes |
With depression |
Total population |
||||
|---|---|---|---|---|---|---|
| % | N | % | N | % | N | |
| Women | 59.6 | 2355 | 71.8 | 3783 | 52.9 | 34,282 |
| Age 45+ | 86.6 | 3107 | 52.5 | 2380 | 43.3 | 25,639 |
| Low HDI | 45.1 | 2254 | 49.6 | 3328 | 50.5 | 40,328 |
| Short education | 69.3 | 2492 | 59.2 | 2775 | 47.9 | 29,003 |
| Low income | 52.5 | 1935 | 62.3 | 3093 | 49,6 | 30,499 |
| Obese | 37.1 | 1309 | 27.1 | 1322 | 20.8 | 12,363 |
| Violence | 3.6 | 177 | 13.3 | 751 | 5.4 | 3666 |
| Diabetes | – | – | 11.5 | 546 | 6.2 | 3636 |
| Depression | 14.5 | 546 | – | – | 7.9 | 5051 |
| Disability | 35.8 | 1280 | 48.2 | 2278 | 13.7 | 8174 |
| Total | 6,2 | 3636 | 7,9 | 5051 | 100.0 | 60,202 |
The first empirical question is to what extent prevalent diabetes and depressive symptoms cluster. A total of 546 persons (0.91%) reported both disorders which is 1.85 times higher than expected if the conditions were not clustering. Table 2 shows that both disorders particularly among women are related to short education and low income. Short educated women have for example a 3.3 (95% CI 2.7;3.9) percentage units higher prevalence of diabetes compared to diabetics with more than short education. and 4.7 (95% CI 3.5;5.9) higher for depression. Diabetes (and to some extent also depression) is unsurprisingly higher among the obese and depression is (strongly) associated with the experience of violence.
Table 2.
Clustering of diabetes and depression. Prevalence rate differences with 95% CI for diabetes and depressive symptoms across socio-economic conditions, risk factors and comorbidity. Brazil PNS 2013.
|
Diabetes |
Depression |
|||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| Low HDI-statea | -1.4 (-1.9;-0.8) | 0.1 (-0.5;0.6) | 0.5 (0.0;1.0) | -0.4 (-1.1;0.3) |
| Short educationb | -0.4 (-1.0;0.1) | 3.3 (2.7;3.9) | 1.9 (1.4;2.4) | 4.7 (4.0;5.5) |
| Low incomec | 0.7 (0.1;1.3) | 0.6 (0.0;1.3) | 2.6 (2.0;3.1) | 2.1 (1.3;2.8) |
| Obesityd | 4.9 (4.2;5.6) | 4.2 (3.5;4.9) | 1.9 (1.2;2.5) | 2.1 (1.3;3.0) |
| Violenced | -0.2 (-1.4;1.0) | 0.0 (-1.2;1.3) | 9.5 (8.4;10.7) | 16.4 (14.9;18.0) |
| Diabetese | – | – | 4.2 (3.0;5.3) | 5.4 (4.0;6.9) |
| Depressione | 4.5 (3.3;5.8) | 3.6 (2.6;4.5) | – | – |
| Diabetesa | – | – | 4.4 (3.2;5.4) | 6.2 (4.8;7.6) |
| Depressiona | 4.7 (3.5;5.9) | 4.0 (3.1;4.9) | – | – |
| Depression * low HDI-statea | -7.6 (-10.1;-5.2) | -1.6 (-3.5;0.2) | – | – |
| Depression * short educationb | -1.7 (-4.3;0.9) | 0.3 (-1.6;2.1) | – | – |
| Depression * low incomec | 2.3 (-0.2;4.5) | 0.0 (-2.0;2.0) | – | – |
| Diabetes * low HDI-statea | – | – | -4.8 (-7.0;-2.5) | -1.0 (-3.7;1.8) |
| Diabetes * short educationb | – | – | -0.0 (-2.3;2.2) | -4.0 (-7.1;-0.9) |
| Diabetes * low incomec | – | – | 6.9 (4.6;9.3) | 3.2 (0.4;6.1) |
| Prevalence % | 5.4 | 7.0 | 4.7 | 10.7 |
| N (weighted) | 1518 | 2236 | 1340 | 3414 |
Adjusted for age.
Adjusted for age + HDI.
Adjusted for age + HDI + education.
adjusted for age + HDI + education + income.
Adjusted for age + HDI + education + income + obesity + violence.
Shared causes (age, female sex, short education, obesity and violence) might generate clustering of the two disorders, but it can be seen in Table 2 that even when adjusted for these shared causes the prevalence of diabetes is for example 4.5 (95% CI: 3.3;5.8) percentage units higher among men with depression compared to those without. Without adjustment for the determinants it can, in the rows below, be seen that the clustering is only slightly more pronounced with a RD of 4.7 (95% CI 3.5;5.9) when only adjusted for age. This means that the other shared causes only play a limited role for the clustering. Table 2 further illustrates that the clustering of the two disorders (measured as the rate difference of diabetes among those with and without depression and vice versa,) among men is less pronounced in states with low HDI. The “effect” of depression on diabetes is thus -7.6 (95% CI -10.1;-5.2) percentage units lower among men in states with low HDI. The clustering seems also to be more pronounced among low income men and women.
As there is a clustering of the two disorders there are rich opportunities for interaction between them. A crucial criterion for whether a syndemic exist is whether diabetes interacts with depressive symptoms or vice versa in the association with disease consequences such as disability (activity limitation). In Table 3 we have spelled out the results of that analysis of interaction between the two disorders. Diabetes and in particular depressive symptoms are unsurprisingly linked to disability. For women the effect on disability of diabetes without depressive symptoms is 14.4 percentage units and for depressive symptoms without diabetes 33.1. The joint effect is 58.3 among those with both disorders which is (58.3-33.1-14.4) = 10.8 (95% CI 6.7;14.9) higher than the sum of the two single effects. For men the interaction effect is even stronger: 21.2 (95% CI 15.9;26.6).
Table 3.
Interaction between diabetes and depression in relation to disability (limited daily activities). Prevalence rate differences in percentage units with 95% CI. Adjusted for age. Brazil PNS 2013.
| Men | Women | |||
|---|---|---|---|---|
| 0 diabetes 0 depression | 0 (ref.) | 0 (ref.) | ||
| + diabetes 0 depression | 9.1 (7.4;10.8) | 14.4 (12.6;16.1) | ||
| 0 diabetes + depression | 34.3 (32.6;36.1) | 33.1 (31.8;34.5) | ||
| + diabetes + depression | 64.7 (59.9;69.4) | 58.3 (54.7;61.8) | ||
| Interaction: diabetes * depression | 21.2 (15.9;26.6) | 10.8 (6.7;14.9) | ||
| Diabetes * Short education | -2.8 (-6.1;0.6) | 7.6 (3.8;11.4) | ||
| Depression * Short education | 9.6 (6.0;13.3) | 14.7 (12.0;17.4) | ||
In Table 3 we have also shown that the association between diabetes and disability is stronger among women than among men. The interaction effect (measured as departure from additivity as explained above) between short education and diabetes is for women 7.6 percentage units (95% CI 3.8;11.4). For depression the interaction is much stronger for both men and women. Income is not included in the analysis since it may be an effect of disability.
It has earlier been shown with data from the PNS2013 that obesity is, particularly among women, strongly associated with short education (Barros et al., 2017), while exposure to violence is not (Mascarenhas, Sinimbu & Malta, 2017). In Table 4 interactions between the determinants are shown. It can be seen that the association between short education and diabetes is not only a result of differential exposure to obesity (as shown by Malta et al., 2016), but also to differential susceptibility. Obesity interacts synergistically with education. The interaction effect on diabetes is 5.1 (95% CI 3.7;6.5) for men and 3.1 (95% CI 1.8;4.4) for women. Obesity also interacts with depression among both men and women. Violence interacts among women with low income with an effect on 3.4 (95% CI 0.3;6.5), but otherwise we find no clear signs of differential susceptibility.
Table 4.
Differential susceptibility to obesity, violence and comorbidity. Adjusted for age, HDI, education and income. Prevalence rate differences in percentage units with 95% CI. Brazil PNS 2013.
| Men | Women | |
|---|---|---|
| Diabetes | ||
| Obesity * low HDI-statea | -3.0 (-4.4;-1.6) | -2.9 (-4.2;-1.5) |
| Obesity * short educationb | 5.1 (3.7;6.5) | 3.1 (1.8;4.4) |
| Obesity * low incomec | 2.0 (0.4;3.6) | -0.9 (-2.3;0.4) |
| Obesity * depressiond | 6.5 (3.5;9.5) | 3.5 (1.4;5.5) |
| Obesity * violenced | 2.2 (-5.4;1.1) | -1.8 (-4.8;1.1) |
| Depression | ||
| Violence * low HDI-statea | 2.3 (0.0;4.6) | -1.4 (-4.5;1.8) |
| Violence * short educationb | -1.5 (-3.8;0.8) | 1.9 (-1.3;5.1) |
| Violence * low incomec | 1.7 (-0.6;4.1) | 3.4 (0.3;6.5) |
| Violence * diabetesd | -4.0 (-10.3;2.3) | 2.6 (-4.5;9.7) |
| Violence * obesityd | -5.7 (-8.8;-2.6) | 3.7 (0.0;7.3) |
Adjusted for age.
Adjusted for age + HDI.
Adjusted for age + HDI + education.
Adjusted forage + HDI + education + income.
Discussion
If we go back to Fig. 1 and the five mechanisms outlined there we can conclude that there in the adult Brazilian population is an interaction between diabetes and depression in their effect on disability [1]. There is also a clustering of the two disorders. That can partly be due to a shared specific cause - obesity [3] – and shared more fundamental causes such as short education and low income [4]. After adjustment for these shared causes there is still a strong clustering – indicating that there might also be a bi-directional causal relationship [2]. There are finally interactions between education/income and obesity indicating a differential susceptibility [5].
The clustering and interaction between the two disorders have been found in a few studies from other parts of the world (Black et al., 2003, Leone et al., 2012, Scott et al., 2009). The clustering is modified by HDI level of states, which might illustrate that increased clustering of these two disorders is a pattern linked to advancing socio-economic development. But Brazilian states are large and very heterogenous societies which might erase many contextual effects. The stronger clustering in rich states could be due to better access to diagnostics in those states, but Table 1 show that the prevalence of each of the two conditions are not related to HDI. Both diabetes and depression is strongly associated with education and income, in particular among women, but the clustering is still quite strong after adjustment for education, obesity and violence. One Danish study has, in a very different context, found that clustering was more pronounced among those with low income (Cleal, Panton, Willaing, & Holt, 2017), and stronger disease clustering among low income people is also found here.
The interaction between diabetes and depression is analyzed for self-reported disability in relation to work and other daily activities. Disability is in itself an interaction between how the individual evaluates his/her health and the demands on him/her of work and other activities. Depressive mood influences not only the functional capacity but might also influence the perception and reporting of disability. The differential susceptibility to obesity has been observed in other studies but with very heterogenous results across genders and regions (Shang et al., 2013, Wang et al., 2014). The strong association between violence and depression, particularly among women, is well known from other studies (Watkins et al., 2014), and we find signs of differential susceptibility to violence for low-income women.
The study is cross-sectional which precludes any firm causal inference even if we are aware that concepts like interaction are suggesting otherwise. Reporting disability due to illness is more an effect than a case of illness, diabetes is more an effect than a cause of obesity and education, but depression might influence both obesity and self-reported violence. Some causes might through inverse causality be influenced by disease (obesity might for example be both an effect and cause of depressed mood) and controlling for obesity as a confounder might lead to an underestimation of the interaction between diseases. The study is an individual level study and is thus not meeting the call for more population level studies (Tsai et al., 2017). Most variables except obesity is self-reported which means that misclassification and underestimation of interactions is likely to occur (Lundberg, Hallqvist, & Diderichsen, 1999).
A central issue of the syndemics concept is the interaction between and comorbidities and between social conditions and diseases. We have in this study applied a formal interaction analysis that illustrates how the social context modifies the clustering and interactions involved. The causal framework illustrated in Fig. 1 might look complicated but is still a crude simplification of reality. While lacking the depth of the anthropological studies with the understanding generated by reference to a local context, we find clear empirical evidence of many of the criteria for a diabetes/depression syndemic in this large heterogenous population, showing the public health relevance of the concept.
Public health policy implications
The socio-economic inequalities in Brazil creates high average exposure levels for some health determinants like violence and large social differences in exposure to others like female obesity. The syndemics framework and the interaction analyses shown on this paper illustrates that large social inequalities in the burden of diabetes and depression is not only generated by these exposure levels but also by a differential vulnerability to the effects of these determinants and to the differential consequences of the diseases. The fact that these patterns of clustering and interaction are more pronounced in more developed states illustrates that health policy in Brazil should focus on reducing health inequalities as they might grow with a growing economy.
In the syndemics literature it has often been concluded that when multiple conditions interact the policy implication is that interventions should be multicomponent addressing all interacting conditions (Tsai et al., 2017, Tsai, 2018). When interaction means conditional causation, the conclusion is rather the opposite: that by tackling one condition, some of the effect of the other condition - that due to the interaction is dependent on the first – will also be eliminated. In this case the results mean that tackling depression will remove a part of the disabling effect of diabetes. Many clinical guidelines recommend a coordinated treatment of both disorders, but there is no evidence from efficacy trials that shows that treatment of one disorder will influence the outcome of the other (Tabak et al., 2014). The Brazilian reality is however not even close to full coverage of needs generated by this syndemic. Of those suffering from both disorders only 22.5% report in this survey that they have regular contact with health professionals for depression and 17.6% that they get care for both disorders. The differential susceptibility to the effects of obesity on diabetes show not only the importance of targeting susceptible groups with short education and low income with preventive efforts, but also that a general reduction of obesity across social groups will reduce the inequality in diabetes due to the higher effect among the more susceptible who are also the more deprived groups (Diderichsen et al., 2018).
Conflict of interest
No conflict of interest declared.
Funding
No Funding used.
Ethics approval
The National Health Survey of Brazil was approved by the Comissão Nacional de Ética em Pesquisa (CONEP – National Commission of Ethics in Research) in June 2013 (no. 328,159).
References
- Anderson R.J., Freedland K.E., Clouse R.E., Lustman P.J. The prevalence of comorbid depression in adults with diabetes. A meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- Atlas Brazil (2013). 〈http://www.atlasbrasil.org.br/2013/en/home/〉. (Accessed 20 July 2018).
- Barros M.B.A., Lima M.G., Azevedo R.C.S., Medina L.B.P., Lopes C.S., Menezes P.R., Malta D.C. Depression and health behaviors in Brazilian adults – PNS 2013. Rev Saude Publica. 2017;51(Suppl.1):8s. doi: 10.1590/S1518-8787.2017051000084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black S.A., Markides K.S., Ray L.A. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care. 2003;26(10):2822–2828. doi: 10.2337/diacare.26.10.2822. [DOI] [PubMed] [Google Scholar]
- Ciechanowski P.S., Katon W.J., Russo J.E. Depression and diabetes. Impact of depressive symptoms on adherence, function and costs. Archives of Internal Medicine. 2000;160:3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- Cleal B., Panton U.H., Willaing I., Holt R.I.G. Diabetes and depression in Denmark 1996–2010: National data stratified by occupational status and annual income. Diabetic Medicine. 2017;34:108–114. doi: 10.1111/dme.13187. [DOI] [PubMed] [Google Scholar]
- Diderichsen F., Hallqvist J., Whitehead M. Differential vulnerability and susceptibility: How to make use of recent development in our understanding of mediation and interaction to tackle health inequalities. International Journal of Epidemiology. 2018 doi: 10.1093/ije/dyy167. [DOI] [PubMed] [Google Scholar]
- Eaton W.W. Epidemiologic evidence on the comorbidity of depression and diabetes. Journal of Psychosomatic Research. 2002;53:903–906. doi: 10.1016/s0022-3999(02)00302-1. [DOI] [PubMed] [Google Scholar]
- Egede L.E. Diabetes, major depression, and functional disability among U.S. adults. Diabetes Care. 2004;27(2):421–428. doi: 10.2337/diacare.27.2.421. [DOI] [PubMed] [Google Scholar]
- GBD 2016 Brazil Collaborators Burden of disease in Brazil, 1990–2016: A systematic sub national analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392:760–775. doi: 10.1016/S0140-6736(18)31221-2. (doi: 0.1016/S0140-6736(18)(31221-2) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C.Q., Dong B.R., Lu Z.C., Yue J.R., Liu Q.X. Chronic diseases and risk for depression in old age: A meta-analysis of published literature. Ageing Research Reviews. 2010;9:131–141. doi: 10.1016/j.arr.2009.05.005. [DOI] [PubMed] [Google Scholar]
- Iser B.P.M., Stopa S.R., Chueiri P.S., Szwarcwald C.L., Malta D.C., da Cruz Monteiro H.O.…Schmidt M.I. Prevalência de diabetes autorreferido no Brasil: Resultados da Pesquisa Nacional de Saúde 2013. Epidemiologia e Serviços de Saúde. 2015;24(2):305–314. [Google Scholar]
- Joseph J.J., Golden S.H. Cortisol dysregulation: The bidirectional link between stress, depression, and type 2 diabetes mellitus. Annals of the New York Academy of Sciences. 2017;1391:20–34. doi: 10.1111/nyas.13217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan C., Silva N., Golden S.H., Rajala U., Timonen M., Stahl D., Ismail K. A systematic review and meta-analysis of the association between depression and insulin resistance. Diabetes Care. 2013;36:480–489. doi: 10.2337/dc12-1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9. Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leone T., Coast E., Narayanan S., Aikins A.G. Diabetes and depression comorbidity and socioeconomic status in low and middle-income countries (LMICs): A mapping of the evidence. Globalization and Health. 2012;8:39. doi: 10.1186/1744-8603-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;(Spec No):80–94. [PubMed] [Google Scholar]
- Lloyd C.E., Roy T., Nouwen A., Chauhan A.M. Epidemiology of depression in diabetes: International and cross-cultural issues. Journal of Affective Disorders. 2012;142(Suppl):S22–S29. doi: 10.1016/S0165-0327(12)70005-8. [DOI] [PubMed] [Google Scholar]
- Lundberg M., Hallqvist J., Diderichsen F. Exposure-dependent misclassification of exposure in interaction analyses. Epidemiology. 1999;10(5):545–549. [PubMed] [Google Scholar]
- Malta D.C., Bernal R.T.I., Souza M.F.M., Szarcwald C.L., Lima M.H., Barros M.B. Social inequalities in the prevalence of self-reported chronic non-communicable diseases in Brazil: National health survey 2013. IInternational Journal for Equity in Health. 2016;15(1):153. doi: 10.1186/s12939-016-0427-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mascarenhas M.D.M., Sinimbu R.B., Malta D.C. Violência cometida por pessoa conhecida – Brasil, 2013. Ciência & Saúde Coletiva. 2017;22(11):3763–3771. doi: 10.1590/1413-812320172211.08672016. [DOI] [PubMed] [Google Scholar]
- McCullers J.A. Insights into the interaction between influenza virus and pneumococcus. Clinical Microbiology Reviews. 2006;19(3):571–582. doi: 10.1128/CMR.00058-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendenhall E. Left Coast Press; San Francisco: 2012. Syndemic suffering: Social distress, depression and diabetes among mexican immigrant women. [Google Scholar]
- Mendenhall E. Beyond comorbidity: A critical perspective of syndemic depression and diabetes in cross-cultural contexts. Medical Anthropology Quarterly. 2016;30(4):462–478. doi: 10.1111/maq.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendenhall E., Kohrt B.A., Norris S.A., Ndetei D., Prabhakaran D. Non-communicable disease syndemics: Poverty, depression, and diabetes among low-income populations. Lancet. 2017;389:953–963. doi: 10.1016/S0140-6736(17)30402-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendenhall E., Norris S.A., Shidhaye R., Prabhakaran D. Depression and type 2 diabetes in low and middle income countries: A systematic review. Diabetes Research and Clinical Practice. 2014;103(2):276–285. doi: 10.1016/j.diabres.2014.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moulton C.D., Pickup J.C., Ismail K. The link between depression and diabetes: The search for shared mechanisms. The Lancet Diabetes & Endocrinology. 2015;3:461–471. doi: 10.1016/S2213-8587(15)00134-5. [DOI] [PubMed] [Google Scholar]
- Naicker K., Johnson J.A., Skogen J.C., Manuel D., Øverland S., Sivertsen B., Colman I. Type 2 diabetes and comorbid symptoms of depression and anxiety: Longitudinal associations with mortality risk. Diabetes Care. 2017;40:352–358. doi: 10.2337/dc16-2018. [DOI] [PubMed] [Google Scholar]
- Oladeji B.D., Gureje O. The comorbidity between depression and diabetes. Current Psychiatry Reports. 2013;15(9):390. doi: 10.1007/s11920-013-0390-3. [DOI] [PubMed] [Google Scholar]
- Petrak F., Baumesiter H., Skinner T.C., Brown A., Holt R.I.G. Depression and diabetes: Treatment and health-care delivery. The Lancet Diabetes & Endocrinology. 2015;3:472–485. doi: 10.1016/S2213-8587(15)00045-5. [DOI] [PubMed] [Google Scholar]
- Petrak, F., Röhrig, B., Ismail, K. (2018). Depression and diabetes. In L. J. De Groot, G. Chrousos, K. Dungan, et al., (Eds.) Endotext [Internet]. Available from: 〈https://www.ncbi.nlm.nih.gov/books/NBK498652/〉.
- Pirraglia P.A., Gupta S. The interaction of depression and diabetes: A review. Current Diabetes Reviews. 2007;3(4):249–251. doi: 10.2174/1573399810703040249. [DOI] [PubMed] [Google Scholar]
- Rothman K., Greenland S., Walker A.M. Concepts of interaction. American Journal of Epidemiology. 1980;112(4):467–470. doi: 10.1093/oxfordjournals.aje.a113015. [DOI] [PubMed] [Google Scholar]
- Rzewuska M., de Azevedo-Marques J.M., Coxon D., Zanetti M.L., Zanetti A.C., Franco L.J., Santos J.L. Epidemiology of multimorbidity within the Brazilian adult general population: Evidence from the 2013 National Health Survey (PNS 2013) PLOS One. 2017;12(2):e0171813. doi: 10.1371/journal.pone.0171813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott K.M., Von Koff M., Alonso J., Angermeyer M.C. Mental–physical co-morbidity and its relationship with disability: Results from the World Mental Health Surveys. Psychological Medicine. 2009;39(1):33–43. doi: 10.1017/S0033291708003188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shang X., Li J., Tao Q., Li J., Li X., Zhang L.…Yang Y. Educational level, obesity and incidence of diabetes among Chinese adult men and women aged 18–59 years old: An 11-year follow-up study. PLOS One. 2013;8(6):e66479. doi: 10.1371/journal.pone.0066479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer M. The spread of Zika and the potential for global arbovirus syndemics. Global Public Health. 2016;12(1):1–18. doi: 10.1080/17441692.2016.1225112. [DOI] [PubMed] [Google Scholar]
- Singer M., Bulled N., Ostrach B., Mendenhall E. Syndemics and the biosocial conception of health. The Lancet. 2017;389:941–950. doi: 10.1016/S0140-6736(17)30003-X. [DOI] [PubMed] [Google Scholar]
- Singer M., Clair S. Syndemics and public health: Reconceptualizing disease in bio-social context. Medical Anthropology Quarterly. 2003;17(4):423–444. doi: 10.1525/maq.2003.17.4.423. [DOI] [PubMed] [Google Scholar]
- Singer M. A dose of drugs, a touch of violence, a case of AIDS. Conceptualizing the SAVA syndemic. Free Inquiry in Creative Sociology. 1996;24(2) (499-110) [Google Scholar]
- Szwarcwald C.L., Malta D.C., Pereira C.A., Vieira M.L.F.P., Conde W.L., Souza P.R.B.…Monteiro C.A. Pesquisa Nacional de Saúde no Brasil: Concepção e metodologia de aplicação. Ciência & Saúde Coletiva. 2014;19(2):333–342. doi: 10.1590/1413-81232014192.14072012. [DOI] [PubMed] [Google Scholar]
- Tabak A.G.T., Akbaraly T.N., Batty D., Kivimäki M. Depression and type 2 diabetes: A causal association? The Lancet Diabetes Endocrinology. 2014;2(3):236–245. doi: 10.1016/S2213-8587(13)70139-6. [DOI] [PubMed] [Google Scholar]
- Tsai A.C. Syndemics: A theory in search of data or data in search of a theory? Social Science & Medicine. 2018;206:117–122. doi: 10.1016/j.socscimed.2018.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Burns B.F.O. Syndemics of psychosocial problems and HIV risk: A systematic review of empirical tests of the disease interaction concept. Social Science & Medicine. 2015;139:26–35. doi: 10.1016/j.socscimed.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Mendenhall E., Trostle J.A., Kawachi I. Co-occurring epidemics, syndemics, and population health. The Lancet. 2017;389:978–982. doi: 10.1016/S0140-6736(17)30403-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C., Venkataramani A.S. Syndemics and health disparities: A methodological note. AIDS and Behavior. 2016;20(2):423–430. doi: 10.1007/s10461-015-1260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsenkova V.K., Karlamangla A. Depression amplifies the influence of central obesity on 10-year incidence of diabetes: Findings from MIDUS. PLOS One. 2016;11(10):e0164802. doi: 10.1371/journal.pone.0164802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang A., Stronks K., Arah O.A. Global educational disparities in the associations between body mass index and diabetes mellitus in 49 low-income and middle-income countries. Journal of Community Health. 2014;68(8):705–711. doi: 10.1136/jech-2013-203200. [DOI] [PubMed] [Google Scholar]
- Watkins L.E., Jaffe A.E., Hoffman L., Gratz K.L., Messman-Moore T.L., DiLillo D. The longitudinal impact of intimate partner aggression and relationship status on women’s physical health and depression symptoms. Journal of Family Psychology. 2014;28(5):655–665. doi: 10.1037/fam0000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver L.J., Mendenhall E. Applying syndemics and chronicity: Interpretations from studies of poverty, depression, and diabetes. Medical Anthropology. 2014;33:92–108. doi: 10.1080/01459740.2013.808637. [DOI] [PubMed] [Google Scholar]