Abstract
Sleep deprivation among adolescents has received much attention from health researchers and policymakers. Recent research indicates that variation in sleep duration from night to night is associated with multiple health outcomes. While there is evidence that sleep deprivation is socially patterned, we know little about how social contexts are associated with nightly sleep variation during adolescence (a life course stage when nightly sleep variation is particularly high). Given the importance of family environments for influencing adolescents’ sleep patterns, we hypothesized that disadvantaged family contexts would be associated with higher intra-individual variation (IIV) in nightly sleep duration, in addition to lower average nightly sleep duration. We tested these hypotheses in a diverse, population-based sample of 11–17 year-olds (N = 1095) from the Adolescent Health and Development in Context Study. Using survey and ecological momentary assessment data and a novel form of multi-level regression modeling (location-scale mixed modeling), we found that adolescents living in unmarried-parent, low SES, economically insecure, and high caregiver stress families had higher IIV in sleep than adolescents in families with more resources and less caregiver stress. There were fewer family effects on average sleep duration. This suggests family social and economic contexts are associated with an under-researched aspect of adolescent sleep, nightly variation, and may contribute to adolescent sleep problems with implications for their health and health disparities.
Highlights
-
•
Consistency in nightly sleep duration is important for adolescent health.
-
•
SES and family stress associated with variability in sleep duration in adolescents.
-
•
Caregiver distress also associated with lower mean sleep duration among adolescents.
1. Introduction
National trends in sleep indicate a growing percentage of U.S. children are getting less than adequate sleep, particularly during adolescence (Hawkins & Takeuchi, 2016). Most are sleeping less than the recommended 9 h per night (Hirshkowitz et al., 2015), with almost 70% of U.S. adolescents categorized as sleep deprived (Healthy People, 2020). Recent research also highlights the high level of variability in nightly sleep duration during adolescence (Cysarz et al., 2018, Urbanek et al., 2018). Nightly sleep variability is associated with multiple health risks in adolescents; including, increased risk of obesity and poor diet (He et al., 2015; Malone et al., 2016), chronic inflammation (Park et al., 2016), substance use (Haynie et al., 2017, Nguyen-Louie et al., 2018), behavioral disorders (Zhang et al. 2017), and mental health problems/negative mood (Bei et al., 2017, Fuligni and Hardway, 2006, Zhang et al., 2017). Thus, in addition to the health risks posed by insufficient mean hours of sleep (Wahlstrom, Berger, & Widome, 2017), variability in sleep may produce health disadvantages among adolescents who are unable to establish regular sleep schedules.
Importantly, sleep disadvantages are not equally distributed across all adolescents, suggesting that social factors are important in ensuring healthy sleep patterns (Guglielmo et al., 2018, Malone et al., 2016). In fact, social conditions may be more important than biological changes in shaping adolescents’ sleep and sleep disparities (Maume, 2013). However, little research has identified how social contexts influence adolescent sleep; with a particular dearth in research on family contexts and on intra-individual variation (IIV) in adolescents’ sleep (Becker, Sidol, Van Dyk, Epstein, & Beebe, 2017). Families, as the most proximate social contexts within which sleep occurs, are likely critical for the establishment of healthy sleep patterns during this important developmental stage. Further, given the changes in family structure and increasing economic inequalities among U.S. families in the past several decades (McLanahan, 2004), family contexts may contribute to increasing sleep disparities among U.S. adolescents.
Sociological and developmental research indicates that disadvantaged family social structures, such as unmarried parent families and low family SES, limit economic resources, reduce parental time, and add stress to families (Conger et al., 1994, McLanahan, 2004), with implications for poor health and behavioral outcomes among adolescents (Adkins et al., 2009, Cavanagh, 2008, Crosnoe and Cavanagh, 2010, Doom et al., 2017). Related to sleep, in particular, fewer economic resources and less parental time may result in less supervision and enforcement of healthy sleep habits among adolescents, and more stressful socio-emotional environments may heighten vigilance and reduce adolescents’ ability to fall asleep and establish regularity in sleep duration (Dahl & Lewin, 2002). Thus, we hypothesize that adolescents living in unmarried and low SES families will have higher variability in nightly sleep duration than those living in married parent and higher SES families. Further, we hypothesize that family conditions such as economic hardship, caregiver distress and low family cohesion may be additionally important family stress measures associated with IIV in sleep. Although we focus on IIV in sleep, we simultaneously estimate the associations with mean sleep duration and expect lower mean sleep duration among youth in more disadvantaged families for the same reasons identified above.
To test our hypotheses, we utilize survey and ecological momentary assessment (EMA) data from the Adolescent Health and Development in Context Study (AHDC), a population-based sample of adolescents ages 11–17 years (N = 1405) living in and around Columbus, OH in the U.S. We use a novel form of multi-level modeling to assess how family conditions (unmarried parent families, low SES, and high family stress) are associated with IIV in sleep, net of individuals’ mean sleep time. The results inform research on adolescent sleep, with a particular focus on how family contexts are associated with variation in nightly sleep duration at this critical developmental stage.
1.1. Prior studies
Empirical studies assessing family context effects on adolescent sleep are limited, and tend to focus on mean rather than variability in nightly sleep duration. With regard to mean sleep duration, a nationally-representative time diary study of adolescents (ages 12–19, n = 1187), found no association between head of household marital status with weekend or weekday sleep duration (Adam, Snell, & Pendry, 2007). The same study found that higher family income was marginally associated with more sleep during the weekend (but not on weekdays), but parental education was not associated with either outcome (Adam et al., 2007). The study included variables related to family functioning and activities that could have been mediating the role of family structure and SES on adolescents’ sleep patterns. Parental rules were associated with more hours slept for 12–19 year olds (Adam et al., 2007), indicating some evidence for family process effects. A major limitation of the study was that the time-diary data, while nationally-representative, only included reports for one weekday and one weekend day per adolescent. Thus, the models, which were run separately for weekday and weekend outcomes, assessed family context effect on sleep diary reports from one day per adolescent. Further, 43% of the diaries were completed by the caregiver rather than the child/adolescent themselves (Adam et al., 2007).
A more recent study using actigraphy (an electronic device worn on the wrist that detects sleep-related activity) found that adolescents (ages 14–19 years) living in single-parent households had significantly shorter sleep duration on weekends and lower 7-day sleep efficiency (percent of time in bed spent sleeping) than similar adolescents in two-parent families (Troxel, Lee, Hall, & Matthews, 2014). Several other actigraphy studies have found that adolescents in lower SES families had lower mean sleep duration than those in higher SES families (Bagley et al., 2015, Marco et al., 2012, Moore et al., 2011). Finally, a recent review article showed evidence of reduced sleep duration among low-SES adolescents across settings (Felden, Leite, Rebelatto, Andrade, & Beltrame, 2015).
Research on family contexts and sleep hour variability is more limited and less consistent in terms of measuring sleep variability. One study of 155 7th graders, using standard deviations in sleep duration measured by actigraphy over a week, found higher standard deviations in sleep time among lower SES adolescents (based on a composite SES score of family income, education and percent of single-homes in the neighborhood) (Marco et al., 2012). Another actigraphy study of 257 youth (mean age 14 years) examined the coefficient of variance in sleep duration (measured as the standard deviation divided by the mean) and found higher parent income and education associated with reduced variance in adolescents’ sleep duration. However, these effects became insignificant in multivariate models (Moore et al., 2011). Finally, a study of 271 adolescents (mean age 11 years) from a semi-rural public school found no association between family income-to-needs ratio and mean-composited variability in sleep duration (Bagley et al., 2015). A limitation of these studies is that their outcomes do not separate mean from IIV aspects of nightly sleep.
1.2. Study contribution
We contribute to research on families and adolescent well-being with this study of family contexts and sleep in adolescents in several ways. First, we focus on the outcome of intra-individual variation (IIV) in sleep duration over a week, while accounting for the mean sleep duration of the adolescents. As previously noted, this is a potentially important, and under-studied, aspect of adolescents’ sleep. Second, we assess multiple aspects of family contexts and their associations with adolescent sleep patterns. In doing so, we hypothesize that unmarried parent and low SES environments will reflect broad family resource constraints that could reduce regularity in adolescents’ sleep duration; and, we consider multiple measures of family stress (economic hardship, caregiver distress and low family cohesion) as potentially important family process and experience measures for adolescents’ sleep.
Third, we make a methodological contribution by using mixed effects location-scale modeling, an extension of multilevel modeling. Unlike standard multilevel models, this approach allows differences in sleep variance across individuals to be a function of both fixed covariates and random variation, ensuring accurate standard error estimates and hypothesis testing of family effects on IIV in sleep (Hedeker & Nordgren, 2013). To our knowledge, this is the first population-based study to apply this method to analyzing nightly sleep duration.
Finally, we test our study hypotheses in a relatively large, population-based sample of youth (N = 1095). Most prior studies using actigraphy – a more objective measure of sleep that does not rely on self-report data – are limited in terms of the size and representativeness of their samples. Although our data are similar to time diary studies of sleep, one advantage of EMA sleep data is that sleep duration had to be reported during the following day when the EMA prompts were available. This encourages reporting on sleep duration each day rather than after a longer time period has elapsed. Our data also include daily reports of multiple nights of sleep (as reported by the adolescent) across a week-long period. This provides a more reliable assessment of mean sleep duration than studies using one or two nights of sleep diary data (Adam et al., 2007), surveys that ask broadly about how much adolescents sleep per night (He et al., 2015), or data reported by caregivers (Hawkins & Takeuchi, 2016). Our data allow for capturing changes in sleep duration across the week, which would not be evident in general survey or single-day measures, and as reported by the adolescents themselves within an established timeframe.
2. Methods
2.1. Data
Our data come from the 2014–16 Adolescent Health and Development in Context (AHDC) study. The AHDC emphasizes the interplay of social, psychological, and biological processes in shaping youth developmental outcomes such as health risk and pro-social behavior, mental and physical health, and educational outcomes. Using a prospective cohort design, the study collected data on multiple contexts of youth development from a representative sample of households with adolescents ages 11–17 residing in an urbanized area of Franklin County, OH (containing a majority of the city of Columbus and several suburban municipalities). Informed consent was obtained from all individual participants included in the study. The data were collected over a week, beginning with entrance surveys with the focal youth and his/her caregiver, followed by a 7-day period when smartphones (provided to youth during the initial visit) were used to obtain ecological momentary assessment (EMA) data (3–4 min surveys administered over the phone). The EMA was administered five times a day – once in the morning (before school) and randomly within 1–2-h time blocks starting after school ended (and all day on weekends). A final end-of-day EMA occurred at around 9 p.m. The data collection was concluded with an end of the week in-home exit survey, which included a review of nightly sleep duration with the adolescents to fill in where EMA data were missing.
2.2. Sample
We limited our sample to adolescents with at least 3 nights of sleep data (N = 1291) given our interest in IIV estimates in addition to mean sleep duration. Importantly, the statistical method we use places more weight on the estimates of adolescents with more sleep nights reported, conditional on covariates included in the model (Hedeker, Mermelstein, & Demirtas, 2008). As a sensitivity analysis we tested models including only adolescents with 5 or more nights of sleep data with comparable results.
Our sample of adolescents with 3 or more reported sleep nights did not differ significantly from those with 0–2 reported sleep nights on family SES. However, our sample is significantly more likely to be white, have married parents, score lower on economic hardship, and score higher on family cohesion than adolescents excluded due to lack of sleep data (0–2 nights). This suggests that by missing more disadvantaged youth we may be underestimating the extent of low sleep duration in this sample, and possibly, the associations between risky family contexts and variance in sleep duration. We also excluded adolescents (n=2) whose mean sleep duration across the week was less than 3 or greater than 13 in line with past studies (Roenneberg, Allebrandt, Merrow, & Vetter, 2012).
Approximately 13% of the sample – 164 adolescents – was missing data on covariates. Over 60% of the 164 missing cases were due to caregivers not reporting household income, while 11% were missing on caregiver marital status. Most of the remaining missing cases result from missing reports of caregiver education (7%) and family cohesion (7%). We find no differences in mean hours of sleep between those with valid information and those with missing information. Due to statistical software limitations for our modeling technique, we were unable to use multiple imputation to preserve these cases. Finally, we excluded 17 adolescents living in foster care, with an unidentified guardian, or whose caregiver was classified as “other.” We drop adolescents in these unusual family settings as outliers and/or unclear caregiver situations. This resulted in an analytical sample of 1095 adolescents with 6276 sleep nights.
2.3. Measures
2.3.1. Dependent variable
Our dependent variable is the number of hours slept, as reported by each adolescent on a given day by responding to the smartphone EMA prompt. The first EMA prompt of each day asked youth to report the number of hours slept the night before. If the youth did not respond to the first EMA prompt, the question regarding sleep duration was pushed forward to subsequent prompts until the youth responded. This provided us with up to 7 days of sleep duration data per youth, including weekday and weekend nights. However, in some cases the youth did not respond to the EMA on a given day. We replaced missing EMA sleep duration with the sleep duration reported for that day in the exit survey at the end of the week, resulting in about 25% of our sample nights obtained from exit interview data. A study comparing various methods for assessing adolescent sleep times indicated few differences in survey-based sleep times when assessed in the past two weeks, compared with daily actigraphy and sleep diaries (Wolfson et al., 2003). We conducted sensitivity analyses and found the results were robust to excluding the exit interview days. Using the EMA only sample, the coefficients of interest remained in the same direction and of the similar magnitude. For some coefficients (income below $30,000, caregiver stress and financial hardship) p-values increased to p < .1, which may be attributed to the smaller sample size and possible loss of adolescents in high stress/poor families when excluding the exit graphic data.
2.3.2. Independent variables
The family context variables were created using the caregiver survey. For family structure, caregivers reported their current marital status, which we categorized as married, cohabiting, single/divorced/separated, and widowed. In initial models we separated out “never-married” from divorced and separated but did not find significant differences across these groups, resulting in the combined category in the final model. We considered other family structure measures, such as the presence of grandparents in the household; however, there were too few cases in these alternative family structures to adequately assess their effects.
Our SES measures were based on caregiver reports of their own education and household income. Education was provided as a categorical variable (less than high school, high school/GED, some college, college degree, graduate education), but we found the main distinction was between those with a college degree and those with less than a college degree. Thus, caregiver education was modeled as a dummy variable of college degree or higher education. We measured total annual household income as categories: less than under $30,000, $30,000-$60,000, $60,000-$150,000, and over $150,000 (reference category).
Family economic difficulties, caregiver distress and the related socioemotional environment were assessed through four variables: economic hardship, caregiver depressive symptoms, caregiver stress, and family cohesion. We assessed family economic hardship by averaging responses across three questions asking about financial difficulties related to buying things, paying rent/mortgage, and making utility payments during the previous year. Response categories included (1) no difficulties at all, (2) a little difficulty, (3) some difficulty, (4) quite a bit of difficulty, and (5) a great deal of difficulty. We averaged these scores across the three measures (α = 0.85). We hypothesized that rather than a linear effect, financial hardship was more likely to be associated with adolescents sleep when it was more than “a little.” Thus, we dichotomized financial hardship, where a score of more than 2 (average difficulty across the domains was “some,” “quite a bit,” or a “great deal”) was coded as 1, and 0 otherwise (little or no hardship).
Caregiver depression was measured using the validated CES-D short form, which includes questions related to experiencing obtrusive thoughts, feelings of hopelessness, feelings of loneliness, and perceptions that others were unfriendly over the course of the previous week (Cole, Rabin, Smith, & Kaufman, 2004). Respondents reported that they felt this way rarely (1 day), some of the time (1–2 days), moderate amount of time (3–4 days), and most/all of the time (5–7 days) for each question. We averaged their responses across 9 measures (α = 0.74) and used the continuous measure in the models.
Caregiver stress was measured based on totaling the scores across 9 items from the perceived stress scale, reverse coding the positively asked questions (Cohen, Kamarck, & Mermelstein, 1983). Caregivers were asked how often (0 = never to 4 = very often) they felt various aspects of stress (being out of control, stressed, couldn’t cope, not on top of things, etc.) in the past month (α = 0.82). We hypothesize that high levels of caregiver stress, compared with low or average stress, is most important for adolescents’ sleep patterns. Thus, we created a measure of “highly stressed” caregivers as those in the top 25% of the sample distribution. This corresponded with a score of 3 or greater.
Family cohesion was based on the caregiver’s answers to 9 questions about the family environment, including: family support, feelings of togetherness, family spirit, and how well the family got along (Boyd et al., 1997, Moos and Moos, 1996). Response categories asked caregivers if their perceptions and feelings were “mostly true” (1) or “mostly false” (0). The responses were averaged across the 9 items to produce an average cohesion score between 0 and 1 (α = 0.63). We reverse coded this variable to indicate less cohesion at higher levels, referring to the variable as lack of family cohesion, and entered it as a continuous variable in the models.
2.3.3. Control variables
The controls in this study included age of the youth (continuous), and gender of the youth (dummy coded with female as reference category). Youth race/ethnicity was reported by the caregiver as white, Black/African American, Asian, Native Hawaiian or other Pacific Islander, American Indian or Alaskan Native, Hispanic, or Other. Other included those reported as multiracial. We collapsed these groups into the following: White (reference), Black/African American (including any multiracial children who reported being Black/African American), Hispanic, and other. We also controlled for number of children in the household, caregiver age and caregiver gender. All covariates, along with the independent variables of interest were measured at the adolescent level. At the day-level, we also included a dummy variable indicating whether the reported sleep duration was for a school or non-school night.
2.4. Analytic strategy
To model both the mean and the within-subject variance in sleep duration, we employed a mixed effects location scale model (Hedeker & Nordgren, 2013). This approach advances the conventional multilevel model by allowing covariates to influence both the mean and IIV and incorporating the potential for heteroskedastic within-person variance. The model takes the following form: At level 1, let Yij be the sleep duration on day i for respondent j, where
Here, β0j is the intercept, βp are coefficients estimating the effects of P day-level covariates Xpij on sleep duration, and rij is an independent, normally distributed error term with mean 0 and with individual/day-specific variance .
At level two (between subjects), individual-level covariates, including family-level social and economic factors were included predicting mean sleep duration across the course of the week as follows:
Here γ00 is the intercept, γ0q are coefficients for Q individual-level covariates Wq, and u0j is an independent, normally distributed individual-level error term with mean 0 and variance .
Finally, the model assumes heteroskedastic within-subject variances and allows for both day- and individual-level predictors of variance in sleep duration:
The natural log of σij2 is assumed to be a linear function of S covariates, Zsj (here, person-level covariates), where π00 is the intercept, π0s are the effects of the covariates, and wij is an error term assumed to be normally distributed with mean 0 and variance . The same covariates were included in modeling the mean and variance.
To date, the mixed effects location-scale model has been used in only one other sleep study – an analysis of 54 participants with chronic insomnia (Ong, Hedeker, Wyatt, & Manber, 2016). We employed this modeling technique to estimate the associations between the family context measures and both mean and intra-individual variance in sleep, controlling for the demographic youth and caregiver characteristics and whether the reported sleep night was a school night or not. We estimated the effects of family structure first, and subsequently added family SES, family economic hardship and caregiver distress measures. Although the model estimates both the mean and IIV jointly, for clarity we present the results in two tables - one for coefficients on the mean, the other for coefficients on the variance. Given our interest in IIV in sleep, we present those results first, followed by the mean model results.
3. Results
Table 1 shows the descriptive statistics for our sample. The outcome of interest, sleep duration, was assessed at the night level. Nightly sleep duration had a mean of 8.1 h and ranged from 0–24 h across the full sample of sleep nights (N = 6276).1 Of all sleep nights assessed, 48% were school nights. At the adolescent level, 77% of our sample adolescents had a mean sleep duration across the week of less than 9 h per night.
Table 1.
Descriptive Statistics. Wave 1 AHDC youth ages 11–17 years with at least 3 sleep night reports. N = 1095 youth, n = 6276 nights.
| Variable | Mean | Std.Dev | Min | Max |
|---|---|---|---|---|
| Nightly sleep (n=6276) | ||||
| Number of hours slept | 8.08 | 2.02 | 0 | 24 |
| Night is a school night | 48% | 0 | 1 | |
| Family Structure | ||||
| Caregiver married | 58% | 0 | 1 | |
| Caregiver cohabiting | 9% | 0 | 1 | |
| Caregiver single | 32% | 0 | 1 | |
| Caregiver widowed | 1% | 0 | 1 | |
| Family SES | ||||
| Caregiver less than college degree | 53% | 0 | 1 | |
| Household income (Under $30k) | 33% | 0 | 1 | |
| Household income ($30-$60k) | 23% | 0 | 1 | |
| Household income ($60-$150k) | 31% | 0 | 1 | |
| Household income ($150k+) | 13% | 0 | 1 | |
| Family Stress | ||||
| Family economic hardship | 2 | 1 | 1 | 5 |
| Caregiver depression score | 1.6 | 0.5 | 1 | 3.6 |
| Caregiver perceived stress score | 2.5 | 0.7 | 1 | 4.6 |
| Lack of family cohesion score | 0.2 | 0.2 | 0 | 1 |
| Youth and Caregiver Demographics | ||||
| Youth age | 14.3 | 1.9 | 11 | 17 |
| Youth male | 46% | 0 | 1 | |
| Youth White | 50% | 0 | 1 | |
| Youth African American | 40% | 0 | 1 | |
| Youth Hispanic | 6% | 0 | 1 | |
| Youth other race | 4% | 0 | 1 | |
| Caregiver age | 45.5 | 8.1 | 27 | 81 |
| Caregiver male | 12% | 0 | 1 | |
| No. children in household | 2.0 | 1.2 | 1 | 8 |
The independent variables of interest and covariates reflect adolescent-level and family-level characteristics. In terms of family structure, over half of the adolescents lived in two, married-parent families (58%), 9% had a caregiver who was cohabiting, and 33% had caregivers that were either never married, divorced, separated or widowed. The family SES measures indicated that 53% of caregivers had less than a college degree and 33% of adolescents lived in families with total household income less than $30,000 per year. At the top of the distribution, 13% of adolescents lived in families with income totaling $150,000 or more in the past year.
For the family stress measures, family hardship ranged from 1–5 with a mean of 2, and 35% of adolescents’ caregivers reported significant hardship (scored more than 2). The average level of caregiver depression was 1.6 out of a possible score of 4. Perceived stress among caregivers was 2.5, on average, and the high-stress caregivers (top 25% of the distribution) had a mean perceived stress score of 3.4. Caregivers reported a mean of 0.2 on the 0–1 lack of family cohesion scale.
The covariates in indicate that the mean youth age was 14 years, and 46% were male. Almost half of the adolescents were white (50%), and 40% were African American. Most caregivers were women, with 12% male caregivers. Average caregiver age was 45 years, with a few cases of grandparent caregivers reflected in the maximum age of 81.
Table 2, Table 3 show the results from the regression models estimating family context associations with nightly sleep duration across the week. Although we estimated the mean and intra-individual variation in sleep duration simultaneously, for clarity, we split the results into two tables: Table 2 shows the results for IIV in sleep duration (our outcome of interest), and Table 3 contains the results for mean sleep duration.
Table 2.
Results from variance portion of the location-scale mixed model of adolescent sleep duration. Wave 1 AHDC youth with at least 3 sleep night reports. N = 1095 youth, n = 6276 nights.
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 |
|---|---|---|---|---|---|---|---|
| Tau (SE) | Tau (SE) | Tau (SE) | Tau (SE) | Tau (SE) | Tau (SE) | Tau (SE) | |
| Family Structure | |||||||
| Married | REF | REF | REF | REF | REF | REF | REF |
| Cohabitating | 0.36(0.13)** | 0.20(0.13) | 0.20(0.13) | 0.19(0.13) | 0.20(0.13) | 0.20(0.13) | 0.21(0.13) |
| Single | 0.28(0.09)** | 0.14(0.09) | 0.13(0.09) | 0.12(0.09) | 0.13(0.09) | 0.13(0.09) | 0.12(0.09) |
| Widowed | 0.11(0.31) | -0.04(0.31) | -0.06(0.31) | -0.06(0.31) | -0.12(0.31) | -0.04(0.31) | -0.11(0.31) |
| Family SES | |||||||
| College Educated | REF | REF | REF | REF | REF | REF | |
| No College | 0.21(0.09)* | 0.18(0.09)* | 0.19(0.09)* | 0.20(0.09)* | 0.19(0.09)* | 0.17(0.09) | |
| Household Income < 30k | 0.39(0.15)** | 0.29(0.15) | 0.33(0.15)* | 0.33(0.15)* | 0.36(0.15)* | 0.24(0.15) | |
| Household Income 30k-60k | 0.25(0.14) | 0.17(0.14) | 0.22(0.14) | 0.21(0.14) | 0.23(0.14) | 0.14(0.14) | |
| Household Income 60k–150k | 0.10(0.12) | 0.07(0.12) | 0.09(0.12) | 0.08(0.12) | 0.09(0.12) | 0.06(0.12) | |
| Household Income 150k+ | REF | REF | REF | REF | REF | REF | |
| Family Stress | |||||||
| Family economic hardship | 0.23(0.08)** | 0.18(0.09)* | |||||
| Caregiver depression | 0.18(0.08)* | ||||||
| High caregiver stress | 0.26(0.08)** | 0.19(0.09)* | |||||
| Lack of family cohesion | 0.38(0.19) | 0.22(0.2) | |||||
| Control Variables | |||||||
| School Day | -0.86(0.05)*** | -0.85(0.05)*** | -0.85(0.05)*** | -0.86(0.05)*** | -0.85(0.05)*** | -0.85(0.05)*** | -0.85(0.05)*** |
| Age of Youth | 0.04(0.02) | 0.03(0.02) | 0.03(0.02) | 0.03(0.02) | 0.03(0.02) | 0.03(0.02) | 0.03(0.02) |
| Male Youth | -0.07(0.07) | -0.06(0.07) | -0.07(0.07) | -0.06(0.07) | -0.06(0.07) | -0.05(0.07) | -0.06(0.07) |
| White Youth | REF | REF | REF | REF | REF | REF | REF |
| Black Youth | 0.22(0.08)** | 0.07(0.09) | 0.07(0.09) | 0.07(0.09) | 0.09(0.09) | 0.07(0.09) | 0.08(0.09) |
| Hispanic Youth | 0.22(0.16) | 0.15(0.16) | 0.16(0.16) | 0.16(0.16) | 0.17(0.16) | 0.15(0.16) | 0.17(0.16) |
| Other Race Youth | 0.25(0.18) | 0.21(0.18) | 0.20(0.18) | 0.20(0.18) | 0.23(0.18) | 0.21(0.18) | 0.21(0.18) |
| Caregiver Age | -0.02(0.01)** | -0.01(0.01)* | -0.01(0.01)* | -0.01(0.01)* | -0.01(0.01)* | -0.01(0.01)* | -0.01(0.01)* |
| Male Caregiver | 0.07(0.11) | 0.08(0.11) | 0.09(0.11) | 0.08(0.11) | 0.10(0.11) | 0.09(0.11) | 0.11(0.11) |
| No. Children in Household | 0.02(0.03) | 0.00(0.03) | -0.01(0.03) | -0.01(0.03) | -0.01(0.03) | 0.00(0.03) | -0.02(0.03) |
| Intercept | 0.99(0.37)** | 0.70(0.37) | 0.68(0.37) | 0.46(0.38) | 0.67(0.37) | 0.7(0.37) | 0.66(0.37) |
| (random scale SD) | 0.92(0.03)*** | 0.9(0.03)*** | 0.89(0.03)*** | 0.89(0.03)*** | 0.89(0.03)*** | 0.9(0.03)*** | 0.89(0.03)*** |
Notes: Standard errors in parentheses.
p<.05
p<.01
p<.001.
Table 3.
Results from mean portion of the location-scale mixed model of adolescent sleep duration. Wave 1 AHDC youth with at least 3 sleep night reports. N=1095 youth, n=6276 nights.
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 |
|---|---|---|---|---|---|---|---|
| Beta (SE) | Beta (SE) | Beta (SE) | Beta (SE) | Beta (SE) | Beta (SE) | Beta (SE) | |
| Family Structure | |||||||
| Married | REF | REF | REF | REF | REF | REF | REF |
| Cohabitating | -0.11(0.12) | -0.10(0.12) | -0.10(0.12) | -0.08(0.12) | -0.10(0.12) | -0.10(0.12) | -0.10(0.12) |
| Single | 0.00(0.08) | 0.01(0.08) | 0.02(0.08) | 0.03(0.08) | 0.02(0.08) | 0.02(0.08) | 0.02(0.08) |
| Widowed | 0.13(0.27) | 0.17(0.27) | 0.17(0.27) | 0.18(0.27) | 0.22(0.27) | 0.16(0.27) | 0.21(0.27) |
| Family SES | |||||||
| College Educated | REF | REF | REF | REF | REF | REF | |
| No College | 0.02(0.08) | 0.03(0.08) | 0.03(0.08) | 0.02(0.08) | 0.03(0.08) | 0.03(0.08) | |
| Household Income < 30k | -0.16(0.13) | -0.15(0.13) | -0.09(0.13) | -0.12(0.13) | -0.15(0.13) | -0.13(0.13) | |
| Household Income 30k–60k | -0.21(0.12) | -0.20(0.12) | -0.17(0.12) | -0.18(0.12) | -0.20(0.12) | -0.18(0.12) | |
| Household Income 60k–150k | -0.19(0.1) | -0.18(0.1) | -0.17(0.1) | -0.17(0.1) | -0.18(0.1) | -0.17(0.1) | |
| Household Income 150k+ | REF | REF | REF | REF | REF | REF | |
| Family Stress | |||||||
| Family economic hardship | -0.03(0.08) | 0.01(0.08) | |||||
| Caregiver depression | -0.20(0.07)** | ||||||
| High caregiver stress | -0.17(0.08)* | -0.16(0.08) | |||||
| Lack of family cohesion | -0.17(0.18) | -0.06(0.19) | |||||
| Control Variables | |||||||
| Intercept | 11.54(0.32)*** | 11.68(0.33)*** | 11.68(0.33)*** | 11.92(0.34)*** | 11.7(0.33)*** | 11.68(0.33)*** | 11.69(0.33)*** |
| School Day | -0.91(0.04)*** | -0.91(0.04)*** | -0.91(0.04)*** | -0.91(0.04)*** | -0.92(0.04)*** | -0.91(0.04)*** | -0.91(0.04)*** |
| Age of Youth | -0.23(0.02)*** | -0.23(0.02)*** | -0.23(0.02)*** | -0.23(0.02)*** | -0.23(0.02)*** | -0.23(0.02)*** | -0.23(0.02)*** |
| Male Youth | 0.11(0.06) | 0.11(0.06) | 0.11(0.06) | 0.10(0.06) | 0.11(0.06) | 0.10(0.06) | 0.11(0.06) |
| White Youth | REF | REF | REF | REF | REF | REF | REF |
| Black Youth | -0.25(0.07)*** | -0.24(0.08)** | -0.24(0.08)** | -0.23(0.08)** | -0.24(0.08)** | -0.23(0.08)** | -0.24(0.08)** |
| Hispanic Youth | 0.04(0.14) | 0.07(0.14) | 0.07(0.14) | 0.06(0.14) | 0.06(0.14) | 0.07(0.14) | 0.07(0.14) |
| Other Race Youth | -0.48(0.17)** | -0.46(0.16)** | -0.46(0.16)** | -0.45(0.17)** | -0.47(0.17)** | -0.46(0.16)** | -0.47(0.17)** |
| Caregiver Age | 0.01(0) | 0.01(0) | 0.01(0) | 0.01(0) | 0.01(0) | 0.01(0) | 0.01(0) |
| Male Caregiver | 0.10(0.09) | 0.10(0.09) | 0.10(0.09) | 0.09(0.09) | 0.09(0.09) | 0.10(0.09) | 0.09(0.09) |
| No. Children in Household | 0.01(0.03) | 0.01(0.03) | 0.01(0.03) | 0.02(0.03) | 0.02(0.03) | 0.01(0.03) | 0.02(0.03) |
| Alpha Intercept | -0.48(0.08)*** | -0.48(0.08)*** | -0.48(0.08)*** | -0.49(0.08)*** | -0.49(0.08)*** | -0.48(0.08)*** | -0.49(0.08)*** |
Notes: Standard errors in parentheses.
p<.05
p<.01
p<.001.
In Table 2, the results of the variance component of the models, positive coefficients indicate more intra-individual variation in nightly sleep duration (a worse outcome). Model 1 shows that adolescents living in single- and cohabiting-parent families had significantly more variation in nightly sleep duration during the week, than those with married parents. This was net of night-level and youth-level demographic control variables. Among the control variables, the school night coefficient (having school the next day vs night with no school the next day) was negative and significant, indicating less variance in sleep duration on school nights compared with non-school nights. The youth demographic correlates further showed that adolescent age was not associated with IIV in nightly sleep duration, but race/ethnicity was. African American adolescents had significantly higher IIV in nightly sleep duration compared to white adolescents.
Model 2, with family SES added, shows that youth with caregivers who had less than a college degree had significantly more variability in their nightly sleep duration than those with more educated caregivers. Further, adolescents in families with lower annual income, below $30,000 and between $30,000 and $60,000, had higher sleep variation than those in higher-income families, net of caregiver education and family structure. In this model, the family structure effect was reduced to non-significance. The race difference was also reduced to non-significance when family SES was added to the model (Models 1 vs. 2, Table 2).
Model 3 included the measure of family economic hardship. Adolescents in families experiencing some or great economic hardship in the past year had significantly higher IIV in sleep duration than those whose caregivers reported little or no hardship experience. The coefficient on the lowest income category was reduced to non-significance in this model, while caregiver education remained significant.
In Models 4 and 5 we added the caregiver distress covariates, as indicated by depression and stress to the variables included in Model 2. Both caregiver depression (p < .05) and caregiver stress (p < .01) were significantly associated with higher IIV in sleep duration net of family structure, SES and the control variables. We were unable to include both variables in the same model due to the relatively high correlation in the measures (r = 0.59).
Model 6 highlights the association between family cohesion and IIV sleep duration. Although the coefficient was not significant at the p < .05 level (p = .052) the effect size and direction was similar to the other family stress measures.
In our final model, we include economic hardship, caregiver stress and family cohesion together in the model, leaving out caregiver depression due to the high correlation with caregiver stress. We found that substantial economic hardship and caregiver stress remained significant in the final model where multiple family stress variables were included along with family structure and SES. We also tested a model with caregiver stress left out and caregiver depression included. Caregiver depression was not significantly associated with IIV in sleep when the economic hardship and lack of family cohesion variables were included in the model (results available upon request).
The additional model component reported at the bottom of Table 2, the standard deviation in the tau variance, is an important aspect of this modeling technique not included in standard multi-level modeling. The significance of this model component indicates that there are significant residual differences in the variation in individuals’ nightly sleep duration. If not included, the model would assume no residual variation in the within-variance across individuals (conditional on covariates in the model), which could result in biased standard errors.
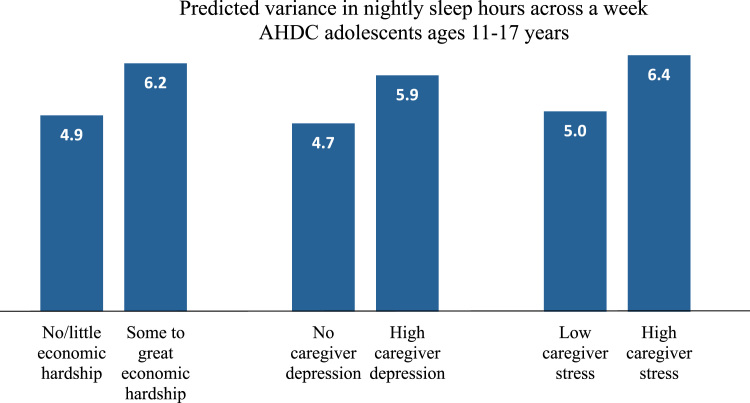
Using the above models 3–5, we calculated predicted variation in sleep duration for the family hardship and caregiver distress measures, as the family stress measures that were significantly (p < .05) associated with IIV in sleep duration in one or more models. In calculating the predictions, we set all other variables at their sample mean values to anchor our predictions around the average adolescent in the sample.
The first two bars indicate the predicted IIV in sleep duration for adolescents in families by economic hardship level. For the average adolescent in our sample, living in families experiencing low or no economic hardship had a predicted variance in sleep duration across the week of 4.9 h. Adolescents with sample average characteristics whose family experienced substantial economic hardship had a predicted 6.2 h variance in their nightly sleep duration across the week holding family structure, SES and control variables constant (see Fig. 1).
Fig. 1.
Estimated based on Models 3–5 variance component (Table 2), holding all other variables at the sample mean. N=1095 adolescents.
For the caregiver depression, we estimated the predicted IIV in sleep duration at the low (score = 1, no depressive symptoms) and the high end of the scale (top 10th percentile). As the second set of bars indicates, adolescents with caregivers who had no reported depressive symptoms had a predicted 4.7 h variation in sleep duration. Those with caregivers who reported high levels of depressive symptoms had a predicted variance in sleep duration of 5.9 hours over the week.
As the third set of bars shows, the marginal effect of high caregiver stress is similar to the hardship effect. We estimated the IIV in sleep duration to be 5.0 h for an average adolescent with low caregiver stress and 6.4 h for an average adolescent with a caregiver reporting high stress (those whose caregivers were in the top 25 percentile in perceived stress).
Since we estimated the IIV and mean components of sleep duration simultaneously in these models, the results for IIV indicate the associations between family contexts and IIV in adolescents’ nightly sleep duration net of their mean sleep duration over the week. We also show the associations between family contexts and mean sleep duration (Table 3), which are estimated while accounting for the adolescents’ IIV in sleep duration.
Overall, we see few significant associations between family contexts and mean level of adolescents’ sleep duration. The caregiver stress measures do seem to matter, with significant association between caregiver depressive symptoms and high caregiver stress and lower mean sleep duration (Table 3, Models 4 & 5). The other measures of family contexts – family structure, family SES, economic hardship, and low family cohesion – were not associated with mean sleep duration. We did find lower sleep duration on school nights, and among older, African American, and other race adolescents.
4. Discussion
Sufficient quality and quantity of sleep are important for a host of health outcomes, and are of particular concern during adolescence when social and biological processes reduce sleep duration. Although associated with multiple negative outcomes among adolescents, less attention has been given to the predictors of variation in nightly sleep duration (Becker et al., 2017). We inform research in this area by studying how key aspects of adolescents’ family social contexts were associated with individual variation (IIV) in nightly sleep duration in a population-based sample of adolescents. Our use of location-scale models allowed us to estimate which aspects of families were associated with instability in nightly sleep duration across the week after accounting for individuals’ mean nightly sleep duration, and while allowing for differing patterns of IIV in sleep duration among adolescents.
Our descriptive statistics indicated that the average sleep duration across the sleep nights was 8 h per night (48% of these nights were school nights), which is below the recommended 9 h per night (Hirshkowitz et al., 2015). The mean for our school nights was 7.5, which is comparable to a recent national survey where adolescents’ reported average sleep duration of 7 h and 43 min on weekdays (Zhang et al., 2017). At the adolescent level, 77% of our sample adolescents had a nightly mean duration across the week of less than 9 h of sleep per night.
Our regression results indicated important within-individual differences in sleep duration over the week-long period, which were associated with adolescents’ family contexts. Our results for the intra-individual variability (IIV) component of our models revealed that adolescents with an unmarried parent and those from lower SES families (caregiver education and household income) had significant associations with increased IIV in adolescents’ sleep duration, independent of their mean sleep duration that week. The association between unmarried parent families and higher IIV in sleep duration was reduced to non-significance when controlling for family SES variables. This indicates that much of the disadvantages found in unmarried parent families with respect to adolescent sleep patterns may be due to their lower SES status compared to married parent families. Further, after controlling for low family SES, the observed IIV difference between African American and white adolescents was reduced to non-significance.
Other measures of family disadvantage, including economic and psychosocial stressors, were also important for adolescents’ IIV in nightly sleep duration. Economic hardship, caregiver depression and caregiver stress were all significantly associated (p < .05) with increased IIV in sleep duration. Lack of family cohesion was marginally (p = .052) associated with IIV in sleep duration net of family structure and SES. In the final model, high economic hardship and high caregiver stress independently and additively predicted increased variability in sleep duration.
The IIV results are supported by a prior study of high school students, where unadjusted models of family structure indicated greater diary-reported standard deviation in bedtimes (the measure closest to IIV in the study) among adolescents in unmarried parent households. Although, the effect was reduced to insignificance when adjusting for SES and other family and individual characteristics in the full model, an interaction effect indicated an association remained for white adolescents (Troxel et al., 2014). We tested interaction effects but found no significant differences in family context effects by race (nor age or gender).
The mean portion of our models illustrated that few of our family context measures were associated with mean sleep duration assessed over a week among the adolescents when accounting for their IIV in sleep duration. Caregiver depression and high caregiver stress were the only family context variables significantly associated with lower mean sleep duration. This contrasts, somewhat, with several studies finding links between SES and sleep duration in adolescents using actigraphy to measure sleep (Bagley et al., 2015, Marco et al., 2012, Moore et al., 2011). Our lack of significant SES effects may be related to our different measurement of sleep or due to our statistical modeling approach that separated out the intra-individual variance component from the mean component of nightly sleep duration.
Several limitations of this study should be noted. First, we relied on sleep data as measured by adolescent reports (to the EMA prompt) rather than actigraphy, which may have affected variance in sleep hours if adolescents reported sleep times with less accuracy than actigraphy-based measures. Further, we lacked daily sleep data for all adolescents, and used exit interview data where possible to reduce missing data and sample selectivity. In sensitivity analyses, our results were robust to models excluding the exit interview data, but using these data may have introduced additional sources of recall bias related to reporting sleep duration at the end of the week rather than daily (as in the EMA data).
Our use of cross-sectional data, with family contexts and sleep patterns assessed during the same week did not allow us to consider the mediating pathways, longer term associations between family conditions and sleep variability, or changes in family contexts and IIV over time among adolescents.
Finally, although we did use a population-based sample, our study results generalize only to adolescents living in Franklin County, Ohio. Importantly, this sample was racially-diverse and included youth in and out of school.2
Notwithstanding these limitations, the findings of this study point us in new directions for future research. First and foremost, social contexts may have important effects on intra-individual variability in sleep not previously detected through the use of mean sleep duration or sleep efficacy measures. Studies that split up weekday and weekend sleep times as distinct dependent variables may miss important variation across the week that could indicate disadvantaged sleep patterns. That family contexts were, overall, more strongly associated with intra-individual variance rather than average sleep times suggests the need for further research on the social contexts that influence IIV in sleep duration during childhood and adolescence.
Secondly, studies that estimate mean and other general measures of sleep may be confounding sleep duration with sleep variability effects. Our models were able to separate out these aspects of weekly sleep patterns. This is important for producing better estimates of both overall sleep time and variation, which may have different associations with social contexts and distinct implications for adolescent health. We found that youth characteristics of age and race had stronger associations with average sleep duration, but family contexts mattered more for intra-individual variations in sleep duration across the week. This suggests that adolescents in more advantaged families are more likely to have stable sleep patterns, which may contribute to health disparities during adolescence and later in the life course. Caregiver depression and stress, however, were potentially important predictors of mean sleep duration among adolescents.
Third, through our use of mixed effects location-scale models, we provided new evidence that nightly sleep duration varies significantly over a week and that the pattern or distribution of this within-individual variance varies across individuals. Regression models that do not allow for differences in intra-individual variance assume, by default, equal variance in sleep patterns across individuals. Our study finds this assumption is not supported by the data, and that we can improve estimation of social determinants of sleep variance with models that allow individuals to have different patterns of sleep variance.
5. Conclusion
The importance of understanding social determinants of sleep among adolescents cannot be overstated. Although biological changes lead to “normal” reductions in sleep duration during this developmental period, social contexts clearly play a role in affecting individuals’ health and health disparities at this important stage of the life course (Maume, 2013). With growing evidence that irregular sleep patterns contribute to multiple health problems, more attention should be paid to the social determinants of adolescents’ intra-individual variation in nightly sleep duration. Family and other social contexts should be further studied in relation to sleep stability to better understand how policies may be developed to improve adolescent sleep and reduce related health disparities.
Acknowledgements
This research was supported by the National Institute on Drug Abuse (R01DA032371 awarded to Browning; R21DA034960 awarded to Ford), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (K01HD077063 awarded to Schmeer; P2CHD058484 awarded to the Ohio State University Institute for Population Research; R01HD088545 awarded to Calder), and the William T. Grant Foundation.
Acknowledgments
Declaration of interests
None.
Ethics approval
This research follows the standards and guidelines for the treatment of human subjects, protections of confidentiality, and the informed consent process set out by the American Sociological Association. The study design and procedures were reviewed and approved by the Institutional Review Board at Ohio State University before fieldwork began. Written parental permission and youth assent to participate in the study was obtained by trained interviewers prior to the beginning of the initial in-home interview.
Footnotes
Although a sleep duration of 24 h is unlikely, we did not have exit interview data to adjust these values. We estimated models dropping the nights with sleep durations ± 3 SD from the mean, and our results did not change.
It should be noted that, while including youth from a variety of school settings, the inclusion of youths’ school start times in our models did not change the results. School start times were associated with mean but not IIV in sleep duration.
References
- Adam E.K., Snell E.K., Pendry P. Sleep timing and quantity in ecological and family context: A nationally representative time-diary study. Journal of Family Psychology. 2007;21(1):4–19. doi: 10.1037/0893-3200.21.1.4. [DOI] [PubMed] [Google Scholar]
- Adkins D.E., Wang V., Dupre M.E., van den Oord E., Elder G.H. Structure and stress: Trajectories of depressive symptoms across adolescence and young adulthood. Social Forces. 2009;88(1):31–60. doi: 10.1353/sof.0.0238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagley E.J., Kelly R.J., Buckhalt J.A., El-Sheikh M. What keeps low-SES children from sleeping well: The role of presleep worries and sleep environment. Sleep Medicine. 2015;16(4):496–502. doi: 10.1016/j.sleep.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S.P., Sidol C.A., Van Dyk T.R., Epstein J.N., Beebe D.W. Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: A systematic review. Sleep Medicine Reviews. 2017;34:94–121. doi: 10.1016/j.smrv.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bei B., Manber R., Allen N.B., Trinder J., Wiley J.F. Too long, too short, or too variable? Sleep intraindividual variability and its associations with perceived sleep quality and mood in adolescents during naturalistically unconstrained sleep. Sleep. 2017;40(2) doi: 10.1093/sleep/zsw067. [DOI] [PubMed] [Google Scholar]
- Boyd C.P., Gullone E., Needleman G.L., Burt T. The family environment scale: Reliability and normative data for an adolescent sample. Family Process. 1997;36(4):369–373. doi: 10.1111/j.1545-5300.1997.00369.x. [DOI] [PubMed] [Google Scholar]
- Cavanagh S.E. Family structure history and adolescent adjustment. Journal of Family Issues. 2008;29(7):944–980. [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cole J.C., Rabin A.S., Smith T.L., Kaufman A.S. Development and validation of a Rasch-derived CES-D short form. Psychological Assessment. 2004;16(4):360–372. doi: 10.1037/1040-3590.16.4.360. [DOI] [PubMed] [Google Scholar]
- Conger R., Ge X., Elder G., Lorenz F., Simons R. Economic-stress, coercive family process, and developmental problems of adolescents. Child Development. 1994;65(2):541–561. [PubMed] [Google Scholar]
- Crosnoe R., Cavanagh S.E. Families with children and adolescents: A review, critique, and future agenda. Journal of Marriage Family. 2010;72(3):594–611. [Google Scholar]
- Cysarz D., Linhard M., Seifert G., Edelhaeuser F. Sleep instabilities assessed by cardiopulmonary coupling analysis increase during childhood and adolescence. Frontiers in Physiology. 2018;9:468. doi: 10.3389/fphys.2018.00468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl R.E., Lewin D.S. Pathways to adolescent health: Sleep regulation and behavior. Journal of Adolescent Health. 2002;31(6):175–184. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- Doom J.R., Mason S.M., Suglia S.F., Clark C.J. Pathways between childhood/adolescent adversity, adolescent socioeconomic status, and long-term cardiovascular disease risk in young adulthood. Social Science Medicine. 2017;188:166–175. doi: 10.1016/j.socscimed.2017.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felden É.P.G., Leite C.R., Rebelatto C.F., Andrade R.D., Beltrame T.S. Sleep in adolescents of different socioeconomic status: A systematic review. Revista Paulista de Pediatria (English Edition) 2015;33(4):467–473. doi: 10.1016/j.rpped.2015.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuligni A.J., Hardway C. Daily variation in adolescents' sleep, activities, and psychological well-being. Journal of Research on Adolescence. 2006;16(3):353–378. [Google Scholar]
- Guglielmo D., Gazmararian J.A., Chung J., Rogers A.E., Hale L. Racial/ethnic sleep disparities in US school-aged children and adolescents: A review of the literature. Sleep Health. 2018;4(1):68–80. doi: 10.1016/j.sleh.2017.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins S.S., Takeuchi D.T. Social determinants of inadequate sleep in US children and adolescents. Public Health. 2016;138:119–126. doi: 10.1016/j.puhe.2016.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynie D.L., Lewin D., Luk J.W., Lipsky L.M., O’Brien F., Iannotti R.J., Simons-Morton B.G. Beyond sleep duration: Bidirectional associations between chronotype, social jetlag, and drinking behaviors in a longitudinal sample of US high school students. Sleep. 2017 doi: 10.1093/sleep/zsx202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He F., Bixler E.O., Berg A., Imamura Kawasawa Y., Vgontzas A.N., Fernandez-Mendoza J.…Liao D. Habitual sleep variability, not sleep duration, is associated with caloric intake in adolescents. Sleep Medicine. 2015;16(7):856–861. doi: 10.1016/j.sleep.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthy People. (2020). Sleep Health | Healthy People 2020. Retrieved from 〈https://www.healthypeople.gov/2020/topics-objectives/topic/sleep-health/national-snapshot〉.
- Hedeker D., Mermelstein R.J., Demirtas H. An application of a mixed-effects location scale model for analysis of ecological momentary assessment (ema) data. Biometrics. 2008;64(2):627–634. doi: 10.1111/j.1541-0420.2007.00924.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedeker D., Nordgren R. Mixregls: A program for mixed-effects location scale analysis. Journal of Statistical Software. 2013;52(12):1–38. doi: 10.18637/jss.v052.i12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirshkowitz M., Whiton K., Albert S.M., Alessi C., Bruni O., DonCarlos L.…Ware J.C. National Sleep Foundation’s updated sleep duration recommendations: Final report. Sleep Health. 2015;1(4):233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- Malone S.K., Zemel B., Compher C., Souders M., Chittams J., Thompson A.L., Lipman T.H. Characteristics associated with sleep duration, chronotype, and social jet lag in adolescents. Journal of School Nursing. 2016;32(2):120–131. doi: 10.1177/1059840515603454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malone S.K., Zemel B., Compher C., Souders M., Chittams J., Thompson A.L., Lipman T.H. Social jetlag, chronotype, and body mass index in 14–17 year old adolescents. Chronobiology International. 2016:1–12. doi: 10.1080/07420528.2016.1196697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marco C.A., Wolfson A.R., Sparling M., Azuaje A. Family socioeconomic status and sleep patterns of young adolescents. Behavioral Sleep Medicine. 2012;10(1):70–80. doi: 10.1080/15402002.2012.636298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maume D.J. Social ties and adolescent sleep disruption. Journal of Health and Social Behavior. 2013;54(4):498–515. doi: 10.1177/0022146513498512. [DOI] [PubMed] [Google Scholar]
- McLanahan S. Diverging destinies: How children are faring under the second demographic transition. Demography. 2004;41(4):607–627. doi: 10.1353/dem.2004.0033. [DOI] [PubMed] [Google Scholar]
- Moore M., Kirchner H.L., Drotar D., Johnson N., Rosen C., Redline S. Correlates of adolescent sleep time and variability in sleep time: The role of individual and health related characteristics. Sleep Medicine. 2011;12(3):239–245. doi: 10.1016/j.sleep.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos R.H., Moos B.S. Family environment scale manual: Development, applications, research. Palo Alto. 1996 (Calif.) [Google Scholar]
- Nguyen-Louie T.T., Brumback T., Worley M.J., Colrain I.M., Matt G.E., Squeglia L.M., Tapert S.F. Effects of sleep on substance use in adolescents: A longitudinal perspective. Addiction Biology. 2018;23(2):750–760. doi: 10.1111/adb.12519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong J.C., Hedeker D., Wyatt J.K., Manber R. Examining the variability of sleep patterns during treatment for chronic insomnia: Application of a location-scale mixed model. Journal of Clinical Sleep Medicine: JCSM: Official Publication of the American Academy of Sleep Medicine. 2016;12(6):797–804. doi: 10.5664/jcsm.5872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park H., Tsai K.M., Dahl R.E., Irwin M.R., McCreath H., Seeman T.E., Fuligni A.J. Sleep and inflammation during adolescence. Psychosomatic Medicine. 2016;78(6):677–685. doi: 10.1097/PSY.0000000000000340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roenneberg T., Allebrandt K.V., Merrow M., Vetter C. Social jetlag and obesity. Current Biology. 2012;22(10):939–943. doi: 10.1016/j.cub.2012.03.038. [DOI] [PubMed] [Google Scholar]
- Troxel W.M., Lee L., Hall M., Matthews K.A. Single-parent family structure and sleep problems in black and white adolescents. Sleep Medicine. 2014;15(2):255–261. doi: 10.1016/j.sleep.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanek J.K., Spira A.P., Di J., Leroux A., Crainiceanu C., Zipunnikov V. Epidemiology of objectively measured bedtime and chronotype in US adolescents and adults: NHANES 2003–2006. Chronobiology International. 2018;35(3):416–434. doi: 10.1080/07420528.2017.1411359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahlstrom K.L., Berger A.T., Widome R. Relationships between school start time, sleep duration, and adolescent behaviors. Sleep Health. 2017;3(3):216–221. doi: 10.1016/j.sleh.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson A.R., Carskadon M.A., Acebo C., Seifer R., Fallone G., Labyak S.E., Martin J.L. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213–216. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- Zhang J.H., Paksarian D., Lamers F., Hickie I.B., He J.P., Merikangas K.R. Sleep patterns and mental health correlates in us adolescents. Journal of Pediatrics. 2017;182:137–143. doi: 10.1016/j.jpeds.2016.11.007. [DOI] [PubMed] [Google Scholar]