Abstract
Virtual healthcare is fast entering medical practice. Research into the feasibility of using it to teach treatment regimens such as exercise has not been explored. Maintaining an exercise regime can be difficult in cystic fibrosis: group classes risk potential infection, yet motivation is hard to maintain when alone. Tai Chi is a low-impact exercise and involves gentle, demanding movements. This study aimed to assess the feasibility, safety and acceptability of learning Tai Chi via an internet-based approach and compared patient-reported outcomes.
Children and adults with cystic fibrosis were recruited to a randomised, comparative effectiveness trial. Participants learnt eight Tai Chi movements; teaching was delivered in eight lessons over 3 months: delivered either via the internet or face-to-face. Assessments were at 3-monthly intervals over 9 months. Outcomes included health status, quality of life, sleep, mindfulness and instructor-led questions.
40 adults and children completed the eight sets of Tai Chi lessons. The median age was 22.8 years (range 6.1–51.5 years); 27 patients were female. The cohort comprised 26 adults (aged >16 years), six teenagers and eight children (aged <12 years). The groups were well matched. Feasibility and safety were demonstrated. Participants showed significant improvements in self-reported sleep, cough (both daytime and night-time), stomach ache and breathing. No differences in lung function, health status, quality of life, sleep or mindfulness was shown before or after completing the lessons.
Tai Chi was safe and well tolerated; it was feasible to deliver individual lessons via the internet, reducing concerns regarding cross-infection, and appeared to improve self-reported symptoms.
Short abstract
Randomised controlled trial of Tai Chi in cystic fibrosis http://ow.ly/YBHW30m7ffT
Introduction
The importance of the role of exercise and physical activity for people with cystic fibrosis (CF) has been emphasised since the 1970s and is now a well-established recommendation in clinical care [1]. Although the specific therapeutic effects of exercise in CF are still under investigation, correlations between aerobic fitness and survival, alleviation of dyspnoea, reductions in the rate of decline in lung function and improvements in quality of life scores have been reported [2]. The ability to practise and access instruction for more gentle exercises may be key to maintaining a regime that is suitable and beneficial to maintain quality of life during times of poor health. Tai Chi can be highly adaptable in nature and intensity.
A Cochrane review on CF concluded that there is evidence for beneficial effects on aerobic fitness and no negative side-effects [3]. It is clear from the literature that individuals with CF who increase their activity levels have a reduction in their decline in forced expiratory volume in 1 s (FEV1), compared with those who are not as active, supporting the view that even low-intensity activity is able to preserve lung function [4]. This is important, as many people with CF cannot sustain high-intensity training.
Tai Chi is a low-impact exercise that involves gentle yet demanding movements. It is practised with respiratory control, postural awareness and mental awareness (mindfulness). It can be practised standing or sitting [5]. Recent evidence suggests that Tai Chi benefits a variety of chronic conditions [6, 7], including chronic obstructive pulmonary disease [8, 9] and cardio-cerebrovascular and musculoskeletal problems [10]. It is suitable for a variety of age groups and fitness levels.
Cross-infection is a concern in CF; this has led to recommendations for total segregation in both clinical and social settings [1]. Group activities are actively discouraged, to lower the risk of cross-infection; this is isolating for patients. In parallel, and perhaps because of segregation advice, social media and web-based engagement are increasingly utilised by both the paediatric and adult CF population, although research into the delivery of care or treatments over the internet has not been well studied.
The literature about the use of Tai Chi in CF is sparse [11]. A pilot study in adults with CF was undertaken to assess the feasibility and usefulness of individual Tai Chi sessions, taking cross-infection into consideration [12]. The small group of 10 participants not only reported improvements in breathing, sleeping and reduced anxiety, but also the positive benefits of face-to-face contact with the Tai Chi teacher. The aims of this study were to assess the feasibility of delivering Tai Chi over the internet, to compare the effectiveness of Tai Chi to standard care and to compare two methods of delivering individualised Tai Chi lessons: either by face-to-face lessons or online “internet-delivered” lessons using Skype.
Methods
Participants
Participants with CF, aged ≥6 years were recruited from the Royal Brompton Hospital (London, UK) specialist adult and paediatric CF centres. Participants were required to have the time to complete the study, be within reasonable distance of the centre for teachers to travel to lessons and have internet access. Individuals were excluded if they were taking part in any other interventional study or if they had participated in the pilot study [12]. They were recruited opportunistically from outpatient clinics after responding to posters or approach by researchers and had no prior experience of practising Tai Chi. A power calculation suggested that 72 participants were needed, with the expectation that 60 would complete the study given an anticipated withdrawal rate of 17% based on the previous study [12].
Study design
A comparative effectiveness randomised trial design was conducted by dividing participants into two groups: Tai Chi lessons via Skype (the internet-delivered group) or lessons in a face-to-face format. After providing informed, written consent (parental consent for children and assent for older children), participants were randomised to either the face-to-face or the internet-delivered group. Random number tables were used to generate random sequencing for blocks of six participants in three age groups (6–11 years; 12–16 years and >16 years). Face-to-face Tai Chi sessions were usually delivered at home, but participants could select other suitable venues, including hospital if convenient. All sessions were taught individually, but participants could choose to invite a friend or family member to participate. Individualised face-to-face sessions were critical to reduce the risk of cross-infection. Participants were given a total of eight sessions delivered over a period of 3 months, timetabled at their own convenience. Parents and/or carers were required to be present for children aged <16 years.
The face-to-face group started their Tai Chi intervention at time zero; the internet-delivered group started their intervention 3 months later, allowing a 3-month period to act as a control group of standard care for the first face-to-face Tai Chi intervention.
Intervention
Tai Chi was taught to both groups by a team of six teachers trained in Wu style Tai Chi-Qigong, who were experienced in teaching people with health problems; they were specifically trained by one of the researchers (AM) to deliver the study intervention and were versed with the study protocol. Wu style Tai Chi is one of the five major family styles of Tai Chi taught across the world. It is known for its smooth rhythm and can be taught in an adaptable manner to accommodate an individual's needs. The lessons employed a short sequence of eight movements focused on developing key Tai Chi principles. These were selected for their specific effect on the respiratory system and assumed overall benefit in CF. Movements were adapted from the “eternal spring” Tai Chi-Qigong set, which uses animal movements. These included mindful breathing “jing gong” (still meditation) and “dong gong” (moving meditation), facilitating skeletal muscle movements, with the aim of improving circulation, respiration and mucus clearance. The start of each session began with postural and breath awareness, and at the end of each session self-massage was included, which reduces tension and aids peripheral circulation.
To aid adherence and to serve as a reminder, a specific DVD and booklet were developed, and stickers, diaries and t-shirts were offered. The DVD comprised three separate sections in order to appeal to different ages and abilities: adults; children and people who may be incapacitated or in hospital experiencing an exacerbation; and those who may need to practise seated. Participants were encouraged to practise the exercises for 5–10 min up to five times a week. Participants continued with their usual routine treatments throughout the study.
Outcome measures
Participants completed validated questionnaires at four main time points: at the start of the study, then 3-monthly until the 9-month end-point. Patient-reported outcome measures (PROMs) included the health-related quality-of-life measure Cystic Fibrosis Questionnaire – Revised (CFQ-R) [13–15], the Pittsburgh Sleep Quality Index (PSQI) [16], the Five Facet Mindfulness Scale (FFMS) [17] for adults aged >16 years and the Child and Adolescent Mindfulness Measure (CAMM) [18, 19] for children. Health status was recorded using body mass index (BMI), FEV1, forced vital capacity (FVC) and oxygen saturation at the same time points. Participants were not asked to keep a diary of events such as pulmonary exacerbations or admissions, in order to keep the burden of the study as low as possible.
During the interventional part of the study Tai Chi teachers administered a short questionnaire developed for the study (instructor's questionnaire) just prior to each of the eight taught sessions. This included questions about breathlessness using the modified Borg dyspnoea scale [20], any change in medication, exacerbations, antibiotic use, frequency and timing of practice, the feasibility of learning and practising Tai Chi, engagement with the process, levels of concentration and perceived health impact, as well as feedback on their participation in the study. “Perceived health” covered five questions on a Likert scale (1–4 corresponding to never, sometimes, often and always, respectively) asking for recall of symptoms in the past week related to 1) trouble sleeping, 2) stomach hurting, 3) cough during the day, 4) being woken by cough at night and 5) trouble breathing. A more general health question was recorded on a visual analogue scale (VAS), with zero being “as bad as it can be” and 100 “as good as it can be” for the question “In the last week where would you put your general health and wellbeing on this scale?”
Ethical approval and funding
The study received ethical approval from the London – Harrow Research Ethics Committee (14/LO/0327), was registered on the clinicaltrials.gov website (registration number NCT02054377) and the study protocol was published [21]. The study was funded by research grants from two charitable bodies (the Tracie Lawlor Trust for Cystic Fibrosis (the major grant funder) and the Cystic Fibrosis Trust); neither contributed to trial design nor this manuscript.
Analysis
Data were analysed using descriptive statistics and multivariate statistical analysis including parametric (t-test), nonparametric (Mann–Whitney) and linear regression models. Overall totals, where appropriate, mean numbers and standard deviations were calculated and significant differences, homogeneity and effect sizes calculated. The differences between time points in the study and the groups were used for calculation of these differences in the PROM questionnaires and clinical outcomes. SPSS (version 21; IBM, Armonk, NY, USA) and Excel (Microsoft, Redmond, WA, USA) were used.
Results
Demographic data
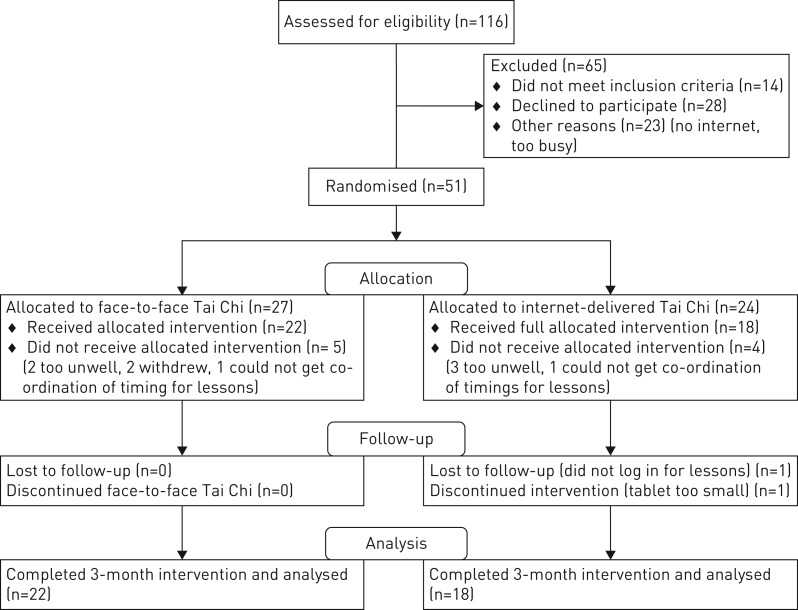
116 children and adults were invited to participate: 65 declined/were not eligible and 51 consented. 40 subjects completed all lessons; age range 6.1–51.5 years; 22 in the face-to-face group and 18 in the internet-delivered group. The CONSORT diagram (figure 1) shows reasons for withdrawal and table 1 demonstrates that there were no statistical differences (t-test) between the two groups at baseline.
FIGURE 1.
CONSORT 2010 flow diagram.
TABLE 1.
Baseline data at trial entry for both groups completing the 3-month Tai Chi intervention
| Face-to-face | Internet-delivered | |
| Subjects | 22 | 18 |
| Male | 6 | 7 |
| Female | 16 | 11 |
| Adults (>16 years) | 15 | 11 |
| Teenagers (12–15 years) | 3 | 3 |
| Children (6–11 years) | 4 | 4 |
| FEV1 % pred | ||
| <40% | 3 | 1 |
| 40–70% | 9 | 5 |
| >70% | 13 | 12 |
| Age | 22.75 (7.1–45.7) | 22.8 (6.1–51.5) |
| FVC# % pred | 87±18.1 | 94±14.1 |
| FEV1# % pred | 69±21.6 | 77±21.8 |
| Height m | 1.56±0.2 | 1.57±0.21 |
| Weight kg | 52.5±18.3 | 52.4±17.7 |
| BMI kg·m−2 | 20.4±4.1 | 20.4±3.2 |
| CFQ-R (respiratory) | 64.5±25.2 | 59.4±26.5 |
| CFQ-R (digestion) | 74.8±25.4 | 75.9±28.1 |
| Pittsburgh Sleep Quality Index | 11.7±8.1 | 11.8±8 |
| Five Facet Mindfulness Scale (adult) | 112.5±14.3 | 107.5±18.9 |
| CAMM (child) | 36.5±3.9 | 34.9±5.2 |
Data are presented as n, median (range) or mean±sd. FEV1: forced expiratory volume in 1 s; FVC: forced vital capacity; BMI: body mass index; CFQ-R: Cystic Fibrosis Questionnaire – Revised; CAMM: Child and Adolescent Mindfulness Measure. #: according to age, height, sex and race.
Clinical outcome measures
There were no significant differences in the clinical outcome measures (FVC, FEV1, oxygen saturation and BMI) for the first 3 months of the study when face-to-face Tai Chi was compared to standard care (with no Tai Chi) during the 3-month run-in period for the internet-delivered Tai Chi group. For the whole group of 40 individuals taught by either method the scores before starting Tai Chi compared to after the end of the 3 months of the Tai Chi intervention showed no statistically significant changes in FVC (−0.24% pred), FEV1 (1.47% pred) or BMI (0.006 kg·m−2). When comparing these changes between the face-to-face and internet-delivered groups before starting and after ending the Tai Chi intervention, there was no significant change.
PROM questionnaires
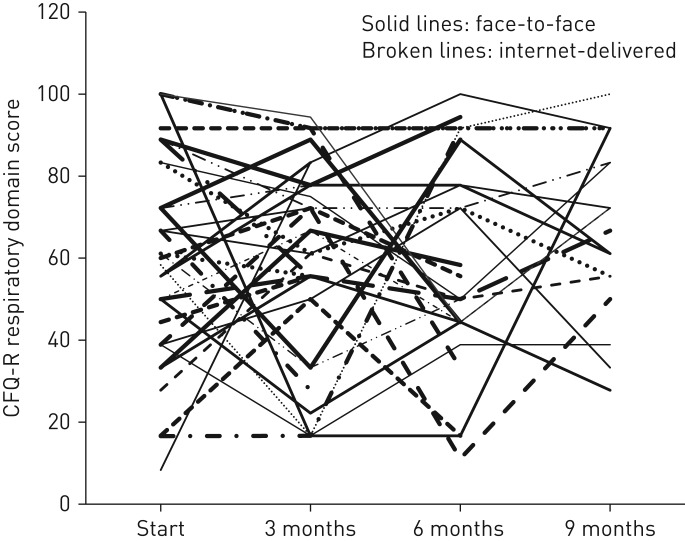
There were no significant differences between the two intervention groups pre and post the delivery of the Tai Chi intervention for the CFQ-R, PSQI, FFMS or CAMM questionnaires. Nor were there differences in these outcomes between the face-to-face group when compared to the no intervention/standard care control group, at 3 months. The individual patient variation over the 9 months of the trial for the CFQ-R was marked, with some individuals showing large variations from 8.33 to 100 and others reporting the same score over the entire duration of the 9 months. Figure 2 shows the substantial individual variation over time for the duration of the study for the respiratory domain for all study participants. Returns of the questionnaire at 9 months were low and no further analyses of the difference at this time were performed.
FIGURE 2.
Cystic Fibrosis Questionnaire – Revised (CFQ-R) respiratory domain results at 3-monthly intervals during the study. Each line represents an individual subject.
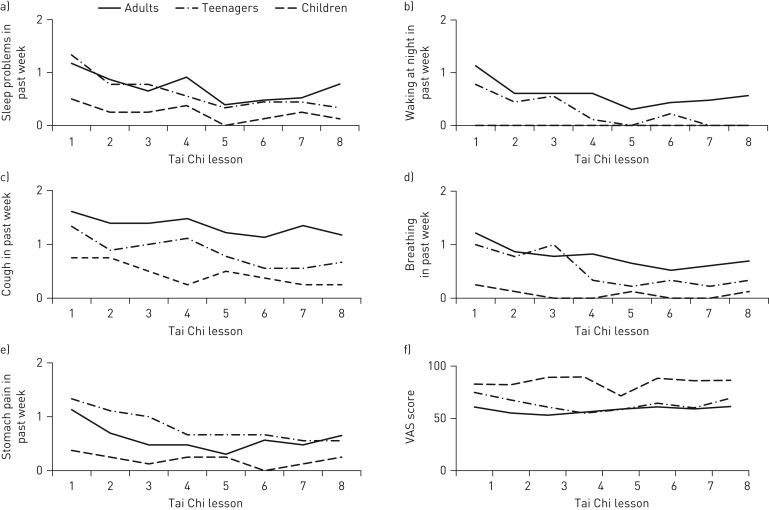
Instructor questionnaires
The instructor questionnaires were conducted on the day of the Tai Chi lessons, prior to the start of the session. A definite trend of improvement across the 3 months of the intervention was shown across the eight taught TC sessions. The graphs show the reducing symptom scores broken down into the three age groups (adults, teenagers and children) in figure 3a–e. The adults reported worse scores for all areas apart from “stomach hurting in the last week”, where teenagers appeared to have more problems. Children did not score any of the symptoms highly. The linear regression analysis for all five symptom domains on perceived health showed statistically significant trends of improvement when time of questionnaire was used as the independent variable (table 2). The VAS for general health and wellbeing did not show any change over time; children tended to report better scores than the adults (figure 3f). The Borg scores pre and post individual lessons did not show any significant change. Antibiotic use did not differ between the groups during the 3-month intervention period, with 14 in the face-to-face group and 13 in the internet-delivered group receiving additional oral antibiotic courses. Six people required a course of hospital i.v. antibiotics in the face-to-face group, and five in the internet-delivered group.
FIGURE 3.
Self-reported symptom scores immediately prior to each of the eight individual Tai Chi lessons for all participants. a) Trouble sleeping; b) waking due to cough; c) daytime cough; d) trouble breathing; e) stomach hurting (scale 0=never, 1=sometimes, 3=often, 4=always); f) visual analogue scores for general health and wellbeing.
TABLE 2.
Linear regression coefficients for instructor questionnaire domains, with time as the independent variable
| Dependent variable | Independent variable |
Unstandardised coefficients |
Standardised coefficient | Significance | |
| β | Standard error | β | |||
| Trouble sleeping | Constant | 0.881 | 0.113 | 0.000 | |
| Time | −0.065 | 0.022 | −0.160 | 0.004 | |
| Stomach ache | Constant | 0.786 | 0.114 | 0.000 | |
| Time | −0.051 | 0.023 | −0.126 | 0.025 | |
| Daytime cough | Constant | 1.317 | 0.104 | 0.000 | |
| Time | −0.060 | 0.021 | −0.161 | 0.004 | |
| Wake with cough | Constant | 0.638 | 0.096 | 0.000 | |
| Time | −0.055 | 0.019 | −0.160 | 0.004 | |
| Trouble breathing | Constant | 0.843 | 0.098 | 0.000 | |
| Time | −0.062 | 0.019 | −0.174 | 0.002 | |
Discussion
Data from this study show that it is feasible to give personalised Tai Chi lessons over the internet, allowing patients to engage in an original way to help them exercise. In addition, it is possible to deliver this teaching across a wide age range, with the youngest subject aged 6 years, and to patients with severe lung disease, with four subjects having lung function <40% pred. There were no significant differences between the internet-delivered and face-to-face teaching for the PROM analysis (the CFQ-R, PSQI, FFMS for adults aged >16 years and the CAMM for children). Participants reported benefits in self-perceived health for breathing, daytime and night-time cough, abdominal pain and sleep to the instructor during the 3-month intervention, irrespective of the way the Tai Chi was delivered. There were no statistical differences in the clinical outcome measures before and after the lessons finished, nor between the different teaching groups.
It is common knowledge that large numbers in the region of 200 are required in trials of CF interventions to show a significant change in lung function, so this finding is not surprising; however, these secondary outcomes were used in the study to ensure safety and make sure there were no significant detrimental effects associated with Tai Chi.
The focus of this relatively small-scale randomised controlled trial was to assess the feasibility of delivering Tai Chi via an online service such as Skype. We did not know whether people with CF would be willing to learn Tai Chi over the internet, nor did we know how well it could be taught, as we could not find any previous models for this approach. This study confirmed that a technically difficult and novel exercise intervention could be taught and successfully learnt over the internet, allowing the possibility that future studies could be conducted this way. Although participants were randomised into face-to-face or internet-delivered lessons, some preselection bias may have been present; we do not know whether a prior belief around the benefits of Tai Chi led to more females being enrolled into the study. We do know that lack of suitable computers or laptops may have excluded some potential participants.
This study was conducted in a largely urban area. This meant that most people had access to superfast broadband and devices that could support the technology needed for live online teaching. It may be more difficult to conduct a study or make learning over the internet readily available in more rural parts of the country or to people unable to afford internet connections that are fast enough. Only two people reported having no or inadequate technology, which precluded participation or was a reason for withdrawal. One of the younger participants withdrew because of difficulties following lessons on a small tablet device. Future studies might budget for and plan for the availability of appropriate technology. In addition, they could work towards delivering a more cost-effective approach using group classes of Tai Chi delivered over the internet.
The power calculation had been based upon a finding of a significant improvement in the CFQ-R respiratory domain in our original pilot study of only 10 patients [12]. This study did not quite meet the sample size of 60 published in our original study protocol [21], a not uncommon experience in research [22, 23]; this was partly due to the limited availability of teachers who could travel to participants’ homes, slow recruitment from the clinics and time constraints over the duration of the study. There was also some fall-out of participants from the time of consent to the start of Tai Chi lessons; there was a very low drop-out rate once lessons had started, suggesting that participants engaged well with the Tai Chi intervention in both groups. The remarkable variation for individuals (figure 2) in CFQ-R over the 9 months of the study suggests that it may not have been a suitable measure as a primary outcome, and questions the reliability of this outcome over long time periods, suggesting that its use in research over time will need to be restricted to larger studies if significance is to be demonstrated. This lack of improvement in quality of life is still disappointing when a recent study has suggested that it may be associated with physical fitness [24], so should have been a reasonable outcome measure in this type of exercise intervention study. However, as is known in CF, respiratory exacerbations will have played a role in the marked variation of CFQ-R score in this study, pulmonary exacerbations were not recorded and this is a limitation of the study.
The instructor-led questionnaires on perceived health in the week prior to lessons, shown in figure 3, show a significant improvement in reported symptoms over the course of the 3 months of intervention, with a slight plateau towards the eighth visit. The forms of Tai Chi chosen for the lessons in this study were directed specifically at the common symptoms of CF, including lung and abdominal symptoms, although it is not possible to define whether this improvement in reported symptoms in the instructor questionnaire is a result of Tai Chi. Participants may have become more comfortable with the teacher, although it would be expected that they would be more able to express their symptoms if this were the case, or they may have improved by merit of participating in a clinical trial. However, increasingly there is evidence in both healthy individuals and those with different disease states to suggest that there are a wide variety of both physical and psychological benefits associated with practising Tai Chi [25, 26], some of which may have direct relevance to people with CF [27–29]. In addition, it is now shown to be unlikely to result in any serious adverse events [30, 31].
Conclusions
CF is one of the commonest life-limiting genetic diseases in the United Kingdom. While survival has increased over the past three decades, cross-infection and complex treatment demands have led to the need for innovative and flexible healthcare support. Tai Chi appears to be a popular and useful method of offering an alternative method of exercise with benefits not previously considered, for example improvements in sleep, abdominal pain and cough. Additionally, Tai Chi can be performed by individuals of varying ages, abilities and disease severity with little or no detriment to health.
This study has shown that it is feasible to follow complex instructions over the internet, in this instance using Tai Chi as the model. It can be successfully taught over the internet with no safety or tolerability issues when compared with Tai Chi taught face-to-face. There was some initial scepticism about learning Tai Chi over the internet from participants; however, the majority of those who took part were enthusiastic in their reporting. As CF care becomes more complex and the number of people with the disease (particularly adults) increases over the next two decades, novel methods of care delivery such as innovative use of the internet and technology must be explored and introduced whenever possible or suitable.
Acknowledgements
Thanks to the study participants for their enthusiasm, engagement and suggestions; to the teachers (Jamie Brown, Jeremy Marshall, Faisal Mian, Nick Goss, Steve McColloch and Matt Cooper, all at the Seven Heavens Clinic for Integrated Medicine, London, UK); our funders, the Wu Shi Taiji and Qi Gong Association, UK, in particular, Michael Acton for his advice and guidance on the Tai Chi intervention. Thanks also go to Penny Agent (Royal Brompton Hospital, London, UK) and Emma Lake (patient advocate), who contributed to the design of the study.
Footnotes
This study was registered at www.clinicaltrials.gov with identifier number NCT02054377. The study protocol is already published (https://doi.org/10.1007/s11655-015-2150-1). Individual patient data for the study are single-centre, and as such will not be released because of the risk of identification of subjects. The trial data will be held in line with current good clinical practice recommendations.
Conflict of interest: S.B. Carr reports receiving personal fees and nonfinancial support for service on an advisory board, and accommodation and travel expenses to the advisory board and scientific committees from Vertex Pharmaceuticals, advisory board fees from Chiesi Pharmaceuticals and lecture fees from Teva Pharmaceuticals, outside the submitted work.
Conflict of interest: P. Ronan has no conflicts of interest to declare.
Conflict of interest: A. Lorenc has nothing to disclose.
Conflict of interest: A. Mian has nothing to disclose.
Conflict of interest: S.L. Madge has nothing to disclose.
Conflict of interest: N. Robinson has no conflicts of interest to declare.
Support statement: Research grants were received from the Tracie Lawlor Trust for Cystic Fibrosis and the Cystic Fibrosis Trust, UK.
References
- 1.Kerem E, Conway S, Elborn S, et al. . Standards of care for patients with cystic fibrosis: a European consensus. J Cyst Fibros 2005; 4: 7–26. [DOI] [PubMed] [Google Scholar]
- 2.Rand S, Prasad SA. Exercise as part of a cystic fibrosis therapeutic routine. Expert Rev Respir Med 2012; 6: 341–351. [DOI] [PubMed] [Google Scholar]
- 3.Radtke T, Nolan SJ, Hebestreit H, et al. . Physical exercise training for cystic fibrosis. Cochrane Database Syst Rev 2015; 6: CD002768. [DOI] [PubMed] [Google Scholar]
- 4.Schneiderman JE, Wilkes DL, Atenafu EG, et al. . Longitudinal relationship between physical activity and lung health in patients with cystic fibrosis. Eur Respir J 2014; 43: 817–823. [DOI] [PubMed] [Google Scholar]
- 5.Lee KY, Hui-Chan CW, Tsang WW. The effects of practicing sitting Tai Chi on balance control and eye-hand coordination in the older adults: a randomized controlled trial. Disabil Rehabil 2015; 37: 790–794. [DOI] [PubMed] [Google Scholar]
- 6.Solloway MR, Taylor SL, Shekelle PG, et al. . An evidence map of the effect of Tai Chi on health outcomes. Syst Rev 2016; 5: 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jahnke R, Larkey L, Rogers C, et al. . A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot 2010; 24: e1–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu W, Liu X, Wang L, et al. . Effects of Tai Chi on exercise capacity and health-related quality of life in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2014; 9: 1253–1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ngai SP, Jones AY, Tam WW. Tai Chi for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev 2016; 6: CD009953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li G, Yuan H, Zhang W. Effects of Tai Chi on health related quality of life in patients with chronic conditions: a systematic review of randomized controlled trials. Complement Ther Med 2014; 22: 743–755. [DOI] [PubMed] [Google Scholar]
- 11.Lorenc AB, Wang Y, Madge SL, et al. . Meditative movement for respiratory function: a systematic review. Respir Care 2014; 59: 427–440. [DOI] [PubMed] [Google Scholar]
- 12.Lorenc A, Mian A, Madge S, et al. . CF-CATS: an uncontrolled feasibility study of using tai chi for adults with cystic fibrosis. Europ J Integr Med 2013; 5: 476–486. [Google Scholar]
- 13.Quittner AL, Sawicki GS, McMullen A, et al. . Erratum to: Psychometric evaluation of the Cystic Fibrosis Questionnaire-Revised in a national, US sample. Qual Life Res 2012; 21: 1279–1290. [DOI] [PubMed] [Google Scholar]
- 14.Quittner AL, Modi AC, Wainwright C, et al. . Determination of the minimal clinically important difference scores for the Cystic Fibrosis Questionnaire-Revised respiratory symptom scale in two populations of patients with cystic fibrosis and chronic Pseudomonas aeruginosa airway infection. Chest 2009; 135: 1610–1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quittner AL, Buu A, Messer MA, et al. . Development and validation of The Cystic Fibrosis Questionnaire in the United States: a health-related quality-of-life measure for cystic fibrosis. Chest 2005; 128: 2347–2354. [DOI] [PubMed] [Google Scholar]
- 16.Buysse DJ, Reynolds C 3rd, Monk TH, et al. . The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28: 193–213. [DOI] [PubMed] [Google Scholar]
- 17.Baer R, Smith GT, Hopkins J, et al. . Using self-report assessment methods to explore facets of mindfulness. Assessment 2006; 13: 27–45. [DOI] [PubMed] [Google Scholar]
- 18.Greco LA, Baer RA, Smith GT. Assessing mindfulness in children and adolescents: development and validation of the Child and Adolescent Mindfulness Measure (CAMM). Psychol Assess 2011; 23: 606–614. [DOI] [PubMed] [Google Scholar]
- 19.Greco LA, Lambert W, Baer RA. Psychological inflexibility in childhood and adolescence: development and evaluation of the Avoidance and Fusion Questionnaire for Youth. Psychol Assess 2008; 20: 93–102. [DOI] [PubMed] [Google Scholar]
- 20.Balfour-Lynn IM, Prasad SA, Laverty A, et al. . A step in the right direction: assessing exercise tolerance in cystic fibrosis. Pediatr Pulmonol 1998; 25: 278–284. [DOI] [PubMed] [Google Scholar]
- 21.Lorenc A, Ronan P, Mian A, et al. . Cystic Fibrosis - Children and Adults Tai Chi Study (CF CATS2): can Tai Chi improve symptoms and quality of life for people with cystic fibrosis? Second phase study protocol. Chin J Integr Med 2015; 10.1007/s11655-015-2150-1. [DOI] [PubMed] [Google Scholar]
- 22.Kadam RA, Borde SU, Madas SA, et al. . Challenges in recruitment and retention of clinical trial subjects. Perspect Clin Res 2016; 7: 137–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McDonald AM, Knight RC, Campbell MK, et al. . What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies. Trials 2006; 7: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hebestreit H, Schmid K, Kiesser S, et al. . Quality of life is associated with physical activity and fitness in cystic fibrosis. BMC Pulm Med 2014; 14: 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jahnke R, Larkey L, Rogers C, et al. . A comprehensive review of health benefits of Qigong and Tai Chi. Am J Health Promot 2010; 24: e1–e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang C-W, Chan CHY, Ho RTH, et al. . Managing stress and anxiety through qigong exercise in healthy adults: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Altern Med 2014; 14: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holmes ML, Manor B, Hsiehe W-H, et al. . Tai Chi training reduced coupling between respiration and postural control. Neurosci Lett 2016; 610: 60–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Qiu Z-H, Guo H-X, Lu G, et al. . Physiological responses to Tai Chi in stable patients with COPD. Respir Physiol Neurobiol 2016; 221: 30–34. [DOI] [PubMed] [Google Scholar]
- 29.Leung RWM, McKeough ZJ, Peters MJ, et al. . Experiences and perceptions of the short-form Sun-style Tai Chi training in Caucasians with COPD. Eur J Integr Med 2015; 7: 131–135. [Google Scholar]
- 30.Wieland LS, Santesso N. A summary of a Cochrane review: Tai chi for chronic obstructive pulmonary disease (COPD). Eur J Integr Med 2016; 8: 894–895. [Google Scholar]
- 31.Wayne PM, Berkowitz BS, Litrownik DE, et al. . What do we really know about the safety of Tai Chi?: a systematic review of adverse event reports in randomized trials. Arch Phys Med Rehabil 2014; 95: 2470–2483. [DOI] [PMC free article] [PubMed] [Google Scholar]